Abstract
Purpose:
Blockade of the angiotensin-renin system, with angiotensin converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs), has been shown to improve cardiac outcomes following myocardial infarction and delay progression of heart failure. Acromegaly is associated with a disease-specific cardiomyopathy, the pathogenesis of which is poorly understood.
Methods:
The cardiac indices of patients with active acromegaly with no hypertension (Group A, n=4), established hypertension not taking ACEi/ARBs (Group B, n=4) and established hypertension taking ACEi/ARBs (Group C, n=4) were compared using cardiac magnetic imaging.
Results:
Patients taking ACEi/ARBs had lower end diastolic volume index (EDVi) and end systolic volume index (ESVi) than the other 2 groups ([C] 73.24 vs. [A] 97.92 vs. [B] 101.03 ml/m 2 , ANOVA p=0.034, B vs. C p<0.01). Groups A and B had EDVi and ESVi values at the top of published reference range values; Group C had values in the middle of the range.
Conclusion:
Acromegaly patients on ACEi/ARBs for hypertension demonstrate improved cardiac indices compared to acromegaly patients with hypertension not taking these medications. Further studies are needed to determine if these drugs have a beneficial cardiac effect in acromegaly in the absence of demonstrable hypertension.
Key words: pituitary, acromegaly, cardiac magnetic resonance, renin-angiotensin
Introduction
Blockade of the renin-angiotensin system, using angiotensin converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs), has been shown to reduce left ventricle (LV) remodeling in patients with myocardial infarction and delay the disease progression in heart failure 1 2 3 . Patients with growth hormone (GH) excess (acromegaly) develop a disease-specific cardiomyopathy associated with biventricular hypertrophy and diastolic dysfunction, that progresses to fulminant cardiac failure if left untreated 4 5 6 . In this preliminary study we compared the cardiac indices of 12 patients with active acromegaly, 4 of whom had no diagnosis of hypertension, 4 with an established diagnosis of hypertension on ACEi or ARBs and 4 with an established diagnosis of hypertension not taking these classes of drugs. Cardiac indices were compared using cardiac magnetic resonance imaging (CMR).
Material and Methods
12 patients with active acromegaly (clinical features, raised insulin-like growth factor 1 [IGF1] and failure to suppress GH on oral glucose tolerance testing) who were about to commence therapy underwent CMR to assess cardiac function and morphology: LV mass index (LVMi); end diastolic volume index (EDVi); end systolic volume index (ESVi); ejection fraction (EF). Measurements were indexed to body surface area. CMR was performed on a Philips Achieva CV 1.5 Tesla MRI scanner (Philips Medical Systems, Guildford, UK). Standard protocols were used. In this observational study, patients were divided into 3 groups: those with no known history of hypertension (A); those with a known diagnosis of hypertension not currently taking ACEi/ARB (B) and those with a known diagnosis of hypertension taking ACEi/ARB (C). Groups B and C patients may also have been taking additional antihypertensive medication ( Table 1 ). Weight, height and blood pressure, serum IGF1 and fasting glucose levels were recorded. Patients with known ischaemic heart disease or heart failure were excluded. Multi-centre ethical approval was given by the local Research Ethics Committee (06/Q0401/53). Statistics were calculated using ANOVA with Bonferroni correction.
Table 1 List of anti-hypertensives patients were on.
| Group B | Group C | ||
|---|---|---|---|
| Patient | Anti-hypertensives | Patient | Anti-hypertensives |
| 5 | Bendrofluazide | 3 | Ramipril |
| 7 | Amiloride Cyclopenthiazide | 4 | Ramipril Bendrofluazide |
| 9 | Atenolol | 10 | Ramipril |
| 11 | None | 12 | Losartan Amlodipine Doxazosin |
Results
Patient characteristics are given in Table 2 , with no significant difference in IGF-1, blood pressure and fasting glucose. Group C patients were older and tended to have higher baseline blood pressure values than the other 2 groups. There was no difference in LVMi between the 3 groups. No patient had evidence of frank heart failure (all had an EF within normal limits). Patients in Group C had lower EDVi and ESVi than the other 2 groups ( Fig. 1 ). Patients in Groups A and B had EDVi and ESVi values at the top of published reference range values. Patients in Group C had values in the middle of the reference range 7 .
Table 2 Patient characteristics. Data given as group mean and [SD]. BP – blood pressure.
| Group A (n=4) | Group B (n=4) | Group C (n=4) | P-value | |
|---|---|---|---|---|
| Number of females | 2/4 | 3/4 | 3/4 | N/A |
| Age (years) | 41.8 [7.6] | 54.5 [10.6] | 62.8 [11.2] | 0.043 |
| IGF1 (SDS) | 11.1 [5.5] | 19.0 [17.2] | 14.4 [11.1] | 0.669 |
| Systolic BP (mmHg) | 125 [26] | 133 [23] | 147 [15] | 0.392 |
| Diastolic BP (mmHg) | 74 [17] | 76 [12] | 82 [6] | 0.655 |
| Fasting Glucose (mmol/L) | 5.5 [0.82] | 5.1 [0.44] | 5.8 [1.13] | 0.483 |
Fig. 1.
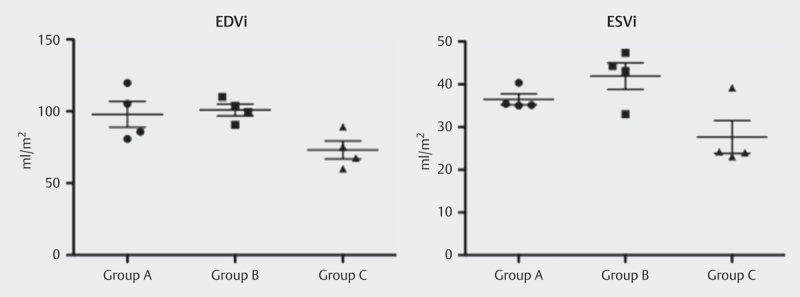
Graph comparing EDVi and ESVi in the 3 groups. There is a significant difference (p<0.01) between Group B and Group C. Error bars indicate SEM.
Discussion
This preliminary study indicated that patients taking ACEi/ARBs had lower end diastolic volume index (EDVi) and end systolic volume index (ESVi) than the other 2 groups including patients with no hypertension or hypertension treated with other drugs. While patients in group C were older and tended to have a higher mean blood pressure than groups A and B, this, if anything, should have increased the prevalence of cardiac remodeling in this group whereas the converse was seen with reduced remodeling, adding more evidence to the suggestion that ACEi/ARBs were influential in reducing EDVi and ESVi.
EDVi and ESVi are markers of cardiac remodeling, the process of change in size, shape and function of the heart, arising from cardiac load or injury 8 . As this process continues, heart failure develops and a reduction in EF is seen. ACEi and ARBs have been shown to delay progression of ischaemic heart failure and to improve survival through prevention and possible reversal of this remodeling process 1 3 9 10 .
The reasons for the improvement in LV EDVi and ESVi in patients treated with ACEi/ARBs are likely to be multifactorial. Firstly, acromegalic cardiomyopathy appears to be more marked in patients who have concurrent hypertension 11 . Additionally, acromegaly may be associated with increased serum aldosterone levels 12 . Blockade of the renin-angiotensin pathway will reduce the effects of aldosterone excess, reducing cardiac pre-load and possibly local myocardial response to aldosterone excess, thought to play a part in promoting remodeling 8 . Furthermore, it has been found that ACEi can attenuate the ability of IGF1 to produce cardiac fibroblast proliferation, indicating that these medications may have a direct effect on the response of the myocardium to GH action, directly inhibiting the development of acromegalic cardiomyopathy 13 .
This study did not demonstrate any reduction in LVMi associated with ACEi/ARB use, although this may be related to group size. Given the changes seen in EDVi and ESVi, and the lower mean LVMi in group C compared to group B, it would be interesting to address this in a larger study.
It should be noted that ACEi are not more efficacious in reducing cardiovascular morbidity or mortality than other forms of anti-hypertensive medications in patients without acromegaly 14 . However, the changes seen in this preliminary study suggest that patients with acromegaly may derive benefits from these medications over and above those arising simply from the normalisation of hypertension.
The main limitation of this study is the small sample size. We note that the study was open to several large UK centres for 3 years and this was the number of acromegaly patients who fulfilled inclusion criteria and agreed to take part in the study. In such a rare condition, greater number of patients is often difficult to achieve. Albeit a small sample, these are the first data suggesting that ACEi/ARBs may have a significant benefit in acromegaly patients over and above normalisation of blood pressure.
Conclusion
In this preliminary study, acromegaly patients with hypertension taking ACEi/ARBs demonstrated evidence of less cardiac remodeling than those taking alternative anti-hypertensives. We suggest that these agents should be considered first line anti-hypertensives in patients with this diagnosis. Larger studies are needed to confirm these findings and determine if there is a role using these medications in patients with active acromegaly who have not yet developed hypertension.
Acknowledgements
This work forms part of the research themes contributing to the translational research portfolio of Barts Cardiovascular Biomedical Research Unit, which is supported and funded by the National Institute for Health Research. The study was supported by unrestricted research grants from Pfizer and Novartis. Declaration of interests: MK is a member of the Scientific Advisory Board of Pfizer.
Footnotes
Conflict of Interest None.
References
- 1.Suzuki H, Kusuyama T, Omori Y et al. Inhibitory effect of candesartan cilexetil on left ventricular remodeling after myocardial infarction. Int Heart J. 2006;47:715–725. doi: 10.1536/ihj.47.715. [DOI] [PubMed] [Google Scholar]
- 2.Bazzino O, Navarro Estrada J L, Sosa Liprandi A et al. Early treatment with low-dose enalapril after acute myocardial infarction: an equilibrium radionuclide angiographic study. Enalapril despues del Infarto (EDI) Trial Investigators. J Nucl Cardiol. 1997;4:133–139. doi: 10.1016/s1071-3581(97)90062-3. [DOI] [PubMed] [Google Scholar]
- 3.Greenberg B, Quinones M A, Koilpillai C et al. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation. 1995;91:2573–2581. doi: 10.1161/01.cir.91.10.2573. [DOI] [PubMed] [Google Scholar]
- 4.Sacca L, Cittadini A, Fazio S. Growth hormone and the heart. Endocr Rev. 1994;15:555–573. doi: 10.1210/edrv-15-5-555. [DOI] [PubMed] [Google Scholar]
- 5.Colao A, Marzullo P, Di Somma C et al. Growth hormone and the heart. Clin Endocrinol. 2001;54:137–154. doi: 10.1046/j.1365-2265.2001.01218.x. [DOI] [PubMed] [Google Scholar]
- 6.Clayton R N. Cardiovascular function in acromegaly. Endocr Rev. 2003;24:272–277. doi: 10.1210/er.2003-0009. [DOI] [PubMed] [Google Scholar]
- 7.Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel E R et al. Normal values for cardiovascular magnetic resonance in adults and children. J Cardiovasc Magn Reson. 2015;17:29. doi: 10.1186/s12968-015-0111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohn J N, Ferrari R, Sharpe N. Cardiac remodeling-concepts and clinical implications: A consensus paper from an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000;35:569–582. doi: 10.1016/s0735-1097(99)00630-0. [DOI] [PubMed] [Google Scholar]
- 9.Konstam M A, Rousseau M F, Kronenberg M W et al. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. SOLVD Investigators. Circulation. 1992;86:431–438. doi: 10.1161/01.cir.86.2.431. [DOI] [PubMed] [Google Scholar]
- 10.Konstam M A, Kronenberg M W, Rousseau M F et al. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dilatation in patients with asymptomatic systolic dysfunction. SOLVD (Studies of Left Ventricular Dysfunction) Investigators. Circulation. 1993;88:2277–2283. doi: 10.1161/01.cir.88.5.2277. [DOI] [PubMed] [Google Scholar]
- 11.Fazio S, Cittadini A, Sabatini D et al. Evidence for biventricular involvement in acromegaly: a Doppler echocardiographic study. Eur Hear J. 1993;14:26–33. doi: 10.1093/eurheartj/14.1.26. [DOI] [PubMed] [Google Scholar]
- 12.Marks P, Vincent R, Wilson B et al. Aldosterone in acromegaly. Am J Med Sci. 1984;287:16–19. doi: 10.1097/00000441-198405000-00005. [DOI] [PubMed] [Google Scholar]
- 13.van Eickels M, Vetter H, Grohé C. Angiotensin-converting enzyme (ACE) inhibition attenuates insulin-like growth factor-I (IGF-I) induced cardiac fibroblast proliferation. Br J Pharmacol. 2000;131:1592–1596. doi: 10.1038/sj.bjp.0703740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansson L, Lindholm L H, Niskanen L et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet. 1999;353:611–616. doi: 10.1016/s0140-6736(98)05012-0. [DOI] [PubMed] [Google Scholar]


