Abstract
Up to 45% of new mothers have reported experiencing birth trauma. For some individuals who have experienced a traumatic event, there can be a positive legacy called posttraumatic growth. Using Tedeschi and Calhoun’s Posttraumatic Growth Model as the theoretical framework, the purpose of this pilot study was to determine levels of posttraumatic stress, core beliefs disruption, and posttraumatic growth in women who have experienced traumatic childbirth. Thirty mothers completed the Posttraumatic Stress Disorder Symptom Scale-Self Report, Core Beliefs Inventory, and Posttraumatic Growth Inventory. Type of birth and length of time since the traumatic birth occurred predicted 38% of the variance in posttraumatic growth. In order to help mothers, childbirth educators need to understand the process involved in posttraumatic growth.
Keywords: posttraumatic growth, posttraumatic stress, traumatic childbirth
Traumatic childbirth is an international public health problem. Examples from various countries reporting birth trauma include Japan (Takegata et al., 2017), Turkey (Gökçe İsbİr et al., 2016), and the United Kingdom (Thomson & Downe, 2016). Up to 45% of new mothers have reported experiencing a traumatic birth (Alcorn, O’Donovan, Patrick, Creedy, & Devilly, 2010). In their meta-analysis, Yildiz, Ayers, and Phillips (2017) reported the mean prevalence of posttraumatic stress disorder (PTSD) in relation to birth trauma in community samples was 4.0% and 18.5% in high-risk groups. Prior mental health disorders and poor quality of provider interaction are risk factors for birth trauma (Simpson & Catling, 2016). Women who are survivors of sexual abuse are at risk for retraumatization during childbearing (LoGiudice, 2016).
Traumatic childbirth has ever widening ripple effects for mothers (Beck, 2015) which childbirth educators need to be aware of. The few minutes or hours that a woman perceived she has been traumatized during birth can be likened to a pebble dropped into a pond resulting in ripples spreading out in the water. Some of these ripples resulting from traumatic childbirth can impact mothers’ breastfeeding experiences (Beck & Watson, 2008), the anniversary of their traumatic births (Beck, 2006), and their subsequent births (Beck & Watson, 2010).
For some persons who have experienced a traumatic event, there can be a positive legacy which is called posttraumatic growth (Tedeschi & Calhoun, 1996). Posttraumatic growth has been reported in a broad range of groups who have experienced traumatic events, such as cancer (Holtmaat, van der Spek, Cuijpers, Leemans, & Verdonck-de Leeuw, 2017), burns (Royse & Badger, 2017), type 2 diabetes (Dirik & Göcek-Yorulmaz, 2018), and myocardial infarction (Rahimi, Heidarzadeh, & Shoaee, 2016).
Tedeschi and Calhoun (2004) developed the Posttraumatic Growth Model, which includes elements of posttraumatic stress, core beliefs disruption, and posttraumatic growth. To date, no studies focusing on posttraumatic growth in mothers who have experienced traumatic childbirth have tested all the components of this model. Therefore, the purpose of this pilot study was to rectify that. If childbirth educators, such as Lamaze instructors, are to assist women in developing posttraumatic growth, they first need to understand the process involved in achieving this growth.
Posttraumatic Growth Model
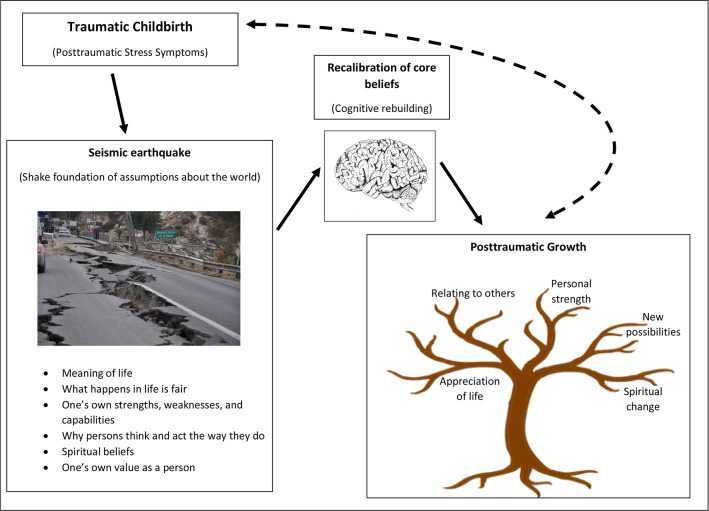
Tedeschi and Calhoun (2004) conceptualized posttraumatic growth as an outcome of the struggle with a traumatic event. In posttraumatic growth, individuals surpass in some parts of their lives what was present before their struggle with the trauma. Not all individuals who experience a traumatic event will also experience posttraumatic growth. In posttraumatic growth, the distress of the trauma does not disappear but coexists with the growth. This growth consists of five dimensions: appreciation of life, relating to others, personal strength, new possibilities, and spiritual change (Tedeschi & Calhoun, 1996). Individuals do not necessarily have to experience positive changes in all five dimensions.
Calhoun and Tedeschi (1998) used the metaphor of an earthquake to illustrate the process of posttraumatic growth. In order for this growth to occur, the person’s traumatic event must be strong enough to successfully “shake the foundations” of the person’s core beliefs and assumptions about the world (p. 216). As in an earthquake, the trauma needs to be seismic in strength in order to shake the person’s world. These assumptions about the world include beliefs about the meaning of life, what happens in life is fair, one’s own strengths, weaknesses, and capabilities, future expectations, why persons think and act the way they do, spiritual beliefs, and one’s own value as an individual.
Just like in the aftermath of an earthquake where physical structures need to be rebuilt, cognitive rebuilding is necessary to achieve posttraumatic growth. Cognitive rebuilding refers to a person giving up certain basic assumptions they held about the world and building new meanings (Tedeschi & Calhoun, 2004). A recalibration of core beliefs is necessary as persons struggle with their traumatic experiences. Tedeschi, Calhoun, and Cann (2007) call this reexamining of core beliefs, rumination. In the early time after a traumatic event, this rumination involves intrusive thoughts. As time passes from when the trauma occurred, however, rumination is less about these intrusive thoughts and more about the person attempting to make sense of their trauma and beginning to rebuild their assumptions about the world. A factor that can play a role in the development of posttraumatic growth is the degree of self-disclosure persons share regarding their emotions and also how their significant others react to this self-disclosure (Calhoun, Cann, & Tedeschi, 2010).
Perinatal Posttraumatic Growth
Six quantitative studies and two qualitative studies were located in the literature in which mothers’ posttraumatic growth was examined. In four of the quantitative studies, samples were used that consisted of women who have given birth but did not necessarily perceive their births to have been traumatic. In Sawyer and Ayers’s (2009) study, 219 mothers who had given birth within the past 36 months completed the Posttraumatic Growth Inventory (PTGI; Tedeschi & Calhoun, 1996) in an electronic survey. Fifty percent of the sample reported moderate levels of posttraumatic growth. The mean PTGI score was 58 for the sample. The PTGI dimension with the highest endorsement was appreciation of life (80%), while spiritual change had the lowest (16%). There was no significant relationship between posttraumatic stress symptoms and posttraumatic growth. Regression analysis revealed that only one variable, age, was a significant predictor of posttraumatic growth. Younger women reported more growth.
The second study was a longitudinal study in the United Kingdom with 125 women who completed the PTGI once during pregnancy and again at 8 weeks postpartum (Sawyer, Ayers, Young, Bradley, & Smith, 2012). Twenty-three percent of the sample perceived their birth as traumatic. A small degree of posttraumatic growth after birth was reported by 48% of the women. The mean PTGI score was 39. The most endorsed dimension of the PTGI was appreciation of life (68%), and spiritual change was the least (22%). A hierarchical multiple regression revealed two significant predictors of posttraumatic growth: higher posttraumatic stress symptoms during pregnancy and cesarean birth.
In the third study, posttraumatic growth was compared with 193 mothers in the United Kingdom and 160 Croatian mothers via an online survey (Sawyer, Nakić Radoš, Ayers, & Burn, 2015). The one criterion to participate and complete the PTGI was that the women had given birth within the last 2 years. A moderate level of growth after childbirth was reported in 44% of the U.K. mothers and 35% of the Croatian mothers. In both the U.K. and Croatian samples, younger maternal age was a significant predictor of posttraumatic growth. Higher posttraumatic stress symptoms were a significant predictor of growth in only the Croatian sample.
The most recent study was conducted in Japan with 117 mothers 1 month after childbirth (Nishi & Usuda, 2017). The short form of the PTGI (Cann et al., 2010a) was used, which contains 10 items scored on a range of 0–5 points per item. The total score can range from 0–50. There are two items in each of the five subscales. The mean short form PTGI score was 27.1. The researchers stated that this mean total score could be viewed as 56.9 in the full PTGI. Regression analysis revealed three variables that were associated with higher PTGI total scores: primiparity, higher resilience, and less fear of childbirth.
Two of the quantitative studies measured posttraumatic growth in women who had experienced pregnancy loss. Women who experienced a miscarriage or stillbirth (N = 328) completed the PTGI and the Core Beliefs Inventory (CBI) in an electronic survey (Krosch & Shakespeare-Finch, 2017). Moderate levels (M = 51.22) of posttraumatic growth were reported. The mean CBI scores were moderately high (M = 29.85). Disruption of core beliefs following a miscarriage or stillbirth was significantly related to higher posttraumatic stress levels (r = .27, p < .001). A significant relationship (r = .29, p < .001) was also found between the PTGI and CBI scores. In the second study of 161 women who experienced pregnancy termination for fetal abnormality, via an online survey, moderate levels of posttraumatic growth using the PTGI (M = 46.6) were reported (Lafarge, Mitchell, & Fox, 2017).
Two qualitative studies have been conducted on posttraumatic growth in women after birth. Black and Sandelowski (2010) interviewed 15 women who had been told during their pregnancy that their fetus had a severe anomaly. One year after giving birth, 12 of the 15 women experienced posttraumatic growth in their lives. The interview data were coded using the five dimensions of Tedeschi and Calhoun (1996) posttraumatic growth model. Relating to others was the dimension that showed the earliest and most long-term change. Beck and Watson (2016) conducted a phenomenological study via the Internet of posttraumatic growth after traumatic childbirth in 15 mothers. Using Colaizzi’s (1978) method of data analysis, four themes emerged that described the essence of mothers’ positive changes in their beliefs or life as a result of their traumatic births: (a) opening oneself up to a new present, (b) achieving a new level of relationship nakedness, (c) fortifying spiritual mindedness, and (d) forging new paths.
To date, none of the research on posttraumatic growth after traumatic childbirth has investigated all the components of Tedeschi and Calhoun’s (2004) posttraumatic growth model: posttraumatic stress, disruption of core beliefs, and posttraumatic growth.
Research Design
This pilot study used a cross-sectional, quantitative design to examine the components of the Posttraumatic Growth Model (Tedeschi & Calhoun, 2004) as they applied to women who perceived they have experienced birth trauma.
Research Questions
What percentage of mothers who perceived their births to be traumatic: (a) experience elevated posttraumatic stress symptom levels, (b) examine their core beliefs, and (c) experience posttraumatic growth?
What are the predictors of posttraumatic growth in women who have experienced traumatic childbirth?
Instruments
Posttraumatic Stress Disorder Symptom Scale-Self Report. The posttraumatic Stress Disorder Symptom Scale-Self Report (PSS-SR; Foa, Riggs, Dancu, & Rothbaum, 1993) is a 17-item Likert scale that consists of three symptom clusters: intrusion (5 items), avoidance (7 items), and arousal (5 items) that are congruent with the PTSD symptom clusters as noted in the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV; American Psychiatric Association, 2000). Participants rate the severity of each symptom over the past 2 weeks using a 4-point scale ranging from 0 = not at all to 3 = very much. Total scores range from 0 to 51. The higher the score, the greater the severity of posttraumatic stress symptoms. A total score of 12 or higher indicates a person is experiencing some posttraumatic stress symptoms. Foa et al. (1993) provided an algorithm for determining if a participant screens positive for meeting the DSM-IV criteria for PTSD. A person must endorse (a rating of 1 or higher) at least one intrusion, 3 avoidance, and 2 arousal symptoms. Reported alpha coefficients by Foa et al. were .91 for the total scale data and .78, .80, and .82 for intrusion, avoidance and arousal subscales, respectively. In this current study, Cronbach’s α for the total PSS-SR data was .92. The subscale alphas were as follows: intrusion (.86), avoidance (.79), and arousal (.91). The PSS-SR has been adapted to make it event specific with its items referring to childbirth (Ayers & Pickering, 2001). This adaptation was used in this electronic survey with mothers who perceived their births to be traumatic.
Core Beliefs Inventory
The CBI is a 9-item 6-point Likert scale that measures the amount that individuals examine their core beliefs and assumptions about the world after experiencing a significant life event (Cann et al., 2010b). The focus of the CBI items is on spiritual and religious beliefs, the nature of human beings, the meaning of life, relationships with other persons, and personal strengths and weaknesses. Responses can range from 0 to 5 with a total score of 0 to 45. The higher the total score, the greater the perceived disruption of core beliefs due to the traumatic event. Cann et al. (2010b) do not recommend any cutoff score but indicate that the mean score can be used to interpret the level of disruption (0 = not at all to 5 = to a very great degree). Cann et al. reported the alpha coefficients ranged from .82 to .87 with college students. In a study with women who experienced pregnancy loss, Krosch and Shakespeare-Finch (2017) reported an alpha coefficient of .85 for the total CBI data. For this current study, the alpha coefficient for the CBI data was .94.
Posttraumatic Growth Inventory
The Posttraumatic Growth Inventory is a 21-item Likert scale that measures the degree of positive changes persons experience after challenging life events (Tedeschi & Calhoun, 1996). This inventory consists of five factors: appreciation of life, relating to others, personal strength, new possibilities, and spiritual change. It uses a 6-point Likert format from 0 = no change to 5 = very great degree. The total score can range from 0 to 105. Tedeschi and Calhoun (1996) do not provide any score category ranges to interpret the total score, however, the mean score can be used (0 = no change to 5 = very great degree). Reported internal consistency reliability for the total PTGI data was .90 and for the subscales .67 to .85.
The reliability of the PTGI data with mothers was assessed by Taubman-Ben-Ari, Findler, and Sharon (2011) in Israel with three samples (N = 150, N = 157, N = 152). Cronbach’s α for the total scale was .90, and for the subscales, .77 (new possibilities), .87 (relating to others), .85 (personal strength), .80 (appreciation of life), and .85 (spiritual change). In studies assessing posttraumatic growth in women after childbirth, reported alpha reliabilities for the PTGI include .93 for the total scale and a range from .67 to .86 for the subscales (Sawyer & Ayers, 2009) and .95 for the total scale and .66 to .84 for the subscales (Sawyer et al., 2012). In women who have experienced pregnancy loss, the reported Cronbach’s coefficient for the total PTGI was .92 (Krosch & Shakespeare-Finch, 2017). For this current study, the alpha coefficient for the total PTGI data was .95. The subscale alphas included relating to others (.86), new possibilities (.91), personal strength (.82), appreciation of life (.66), and spiritual change (.80).
Procedure
Recruitment started after receiving approval from the University’s Institutional Review Board. Participants were obtained through a recruitment notice placed on Trauma and Birth Stress (TABS; www.tabs.org.nz), a charitable trust located in New Zealand, whose mission is to support women who have experienced birth trauma. The second author of this pilot study is the chairperson of TABS who was instrumental in recruiting the sample. A link to our electronic survey was placed on the TABS’ website. There was only one criterion for sample inclusion, that being, women perceived their births to have been traumatic. The return of the completed electronic survey implied informed consent. All data were anonymous. The online survey was open for 11 months.
Data Analysis
IBM SPSS statistics (Version 24.0) were used to analyze the quantitative data obtained from the PSS-SR, CBI, and the PTGI. Descriptive statistics and correlations were used to identify any characteristics of the mothers that correlated with posttraumatic stress, core beliefs, and posttraumatic growth. Effect sizes were interpreted using Huck’s (2011) guidelines for r2 : .01 = small effect size, .09 = medium effect size, and .25 = large effect size. Stepwise multiple regressions were calculated to identify any significant predictors of posttraumatic stress, core beliefs, and posttraumatic growth.
Results
Sample
The Internet sample consisted of 30 mothers who perceived they had experienced a traumatic birth (Table 1). Seven (23%) of the women reported prior trauma, such as sexual assault. The top three most frequently reported birth traumas were emergency cesarean, lack of respect and compassion (what some women termed “obstetric rape”), and the infant needing to go to the Newborn Intensive Care Unit. The mean age of the sample was 35.63 years (standard deviation [SD] = 10.21). The range was 23 to 59 years of age. The mean length of time since their birth trauma was 5.4 years (SD = 7.79 years). The range was 1 month to 24 years. T-tests revealed that none of the following variables (education, country, parity, PTSD diagnosis, or history of prior trauma) differed significantly on the PSS-SR, CBI, and PTGI total scores.
TABLE 1. Demographic and Obstetric Characteristics of the Sample (N = 30).
| Variable | n | % | ||||||
|---|---|---|---|---|---|---|---|---|
| Country | ||||||||
| United States | 10 | 33.3 | ||||||
| New Zealand | 15 | 50.0 | ||||||
| Canada | 3 | 10.0 | ||||||
| Poland | 1 | 3.3 | ||||||
| Romania | 1 | 3.3 | ||||||
| Race | ||||||||
| White, non-Hispanic | 27 | 90.0 | ||||||
| Multiracial | 1 | 3.3 | ||||||
| Other | 2 | 6.7 | ||||||
| Education | ||||||||
| High school | 8 | 30.0 | ||||||
| Associate | 2 | 6.7 | ||||||
| Bachelors | 13 | 43.3 | ||||||
| Masters | 5 | 16.7 | ||||||
| PhD or equivalent | 1 | 3.3 | ||||||
| Marital status | ||||||||
| Single | 1 | 3.3 | ||||||
| Cohabitating | 6 | 20.0 | ||||||
| Married | 22 | 73.3 | ||||||
| Separated | 1 | 3.3 | ||||||
| Prior trauma history | ||||||||
| Yes | 8 | 26.7 | ||||||
| No | 22 | 73.3 | ||||||
| Parity | ||||||||
| Primipara | 19 | 63.3 | ||||||
| Multipara | 11 | 36.7 | ||||||
| Birth type | ||||||||
| Vaginal | 5 | 16.7 | ||||||
| Vaginal with forceps or vaccum extraction | 9 | 30.0 | ||||||
| Cesarean | 16 | 53.3 | ||||||
| Number of traumatic births | ||||||||
| 1 | 26 | 86.7 | ||||||
| 2 | 2 | 6.7 | ||||||
| Missing | 2 | 6.7 | ||||||
| PTSD diagnosis | ||||||||
| Yes | 11 | 36.7 | ||||||
| No | 19 | 63.3 | ||||||
| Currently under care of therapists | ||||||||
| Yes | 4 | 13.3 | ||||||
| No | 26 | 86.7 | ||||||
Note. PTSD = posttraumatic stress disorder.
Posttraumatic Stress
The PSS-SR mean was 1.31, which indicated a small degree of posttraumatic stress. The mean total PSS-SR score for the sample was 22.27 (SD = 12.77). The range of total scores was 1 to 47, with 51 being the highest score possible. When focusing on the subscales, the mean total scores were 5.53 (SD = 4.13) for intrusion, 9.80 (SD = 5.46) for avoidance, and 6.93 (SD = 4.88) for arousal. In this sample 86% of the women endorsed intrusion symptoms, 83% avoidance symptoms, and 73% arousal symptoms. Using Foa et al.’s (1993) algorithm to determine if women met the PTSD criteria according to the DSM-IV, 66.7% of the sample did screen positive for PTSD.
Core Beliefs
The mean total score for the CBI was 27.70 (SD = 12.72). The range of total scores was 1–45, with 45 being the highest score possible. The CBI mean was 3.08, indicating a moderate degree of disruption of core beliefs. The CBI total score was significantly related to the total PSS-SR score (r = .58, p = .001), which was a large effect size (r2 = .34). Also, the CBI total score differed significantly depending on whether the women screened positive for PTSD versus those women who did not (t = 5.29, p < .001). The women who screened positive for PTSD reported a significantly higher amount of disruption in their core beliefs due to their birth trauma.
Posttraumatic Growth
The PTGI mean was 2.07 which reflected a small degree of growth. In this sample, the mean total PTGI score was 43.37 (SD = 25.53) with a range of 6–95. The highest score possible for the inventory is 105. For the five subscales, the mean total scores were as follows: relating to others 14.17 (SD = 8.59), new possibilities 9.33 (SD = 8.15), personal strength 9.10 (SD = 5.86), appreciation of life 8.27 (SD = 3.64), and spiritual change 2.50 (SD = 3.38). The length of time since the traumatic births occurred was significantly related to the total PTGI score (r = .37, p = .05), which indicated a medium effect size (r2 = .14). The longer the time since the traumatic birth happened, the greater the mother’s posttraumatic growth. T-tests revealed a significant difference in the PTGI total score according to the type of birth (t = 2.46, p = .02). Women who gave birth by a cesarean reported significantly higher levels of posttraumatic growth than women who gave birth vaginally (t = 5.29, p < .001).
The correlations between the CBI scores and the PTGI scores just missed significance (r = .34, p = .06). However, when looking at the subscales of the PTGI, three of the five subscales were significantly correlated with the CBI scores. Personal strength was significantly correlated with the CBI total score (r = .37, p < .05), appreciation of life (r = .53, p < .01), and spiritual change (r = .37, p < .05). Both personal strength and spiritual change had medium effect sizes (r2 = .14) and appreciation of life (r2 = .28) had a large effect size.
Stepwise Multiple Regressions
A stepwise multiple regression analysis was performed with the PSS-SR scores as the dependent variable. Three predictor variables were entered into the regression: age, type of birth, and length of time since the traumatic birth. Age was the only significant variable which explained 15% (r = .39, p = .03) of the variance in posttraumatic stress scores with a medium effect size (r2 = .15). Older women were associated with lower posttraumatic stress symptoms.
A second regression analysis was performed this time with the CBI scores as the dependent variable. Entered into the regression were birth type, length of time since the traumatic birth, and the PSS-SR scores. The only significant predictor variable was the posttraumatic stress scores which explained 34% (r = .58, p = .001) of the variance in the CBI scores with a large effect size (r2 = .34).
The third stepwise multiple regression was performed on the PTGI scores as the dependent variable. Four predictor variables were entered into the regression: birth type, length of time since the traumatic birth, PSS-SR and CBI scores. Two variables significantly predicted 38% (R = .62, p = .006) of posttraumatic growth: birth type and the length of time since the birth trauma with a large effect size (r2 = .38). Women who had cesarean births and had a longer time since the birth trauma occurred were associated with higher levels of posttraumatic growth.
Discussion
Birth trauma can be perceived as a psychologically seismic occurrence of a magnitude that can severely shake the foundations of mothers’ assumptive worlds. In this study, the seismic waves from traumatic births had enough power to lead to a small degree of posttraumatic growth in mothers. Mothers in this sample reported a small degree of posttraumatic stress symptoms, a moderate level of disruption of their core beliefs, and a small degree of posttraumatic growth (Figure 1).
Figure 1. Illustration of Tedeschi and Calhoun’s posttraumatic growth model in traumatic childbirth.
Age was the only demographic characteristic that was significantly related to posttraumatic stress symptoms. The older that mothers were, the less posttraumatic stress they reported. Age was not, however, significantly correlated with either the PTGI or CBI scores. In two prior studies, age was found to be significantly related to posttraumatic growth where younger mothers reported more growth (Sawyer & Ayers, 2009; Sawyer et al., 2015). Tedeschi and Calhoun (2004) hypothesize that younger persons might be more amenable to learning and changing, while older persons may be less open to change.
Women who gave birth by cesarean experienced significantly more posttraumatic growth than women who gave birth vaginally. This confirmed earlier findings of Sawyer et al. (2012) where cesarean birth was a significant predictor of posttraumatic growth in mothers. These results supported Tedeschi and Calhoun’s (2004) posttraumatic growth model that purports that in order for this type of growth to occur, the traumatic event needs to be seismic in strength to shake an individual’s core beliefs and challenge fundamental assumptions. The reason for the emergency cesarean births in this current sample was for fetal distress, which could be perceived as more traumatic by the mothers than women giving birth vaginally whose unborn infants were not in distress.
Also supportive of Tedeschi and Calhoun’s (2004) posttraumatic growth model was the finding that mothers’ scores on the PSS-SR were significantly related to their CBI scores. The higher the level of posttraumatic stress symptoms, the greater the amount of disruption in mothers’ core beliefs. The PSS-SR scores explained 34% of the variance in CBI scores. The finding in this study which did not support the posttraumatic growth model was the nonsignificant relationship between the amount of core belief disruption in mothers and the amount of their posttraumatic growth. It just missed significance at p = .06. The two significant predictors of posttraumatic growth, birth type and length of time since the traumatic birth occurred, predicted 38% of the variance. The longer the time from the traumatic birth, the higher the level of posttraumatic growth which supported Tedeschi and Calhoun’s (2004) model in which they proposed that as time passes from when the traumatic event occurred, the intrusive thoughts decrease and become more about the individual making sense of the events and rebuilding their core assumptions.
When comparing the mean total PTGI score for this study with the five prior research studies, in four of the five studies, the PTGI score was higher than the current study. Two of these studies with mothers who had experienced pregnancy loss (Krosch & Shakespeare-Finch, 2017; Lafarge et al., 2017) reported higher PTGI scores, which would be expected. The one study that reported lower PTGI scores was Sawyer et al. (2012), with a community sample.
In both the studies by Sawyer et al. (2012) and Sawyer et al. (2015), appreciation of life was the highest dimension of posttraumatic growth, while spiritual change was the lowest. In this current study, relating to others was the highest dimension reported by the mothers but, like the other studies, spiritual change was the lowest. Relating to others was one of the top two most frequently cited dimensions in Beck and Watson (2016) qualitative study of posttraumatic growth in mothers after birth trauma.
In Krosch and Shakespeare-Finch’s (2017) study that examined the relationship between CBI and PTGI scores, a significant relationship (r = .27, p < .001) was found. Lafarge et al. (2017) also reported a significant relationship between CBI and PTGI scores (r = .29, p < .001). Both of these studies’ samples consisted of women who had experienced pregnancy losses. In this current study, the correlation between these two scales’ total scores just missed significance (p = .06).
Mothers’ posttraumatic stress symptom scores were significantly correlated with their core beliefs scores (r = .58, p < .001). This revealed a large effect size (.34). This finding supported Tedeschi and Calhoun’s (2004) posttraumatic growth model, which proposed that essential to posttraumatic growth is the trauma’s ability to successfully “shake the foundations” of the person’s assumptive world. The higher the posttraumatic stress symptoms, the higher the mothers’ disruption of their core belief scores.
Limitations and Recommendations for Future Research
In consideration of the findings of this pilot study, it is important to address some of its limitations. First, it was a cross-sectional study. We cannot determine causation. The small sample size of 30 mothers is another limitation. The majority of the sample consisted of white well-educated women. In future studies, a more diverse sample would strengthen the generalizability of the findings. Another limitation of the sample was the wide range of time since the traumatic births occurred. In future research, more careful sample criteria related to prior trauma history are needed since this is a reported risk factor for traumatic births. The low Cronbach’s α of one subscale of the PTGI, appreciation of life (r = .66), must be noted. The low reliability coefficient of this subscale was also recognized by the instrument developers (Tedeschi & Calhoun, 1996). This current study does provide beginning pilot data for a future study with a larger sample.
It must be acknowledged that the PSS-SR is based on the DSM-IV (American Psychiatric Association, 2000) criteria for PTSD which focused on the three symptom clusters of intrusion, avoidance, and arousal. This pilot study was initiated prior to the publication of the latest revision of this scale using to the DSM-V criteria (Foa et al., 2016). In the DSM-V (American Psychiatric Association, 2013), there are now four symptoms clusters. The symptom cluster of avoidance was divided into two clusters: avoidance and negative alterations in cognition and mood. Three new symptoms were added that focus on persistent negative beliefs, distorted blame of self or others regarding the trauma, and negative emotional state. Future research should use this DSM-V version of the scale. Another recommendation for future research can include designing mixed methods studies in order to add some qualitative data where women have the opportunity to share their birth stories and explain what they learned from their experiences.
Implications for Practice
In Simpson and Catling’s (2016) literature review of traumatic birth experiences, they identified some risk factors, such as prior mental health disorders or a prior trauma, that are identifiable in the prenatal period. These risk factors can be addressed before birth with the hopes of minimizing a woman experiencing a traumatic birth. Lamaze instructors and other childbirth educators need to be vigilant in identifying mothers who may be struggling with the aftermath of birth trauma. Metaphors women use to help describe their experiences with posttraumatic stress can provide important clues for providers (Beck, 2016). Examples of such metaphors women have used include a ticking time bomb, an invisible wall, a video on constant replay, a mechanical robot, and a dangerous ocean. Mothers may not possess the medical jargon to communicate what they are experiencing and that is where metaphors are helpful.
Decreasing the risk of women experiencing a traumatic birth needs to be a priority for all health-care providers who care for women during the child-bearing cycle. If, however, a mother does experience birth trauma, Lamaze instructors and other childbirth educators are in an ideal position to support these new mothers. Trusting relationships have been built and mothers may be more open to disclosing to their childbirth educators their experiences of a traumatic birth and the emotions they are struggling with. Self-disclosure regarding the emotions that a traumatized person shares and how others react to this self-disclosure play an important role in the development of posttraumatic growth (Calhoun et al., 2010). We can offer mothers hope that some may have positive changes in their lives as a result of struggling with their posttraumatic stress after birth trauma. Childbirth educators must be careful, however, not to give mothers false expectations that posttraumatic growth will occur in all trauma survivors. “Expert companion” is the term that Calhoun and Tedeschi (2013) give to the approach clinicians can use in working with trauma survivors. This approach calls for clinicians to have a sense of humility in order to set the stage for an environment where survivors’ personal exploration can help to promote their posttraumatic growth. While respecting the survivors’ struggles as a result of their traumatic experience, psychiatric and mental health-care professionals need to permit the survivors to explore the possibility of posttraumatic growth.
Biographies
CHERYL TATANO BECK is a distinguished professor in the School of Nursing at the University of Connecticut.
SUE WATSON is the Chairperson of Trauma and Birth Stress, Auckland, New Zealand.
ROBERT K. GABLE is an emeritus professor in the Neag School of Education at the University of Connecticut.
References
- Alcorn, K. L., O’Donovan, A., Patrick, J. C., Creedy, D., & Devilly, G. J. (2010). A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychological Medicine, 40(11), 1849–1859. 10.1017/S0033291709992224 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Ayers, S., & Pickering, A. D. (2001). Do women get post-traumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth, 28(2), 111–118. 10.1046/j.1523-536X.2001.00111.x [DOI] [PubMed] [Google Scholar]
- Beck, C. T. (2006). The anniversary of birth trauma: Failure to rescue. Nursing Research, 55(6), 381–390. [DOI] [PubMed] [Google Scholar]
- Beck, C. T. (2015). Middle range theory of traumatic childbirth. Global Qualitative Nursing Research, 2, 1–13. 10.1177/2333393615575313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, C. T. (2016). Posttraumatic stress disorder after birth: A metaphor analysis. MCN: The American Journal of Maternal Child Nursing, 41(2), 76–83. 10.1097/NMC.0000000000000211 [DOI] [PubMed] [Google Scholar]
- Beck, C. T., & Watson, S. (2008). Impact of birth trauma on breast-feeding: A tale of two pathways. Nursing Research, 57(4), 228–236. 10.1097/01.NNR.0000313494.87282.90 [DOI] [PubMed] [Google Scholar]
- Beck, C. T., & Watson, S. (2010). Subsequent childbirth after a previous traumatic birth. Nursing Research, 59(4), 241–249. 10.1097/NNR.0b013e3181e501fd [DOI] [PubMed] [Google Scholar]
- Beck, C. T., & Watson, S. (2016). Posttraumatic growth following birth trauma: “I was broken. Now I am unbreakable.” MCN: The American Journal of Maternal Child Nursing, 41, 264–271. [DOI] [PubMed] [Google Scholar]
- Black, B., & Sandelowski, M. (2010). Personal growth after severe fetal diagnosis. Western Journal of Nursing Research, 32(8), 1011–1030. 10.1177/0193945910371215 [DOI] [PubMed] [Google Scholar]
- Calhoun, L. G., Cann, A., & Tedeschi, R. G. (2010). The posttraumatic growth model: Sociocultural considerations Weiss, T & Berger, R (Eds.), Posttraumatic growth and culturally competent practice: Lessons learned from around the globe. Hoboken, NJ: Wiley. [Google Scholar]
- Calhoun, L. G., & Tedeschi, R. G. (2013). Posttraumatic growth in clinical practice. New York, NY: Routledge. [Google Scholar]
- Calhoun, L. G., & Tedeschi, R. G. (1998). Posttraumatic growth: Future directions Tedeschi, R. G, Park, C. L., & Calhoun, L. G (Eds.), Posttraumatic growth: Positive change in the aftermath of crisis ( 215–238). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Kilmer, R. P., Gil-Rivas, V., Vishnevsky, T., & Danhauer, S. C. (2010b). The core beliefs inventory: A brief measure of disruption in the assumptive world. Anxiety, Stress & Coping, 23(1), 19–34. 10.1080/10615800802573013 [DOI] [PubMed] [Google Scholar]
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., Vishnevsky, T., Triplett, K. N., & Danhauer, S. C. (2010a). A short form of the Posttraumatic Growth Inventory. Anxiety, Stress & Coping, 23(2), 127–137. 10.1080/10615800903094273 [DOI] [PubMed] [Google Scholar]
- Colaizzi’s, P. (1978). Psychological research as the phenomenologist views it Valle, R & King, M (Eds.), Existential phenomenological alternatives for psychology ( 48–71). New York, NY: Oxford University Press. [Google Scholar]
- Dirik, G., & Göcek-Yorulmaz, E. (2018). Positive sides of the disease: Posttraumatic growth in adults with Type 2 diabetes. Behavioral Medicine, 44(1), 1–10. 10.1080/08964289.2016.1173635 [DOI] [PubMed] [Google Scholar]
- Foa, E. B., McLean, C. P., Zang, Y., Zhong, J., Rauch, S., Porter, K., … Kauffman, B. Y. (2016). Psychometric properties of the Posttraumatic Stress Disorder Symptom Scale Interview for DSM-5 (PSSI-5). Psychological Assessment, 28(10), 1159–1165. 10.1037/pas0000259 [DOI] [PubMed] [Google Scholar]
- Foa, E. B., Riggs, D. S., Dancu, C. V., & Rothbaum, B. O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6(4), 459–473. 10.1002/jts.2490060405 [DOI] [Google Scholar]
- Gökçe İsbİr, G., İncİ, F., Bektaş, M., Dikmen Yıldız, P., & Ayers, S, Gökce, I. G, Incl, F., Bektas, M., Yildiz, D. P. (2016). Risk factors associated with post-traumatic stress symptoms following childbirth in Turkey. Midwifery, 41, 96–103. 10.1016/j.midw.2016.07.016 [DOI] [PubMed] [Google Scholar]
- Holtmaat, K., van der Spek, N., Cuijpers, P., Leemans, C. R., & Verdonck-de Leeuw, I. M. (2017). Posttraumatic growth among head and neck cancer survivors with psychological distress. Psycho-Oncology, 26(1), 96–101. 10.1002/pon.4106 [DOI] [PubMed] [Google Scholar]
- Huck’s, S. W. (2011). Reading statistics and research. Boston, MA: Allyn and Bacon. [Google Scholar]
- Krosch, D. J., & Shakespeare-Finch, J. (2017). Grief, traumatic stress, and posttraumatic growth in women who have experienced pregnancy loss. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 425–433. 10.1037/tra0000183 [DOI] [PubMed] [Google Scholar]
- Lafarge, C., Mitchell, K., & Fox, P. (2017). Posttraumatic growth following pregnancy termination for fetal abnormality: The predictive role of coping strategies and perinatal grief. Anxiety, Stress, & Coping, 30(5), 536–550. 10.1080/10615806.2016.1278433 [DOI] [PubMed] [Google Scholar]
- LoGiudice, J. A. (2016). A systematic literature review of the childbearing cycle as experienced by survivors of sexual abuse. Nursing for Women’s Health, 20(6), 582–594. 10.1016/j.nwh.2016.10.008 [DOI] [PubMed] [Google Scholar]
- Nishi, D., & Usuda, K. (2017). Psychological growth after childbirth: An exploratory prospective study. Journal of Psychosomatic Obstetrics & Gynecology, 38(2), 87–93. 10.1080/0167482X.2016.1233170 [DOI] [PubMed] [Google Scholar]
- Rahimi, R., Heidarzadeh, M., & Shoaee, R. (2016). The relationship between posttraumatic growth and social support in patients with myocardial infarction. Canadian Journal of Cardiovascular Nursing, 26(2), 19–24. [PubMed] [Google Scholar]
- Royse, D., & Badger, K. (2017). Near-death experiences, posttraumatic growth, and life satisfaction among burn survivors. Social Work in Health Care, 56(3), 155–168. 10.1080/00981389.2016.1265627 [DOI] [PubMed] [Google Scholar]
- Sawyer, A., & Ayers, S. (2009). Post-traumatic growth in women after childbirth. Psychology & Health, 24(4), 457–471. 10.1080/08870440701864520 [DOI] [PubMed] [Google Scholar]
- Sawyer, A., Ayers, S., Young, D., Bradley, R., & Smith, H. (2012). Posttraumatic growth after childbirth: A prospective study. Psychology & Health, 27(3), 362–377. 10.1080/08870446.2011.578745 [DOI] [PubMed] [Google Scholar]
- Sawyer, A., Nakić Radoš, S., Ayers, S., & Burn, E. (2015). Personal growth in UK and Croatian women following childbirth: A preliminary study. Journal of Reproductive and Infant Psychology, 33(3), 294–307. 10.1080/02646838.2014.981801 [DOI] [Google Scholar]
- Simpson, M., & Catling’s, C. (2016). Understanding psychological traumatic birth experiences: A literature review. Women and Birth, 29(3), 203–207. 10.1016/j.wombi.2015.10.009 [DOI] [PubMed] [Google Scholar]
- Takegata, M., Haruna, M., Matsuzaki, M., Shiraishi, M., Okano, T., & Severinsson, E. (2017). Aetiological relationships between factors associated with postnatal traumatic symptoms among Japanese primiparas and multiparas: A longitudinal study. Midwifery, 44, 14–23. 10.1016/j.midw.2016.10.008 [DOI] [PubMed] [Google Scholar]
- Taubman-Ben-Ari, O., Findler, L., & Sharon, N. (2011). Personal growth in mothers: Examination of the suitability of the posttraumatic growth inventory as a measurement tool. Women & Health, 51(6), 604–622. 10.1080/03630242.2011.614324 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. 10.1002/jts.2490090305 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun’s, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. 10.1207/s15327965pli1501_01 [DOI] [Google Scholar]
- Tedeschi, R. G., Calhoun, L. G., & Cann, A. (2007). Evaluating resource gain: Understanding and misunderstanding posttraumatic growth. Applied Psychology, 56(3), 396–406. 10.1111/j.1464-0597.2007.00299.x [DOI] [Google Scholar]
- Thomson, G., & Downe, S. (2016). Emotions and support needs following a distressing birth: Scoping study with pregnant multigravida women in North-West England. Midwifery, 40, 32–39. 10.1016/j.midw.2016.06.010 [DOI] [PubMed] [Google Scholar]
- Yildiz, P. D., Ayers, S., & Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders, 208, 634–645. 10.1016/j.jad.2016.10.009 [DOI] [PubMed] [Google Scholar]