Abstract
Objective: Treatment with levothyroxine in primary hypothyroid patients does not always provide complete regression of associated symptoms despite normalised TSH levels. Several sources report ratios of triiodothyronine (T3) to thyroxine (T4) are diminished in hypothyroid patients following a daily levothyroxine regimen. It is known that thyroid-stimulating hormone (TSH) increases de-iodination of T4 to T3. We hypothesise that a raise in TSH levels caused by a temporary withdrawal of oral levothyroxine will be followed by an increased conversion of T4 to T3. Methods: Thirteen patients treated with monotherapy of levothyroxine were included in our pilot study. Treatment was temporarily discontinued for one week in which TSH, free T3 (fT3) and free T4 (fT4) were monitored. TSH and fT3 to fT4 ratios were compared with baseline values. Results: Statistically significant elevations in TSH and fT3 plasma levels relative to fT4 were demonstrated in all patients after withdrawal of levothyroxine. Conclusion: Both TSH and fT3 to fT4 ratios rose following temporary discontinuation of levothyroxine. The effect on symptoms and quality of life is not evaluated in this pilot study. Our results warrant further investigation into whether or not longer dosing intervals would demonstrate commensurate hormone elevations that better reflects the hormonal ratios in healthy subjects and if this also has an effect on quality of life scores.
Keywords: Hypothyroidism, chronic autoimmune thyroiditis, levothyroxine, monotherapy, combination therapy, T3/T4-ratio in plasma
Hypothyroidism is a ubiquitous condition. According to the National Board of Health and Welfare, thyroid-hormone replacement was prescribed to approximately 370,000 individuals in Sweden during 2010. Eighty-three percent were women, representing more than 6 % of the female population.1 Autoimmune thyroiditis is the most predominant cause, but it may also be a consequence of previous radioiodine therapy or thyroidectomy. Hoarse voice, dry skin and muscle cramps are common symptoms. Intensified fatigue, coldness, tendency to constipation or depressive symptoms will often force the patient to a physician. An increased thyroid-stimulating hormone (TSH) – indicating a primary hypothyroid insufficiency – may contribute to the diagnosis of hypothyroidism. However, a weak association is reported between a higher TSH and a number of symptoms.2
A hypothyroid patient is commonly treated with levothyroxine and the dose adjusted until TSH is normalised.3 Despite treatment resulting in normalised serum TSH Saravanan et al. have reported that patients show a permanent impairment in psychological wellbeing compared with healthy subjects.4 A coupling to the lower triiodothyronine (T3) to thyroxine (T4) ratio noted in levothyroxine-treated patients compared with healthy subjects5–8 has been proposed to be a contributing cause. Thus, combined T3 and T4 treatment have been tried to improve patient’s wellbeing. However, a recent meta-analysis of 1,200 patients demonstrated ambiguous results when searching for clear correlation.9
Another study using higher T3 supplementation supported the notion that an increased T3 level may be associated with a better wellbeing.10 The conversion from T4 to T3 is regulated by deiodinase and the activity is elevated in the hypothyroid state as supported by in vitro studies in which thyroid cells incubated with TSH demonstrated increased deiodinase and messenger RNA (mRNA) activity.11,12
Our study’s aim was to determine if withdrawal of oral levothyroxine would elevate TSH and free T3 (fT3) to free T4 (fT4) ratios due to an increased conversion of fT4 to fT3. Bearing in mind the limited number of patients studied it was not intended to evaluate changes in symptoms.
Materials and Methods
Patients with primary hypothyroidism, 18–70 years of age, regularly controlled at our out-patient clinic, the Medical Department at Halland County Hospital, Sweden, were registered. The 71 patients who had treatment with levothyroxine alone without dose adjustments during the last three months, with normalised fT4 levels and normal or subnormal TSH were sent a written invitation. Patients with a symptomatic cardiac disease undergoing treatment with drugs that might affect the levels of thyroid hormone in the last three months were excluded (iodine-containing X-ray contrast and antidepressants). In addition, pregnant and nursing women were also excluded. A total of 13 patients, after written consent was received, were included in our study.
During basal treatment TSH, fT3 and fT4 plasma levels were monitored on two consecutive days and a mean value was calculated (day 0). After obtaining baseline values, daily oral treatment was discontinued. Thereafter, plasma hormone level sampling was repeated after three, six and seven days before re-initiating ordinary treatment. The samples were obtained in fasting state at 8 am and analysed at the Department of Clinical Chemistry of Halland County Hospital, Halmstad. The assay used was an electro-chemical-luminescence immunoassay manufactured by Roche Diagnostics GmbH (Mannheim, Germany).13 The reference range for TSH was 0.40–4.00 mU/l, the inter- and intra-assay coefficient of variation (CV) were 3.8 and 9 %. The reference range for fT3, 3.1–7.0 pmol/l, inter- and intra-assay CV were 5.5 and 7.4 %, respectively. The reference range for fT4, 11–22 pmol/l, inter-and intra-assay CV were 5.2 and 7.4%, respectively.
The study was approved by the Regional Ethical Review Board in Lund 2011-02-17 DNR 2011/66. Consent was received from each patient after full explanation of the purpose and nature of all procedures used.
Statistical methods: T3/T4 and TSH-levels across the observation points (baseline, days 3, 6 and 7) were compared using Friedman’s test.14
Moreover, paired levels between adjacent observation points (baseline versus day three, day three versus day six and day six versus day seven) were compared by Wilcoxon’s signed rank test; and the p-values reported were adjusted for multiple comparisons by the Bonferroni method.14 The methods used to calculate p-values were exact, rather than asymptotic.
Results
Altogether 13 patients, of whom one was male, were included. The average age was 43 years (28–60) and the mean dose levothyroxin was 109 µg (75–162.5). Two hormone samples were excluded, one because the sample were taken at the wrong time, another dropped out after three days due to intolerable fatigue.
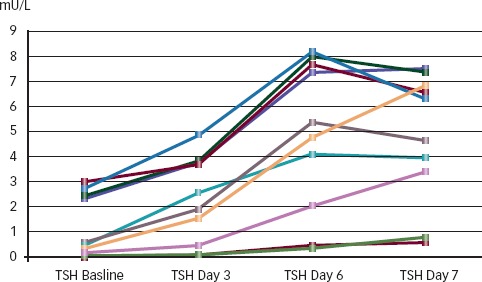
Individual fT3/fT4 and TSH-levels are shown in Figures 1 and 2, respectively. A statistically significant systematic change in fT3/fT4-levels (p<0.001) was observed. Median fT3/fT4 increased from 0.23 (0.17–0.32) to 0.28 (0.22–0.42) pmol/l. Similarly, there was a rise in TSH-levels (p<0.001) across the observation points. Median TSH increased from 0.6 (0.03–3.04) to 4.64 (0.58-7.52) mU/l during the study. Additionally, a statistically significant increase in T3/T4-levels was seen between days 3 and 6 (p=0.05). TSH-levels increased significantly between baseline and day 3 (p=0.004) as well as between days 3 and 6 (p=0.004).
Figure 1: Study Subjects’ fT3 to fT4 Ratios.
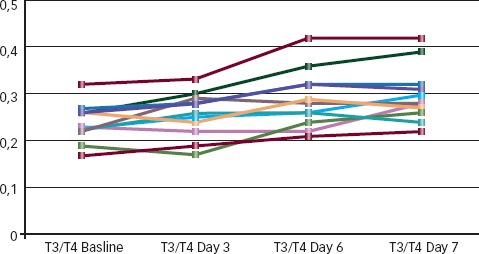
Figure 2: Study Subjects’ Thyroid-stimulating Hormone Levels.
Discussion
In the treatment of hypothyroidism seen in clinical practice, levothyroxine is given in monotherapy and adequate dosing is considered when plasma TSH levels normalise. Despite this, many patients have recalcitrant symptoms of hypothyroidism. Several studies have found that the ratio of T3/T4 differ and are consistently lower with levothyroxine substitution compared with healthy subjects.5–8 The ratio of those who received replacement therapy with the intention to normalise or even to attain subnormal levels of serum TSH was studied. The ratio of fT3/fT4 was lowest in the group with subnormal TSH, although the difference was not significant.8
It is known that TSH is important for the conversion to fT3 although the clinical significance of this is not completely understood. In the present study we demonstrated that temporary discontinuation of oral levothyroxine results in increased plasma TSH levels and fT3 to fT4 ratios. Within three days after discontinuation of levothyroxine, a significant trend was noted. Our results suggest that there is a direct correlation between TSH levels and the conversion of fT4 to fT3. Since treatment of hypothyroidism lowers TSH, it may be an explanation for why patients with replacement therapy have a fT3/fT4 ratio that is lower than healthy controls.
As some patients have remaining symptoms and relatively lower levels of T3, levothyroxine treatment in monotherapy has frequently been questioned. Investigations mimicking healthy subjects with T4 and T3 in combination have been tested in several studies but have produced ambiguous results. A meta-analysis including 11 studies and 1,200 patients found no advantage of T3 and T4 in combination regarding terms of quality of life (QOL) and residual hypothyroidism symptoms.9 However, in a more recent study by Nygaard et al., which differs from previous studies in that a higher dose of T3 in combination with T4 was given, benefits of combined therapy in terms of QOL, depression and anxiety were shown. The T3/T4-ratio in that study was even higher than in healthy controls.10 This indicates that it may be relevant to raise the levels of T3.
Thus far, only combination therapies using T4 and T3 have been attempted. If a treatment could provide levothyroxine in adequate quantities without a simultaneous downregulation of TSH levels, it may be possible to raise that ratio to better reflect the hormonal patterns of healthy subjects. Hypothetically, an oral replacement regimen scheduled every other or every third day may be beneficial.
Our results justify further and more extensive studies concerning such regimens. Hopefully, it would also provide fewer of the side effects that occur with oral T3. In summary, this study showed that short-term withdrawal of levothyroxine was associated with higher plasma TSH levels and an increased fT3 to fT4 ratio, which more closely resembled ones found in healthy subjects. The study was too small to make measurements on symptoms and quality of lives scores.
Acknowledgments
The authors thank Mr Tom Lundahl of the Department of Clinical Chemistry, Halland County Hospital who carried out the biochemical analysis. Professor Ulf Strömberg and Mr Anders Holmén of the Department of Clinical Research Center, Halland County Hospital, who performed the statistical analysis. We also wish to thank Dr Max Berry, Department of Vascular and Interventional Radiology, University of Alabama, Birmingham for critical reading and valuable feedback on the manuscript.
References
- 1.Leimanis A., Lndquist P., Schiöler H.. Pharmaceuticals – statistics for 2010. The National Board of Health and Welfare. 2011 Mar 15th; published. (available at http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18278/2011-3-30.pdf)
- 2.Canaris G. J., Steiner J. F., Ridgway E. C.. Do traditional symptoms of hypothyroidism correlate with biochemical disease? J Gen Intern Med. 1997;12(9):544–50. doi: 10.1046/j.1525-1497.1997.07109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baskin H. J., Cobin R. H., Duick D. S.. et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002;8(6):457–69. [PubMed] [Google Scholar]
- 4.Saravanan P., Chau W. F., Roberts N.. et al. Psychological well-being in patients on ‘adequate’ doses of l-thyroxine: results of a large, controlled community-based questionnaire study. Clin Endocrinol (Oxf) 2002;57(5):577–85. doi: 10.1046/j.1365-2265.2002.01654.x. [DOI] [PubMed] [Google Scholar]
- 5.Sesmilo G., Simo O., Choque L.. et al. Serum free triiodothyronine (T3) to free thyroxine (T4) ratio in treated central hypothyroidism compared with primary hypothyroidism and euthyroidism. Endocrinol Nutr. 2011;58(1):9–15. doi: 10.1016/j.endonu.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Woeber K. A.. Levothyroxine therapy and serum free thyroxine and free triiodothyronine concentrations. J Endocrinol Invest. 2002;25(2):106–9. doi: 10.1007/BF03343972. [DOI] [PubMed] [Google Scholar]
- 7.Jonklaas J., Davidson B., Bhagat S., Soldin S. J.. Triiodothyronine levels in athyreotic individuals during levothyroxine therapy. JAMA. 2008;299(7):769–77. doi: 10.1001/jama.299.7.769. [DOI] [PubMed] [Google Scholar]
- 8.Mortoglou A., Candiloros H.. The serum triiodothyronine to thyroxine (T3/T4) ratio in various thyroid disorders and after Levothyroxine replacement therapy. Hormones (Athens) 2004;3(2):120–26. doi: 10.14310/horm.2002.11120. [DOI] [PubMed] [Google Scholar]
- 9.Grozinsky-Glasberg S., Fraser A., Nahshoni E.. et al. Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2006;91(7):2592–9. doi: 10.1210/jc.2006-0448. [DOI] [PubMed] [Google Scholar]
- 10.Nygaard B., Jensen E. W., Kvetny J.. et al. Effect of combination therapy with thyroxine (T4) and 3,5,3’-triiodothyronine versus T4 monotherapy in patients with hypothyroidism, a double-blind, randomised cross-over study. Eur J Endocrinol. 2009;16(16):895–902. doi: 10.1530/EJE-09-0542. [DOI] [PubMed] [Google Scholar]
- 11.Imai Y., Toyoda N., Maeda A.. et al. Type 2 iodothyronine deiodinase expression is upregulated by the protein kinase A-dependent pathway and is downregulated by the protein kinase C-dependent pathway in cultured human thyroid cells. Thyroid. 2001;11(10):899–907. doi: 10.1089/105072501753210957. [DOI] [PubMed] [Google Scholar]
- 12.Borges M., Ingbar S. H., Silva J. E.. Iodothyronine deiodinase activities in FRTL5 cells: predominance of type I 5’-deiodinase. Endocrinology. 1990;126(6):3059–68. doi: 10.1210/endo-126-6-3059. [DOI] [PubMed] [Google Scholar]
- 13.Ellis S., Ekins R.. The radioimmunoassay of the free (diffusible) T3 and T4 concentrations in serum. J Endocrinol. 1973;59(2):43. [PubMed] [Google Scholar]
- 14.Altman D. G. Practical statistics for medical research. London: Chapman and Hall; 1991. 611 [Google Scholar]


