Abstract
This study evaluated between-session reliability of opto-electronic motion capture to measure trunk posture and three-dimensional ranges of motion (ROM). Nineteen healthy participants aged 24 to 74 years underwent spine curvature, pelvic tilt and trunk ROM measurements on two separate occasions. Rigid four-marker clusters were attached to the skin overlying seven spinous processes, plus single markers on pelvis landmarks. Rigid body rotations of spine marker clusters were calculated to determine neutral posture and ROM in flexion, extension, total lateral bending (left-right) and total axial rotation (left-right). Segmental spine ROM values were in line with previous reports using opto-electronic motion capture. Intraclass correlation coefficients (ICC) and standard error of measurement (SEM) were calculated as measures of between-session reliability and measurement error, respectively. Retroreflective markers showed fair to excellent between-session reliability to measure thoracic kyphosis, lumbar lordosis, and pelvic tilt (ICC= 0.82, 0.63, and 0.54, respectively). Thoracic and lumbar segments showed highest reliabilities in total axial rotation (ICC=0.78) and flexion-extension (ICC= 0.77–0.79) ROM, respectively. Pelvic segment showed highest ICC values in flexion (ICC=0.78) and total axial rotation (ICC=0.81) trials. Furthermore, it was estimated that four or fewer repeated trials would provide good reliability for key ROM outcomes, including lumbar flexion, thoracic and lumbar lateral bending, and thoracic axial rotation. This demonstration of reliability is a necessary precursor to quantifying spine kinematics in clinical studies, including assessing changes due to clinical treatment or disease progression.
Keywords: trunk, kinematics, motion analysis, repeatability, spine curvature
1. Introduction
Spinal disorders remain common and costly complaints in clinical practice (Martin et al., 2008). Various disorders, including back pain, developmental disorders, vertebral fracture, and spinal stenosis, impact trunk posture and kinematics (Christe et al., 2017; Chun et al., 2017; Kuwahara et al., 2016; Schmid et al., 2016). Therefore, objective evaluation of trunk posture and motion can help in assessing the functional impact of spinal disorders (e.g. diagnosis of segmental instability, assessment of spine mobility), and in the development and evaluation of evidencebased treatments for spinal disorders (e.g. surgical planning, tracking rehabilitation progress). Opto-electronic motion capture systems have been used to measure trunk posture and motion (Hidalgo et al., 2012; Ignasiak et al., 2017; Marich et al., 2017; Nairn et al., 2013; Preuss and Popovic, 2010; Rast et al., 2016; Schmid et al., 2016), but there is no preferred or standardized method. Establishing motion capture reliability in assessing three-dimensional spine position would facilitate its use in clinical studies and clinical trials. A few studies have reported between-session reliability of motion capture in measuring trunk posture (Dunk et al., 2004; Dunk et al., 2005; Muyor et al., 2017) and range of motion (ROM) (Hidalgo et al., 2012; Montgomery et al., 2011; Rast et al., 2016). However, none of these utilize marker clusters applied to the spine, which are needed for appropriate assessment of three-dimensional motion including evaluation of non-sagittal and coupled motions of the spine. Furthermore, only one study has examined within-session reliability of motion with marker clusters on the spine (Schinkel-Ivy et al., 2015). Therefore, the aim of this study was to measure thoracic kyphosis (TK), lumbar lordosis (LL), and pelvic tilt (PT), as well as three-dimensional spine flexion, extension, lateral bending, and axial rotation ROMs, with three-dimensional marker clusters on the spine, and to determine the between-session reliability of these measurements.
2. Methods
2.1. Participants.
Nineteen healthy (8 female) volunteers participated in this study. The mean±SD (range) age, height, weight, and BMI of the participants were 47±17 (24–74) years, 172±7 (162–185) cm, 71.4±13.9 (44.7–98.1) kg, and 24.0±3.3 (17.0–31.0) kg/m2, respectively. Individuals with recent back pain, history of spinal surgery, traumatic fracture, thoracic deformity, or conditions that affect balance, movement, or ability to stand were excluded. This study was approved by the Institutional Review Board of Beth Israel Deaconess Medical Center, and all participants provided written informed consent before participation.
2.2. Procedure
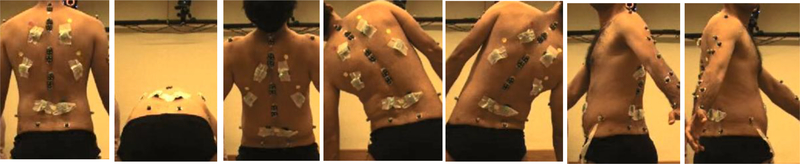
Each participant underwent the same set of measurements on two separate occasions, an average of 7 days apart (range 2–14 days). In each session, before marker placement, spine curvature and pelvic tilt were measured with the flexicurve and Palpation Meter, respectively (see Supplement 1 for details and related results). Then anatomical landmarks were found for marker placement, but no marks were made on the skin (e.g. with grease pencil or marker) as they might have affected placement in the second session. Rigid clusters with four markers each were attached to the skin overlying the T1, T4, T5, T8, T9, T12 and L1 spinous processes using double-adhesive tape. Pelvic markers were placed on the posterior (PSIS) and anterior (ASIS) superior iliac spines and iliac crests. An additional 69 single markers were placed on C7, head, sternum and clavicles, and extremities. Marker data was collected with a 10-camera motion analysis system (Vicon Motion Systems, Oxford, UK) while the participant stood in the middle of the room with feet shoulder-width apart. Marker positions were first captured in the neutral upright standing posture (5 sec). Next, participants were instructed to move their trunk toward full flexion, extension, right and left lateral bending, and right and left axial rotation as smoothly as possible, and hold each position for 5 seconds while data was collected (Figure 1). The same protocol was followed and all participants received consistent instructions in both sessions.
Figure 1.
Posterior views of a subject performing range of motion trials, with spine marker clusters visible. From left to right: neutral posture, full flexion, extension, left lateral bending, right lateral bending, left axial rotation, right axial rotation trials.
2.3. Data reduction, processing, and analysis
Marker positions were averaged over one second from each trial with minimal movement and/or noise in the marker data (or the first one second if no movement or noise was seen). A custom MATLAB (The Mathworks, Inc., Natick, MA, USA) program was used to evaluate 3D orientations. A local coordinate system was created for each spinal marker cluster and the pelvis with x positive to the right. In the spine y and z were normal and tangent to the neutral spine curvature, respectively. In the pelvis y and z were parallel and perpendicular to the plane of the ASIS and PSIS markers, respectively. An Euler angle sequence of x (flexion-extension), y (lateral bending), z (axial rotation) was used to calculate segment orientation and relative orientations between segments, following previous studies (Cotter et al., 2014; Preuss and Popovic, 2010). The relative rotations between clusters in the neutral position were measured for thoracic kyphosis (T1-L1) and lumbar lordosis (L1 – Sacrum), and the orientation of the pelvis for pelvic tilt. Similarly, the relative rotations in ROM trials were calculated to determine ROM outcomes. ROM was defined as the difference in angle for a spine segment (or the pelvis) between neutral posture and the trial. Total ROM was defined as the largest magnitude of angular motion between neutral, flexion, and extension trials (for flexion – extension), and between neutral, left, and right trials (for lateral bending and axial rotation). Circle fitting (Schmid et al., 2016) and polynomial fitting (Ignasiak et al., 2017) approaches were also applied to estimate sagittal plane angles from marker data, with details and results provided in Supplement 2.
2.4. Statistical analysis:
Primary outcomes were magnitude and reliability of thoracic (T1-L1), lumbar (L1 – Sacrum), and pelvic neutral posture and ROMs. Specifically, the primary outcomes for flexion and extension trials were flexion-extension angles. Since lateral bending and axial rotation include significant coupling with other motions, total ROMs of both primary and coupled motions were examined. Secondary outcomes, including ROMs for left and right ROMs separately and for thoracic sub-segments, are presented in Supplement 3. Outcomes were checked for normality by Shapiro-Wilk tests.
Reliability of each outcome was examined using intraclass correlation coefficients (ICC), and classified as poor (ICC <0.4), fair to good (ICC between 0.4 and 0.75) or excellent (ICC >0.75) (Shrout and Fleiss, 1979). Standard error of measurement (SEM) as a parameter of absolute reliability indicates magnitude of error and within-subject variability across repeated trials and was calculated as:
| (1) |
Reliability can be improved by averaging repeated trials, which provides a better estimate of the true measure. Given the ICC for an individual trial, ICC(1), the ICC for m repeated trials can be estimated using the Spearman-Brown formula:
| (2) |
Thus, using Equations 1 and 2, the required number of trials, m, was calculated for each outcome measure to meet the criteria ICC(m)≥0.80 and SEM%<25% as proposed by Schinkel-Ivy et al. (2015). Analyses were performed with Stata/IC 13.1 (StataCorp LP, College Station, TX, USA).
3. Results
About 13% of primary outcome variables had significant Shapiro-Wilk tests (p < 0.05), more than would be expected by chance, suggesting some outcomes may not be normally distributed. Thus, both mean (SD) and median (IQR) are reported as descriptive statistics. In the neutral posture mean TK, LL, and PT were 42.4°, 17.8°, and 4.6°, respectively (Table 1). Lumbar and pelvic segments combined to produce the majority of flexion and extension ROM (Table 1). The thoracic segment accounted for about half of lateral bending ROM, with the rest split between lumbar and pelvic motion (Table 2). Thoracic and pelvic segments combined produced the majority of axial rotation ROM (Table 3). The ICC values ranged from 0.54 to 0.82 for trunk posture, 0.56 to 0.78 for flexion ROM, 0.69 to 0.79 for extension ROM, 0.56 to 0.71 for lateral bending ROM and 0.51 to 0.81 for axial rotation ROM (Table 1–3). Reliability of the trunk segments for coupled motions during lateral bending and axial rotation ranged from poor to good (Tables 2 and 3). The SEM values of the trunk segments in all ROM trials showed a varied range from 1.6° to 11.5° (Tables 1–3).
Table 1.
Mean (SD) and median (IQR) of neutral postural measures, flexion ROM and extension ROM (in degrees), between-session ICCs (95% CI), and thoracic, lumbar and pelvic segments. Negative angles indicate kyphosis, flexion, anterior tilt or anterior pelvic rotation, positive indicate lordosis, extension, posterior tilt or posterior rotation. The number of trials, m, required to meet the criteria ICC(m)≥0.80 and SEM%<25% are also reported. Bold ICC values are significant (p<0.05).
| Measurement | Mean (SD) | Median (IQR) | ICC (95%CI) | SEM | # Trials |
|---|---|---|---|---|---|
| Neutral Posture | |||||
| Thoracic kyphosis | −42.4 (10.9) | −43.5 (17.5) | 0.82 (0.59–0.93) | 4.6 | 1 |
| Lumbar lordosis | 17.8 (7.9) | 17.6 (11.4) | 0.63 (0.26–0.84) | 4.8 | 3 |
| Pelvic tilt | −4.6 (5.6) | −3.6 (7.4) | 0.54 (0.12–0.79) | 3.8 | >10 |
| Flexion | |||||
| Thoracic | −7.1 (11.8) | −5.9 (12.6) | 0.56 (0.17–0.80) | 7.8 | >10 |
| Lumbar | −47.4 (15.6) | −46.3 (22.5) | 0.77 (0.50–0.91) | 7.5 | 2 |
| Pelvic | −51.8 (15.1) | −52.8 (21.4) | 0.78 (0.51–0.91) | 7.1 | 2 |
| Extension | |||||
| Thoracic | 9.5 (14.2) | 8.9 (11.8) | 0.78 (0.48–0.92) | 6.7 | 10 |
| Lumbar | 10.9 (10.9) | 8.1 (5.8) | 0.79 (0.50–0.92) | 5.0 | 4 |
| Pelvic | 12.5 (6.1) | 12.6 (6.4) | 0.69 (0.35–0.87) | 3.4 | 2 |
IQR; InterQuartile Range, ICC: Intraclass Correlation Coefficient; SEM: Standard Error of Measurement (in degrees)
Table 2.
Mean (SD) and median (IQR) of the ranges of motion (in degrees), between session ICCs (95% CI), and SEM for the trunk segments in axial rotation tests. Results are reported for total ranges of motion (left-neutral-right) in primary and coupled directions of motion. The number of trials, m, required to meet the criteria ICC(m)≥0.80 and SEM%<25% are also reported. Bold ICC values are significant (p<0.05).
| Measurement | Mean (SD) | Median (IQR) | ICC (95%CI) | SEM | # Trials |
|---|---|---|---|---|---|
| Thoracic | |||||
| Lateral Bending | 56.2 (16.3) | 56.7 (21.9) | 0.56 (0.17–0.80) | 10.8 | 4 |
| Flexion-Extension (coupled) | 12.0 (7.5) | 10.4 (9.7) | 0.65 (0.29–0.84) | 4.4 | 3 |
| Axial Rotation (coupled) | 28.4 (14.4) | 28.0 (21.6) | 0.60 (0.22–0.82) | 9.1 | 3 |
| Lumbar | |||||
| Lateral Bending | 28.6 (10.9) | 29.2 (18.1) | 0.70 (0.37–0.87) | 6.0 | 2 |
| Flexion-Extension (coupled) | 12.0 (5.7) | 12.6 (6.9) | 0.04 (−0.44–0.48) | 5.6 | >10 |
| Axial Rotation (coupled) | 10.9 (7.9) | 8.6 (9.5) | 0.22 (−0.27–0.61) | 7.0 | >10 |
| Pelvic | |||||
| Lateral Bending | 26.5 (8.8) | 26.5 (11.3) | 0.71 (0.39–0.87) | 4.7 | 2 |
| Flexion-Extension (coupled) | 6.5 (4.9) | 4.8 (6) | 0.48 (0.03–0.75) | 3.5 | 9 |
| Axial Rotation (coupled) | 15.5 (9.3) | 15.8 (13.8) | 0.27 (−0.22–0.64) | 7.9 | >10 |
IQR; InterQuartile Range, ICC; Intraclass Correlation Coefficient, SEM; Standard Error of Measurement (in degrees)
Table 3.
Mean (SD) and median (IQR) of the ranges of motion (in degrees), between session ICCs (95% CI), and SEM for the trunk segments in axial rotation tests. Results are reported for total ranges of motion (left-neutral-right) in primary and coupled directions of motion. The number of trials, m, required to meet the criteria ICC(m)≥0.80 and SEM%<25% are also reported. Bold ICC values are significant (p<0.05).
| Measurement | Mean (SD) | Median (IQR) | ICC (95%CI) | SEM | # Trials |
|---|---|---|---|---|---|
| Thoracic | |||||
| Axial Rotation | 108 (18.3) | 103.5 (24.5) | 0.78 (0.50–0.91) | 8.6 | 2 |
| Flexion-Extension (coupled) | 40.9 (17) | 40.7 (20.8) | 0.75 (0.46–0.89) | 8.5 | 2 |
| Lateral Bending (coupled) | 23.8 (15.2) | 19.2 (18.9) | 0.46 (0.02–0.75) | 11.2 | 7 |
| Lumbar | |||||
| Axial Rotation | 21.2 (13.4) | 20.4 (18.1) | 0.51 (0.05–0.78) | 9.4 | 6 |
| Flexion-Extension (coupled) | 14.7 (8.7) | 13.6 (9.1) | 0.44 (0.00–0.74) | 6.5 | 6 |
| Lateral Bending (coupled) | 32.4 (18.6) | 33.7 (28.4) | 0.62 (0.22–0.83) | 11.5 | 3 |
| Pelvic | |||||
| Axial Rotation | 103.1 (2.5) | 107.7 (34.8) | 0.81 (0.55–0.92) | 11.0 | 1 |
| Flexion-Extension (coupled) | 5.7 (2.6) | 5.1 (3.7) | 0.62 (0.25–0.83) | 1.6 | 3 |
| Lateral Bending (coupled) | 8.9 (6.3) | 7.1 (3.5) | 0.51 (0.06–0.77) | 4.4 | 7 |
IQR; InterQuartile Range, ICC; Intraclass Correlation Coefficient, SEM; Standard Error of Measurement (in degrees)
4. Discussion
Opto-electronic motion capture showed excellent between-session reliability to measure trunk sagittal posture in healthy participants. Our results are in agreement with prior studies reporting fair to excellent between-session reliability of thoracic and lumbar sagittal curves and pelvic tilt with spinal markers (Dunk et al., 2004; Dunk et al., 2005; Muyor et al., 2017). However, these prior studies did not use motion analysis of spinal clusters.
In agreement with other kinematics studies, lumbar and pelvic segments contributed most to flexion and extension ROM, thoracic segment to lateral bending, and both thoracic and pelvic segments to axial rotation ROM. Mean angles of thoracic and lumbar segments are also in line with previously reported marker-based measurements (Schinkel-Ivy et al., 2015; Tojima et al., 2013; Willems et al., 1996). Greater contribution of a segment to a particular motion was often associated with higher reliability. In general, we found fair to excellent between-session reliability to measure ROM during flexion and extension trials. Our results also show fair to excellent between-session reliability for trunk ROM in lateral bending and axial rotation trials for primary and most coupled direction motions. It should also be noted that reliability does not guarantee accuracy of measurement. Motion analysis is subject to error, for example due to soft tissue artefacts, although it has been shown that sagittal angles and motions can be measured with reasonable accuracy (Schmid et al., 2015; Zemp et al., 2014). Prior studies measuring 3D spine motion have used rigid clusters that spanned the spine and paraspinal musculature (Cotter et al., 2014; Preuss and Popovic, 2010). We used smaller clusters that fit on the spine midline with little overlap of paraspinal muscles. While this may reduce error due to soft tissue artefact, having markers closer together may have increased noise and reconstruction errors.
We estimate that three to four trials would provide satisfactory between-session reliability for the majority of measures examined in this study. Repeated measurements improve error and reliability, and good within-session reliability can reportedly be obtained with two to five trials for most trunk kinematic measures (Schinkel-Ivy et al., 2015). While between-session reliability might be expected to be lower than within-session, this suggests that the two are not dissimilar. Overall, this shows that reliable measurements of key spine motions can be obtained with a reasonable number of trial repetitions.
While testing a relatively small sample of healthy adults is a limitation of this study, our participants included men and women and ranged in age from 24 to 74 years old. Thus the reliability results are applicable for both sexes and across the age span. The BMI of the recruited participants mostly fell in the normal to overweight range of BMI, so our results may not be applicable to obese people, in whom reliability might be affected by increased soft tissue artefacts. Additional studies would be required to examine whether reliability might vary with characteristics such as age, sex, and obesity, or in patients with pain or other pathological conditions.
In summary, this study demonstrates that opto-electronic motion capture measurements afford objective, quantitative and reliable data on a patient’s posture and kinematics. Importantly, we demonstrate that reliable data can be obtained with a reasonable number of trial repetitions for most outcomes. In addition motion capture allows for three-dimensional and dynamic outcomes to be assessed, which would not be possible with standard diagnostic approaches such as radiographic studies. We also report results for the thoracic spine, lumbar spine, and pelvis, including non-sagittal and coupled ROMs, which provide a more comprehensive set of spine ROM outcomes than prior studies. Overall, this information supports the use of motion capture systems to assess spine posture and motion in future clinical studies, for example to better understand the effects of aging and spine disorders.
Supplementary Material
Acknowledgments
This work was conducted with support from the National Institute on Aging of the National Institutes of Health (R00AG042458), the Department of Orthopaedic Surgery at Beth Israel Deaconess Medical Center, and Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health. The study sponsors had no role in the study design, data collection, analysis, manuscript preparation, or the decision to submit the manuscript for publication.
Footnotes
Conflict of interest statement
All authors have declared no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Christe G, Kade F, Jolles BM, Favre J, 2017. Chronic low back pain patients walk with locally altered spinal kinematics. J Biomech 60, 211–218. [DOI] [PubMed] [Google Scholar]
- Chun SW, Lim CY, Kim K, Hwang J, Chung SG, 2017. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J 17, 1180–1191. [DOI] [PubMed] [Google Scholar]
- Cotter BD, Nairn BC, Drake JD, 2014. Should a standing or seated reference posture be used when normalizing seated spine kinematics? J Biomech 47, 2371–2377. [DOI] [PubMed] [Google Scholar]
- Dunk NM, Chung YY, Compton DS, Callaghan JP, 2004. The reliability of quantifying upright standing postures as a baseline diagnostic clinical tool. J Manipulative Physiol Ther 27, 91–96. [DOI] [PubMed] [Google Scholar]
- Dunk NM, Lalonde J, Callaghan JP, 2005. Implications for the use of postural analysis as a clinical diagnostic tool: reliability of quantifying upright standing spinal postures from photographic images. J Manipulative Physiol Ther 28, 386–392. [DOI] [PubMed] [Google Scholar]
- Hidalgo B, Gilliaux M, Poncin W, Detrembleur C, 2012. Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med 44, 756–763. [DOI] [PubMed] [Google Scholar]
- Ignasiak D, Rueger A, Ferguson SJ, 2017. Multi-segmental thoracic spine kinematics measured dynamically in the young and elderly during flexion. Hum Mov Sci 54, 230–239. [DOI] [PubMed] [Google Scholar]
- Kuwahara W, Deie M, Fujita N, Tanaka N, Nakanishi K, Sunagawa T, Asaeda M, Nakamura H, Kono Y, Ochi M, 2016. Characteristics of thoracic and lumbar movements during gait in lumbar spinal stenosis patients before and after decompression surgery. Clin Biomech (Bristol, Avon) 40, 45–51. [DOI] [PubMed] [Google Scholar]
- Marich AV, Hwang CT, Salsich GB, Lang CE, Van Dillen LR, 2017. Consistency of a lumbar movement pattern across functional activities in people with low back pain. Clin Biomech (Bristol, Avon) 44, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD, 2008. Expenditures and health status among adults with back and neck problems. JAMA 299, 656–664. [DOI] [PubMed] [Google Scholar]
- Montgomery T, Boocock M, Hing W, 2011. The effects of spinal posture and pelvic fixation on trunk rotation range of motion. Clin Biomech (Bristol, Avon) 26, 707–712. [DOI] [PubMed] [Google Scholar]
- Muyor JM, Arrabal-Campos FM, Martinez-Aparicio C, Sanchez-Crespo A, Villa-Perez M, 2017. Test-retest reliability and validity of a motion capture (MOCAP) system for measuring thoracic and lumbar spinal curvatures and sacral inclination in the sagittal plane. J Back Musculoskelet Rehabil 30, 1319–1325. [DOI] [PubMed] [Google Scholar]
- Nairn BC, Chisholm SR, Drake JD, 2013. What is slumped sitting? A kinematic and electromyographical evaluation. Man Ther 18, 498–505. [DOI] [PubMed] [Google Scholar]
- Preuss RA, Popovic MR, 2010. Three-dimensional spine kinematics during multidirectional, targetdirected trunk movement in sitting. J Electromyogr Kinesiol 20, 823–832. [DOI] [PubMed] [Google Scholar]
- Rast FM, Graf ES, Meichtry A, Kool J, Bauer CM, 2016. Between-day reliability of three dimensional motion analysis of the trunk: A comparison of marker based protocols. J Biomech 49, 807–811. [DOI] [PubMed] [Google Scholar]
- Schinkel-Ivy A, DiMonte S, Drake JD, 2015. Repeatability of kinematic and electromyographical measures during standing and trunk motion: how many trials are sufficient? J Electromyogr Kinesiol 25, 232–238. [DOI] [PubMed] [Google Scholar]
- Schmid S, Studer D, Hasler CC, Romkes J, Taylor WR, Brunner R, Lorenzetti S, 2015. Using Skin Markers for Spinal Curvature Quantification in Main Thoracic Adolescent Idiopathic Scoliosis: An Explorative Radiographic Study. PLoS One 10, e0135689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid S, Studer D, Hasler CC, Romkes J, Taylor WR, Lorenzetti S, Brunner R, 2016. Quantifying spinal gait kinematics using an enhanced optical motion capture approach in adolescent idiopathic scoliosis. Gait Posture 44, 231–237. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL, 1979. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86, 420–428. [DOI] [PubMed] [Google Scholar]
- Tojima M, Ogata N, Yozu A, Sumitani M, Haga N, 2013. Novel 3-dimensional motion analysis method for measuring the lumbar spine range of motion: repeatability and reliability compared with an electrogoniometer. Spine (Phila Pa 1976) 38, E1327–1333. [DOI] [PubMed] [Google Scholar]
- Willems JM, Jull GA, J KF, 1996. An in vivo study of the primary and coupled rotations of the thoracic spine. Clin Biomech (Bristol, Avon) 11, 311–316. [DOI] [PubMed] [Google Scholar]
- Zemp R, List R, Gulay T, Elsig JP, Naxera J, Taylor WR, Lorenzetti S, 2014. Soft tissue artefacts of the human back: comparison of the sagittal curvature of the spine measured using skin markers and an open upright MRI. PLoS One 9, e95426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.