Abstract
Background:
Based on the strong link between poverty and child health outcomes, both the AAP and national pediatric oncology associations have advocated for routine clinical poverty screening. Systematic implementation of this recommendation in pediatric oncology is not yet standard, and feasibility data are needed. We report the feasibility of routine poverty screening in a pediatric oncology referral center and baseline poverty characteristics of this population.
Methods:
From 2013–2017, 448 newly diagnosed pediatric cancer families at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center were offered the Psychosocial Assessment Tool 2.0 (PAT) as part of routine care. The PAT includes a two-item screen for household material hardship (HMH). All families were asked about annual household income by a Resource Specialist. Data were abstracted with sociodemographic and child/disease characteristics. Descriptive statistics are reported.
Results:
413 families completed the PAT (response rate 92%), of whom 394 (95%) completed specific questions assessing for HMH. Ninety-four percent of families who met with a Resource Specialist disclosed their annual household income. One quarter (27%) of families were ≤200% Federal Poverty Level (FPL) at diagnosis, and 44% of families endorsed at least one domain of HMH. The most frequent domains of HMH included housing (24%), utilities (20%), and transportation (20%).
Conclusions:
Systematic poverty screening per AAP and pediatric oncology psychosocial standards of care is feasible in routine cancer care. There is a high baseline incidence (44%) of HMH in at least one domain in newly diagnosed pediatric cancer families who may benefit from early identification and resource intervention.
Keywords: Poverty screening, household material hardship, health services, psychosocial care
Introduction
Over 40% of children in the United States live in “poor, near poor, or low income” households,[1] with an ever-growing literature base demonstrating the negative effects of poverty on child health.[2–4] Poverty and associated toxic stress have been linked to adult chronic health burden, as well as early death.[5] The profound implications and magnitude of this problem prompted the American Academy of Pediatrics (AAP) to release a policy statement in 2016 advocating for systematic poverty screening in the medical home.[6] Subsequent social resource screening and intervention studies conducted in the primary care/general pediatrics setting demonstrate both feasibility and efficacy of such screening.[7–11] However, such evaluation has not been expanded to subspecialty pediatric settings which frequently function as medical homes for the estimated 18% of U.S. children with chronic health conditions (e.g. cancer, congenital heart disease, metabolic condition, developmental/behavioral disorder, etc.) and special health care needs.[12] Given that pediatric oncologists routinely replace the traditional primary care medical home to assume primary care for children during active cancer treatment and early survivorship, pediatric oncology represents an obvious subspecialty in which to investigate the feasibility of integrating AAP recommendations.
In 2015, the AAP call to action for systematic poverty screening was echoed by an interdisciplinary group of pediatric oncology psychosocial professionals who included systematic assessment of financial burden as one of 15 recommended standards of psychosocial care for all children with cancer.[13,14] As part of this project, Pelletier and Bona published an extensive review concluding that financial hardship during treatment of childhood cancer affected a significant proportion of families and negatively impacted their well-being.[15] These psychosocial standards were publicly endorsed by a majority of pediatric oncology national organizations including the Children’s Oncology Group (COG), American Society of Pediatric Hematology/Oncology (ASPHO), American Psychosocial Oncology Society (APOS), Association of Pediatric Oncology Social Workers (APOSW) and the Association of Pediatric Hematology/Oncology Nurses (APHON) among others. In the intervening 3 years, studies investigating implementation of these standards of care found that over 40% of centers report non-adherence to systematic assessment of family financial burden.[16,17] These studies concluded that there is a need for more evidence-based approaches to inform the feasibility of practically implementing systematic poverty screening across a wide-range of pediatric oncology practices.
Family poverty can be assessed in multiple domains including both income poverty as well as concrete measures of basic need (known as household material hardship, HMH) such as food, housing, utility, or transportation insecurity. HMH as a measure of poverty is appealing in the context of systematic clinical screening as it is both associated with child health outcomes, and remediable with clinic-based intervention.[18–21] HMH is widely prevalent in the U.S.—nearly 1 in 5 U.S. children lives in a food insecure home—and primary care data demonstrate that linking families with HMH with targeted “safety-net” programs (e.g. food stamps or food banks) can improve child outcomes.[11,22] To date, only a single small research study has explored the feasibility of poverty screening in pediatric oncology.[23] Potential barriers to systematic screening include both parental reluctance to participate, as well as challenges with adequate staffing to perform and respond to such screening. It is plausible that caregivers in the time-sensitive and life-threatening context of a child’s cancer diagnosis may be less willing to share socioeconomic information than in the primary care setting due to fears about how this information could impact the care of their child. To help guide the integration of both AAP and pediatric oncology psychosocial into routine pediatric cancer care, we report the feasibility of systematic poverty screening as part of routine pediatric cancer care and identify the incidence of HMH in a clinical cohort of over 400 newly diagnosed pediatric cancer families.
Patients and Methods
Study Population and Data Collection
From April 2013 to January 2017, a total of 448 families of children (age <21 years old) with a new diagnosis of cancer and planned chemotherapy receipt at the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center Institute (DF/BCH) were offered the Psychosocial Assessment Tool 2.0 (PAT) as part of routine pediatric psychosocial oncology care. Routine clinical practice during this time-frame included offering the PAT as clinical screening to all families who met the following criteria: (1) child aged <21 years within 4 weeks of a new cancer diagnosis; (2) planned to receive chemotherapy at DF/BCH; (3) spoke English or Spanish; (4) child was not critically ill in the ICU during the 4 week time-frame. The PAT is a validated two-page self-report measure consisting of 15-item sets utilized to broadly assess for psychosocial risk.[24] The PAT is not specifically focused on poverty screening, but includes questions regarding financial hardship in its introductory demographic section. For this analysis, as detailed below, we examined two questions from the sociodemographic section of the PAT that assess financial hardship and HMH.
One parent/guardian was asked to complete the paper-pencil PAT by a non-clinical member of the psychosocial oncology staff while inpatient at Boston Children’s Hospital or outpatient at the Dana-Farber Cancer Institute (DF/BCH) generally within one month of diagnosis (median time to administration: 21 days from diagnosis). The PAT is a part of routine clinical care, thus research consent was not obtained at the time of administration. Parents placed the completed form in an envelope and left it with administrative staff for collection. The assessment tool was then scanned into the electronic medical record. In addition to the PAT, all families treated at DF/BCH are routinely screened in-person by a Resource Specialist to identify concrete resource needs, including a question about annual household income which Resource Specialists utilize to identify resource eligibility. Resource Specialist screenings are documented in the electronic medical record. This study was approved by the Dana-Farber Cancer Institute Institutional Review Board.
Outcome Measures
The demographic section of the PAT contains two questions assessing for general financial hardship and then specific domains of HMH. Families are first asked “Is your family having money problems? (check one box): none, some problems, many problems, it’s hard to meet our basic needs.” This is followed by: “In what areas are you having money problems? (check all boxes that apply): none, phone/heat/light bills, paying rent/mortgage, buying food, car costs (upkeep/gas/insurance), medical bills, other.” For this analysis, any response other than “none” to the first question was considered a report of some degree of financial hardship. Families were considered to have HMH if they answered affirmatively to any response other than “none” in the second question regarding basic needs. If families answered “none” to the first question and left the second question blank, we coded this as “none” for the second question. We additionally examined two other questions from the PAT: “How will you get to the hospital or clinic for appointments?” and “Who can offer help with money/finances?”
Baseline family income was routinely collected at Resource Specialist intake and documented as a free text variable in a separate intake note. Income was transformed into a percentage of Federal Poverty Level (FPL) for the year the intake was completed and stratified into two levels (≤200%, >200%).[25] Stratification at ≤200% FPL is consistent with other publications focusing on poor and near-poor families and may additionally identify those eligible for governmental supports.[26,27]
Chart Abstraction
Medical chart abstraction was performed by a trained research assistant and duplicated by a second research assistant for every tenth subject with inconsistencies reconciled with the principal investigator (KB). Data elements were abstracted from responses to the parent-reported PAT survey entered into the electronic medical record including: child’s sex, age at diagnosis, date of diagnosis, date of survey completion, race/ethnicity, cancer diagnosis, health insurance, caregiver’s relationship to child, caregiver’s highest level of education, primary language in household, single parent household, household size, and the specific questions regarding financial hardship, HMH, transportation, and financial help described in the preceding section. Annual household income in dollars was abstracted from the free-text Resource Specialist note.
Statistical Analysis
Child, disease, care and family characteristics were described with medians and interquartile ranges for continuous variables and frequencies and proportions for categorical variables. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Feasibility and response rates
From April 7, 2013 to January 6, 2017, the psychosocial oncology team met with 950 families. Of these families, 448 families met their clinical eligibility criteria detailed in the Methods section and were offered the PAT to complete. The remaining 502 families were not offered the PAT as part of routine care for the following reasons: N=128 spoke a language other than English or Spanish, N=128 had relapsed disease, N=246 were planning to transfer care, were not receiving chemotherapy (e.g. surgery only) or were >21 years of age. Of the 448 families offered the PAT to complete, 413 returned a completed survey (participation rate 92%). Among 413 completed surveys, the response rates for the two questions related to financial hardship and HMH were 98% (N=404) and 95% (N=394) respectively, with recoding of blank responses for HMH as “none” if a family had reported no financial hardship. Ninety-six percent (N=396) of families completed a consultative intake visit with a Resource Specialist based on the presence of an intake note in the electronic medical record. Of these, 94% (N=372) reported household income to the Resource Specialist.
Patient, caregiver, and household characteristics
At the time of diagnosis, children were a median age of 7.5 years (IQR: 3.4 – 14.5) and 70% were non-Hispanic White (Table 1). Hematological malignancies were overrepresented at 52% of the cohort, and brain tumors were underrepresented at 12% of the cohort.[28] In terms of insurance at diagnosis, 85% had private insurance, 13% of children relied on Medicaid only, and 2% were uninsured. A majority of survey respondents (72%) were mothers, and 29% had an educational attainment of high school or less. Approximately 10% of patients came from single parent households.
Table 1.
Patient, caregiver and household characteristics at time of diagnosis (N=413)
| N (%) | |
|---|---|
| Patient characteristics | |
| Sex (N=413) Male Female |
244 (59.1) 169 (40.9) |
| Age at diagnosis in years, median (IQR, N=413) | 7.5 (3.4–14.5) |
| Race/Ethnicity (N=385) White, non-Hispanic Other |
269 (69.9) 116 (30.1) |
| Cancer Diagnosis (N=396) Hematologic malignancy Solid tumor Brain tumor |
204 (51.5) 146 (36.9) 46 (11.6) |
| Health Insurance (N=403) None Medicaid only Any private insurance |
6 (1.5) 54 (13.4) 343 (85.1) |
| Caregiver characteristics | |
| PAT Respondent’s Relationship to Child (N=413) Mother Father Other |
299 (72.4) 107 (25.9) 7 (1.7) |
| Highest level of educational attainment (N=408) High school or less Associate/Bachelors Masters/Doctorate |
120 (29.4) 173 (42.4) 115 (28.2) |
| Household characteristics | |
| Primary language (N=393) English Other |
371 (94.4) 22 (5.6) |
| Single Parent Household (N=406) Yes No |
41 (10.1) 365 (89.9) |
| Household size (N=413) 2 people 3 people 4 people ≥5 people |
18 (4.4) 91 (22.0) 168 (40.7) 136 (32.9) |
Income and household material hardship
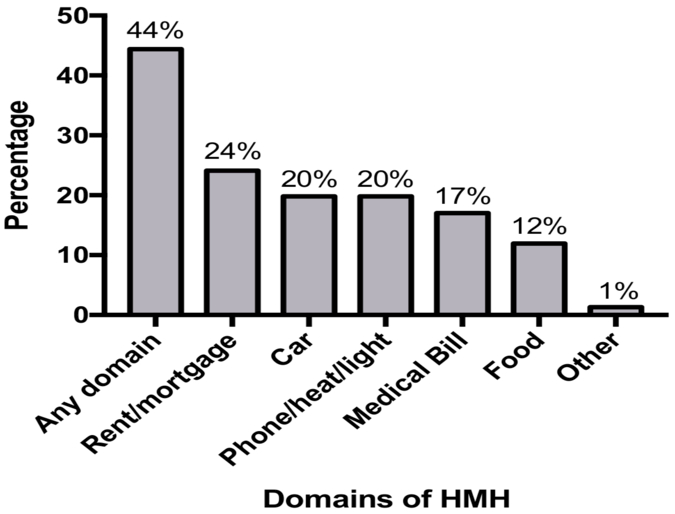
Median household income for the cohort was $94,000 (IQR=$45,500 – $150,000), similar to the median household income for families with children in Massachusetts of $98,400 in 2016.[29] Twenty-seven percent of families reported household incomes ≤200% FPL (Table 1). Forty-six percent of families endorsed any level of financial hardship (some money problems, many money problems, it’s hard to meet basic needs) with 13% citing “many problems” or that it was “hard to meet basic needs” (Table 2). Forty-four percent of families endorsed at least one domain of household material hardship (Figure 1), with 32% endorsing HMH in the core basic needs of food, housing and utilities. The most frequent domains of HMH reported included rent/mortgage (24%), car (20%), and phone/heat/light (20%). Of those who reported HMH, a majority (59%) endorsed difficulty in more than one domain. Even among higher income families (household income >200% FPL), 36.3% endorsed at least one domain of HMH. Similarly, 38.4% of privately insured families endorsed at least one domain of HMH (Table 2). Regarding non-emergency medical transportation to clinic, 9% of families reported using public transportation, 12% reported needing rides from others, and 5% reported being unsure of how they would get to the hospital for appointments (Table 2). Over 10% of families reported that they felt they had no one who could help with money/finances.
Table 2.
Caregiver-reported household income and resource needs at time of diagnosis (N=413)
| N (%) | |
|---|---|
| Household income | |
| Household income at diagnosis in dollars, median (IQR, N=372) | 94,000 (45,500–150,000) |
| Household income as percent of FPL (N=372) ≤200% FPL >200% FPL |
100 (26.9) 272 (73.1) |
| Household material hardship | |
| “Is your family having money problems?” (N=404) None Some problems Many problems It’s hard to meet our basic needs |
218 (54.0) 135 (33.4) 23 (5.7) 28 (6.9) |
| “In what areas are you having money problems?” (N=394) None Any domain of HMH 1 domain of HMH ≥2 domains of HMH ≥1 domain of HMH in families with income >200% FPL (N=223) ≥1 domain of HMH in families with private insurance (N=276) |
219 (55.6) 175 (44.4) 71 (40.6) 104 (59.4) 81 (36.3) 106 (38.4) |
| Other measures of resource need and support | |
| “How will you get to the hospital or clinic for appointments?” (N=411, select all that apply) Own car Rides Public transport Unsure |
356 (86.6) 50 (12.2) 37 (9.0) 19 (4.6) |
| “Who can offer help with money/finances?” (N=385, select all that apply) Husband/wife/partner Child’s grandparents Other family members Friends People at work Other No one |
271 (70.4) 194 (50.4) 132 (34.3) 93 (24.2) 32 (8.3) 24 (6.2) 46 (12.0) |
Figure 1.
Household Material Hardship Reported by Families (N=394)*
*Percentage totals exceed 100% since respondents may select one or more domains of HMH.
Discussion
In this cohort of newly diagnosed pediatric cancer families at a major referral center, we found that over 40% reported “money problems” in at least one basic resource domain around the time of their child’s diagnosis, with 59% citing difficulties in more than one domain of HMH. A striking 13% of families reported having “many” money troubles or that it was “hard to meet basic needs.” Families were overwhelmingly willing to answer questions with regard to finances and poverty as part of routine care. Of the 413 families who completed the PAT, 95% answered specific questions assessing for HMH on a self-report tool. Of the 396 families who completed a consultative intake visit with a Resource Specialist, 94% shared baseline annual household income. Our study demonstrates that screening for poverty as part of routine pediatric oncology care is feasible and acceptable to parents. Given the high incidence of HMH identified, our data additionally point to the need for systematic clinical responses to these data including future intervention work.
To our knowledge, this is the largest study to date describing baseline HMH in families of children newly diagnosed with cancer. Compared to a smaller research study by our group which found that 20% of families presented with HMH at diagnosis,[23] routine clinical screening identified a higher incidence (44%) in this sample. This difference is likely due both to use of a more restrictive HMH domains (housing, food, and utilities only) in the earlier research study, as well as use of validated and more specific HMH measures than the single item utilized in the PAT [30,31]. When we restrict our definition to “money problems” in domains of housing, food and utilities in this clinical cohort, we approach a more comparable rate of 32%. It should be noted, that the PAT item regarding basic needs asks families to endorse “money problems” not “unmet needs” in each domain. This more inclusive definition of HMH may over-estimate the proportion of families in need of support at time of diagnosis.
This said, prior publications have demonstrated an increase in financial hardship over the course of cancer treatment secondary to income losses (due to work disruption) as well as out-of-pocket expenses (e.g. travel, accommodation, and communication costs) in populations without pre-existing HMH or low-income at the time of diagnosis.[23,32–37] Other studies show that some patients and families may be affected by these financial burdens for several years following diagnosis and even into survivorship.[38–40] We found a substantial proportion (36.3%) of families with incomes >200% FPL who endorsed at least one domain of HMH. There were similarly many families (38.4%) who identified HMH despite having private health insurance. Together, these results suggest that income and insurance screening alone are insufficient approaches to uncovering basic hardship for families. In a 2003 study using data from welfare recipients, Sullivan et al found that current annual income was not strongly related to most measures of material hardship.[41] This is consistent with past literature arguing that there are only weak to moderate correlations between income and HMH and that models of family income must contain indices of material hardship to better understand the complex patterns of poverty which affect child health.[42–48] The optimal sensitivity and specificity of a clinical screen for financial hardship in the pediatric oncology setting should be investigated in future studies.
With evidence of poverty-related cancer outcome disparities[49] and both the AAP and the pediatric oncology psychosocial standards of care advocating for systematic poverty screening, there is a clear need for moving towards consistent integration of this practice. Our data demonstrate that families are willing to participate in routine poverty screening utilizing both self-report (e.g. the PAT) and face-to-face (e.g. Resource Specialist intake) methodologies. The former is perhaps most pertinent when considered in the context of scalability across pediatric oncology centers with more limited psychosocial staffing. In-line with data from general pediatrics [8], our data demonstrate that 95% of families provided with self-report questions to screen for poverty will complete such a screen. This approach to systematic screening is likely generalizable across centers with even basic staffing. In general pediatrics, numerous interventions have proven effective in reducing HMH and connecting families to resources. Innovative examples include a novel program, StreetCred, developed by Hole and colleagues which embeds free tax-filing services in a primary care clinic to assist low income families;[50] systematic clinic-based screening and referral for HMH such as WECARE;11 and utilization of trained undergraduate volunteers in urban clinics such as HealthLeads to facilitate patient resource connection.[9] Our data demonstrate the feasibility of systematic screening for poverty measures as part of routine care in pediatric oncology. Next steps should include evaluation of previously published primary care resource connection interventions and consideration of tailored intervention development. Further consideration of optimal screening measures is additionally needed.
Our data must be interpreted in light of certain limitations. This is a single institution study from a large academic referral center that is well-staffed with designated Resource Specialists and psychosocial clinicians, which may limit the generalizability of our findings. A recent survey of the availability of psychosocial staff at 144 pediatric oncology programs concluded that not having a comprehensive multidisciplinary team was a barrier to full implementation of the psychosocial standards of care despite most programs having basic staffing.[51] With regard to the prevalence of poverty in our sample, our data are limited by the fact that the PAT was administered only in English and Spanish that likely resulted in an underrepresentation of racial and ethnic minorities in our sample. Given that racial and ethnic minorities in the United States are more likely to live in poverty, it is possible that our cohort underestimates the true prevalence of HMH and financial hardship across pediatric oncology families.[52] Future clinical and research screening efforts must deliberately include instruments validated in languages other than English. The PAT is now available in over 10 languages, with more translations in process suggesting its potential applicability in international settings.[53] Furthermore, alternative screening tools for HMH (e.g. the Hunger Vital Sign) are validated in both English and Spanish [54]. The cross-sectional nature of this study does not capture how financial burden changes over time. Due to the heterogeneity of cancer diagnoses in this cohort, our data cannot be correlated with clinical outcomes. Future studies with larger samples are needed to characterize associations of poverty measures and health outcomes in this patient population, as well as how these measures change longitudinally over the course of treatment and into survivorship. Lastly, this study is limited by a caregiver’s subjective interpretation of their financial need. We specifically chose to use a more inclusive definition of financial hardship (i.e. any response other than “none” when asked about money problems) because the purpose of a broader initial screen for HMH would be to identify all families that may benefit from and qualify for intervention.
Conclusions
Child poverty is a critical health issue pertinent to pediatric oncology. As has been demonstrated in general pediatrics, a staggering proportion of newly diagnosed pediatric cancer families report financial hardship and HMH at baseline and may benefit from early intervention and connection to resources. Systematic screening for poverty as part of routine care is feasible even in the context of a time-sensitive and life-threatening diagnosis of cancer. Pediatric oncology must embrace both the AAP and the pediatric oncology psychosocial standards’ call for systematic poverty screening as part of standard of care clinical practice and begin efforts to evaluate systematic interventions. General pediatricians who have led early adoption efforts can help educate and inform future work exploring clinic-based interventions and poverty-related outcomes research in the subspecialty setting.
Acknowledgments:
We would like to thank our patients and families. We would also like to thank Joe Chabot and our Resource Specialist team for their amazing work with our patients and families. Finally, we would like to thank Madeline Bilodeau, Porag Das and Danielle Renzi for their attention to detail in medical record abstraction.
Funding Source: This study was funded in part by a grant from Pedals for Pediatrics. Dr. Bona is supported by National Cancer Institute 1K07CA211847.
Abbreviations Table:
- AAP
American Academy of Pediatrics
- HMH
Household material hardship
- PAT
Psychosocial Assessment Tool 2.0
- DF/BCH
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center Institute
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest relevant to this article to disclose.
Financial Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest
The authors declare they have no conflicts of interest relevant to this article to disclose.
References
- 1.DeNavas-Walt C, Proctor BD. Current population reports, P60–252, income and poverty in the United States: 2014 Washington, DC: US Government Printing Office; 2015. [Google Scholar]
- 2.Wood D Effect of child and family poverty on child health in the United States. Pediatrics 2003:112(Supplement 3):707–711. [PubMed] [Google Scholar]
- 3.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. The future of children 1997:55–71. [PubMed] [Google Scholar]
- 4.Ratcliffe C, McKernan S-M. Childhood poverty persistence: Facts and consequences: Urban Institute; Washington, DC; 2010. [Google Scholar]
- 5.Shonkoff JP, Garner AS, Siegel BS, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012:129(1):e232–e246. [DOI] [PubMed] [Google Scholar]
- 6.Gitterman BA, Flanagan PJ, Cotton WH, et al. Poverty and child health in the United States. Pediatrics 2016:peds. 2016–0339. [DOI] [PubMed] [Google Scholar]
- 7.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA pediatrics 2016:170(11):e162521–e162521. [DOI] [PubMed] [Google Scholar]
- 8.Garg A, Butz AM, Dworkin PH, et al. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics 2007:120(3):547–558. [DOI] [PubMed] [Google Scholar]
- 9.Garg A, Marino M, Vikani AR, et al. Addressing families’ unmet social needs within pediatric primary care: the health leads model. Clinical pediatrics 2012:51(12):1191–1193. [DOI] [PubMed] [Google Scholar]
- 10.Garg A, Sarkar S, Marino M, et al. Linking urban families to community resources in the context of pediatric primary care. Patient education and counseling 2010:79(2):251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garg A, Toy S, Tripodis Y, et al. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics 2015:135(2): e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newacheck PW, Strickland B, Shonkoff JP, et al. An epidemiologic profile of children with special health care needs. Pediatrics 1998:102(1):117–123. [DOI] [PubMed] [Google Scholar]
- 13.Kazak AE, Abrams AN, Banks J, et al. Psychosocial assessment as a standard of care in pediatric cancer. Pediatric blood & cancer 2015:62(S5). [DOI] [PubMed] [Google Scholar]
- 14.Wiener L, Kazak AE, Noll RB, et al. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatric blood & cancer 2015:62(S5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pelletier W, Bona K. Assessment of financial burden as a standard of care in pediatric oncology. Pediatric blood & cancer 2015:62(S5). [DOI] [PubMed] [Google Scholar]
- 16.Jones B, Currin-Mcculloch J, Pelletier W, et al. Psychosocial standards of care for children with cancer and their families: A national survey of pediatric oncology social workers. Social work in health care 2018:57(4):221–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scialla MA, Canter KS, Chen FF, et al. Delivery of care consistent with the psychosocial standards in pediatric cancer: Current practices in the United States. Pediatric blood & cancer 2018:65(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyers A, Cutts D, Frank DA, et al. Subsidized housing and children’s nutritional status: data from a multisite surveillance study. Archives of pediatrics & adolescent medicine 2005:159(6):551–556. [DOI] [PubMed] [Google Scholar]
- 19.Cook JT, Frank DA, Berkowitz C, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. The Journal of nutrition 2004:134(6):1432–1438. [DOI] [PubMed] [Google Scholar]
- 20.Frank DA, Neault NB, Skalicky A, et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics 2006:118(5):e1293–e1302. [DOI] [PubMed] [Google Scholar]
- 21.Black MM, Cutts DB, Frank DA, et al. Special Supplemental Nutrition Program for Women, Infants, and Children participation and infants’ growth and health: a multisite surveillance study. Pediatrics 2004:114(1):169–176. [DOI] [PubMed] [Google Scholar]
- 22.Sege R, Preer G, Morton SJ, et al. Medical-legal strategies to improve infant health care: a randomized trial. Pediatrics 2015:136(1):97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bona K, London WB, Guo D, et al. Trajectory of material hardship and income poverty in families of children undergoing chemotherapy: a prospective cohort study. Pediatric blood & cancer 2016:63(1):105–111. [DOI] [PubMed] [Google Scholar]
- 24.Pai AL, Patiño-Fernández AM, McSherry M, et al. The Psychosocial Assessment Tool (PAT2. 0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. Journal of pediatric psychology 2007:33(1):50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U.S. Department of Health and Human Services. Prior HHS Poverty Guidelines and Federal Register References. Available at: http://aspe.hhs.gov/poverty/figures-fed-reg.shtml. Accessed: January 3, 2012.
- 26.Newacheck PW, Hughes DC, Hung Y-Y, et al. The unmet health needs of America’s children. Pediatrics 2000:105(Supplement 3):989–997. [PubMed] [Google Scholar]
- 27.Silver EJ, Stein RE. Access to care, unmet health needs, and poverty status among children with and without chronic conditions. Ambulatory Pediatrics 2001:1(6):314–320. [DOI] [PubMed] [Google Scholar]
- 28.Ward E, DeSantis C, Robbins A, et al. Childhood and adolescent cancer statistics, 2014. CA: a cancer journal for clinicians 2014:64(2):83–103. [DOI] [PubMed] [Google Scholar]
- 29.Center NKCD. 2017. October 8 Median family income among households with children. Annie E. Casey Foundation <http://datacenter.kidscount.org/data/tables/123-median-family-income-among-households-with-children-by-family-nativity-detailed/1/any/false/573,869,36,868,867/78,79/461>. Accessed 2017 October 8.
- 30.Blumberg SJ, Bialostosky K, Hamilton WL, et al. The effectiveness of a short form of the Household Food Security Scale. American journal of public health 1999:89(8):1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics 2010:125(5): e1115–e1123. [DOI] [PubMed] [Google Scholar]
- 32.Bona K, Dussel V, Orellana L, et al. Economic impact of advanced pediatric cancer on families. Journal of pain and symptom management 2014:47(3):594–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fluchel MN, Kirchhoff AC, Bodson J, et al. Geography and the burden of care in pediatric cancers. Pediatric blood & cancer 2014:61(11):1918–1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohn RJ, Goodenough B, Foreman T, et al. Hidden financial costs in treatment for childhood cancer: an Australian study of lifestyle implications for families absorbing out-of-pocket expenses. Journal of pediatric hematology/oncology 2003:25(11):854–863. [DOI] [PubMed] [Google Scholar]
- 35.Miedema B, Easley J, Fortin P, et al. The economic impact on families when a child is diagnosed with cancer. Current Oncology 2008:15(4):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abel GA, Albelda R, Khera N, et al. Financial hardship and patient-reported outcomes after hematopoietic cell transplantation. Biology of Blood and Marrow Transplantation 2016:22(8):1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bona K, London WB, Guo D, et al. Prevalence and impact of financial hardship among New England pediatric stem cell transplantation families. Biology of Blood and Marrow Transplantation 2015:21(2):312–318. [DOI] [PubMed] [Google Scholar]
- 38.Hiyoshi A, Montgomery S, Bottai M, et al. Trajectories of income and social benefits for mothers and fathers of children with cancer: A national cohort study in Sweden. Cancer 2018:124(7):1492–1500. [DOI] [PubMed] [Google Scholar]
- 39.Mader L, Roser K, Baenziger J, et al. Household income and risk‐of‐poverty of parents of long‐term childhood cancer survivors. Pediatric blood & cancer 2017:64(8):e26456. [DOI] [PubMed] [Google Scholar]
- 40.Lindahl Norberg A, Montgomery SM, Bottai M, et al. Short‐term and long‐term effects of childhood cancer on income from employment and employment status: A national cohort study in Sweden. Cancer 2017:123(7):1238–1248. [DOI] [PubMed] [Google Scholar]
- 41.Sullivan JX, Turner L, Danziger S. The relationship between income and material hardship. Journal of Policy Analysis and Management 2008:27(1):63–81. [Google Scholar]
- 42.Mayer SE, Jencks C. Poverty and the distribution of material hardship. Journal of Human resources 1989:88–114. [Google Scholar]
- 43.Mayer SE, Jencks C. Recent trends in economic inequality in the United States: Income versus expenditures versus material well-being Poverty and Prosperity in the USA in the Late Twentieth Century: Springer; 1993. p 121–207. [Google Scholar]
- 44.Rector RE, Johnson KA, Youssef SE. The extent of material hardship and poverty in the United States. Review of Social Economy 1999:57(3):351–387. [Google Scholar]
- 45.Boushey H, Brocht C, Gundersen B, et al. Hardships in America: The real story of working families: ERIC; 2001. [Google Scholar]
- 46.Perry B The mismatch between income measures and direct outcome measures of poverty. Social Policy Journal of New Zealand 2002:101–127. [Google Scholar]
- 47.Bradshaw J, Finch N. Overlaps in dimensions of poverty. Journal of social policy 2003:32(4):513–525. [Google Scholar]
- 48.Gershoff ET, Aber JL, Raver CC, et al. Income is not enough: Incorporating material hardship into models of income associations with parenting and child development. Child development 2007:78(1):70–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bona K, Blonquist TM, Neuberg DS, et al. Impact of Socioeconomic Status on Timing of Relapse and Overall Survival for Children Treated on Dana‐Farber Cancer Institute ALL Consortium Protocols (2000–2010). Pediatric blood & cancer 2016:63(6):1012–1018. [DOI] [PubMed] [Google Scholar]
- 50.Hole MK, Marcil LE, Vinci RJ. Improving Access to Evidence-Based Antipoverty Government Programs in the United States: A Novel Primary Care Initiative. JAMA pediatrics 2017:171(3):211–212. [DOI] [PubMed] [Google Scholar]
- 51.Scialla MA, Canter KS, Chen FF, et al. Implementing the psychosocial standards in pediatric cancer: Current staffing and services available. Pediatric blood & cancer 2017:64(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burton LM MM, Pedroza J, Welsh W. The Poverty and Inequality Report. The Stanford Center on Poverty and Inequality: State of the Union 20172017. [Google Scholar]
- 53.Psychosocial Assessment Tool (PAT) - Translating the PAT. <https://www.psychosocialassessmenttool.org/translation-of-the-pat>.
- 54.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010:126(1):e26–e32. [DOI] [PubMed] [Google Scholar]