Highlights
-
•
The Lassa virus GPC trimer has a unique architecture amongst class I viral GPCs.
-
•
Multiple conformations of both Lassa virus subunits exist.
-
•
Quaternary epitope antibodies are the most potent in Lassa virus neutralization.
-
•
Features specific to the arenavirus GPC can guide vaccine design.
Abstract
The structure of a prefusion arenavirus GPC was enigmatic for many years, owing to the metastable and non-covalent nature of the association between the receptor binding and fusion subunits. Recent engineering efforts to stabilize the glycoprotein of the Old World arenavirus Lassa in a native, yet cleaved state, allowed the first structure of any arenavirus prefusion GPC trimer to be determined. Comparison of this structure with the structures of other arenavirus glycoprotein subunits reveals surprising findings: that the receptor binding subunit, GP1, of Lassa virus is conformationally labile, while the GP1 subunit of New World arenaviruses is not, and that the arenavirus GPC adopts a trimeric state unlike other glycoproteins with similar fusion machinery. Structural analysis, combined with recent biochemical data regarding antibody epitopes and receptor binding requirements, provides a basis for rational vaccine design.
Current Opinion in Immunology 2018, 31:52–58
This review comes from a themed issue on Virus structure and expression
Edited by Kay Grünewald and Thomas Krey
For a complete overview see the Issue and the Editorial
Available online 26th May 2018
https://doi.org/10.1016/j.coviro.2018.05.002
1879-6257/© 2018 Elsevier B.V. All rights reserved.
Introduction
The arenavirus family (genus Mammarenavirus) includes over 30 known pathogens that exist on all populated continents on Earth. The Old World family of arenaviruses contains, among others, Lassa virus (LASV), which can cause hemorrhagic fever and is endemic in West Africa [1]; lymphocytic choriomeningitis virus (LCMV), which causes febrile illness, neurological disease and birth defects with a 2–5% seroprevalence in North America and Europe [2]; and the 80% lethal hemorrhagic fever virus Lujo (LUJV), which emerged in Southern Africa in 2008 [3]. Arenaviruses in the New World category include Machupo virus (MACV, [4]) and Junin virus (JUNV, [5]), the causative agents of Bolivian and Argentinian hemorrhagic fever, respectively, as well numerous other agents such as Sabía virus [6] and Guanarito virus [7].
All arenaviruses express a single protein, termed GPC, on the virion surface. GPC mediates host cell attachment and membrane fusion and entry. It is the sole antigen on the viral surface, the primary target of protective humoral immune responses [8•,9•] and a focus for vaccine design efforts. For all arenaviruses, GPC is a trimer that is synthesized as a single polypeptide chain and is subsequently cleaved by host cell proteases to attain its fusion-competent state. The mature GPC is a trimer of heterotrimers composed of the non-covalently associated subunits SSP, GP1 and GP2. SSP is the transmembrane stable signal peptide and is essential for viral infectivity [10, 11, 12, 13, 14, 15, 16, 17, 18]. GP1 binds receptor and determines tropism [19, 20, 21, 22, 23, 24, 25]. GP2 drives fusion of virus and host membranes, wherein GP2 undergoes an acid pH-driven, conformational change from a metastable, prefusion structure to a more stable, postfusion, six-helix bundle [26, 27, 28].
While all arenaviruses have the same GPC organization on their surface, receptor usage differs. Pathogenic New World arenaviruses such as MACV and JUNV use Transferrin Receptor 1 (TfR1) to enter cells [21]. Old World arenaviruses, such as LASV, bind to a sugar termed matriglycan attached to the protein alpha-dystroglycan (αDG) as their extracellular receptor [29, 30, 31]. LUJV appears to be different yet again and uses the recently identified protein neuropilin 2 (NRP2) as a receptor [32]. LASV requires the endosomal receptor LAMP1 for entry [33••], while LUJV requires the endosomal entry factor CD63 [32]. Use of both cell-surface and endosomal entry factors may be a feature shared amongst some pathogenic Old World arenaviruses, but is a feature not known for New World arenaviruses.
In the past 10 years, multiple structures of individual GP1 and GP2 subunits of various arenaviruses have been determined from the Harrison, Bowden, Abraham, Diskin, Rey, and Nunberg groups [19,27,28,34, 35, 36,37•,38••,39,40], along with a prefusion GP1–GP2 protomer of LCMV [41]. Most recently, the structure of the prefusion trimeric assembly of LASV was determined, bound to a human neutralizing antibody [42••]. Here, we review the current knowledge of arenavirus glycoprotein structures, focusing particularly on the prefusion trimeric structure of LASV GP, and discuss how this and other arenavirus structures can inform rational design of antibody therapeutics and vaccines.
The unique architecture of the arenavirus glycoprotein
The arenavirus GPC is a class I fusion protein and is a trimer on the viral surface [26,33••,42••]. Class I fusion proteins require a proteolytic cleavage event to release the fusion peptide or loop of the membrane-proximal subunit (termed GP2 in the case of the arenaviruses) from the polyprotein and allows the glycoprotein to adopt a metastable prefusion state. This inherent metastability coupled with the lack of a covalent linkage between the GP1 and GP2 subunits hindered determination of the prefusion arenavirus GPC trimer structure for many years. However, these challenges were recently overcome by structure-based design of a di-cysteine linkage between the GP1 and GP2 subunit to enable the GPC to be processed, yet maintain a prefusion state [41,42••].
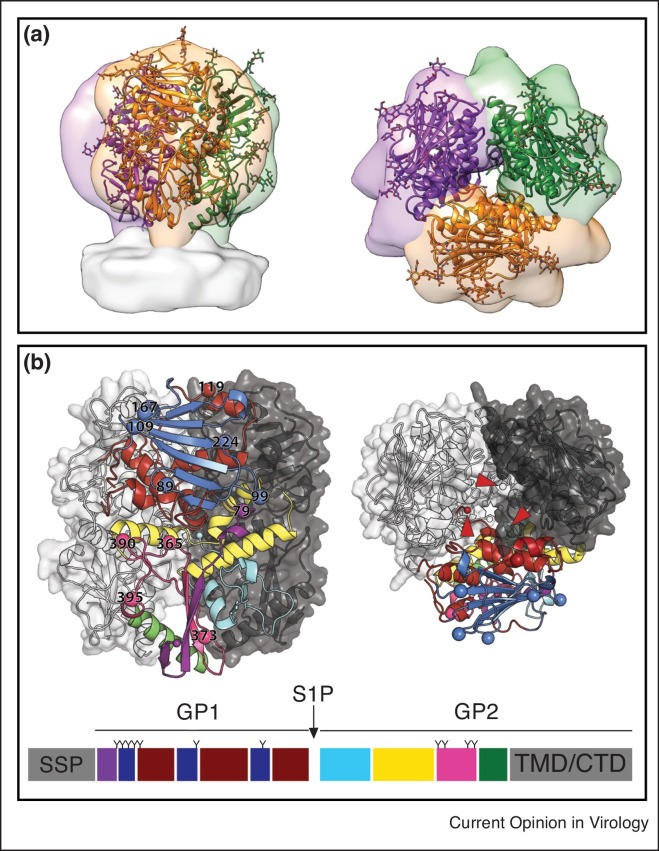
The crystal structure of the LASV GPC trimer adopts a compact tripod shape that closely matches the tomographic reconstruction of the GPC spike from authentic Lassa virions [33••] (Figure 1 a). Comparison of the LASV GPC trimer with that of the previously determined LCMV GPC prefusion structure [41] reveals why enzymatic cleavage between the GP1 and GP2 subunits is required for proper GPC trimer assembly: cleavage frees the GP1 C terminus, allowing it to achieve a necessary 30 Å repositioning into the trimer apex. There, it facilitates trimerization by packing against the GP1 subunit of the neighboring monomer (Figure 1b).
Figure 1.
The unusual arenavirus GP trimer. (a) The crystal structure of the LASV GP trimer (cartoon, PDB: 5VK2) docked into the tomographic reconstruction of the LASV GPC spike from fixed virions (surface, EMD: 3290). Glycans visible in the crystal structure are shown as ball and stick. (b) GP monomer A is shown in cartoon representation. LASV GP1 can be divided into three subdomains: (1) the N-terminal β-strands (purple, interacting with GP2); (2) the upper, β-sheet core (blue); and (3) the lower helix-loop surface (dark red). LASV GP2 can be divided into four subdomains: (1) the fusion region (cyan), which is composed of the fusion peptide and fusion loop; (2) HR1a-d (yellow); (3) the T-loop (magenta); and (4) HR2 (green). N-linked glycosylation sites are shown as spheres and numbered on their respective Asn residue. GP monomers B and C are shown as surfaces. The C terminus of each GP1 subunit is indicated with an arrow and the N termini of the GP2 subunits, which are positioned at the threefold axis and 30 Å below the apex of the trimer, are indicated with a star. A linear representation of the GPC protomer is shown a bottom with each subdomain of GPC colored according to the cartoon representation, with each N-linked glycosylation site indicated with a `Y’.
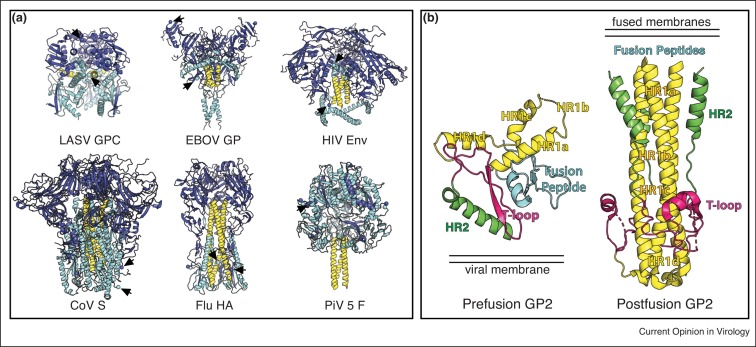
Comparison of LASV GPC to that of other class I viral glycoprotein trimers reveals two notable differences. First, in every type I viral glycoprotein structure determined to date, the trimer is formed about a central three-helix bundle of the fusion subunit (Figure 2 a). This three-helix core remains largely unaltered in structure upon transition from the prefusion conformation to that of the postfusion conformation. LASV GPC, however, lacks such a core and instead the equivalent region of GP2 is oriented nearly perpendicularly to the threefold axis. As a result, every section of LASV GP2 must unravel from the GPC protomer and move upon viral and host cell fusion (Figure 2b). Secondly, in each of the other class I fusion GPs, the cleavage site, which releases the equivalent GP1 and GP2 termini from each other, is located more or less on the outside of the trimer. In contrast, the N-terminus of LASV GP2 is oriented towards the core of the trimer and lies at the threefold axis, while the LASV GP1 C terminus, once released from GP2, rotates 30 Å up towards the apex of the trimer and is buried in a hydrophobic pocket of the neighboring monomer [41,42••] (Figure 2a).
Figure 2.
The LASV GP trimer is unique amongst class I glycoproteins. Comparison of the LASV GP trimer to the trimeric structures of the class I glycoproteins from Ebola virus (PDB: 5JQ7), HIV (PDB: 4NCO), Coronavirus (PDB: 5I08), Influenza (PDB: 1RUZ) and Paramyxovirus F (PDB: 2B9B) are shown. For EBOV, HIV, Influenza and CoV, the GP1-equivalent subunit for each virus is colored dark blue and the GP2-equivalent subunit is colored cyan. The three-helix core of each viral glycoprotein and the equivalent region in LASV GP2 is colored yellow. Note: Paramyxoviruses such as PiV5 have two surface glycoproteins, of which F is responsible for fusion of viral and host cell membranes. The larger, carboxy-terminal domain, F1, is colored cyan and the smaller, N-terminal domain, F2, is colored dark blue. A three-helix bundle is formed by the HRB subdomain of F1 and is colored yellow. The C-termini and N-termini of each subunit (GP1 and GP2 equivalent for EBOV, HIV, Influenza and CoV and F1 and F2 for PiV 5) are shown as spheres and indicated by arrows. (b) Comparison between prefusion LASV GP2 and postfusion GP2 of LCMV (PDB: 3MKO), a close relative of LASV. In the prefusion conformation of LASV GP2, HR1 (yellow) is broken up into four segments (HR1a-d) and connected to HR2 through the T-loop (pink), which forms a β-sheet with β1 of GP1. In contrast, in the postfusion conformation of GP2, HR1 forms a single α helix while the T-loop forms an α helix. The relative locations of the viral membrane in the prefusion state and the fused viral and host cell membranes in the postfusion state are indicated. The fusion peptide residues were not included in the postfusion GP2 crystallization construct but would be embedded in the fused membranes.
The lack of a stabilizing three-helical core and the orientation of cleavage site to the interior of the trimer have implications for the design of immunogens with which to elicit an effective antibody response, as discussed in the section `Structure-based considerations for vaccine design’.
Structures of arenavirus GP1 subunits: a shared architecture for different outcomes
All arenavirus GP1 structures solved to date, whether solved alone [36,37•,38••,39]; bound to their cognate receptor [19] or to antibody [35,40]; or as part of a GPC protomeric complex [41,42••], share a common core comprised of a central β-sheet that sits atop a bed of helices and loops. Structures of the GP1–GP2 protomers of LCMV and LASV contain the full-length GP1 subunit, rather than an N-terminally truncated version. That N-terminal region forms a β-strand that extends down from the main body of GP1 to interact with two strands from GP2 and assemble a three-stranded, anti-parallel β-sheet. Underlying the β-sheet core are several α-helices that, in the prefusion LASV GPC complex, interact with its cognate GP2 subunit, as well as the GP1 and GP2 subunits in neighboring protomers of the trimer (Figure 1b).
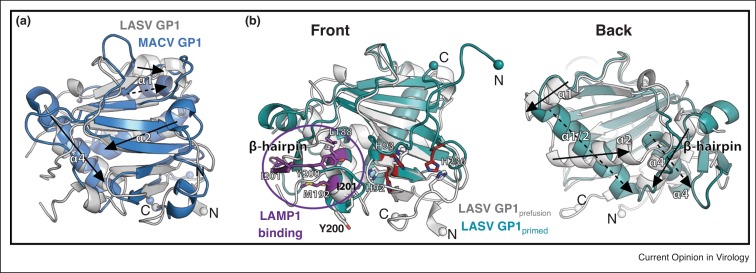
Structural overlay of the MACV [19,36], JUNV [35,40] and Whitewater Arroyo virus (WWAV, [39]) GP1 subunits with either of the GP1 subunits from the prefusion structure of LCMV [41] and LASV GPC [42••] reveals that the general architecture of the α-helices that lie underneath the conserved β-core is also highly similar (Figure 3 a) — despite the genetic and geographic divergence between New and Old world groups, and despite the fact that these New World structures were produced and solved as solitary GP1 subunits and that MACV GP1 was solved at low-pH.
Figure 3.
Comparison of arenavirus GP1 subunits. (a) Structural alignment of LASV GP1 (gray, PDB: 5VK2) and MACV GP1 (blue, PDB: 3KAS). Despite low sequence similarity of 20%, the GP1 subunits of LASV and MACV align with an r.m.s.d. of 2 Å. Major differences map to the loops that connect the β-sheet. For clarity, only the MACV GP1 subunit is shown; other New World arenavirus GP1 subunits align with similar r.m.s.d.s. (b) Overlay of the crystal structures of prefusion GP1, solved at neutral pH (gray, PDB: 5VK2), to the `primed’ GP1 subunit of LASV determined at pH 5 (cyan, PDB: 4ZJF). The histidine triad responsible for sensing pH [37•,43] is shown as ball and stick and is colored gray at neutral pH and red at pH 5. The LAMP1 binding site as it exists at pH 5 is colored purple [38••]. Structural elements of LASV GP1 that vary between the low-pH and neutral-pH forms are indicated. Spheres indicate the N-terminal and C-terminal residues visible in the low-pH GP1 structure and the location of the equivalent residues in the LASV GP trimer structure.
In contrast, aside from the conserved β-core, there are several significant structural differences between the conformation of LASV GP1 as it exists in the prefusion trimeric complex [42••] and the conformation of LASV GP1 solved as an isolated subunit at pH 5 [37•] (Figure 3b). Specifically, there are: Firstly, an elongation and rotation of α1 and α2 from two antiparallel helices in GP1 of the neutral-pH prefusion complex to a single helix in the low-pH GP1 monomer; secondly, rearrangement of residues 200–214 from a helix/loop structure in the prefusion complex to a two-stranded β-sheet, termed the β-hairpin, in the low-pH monomer; and finally, an ∼35 Å relocation of the N and C termini of GP1 from a more downward position in the trimer to a position situated above the β-core. Hence, LASV GP1 seems inherently more mobile or more flexible than the New World virus GP1s.
Conformational changes in GP2 are well known during fusion. These recent structural and biochemical data suggest that in additional to the known and well-characterized structural changes that occur in the GP2 subunit, there are also significant conformational changes that occur in GP1 during low pH-mediated LASV entry. The conformational switch in LASV GP1, from prefusion to a different conformation, perhaps a `primed’ conformation, is likely related to the receptor switching to LAMP1 that occurs in the endosome. Indeed, the repositioning of the N and C termini of GP1 results in the relocation of residues contained in the histidine triad identified by the Diskin group as a pH-sensor for LAMP1 switching [37•,38••,43] (Figure 3b). Further, the Diskin group also recently identified residues in the conformationally flexible β-hairpin as major determinants for LAMP1 binding [38••] (Figure 3b).
While a prefusion GP1–GP2 structure is not yet available for a New World arenavirus, the similarities between the LCMV and LASV GP1 when in their prefusion complex to the MACV, JUNV and WWAV when viewed as isolated GP1 subunits indicates that the New World arenaviruses may not undergo conformational changes in their GP1 subunits, and have only the one constant conformation. Indeed, the pathogenic New World arenaviruses are known to require only TfR1 and to not switch to another receptor in the endosome as does LASV.
The antigenic landscape of the prefusion LASV GP trimer
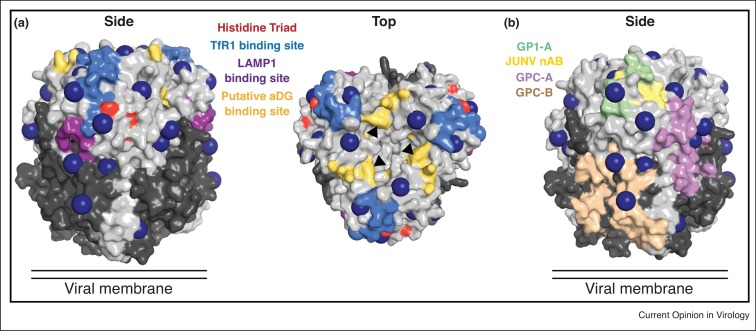
LASV GPC is a key therapeutic target, yet vaccine design efforts have been hindered by the substantial host-derived glycosylation that cloaks the virion surface. LASV GPC has eleven N-linked glycosylation sites on each monomer, which together comprise ∼25% of the total mass of the protein (Figure 4 a). This glycan shield leaves few regions vulnerable to antibody binding — specifically, the β-sheet face where LAMP-1 and the New World arenavirus receptor TfR1 bind [19,37•], the fusion peptide and fusion loop and HR2 of GP2, and across GPC protomers at the apex of the trimer. Indeed, a recent study by the Pinschewer group demonstrates that site-specific deletion of one or more of the glycosylation sites on the GP1 subunit of LASV and other arenaviruses enhances the neutralizing antibody response in mice infected with recombinant viruses [9•].
Figure 4.
Receptor binding and the antigenic landscape of GP. (a) Left: Side view of a surface representation of the LASV GP trimer is shown with N-glycosylation sites shown as blue spheres. The GP1 subunit is colored light gray and the GP2 subunit colored dark gray. The TfR1 binding site for pathogenic New World arenaviruses such as MACV and JUNV has been mapped onto the LASV GP structure and is colored light blue; the LAMP1 binding site (as it exists in the context of the trimer) is colored purple. Right: The top view of the trimer highlights residues involved in binding to the LASV and LCMV receptor αDG (yellow) [22, 23, 24,41,51]. Note that for LASV and LCMV GPC, not GP1 alone, is required for cell surface receptor binding [41,52]. Hence, a quaternary assembly of GP1, provided only in the context of the GPC, may be necessary for αDG engagement. (b) LASV neutralizing antibody epitopes are colored by epitope group: GP1-A, which recognizes the GP1 subunit alone is colored green; GPC-A, which recognizes a single prefusion GP monomer is colored purple; GPC-B, which recognizes a quaternary epitope that spans two GP monomers within the trimer is colored peach. Neutralizing antibodies against JUNV GP1 are colored yellow and partially overlap with those of the LASV GP1-A group.
Characterization of the neutralizing antibody response to LASV in humans suggests that the primary target for antibodies is prefusion GPC complex rather than either subunit alone [8•], with most neutralizing antibodies targeting a single epitope group, termed GPC-B. The precise epitope for one of the GPC-B antibodies was recently identified and spans two monomers within the trimer thus neutralizing virus by blocking conformational changes required for both LAMP1 engagement and fusion of host and virus membranes [42••] (Figure 4b).
The finding that most neutralizing antibodies target quaternary epitopes on LASV GPC which are only displayed in the context of the prefusion GPC trimer is in contrast to New World arenaviruses, such as Junin virus, for which the GP1 subunit alone is necessary and sufficient for binding by all neutralizing antibodies thus far characterized. All of these antibodies function to directly block binding to TfR1 [35,40,44,45] (Figure 4). Notably, as previously discussed, no evidence yet exists that New World arenaviruses employ receptor switching in the endosome nor does structural analysis of several New World GP1 subunits suggest that conformational changes occur upon exposure to low-pH or separation from GP2. Hence, the difference in epitope requirements for neutralizing antibodies may reflect the particular entry strategy employed by New World viruses versus LASV.
Structure-based considerations for vaccine design
One of the primary challenges facing the development of a LASV vaccine is how to elicit a sustained, neutralizing antibody response against the metastable glycoprotein. Surmounting data indicate that single subunit-based vaccines (such as with the GP1 subunit alone) may be unsuccessful and instead, vaccine design efforts may need to take into account the complex entry mechanism of LASV that relies on the multiple conformations of both the GP1 and GP2 subunits and the unique arrangement of the glycoprotein trimer. The multiple steps in entry and multiple forms of the LASV glycoprotein suggests that antibodies that target a single subunit conformation could be less effective. Indeed, the most potent antibodies are those that can stabilize the GPC protomer in a prefusion state [8•]. These antibodies prevent not only the conformational changes that occur in GP2, but also the appearance of a `primed’ GP1 [42••]. In contrast, antibodies that bind to the GP1 subunit only when it is in its prefusion conformation may lose their ability neutralize unless they are also able to prevent the appearance of primed GP1 during viral entry.
Further, of those antibodies that neutralize, the most protective are those that span across multiple GPC protomers rather than just a single monomer of GPC [8•,42••,46,47]. Hence, vaccines designed with the intent to elicit neutralizing antibodies, should focus on stabilizing both GP1 in its prefusion, unprimed state and GP2 in its prefusion, metastable state.
Engineered, soluble LASV GPC ecotodomains do not form trimers in solution [42••], which is perhaps not surprising as soluble LASV GPC lacks the trimer-stabilizing central three-helix bundle present in all other class I GPs. This reality, combined with the knowledge that the majority of the human neutralizing antibody response is against a quaternary epitope only displayed on prefusion GPC trimers, suggests that if a purified LASV GPC immunogen is to be used as a vaccine, it may need to be in a trimer-stabilized form, either through the use of exogenous trimerization domains or through enhancement of the trimeric interface through mutagenesis. Alternatively, VSV (or other recombinant virus platform)-based or DNA-based vaccines may see a boost in the neutralizing antibody response through the incorporation of protomer-stabilizing mutations such as those used to obtain the crystal structure.
Lastly, the requirement for GP1-GP2 processing for GPC trimerization due to the location of the termini on the interior of the trimer, particularly for the GP2 N-terminus, poses yet another consideration for vaccine design efforts. Strategies to mimic GP1–GP2 cleavage, such as through the introduction of variable length linkers as has been successful for HIV Env [48,49], may be unsuccessful for LASV, as these linkers will not fit in the interior cavity of the threefold axis and therefore would prevent the formation of native-like trimers.
For New World viruses, GP1-subunit based vaccines or vaccines that do not incorporate stabilized GPC may find more success, perhaps owing to their simpler single-receptor entry mechanism. The availability (and success) of an attenuated JUNV vaccine in Argentina [50] as well as the identification of only GP1-specific neutralizing antibodies lends credence to this. Regardless, it is possible that New World arenaviruses might also benefit from vaccination strategies that incorporate prefusion-stabilized GPC.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Acknowledgements
This work was supported by the National Institutes of Health grants U19AI10972 and R21AI116112. EOS is an Investigator in the Pathogenesis of Infectious Disease from the Burroughs Wellcome Fund. This is manuscript #29681 from The Scripps Research Institute.
References
- 1.Richmond J.K., Baglole D.J. Lassa fever: epidemiology, clinical features, and social consequences. BMJ. 2003;327:1271–1275. doi: 10.1136/bmj.327.7426.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oldstone M.B.A. Biology and pathogenesis of lymphocytic choriomeningitis virus infection. Arenaviruses II. Curr Top Microbiol Immunol. 2002;263:83–117. doi: 10.1007/978-3-642-56055-2_6. [DOI] [PubMed] [Google Scholar]
- 3.Briese T., Paweska J.T., McMullan L.K., Hutchison S.K., Street C., Palacios G., Khristova M.L., Weyer J., Swanepoel R., Egholm M. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS Pathog. 2009;5:e1000455. doi: 10.1371/journal.ppat.1000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patterson M., Grant A., Paessler S. Epidemiology and pathogenesis of Bolivian hemorrhagic fever. Curr Opin Virol. 2014;5:82–90. doi: 10.1016/j.coviro.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia J.B., Morzunov S.P., Levis S., Rowe J., Calderon G., Enria D., Sabattini M., Buchmeier M.J., Bowen M.D., St Jeor S.C. Genetic diversity of the Junin virus in Argentina: geographic and temporal patterns. Virology. 2000;272:127–136. doi: 10.1006/viro.2000.0345. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez J.P., Bowen M.D., Nichol S.T., Rico-Hesse R. Genetic characterization and phylogeny of Sabia virus, an emergent pathogen in Brazil. Virology. 1996;221:318–324. doi: 10.1006/viro.1996.0381. [DOI] [PubMed] [Google Scholar]
- 7.Tesh R.B., Jahrling P.B., Salas R., Shope R.E. Description of Guanarito virus (Arenaviridae: Arenavirus), the etiologic agent of Venezuelan hemorrhagic fever. Am J Trop Med Hyg. 1994;50:452–459. doi: 10.4269/ajtmh.1994.50.452. [DOI] [PubMed] [Google Scholar]
- 8•.Robinson J.E., KM Hastie, RW Cross, RE Yenni, DH Elliott, JA Rouelle, CB Kannadka, AA Smira, CE Garry, Bradley B.T. Most neutralizing human monoclonal antibodies target novel epitopes requiring both Lassa virus glycoprotein subunits. Nat Commun. 2016;7:11544. doi: 10.1038/ncomms11544. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study characterizes the first panel of human antibodies against Lassa virus and determines that most neutralizing antibodies against Lassa virus recognize epitopes displayed only on the prefusion glycoprotein trimer
- 9•.Sommerstein R., Flatz L., Remy M.M., Malinge P., Magistrelli G., Fischer N., Sahin M., Bergthaler A., Igonet S., Ter Meulen J. Arenavirus glycan shield promotes neutralizing antibody evasion and protracted infection. PLoS Pathog. 2015;11:e1005276. doi: 10.1371/journal.ppat.1005276. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates the glycan shield which is a critical component of viral evasion of antibody neutralization
- 10.Eichler R., Lenz O., Strecker T., Garten W. Signal peptide of Lassa virus glycoprotein GP-C exhibits an unusual length. FEBS Lett. 2003;538:203–206. doi: 10.1016/s0014-5793(03)00160-1. [DOI] [PubMed] [Google Scholar]
- 11.Froeschke M., Basler M., Groettrup M., Dobberstein B. Long-lived signal peptide of lymphocytic choriomeningitis virus glycoprotein pGP-C. J Biol Chem. 2003;278:41914–41920. doi: 10.1074/jbc.M302343200. [DOI] [PubMed] [Google Scholar]
- 12.Kunz S., Edelmann K.H., de la Torre J.C., Gorney R., Oldstone M.B. Mechanisms for lymphocytic choriomeningitis virus glycoprotein cleavage, transport, and incorporation into virions. Virology. 2003;314:168–178. doi: 10.1016/s0042-6822(03)00421-5. [DOI] [PubMed] [Google Scholar]
- 13.Saunders A.A., Ting J.P., Meisner J., Neuman B.W., Perez M., de la Torre J.C., Buchmeier M.J. Mapping the landscape of the lymphocytic choriomeningitis virus stable signal peptide reveals novel functional domains. J Virol. 2007;81:5649–5657. doi: 10.1128/JVI.02759-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schrempf S., Froeschke M., Giroglou T., von Laer D., Dobberstein B. Signal peptide requirements for lymphocytic choriomeningitis virus glycoprotein C maturation and virus infectivity. J Virol. 2007;81:12515–12524. doi: 10.1128/JVI.01481-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.York J., Nunberg J.H. Role of the stable signal peptide of Junin arenavirus envelope glycoprotein in pH-dependent membrane fusion. J Virol. 2006;80:7775–7780. doi: 10.1128/JVI.00642-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.York J., Nunberg J.H. Distinct requirements for signal peptidase processing and function in the stable signal peptide subunit of the Junin virus envelope glycoprotein. Virology. 2007;359:72–81. doi: 10.1016/j.virol.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 17.York J., Nunberg J.H. Intersubunit interactions modulate pH-induced activation of membrane fusion by the Junin virus envelope glycoprotein GPC. J Virol. 2009;83:4121–4126. doi: 10.1128/JVI.02410-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.York J., Romanowski V., Lu M., Nunberg J.H. The signal peptide of the Junin arenavirus envelope glycoprotein is myristoylated and forms an essential subunit of the mature G1-G2 complex. J Virol. 2004;78:10783–10792. doi: 10.1128/JVI.78.19.10783-10792.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abraham J., Corbett K.D., Farzan M., Choe H., Harrison S.C. Structural basis for receptor recognition by New World hemorrhagic fever arenaviruses. Nat Struct Mol Biol. 2010;17:438–444. doi: 10.1038/nsmb.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burns J.W., Buchmeier M.J. Protein–protein interactions in lymphocytic choriomeningitis virus. Virology. 1991;183:620–629. doi: 10.1016/0042-6822(91)90991-j. [DOI] [PubMed] [Google Scholar]
- 21.Radoshitzky S.R., Abraham J., Spiropoulou C.F., Kuhn J.H., Nguyen D., Li W., Nagel J., Schmidt P.J., Nunberg J.H., Andrews N.C. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature. 2007;446:92–96. doi: 10.1038/nature05539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smelt S.C., Borrow P., Kunz S., Cao W., Tishon A., Lewicki H., Campbell K.P., Oldstone M.B. Differences in affinity of binding of lymphocytic choriomeningitis virus strains to the cellular receptor alpha-dystroglycan correlate with viral tropism and disease kinetics. J Virol. 2001;75:448–457. doi: 10.1128/JVI.75.1.448-457.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan B.M., Emonet S.F., Welch M.J., Lee A.M., Campbell K.P., de la Torre J.C., Oldstone M.B. Point mutation in the glycoprotein of lymphocytic choriomeningitis virus is necessary for receptor binding, dendritic cell infection, and long-term persistence. Proc Natl Acad Sci U S A. 2011;108:2969–2974. doi: 10.1073/pnas.1019304108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teng M.N., Borrow P., Oldstone M.B., de la Torre J.C. A single amino acid change in the glycoprotein of lymphocytic choriomeningitis virus is associated with the ability to cause growth hormone deficiency syndrome. J Virol. 1996;70:8438–8443. doi: 10.1128/jvi.70.12.8438-8443.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin V.K., Droniou-Bonzom M.E., Reignier T., Oldenburg J.E., Cox A.U., Cannon P.M. Investigation of clade B New World arenavirus tropism by using chimeric GP1 proteins. J Virol. 2010;84:1176–1182. doi: 10.1128/JVI.01625-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eschli B., Quirin K., Wepf A., Weber J., Zinkernagel R., Hengartner H. Identification of an N-terminal trimeric coiled-coil core within arenavirus glycoprotein 2 permits assignment to class I viral fusion proteins. J Virol. 2006;80:5897–5907. doi: 10.1128/JVI.00008-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Igonet S., Vaney M.C., Vonhrein C., Bricogne G., Stura E.A., Hengartner H., Eschli B., Rey F.A. X-ray structure of the arenavirus glycoprotein GP2 in its postfusion hairpin conformation. Proc Natl Acad Sci U S A. 2011;108:19967–19972. doi: 10.1073/pnas.1108910108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parsy M.L., Harlos K., Huiskonen J.T., Bowden T.A. Crystal structure of Venezuelan hemorrhagic fever virus fusion glycoprotein reveals a class 1 postfusion architecture with extensive glycosylation. J Virol. 2013;87:13070–13075. doi: 10.1128/JVI.02298-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao W., Henry M.D., Borrow P., Yamada H., Elder J.H., Ravkov E.V., Nichol S.T., Compans R.W., Campbell K.P., Oldstone M.B. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science. 1998;282:2079–2081. doi: 10.1126/science.282.5396.2079. [DOI] [PubMed] [Google Scholar]
- 30.Inamori K., Yoshida-Moriguchi T., Hara Y., Anderson M.E., Yu L., Campbell K.P. Dystroglycan function requires xylosyl- and glucuronyltransferase activities of LARGE. Science. 2012;335:93–96. doi: 10.1126/science.1214115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshida-Moriguchi T., Campbell K.P. Matriglycan: a novel polysaccharide that links dystroglycan to the basement membrane. Glycobiology. 2015;25:702–713. doi: 10.1093/glycob/cwv021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raaben M., Jae L.T., Herbert A.S., Kuehne A.I., Stubbs S.H., Chou Y.Y., Blomen V.A., Kirchhausen T., Dye J.M., Brummelkamp T.R. NRP2 and CD63 are host factors for Lujo virus cell entry. Cell Host Microbe. 2017;22:688–696. doi: 10.1016/j.chom.2017.10.002. e685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33••.Li S., Sun Z., Pryce R., Parsy M.L., Fehling S.K., Schlie K., Siebert C.A., Garten W., Bowden T.A., Strecker T. Acidic pH-induced conformations and LAMP1 binding of the Lassa virus glycoprotein spike. PLoS Pathog. 2016;12:e1005418. doi: 10.1371/journal.ppat.1005418. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study presents the tomographic reconstructions of bona fide Lassa virus at neutral and virus-like particles acidic pH, which reveal the conformational changes that occur in the glycoprotein spike upon acidification
- 34.Briknarova K., Thomas C.J., York J., Nunberg J.H. Structure of a zinc-binding domain in the Junin virus envelope glycoprotein. J Biol Chem. 2011;286:1528–1536. doi: 10.1074/jbc.M110.166025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeltina A., Krumm S.A., Sahin M., Struwe W.B., Harlos K., Nunberg J.H., Crispin M., Pinschewer D.D., Doores K.J., Bowden T.A. Convergent immunological solutions to Argentine hemorrhagic fever virus neutralization. Proc Natl Acad Sci U S A. 2017;114:7031–7036. doi: 10.1073/pnas.1702127114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bowden T.A., Crispin M., Graham S.C., Harvey D.J., Grimes J.M., Jones E.Y., Stuart D.I. Unusual molecular architecture of the Machupo virus attachment glycoprotein. J Virol. 2009;83:8259–8265. doi: 10.1128/JVI.00761-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37•.Cohen-Dvashi H., Cohen N., Israeli H., Diskin R. Molecular mechanism for LAMP1 recognition by Lassa virus. J Virol. 2015;89:7584–7592. doi: 10.1128/JVI.00651-15. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes the structure of the GP1 subunit of Lassa virus at low pH and provides a basis for the unexpected conformational changes that occur in the GP1 subunit during Lassa virus infection
- 38••.Israeli H., Cohen-Dvashi H., Shulman A., Shimon A., Diskin R. Mapping of the Lassa virus LAMP1 binding site reveals unique determinants not shared by other old world arenaviruses. PLoS Pathog. 2017;13:e1006337. doi: 10.1371/journal.ppat.1006337. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study idenfies the LAMP1 binding site through comparative structural analysis of the receptor-binding subunits of the LAMP1-dependent Lassa virus and the LAMP1-independent Morogoro virus
- 39.Shimon A., Shani O., Diskin R. Structural basis for receptor selectivity by the Whitewater Arroyo Mammarenavirus. J Mol Biol. 2017;429:2825–2839. doi: 10.1016/j.jmb.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 40.Mahmutovic S., Clark L., Levis S.C., Briggiler A.M., Enria D.A., Harrison S.C., Abraham J. molecular basis for antibody-mediated neutralization of New World hemorrhagic fever Mammarenaviruses. Cell Host Microbe. 2015;18:705–713. doi: 10.1016/j.chom.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hastie K.M., Igonet S., Sullivan B.M., Legrand P., Zandonatti M.A., Robinson J.E., Garry R.F., Rey F.A., Oldstone M.B., Saphire E.O. Crystal structure of the prefusion surface glycoprotein of the prototypic arenavirus LCMV. Nat Struct Mol Biol. 2016;23:513–521. doi: 10.1038/nsmb.3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42••.Hastie K.M., Zandonatti M.A., Kleinfelter L.M., Heinrich M.L., Rowland M.M., Chandran K., Branco L.M., Robinson J.E., Garry R.F., Saphire E.O. Structural basis for antibody-mediated neutralization of Lassa virus. Science. 2017;356:923–928. doi: 10.1126/science.aam7260. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes the structure of the prefusion Lassa virus glycoprotien trimer bound to a human neutralizing antibody that bridges the glycoprotein trimer
- 43.Cohen-Dvashi H., Israeli H., Shani O., Katz A., Diskin R. The role of LAMP1 binding and pH sensing by the spike complex of Lassa virus. J Virol. 2016 doi: 10.1128/JVI.01624-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sanchez A., Pifat D.Y., Kenyon R.H., Peters C.J., McCormick J.B., Kiley M.P. Junin virus monoclonal antibodies: characterization and cross-reactivity with other arenaviruses. J Gen Virol. 1989;70(Pt 5):1125–1132. doi: 10.1099/0022-1317-70-5-1125. [DOI] [PubMed] [Google Scholar]
- 45.Zeitlin L., Geisbert J.B., Deer D.J., Fenton K.A., Bohorov O., Bohorova N., Goodman C., Kim D., Hiatt A., Pauly M.H. Monoclonal antibody therapy for Junin virus infection. Proc Natl Acad Sci U S A. 2016;113:4458–4463. doi: 10.1073/pnas.1600996113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cross R.W., Mire C.E., Branco L.M., Geisbert J.B., Rowland M.M., Heinrich M.L., Goba A., Momoh M., Grant D.S., Fullah M. Treatment of Lassa virus infection in outbred guinea pigs with first-in-class human monoclonal antibodies. Antiviral Res. 2016;133:218–222. doi: 10.1016/j.antiviral.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mire C.E., Cross R.W., Geisbert J.B., Borisevich V., Agans K.N., Deer D.J., Heinrich M.L., Rowland M.M., Goba A., Momoh M. Human-monoclonal-antibody therapy protects nonhuman primates against advanced Lassa fever. Nat Med. 2017 doi: 10.1038/nm.4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kovacs J.M., Noeldeke E., Ha H.J., Peng H., Rits-Volloch S., Harrison S.C., Chen B. Stable, uncleaved HIV-1 envelope glycoprotein gp140 forms a tightly folded trimer with a native-like structure. Proc Natl Acad Sci U S A. 2014;111:18542–18547. doi: 10.1073/pnas.1422269112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sharma S.K., de Val N., Bale S., Guenaga J., Tran K., Feng Y., Dubrovskaya V., Ward A.B., Wyatt R.T. Cleavage-independent HIV-1 Env trimers engineered as soluble native spike mimetics for vaccine design. Cell Rep. 2015;11:539–550. doi: 10.1016/j.celrep.2015.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maiztegui J.I., McKee K.T., Jr., Barrera Oro J.G., Harrison L.H., Gibbs P.H., Feuillade M.R., Enria D.A., Briggiler A.M., Levis S.C., Ambrosio A.M. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J Infect Dis. 1998;177:277–283. doi: 10.1086/514211. [DOI] [PubMed] [Google Scholar]
- 51.Sevilla N., Kunz S., Holz A., Lewicki H., Homann D., Yamada H., Campbell K.P., de La Torre J.C., Oldstone M.B. Immunosuppression and resultant viral persistence by specific viral targeting of dendritic cells. J Exp Med. 2000;192:1249–1260. doi: 10.1084/jem.192.9.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jae L.T.R.M., Herbert A.S., Kuehne A.I., Wirchnianski A.S., Soh T.K., Stubbs S.H., Janssen H., Damme M., Saftig P., Whelan S.P., Dye J.M., Brummelkamp T.R. Lassa virus entry requires a trigger-induced receptor switch. Science. 2014;344:1506–1510. doi: 10.1126/science.1252480. [DOI] [PMC free article] [PubMed] [Google Scholar]