Abstract
Background
Individuals born extremely preterm are exposed to significant perinatal stresses that are associated with an increased risk of psychopathology. However, a paucity of longitudinal studies has prevented the empirical examination of long-term, dynamic effects of perinatal adversity on mental health. Here, internalizing and externalizing problems from adolescence through adulthood were compared in individuals born at extremely low birth weight (ELBW; <1000 g) and normal birth weight (NBW; >2500 g).
Methods
Internalizing and externalizing data were collected over 20 years in three waves, during adolescence, young adulthood, and adulthood. Growth models were used to compare longitudinal trajectories in a geographically-based sample of 151 ELBW survivors and 137 NBW control participants born between 1977 and 1982 matched for age, sex, and socioeconomic status at age 8.
Results
After adjusting for sex, immigrant and socioeconomic status, and family functioning, ELBW survivors failed to show the normative, age-related decline in internalizing problems over time relative to their NBW peers (β = 0.21; p<.01). Both groups exhibited small declines in externalizing problems over the same period. Self-esteem (but not physical health, IQ, or maternal mood) partially mediated the association between ELBW status and internalizing problems.
Conclusions
ELBW survivors experienced a blunting of the expected improvement in depression and anxiety from adolescence to adulthood. These findings suggest that altered physiological regulatory systems supporting emotional and cognitive processing may contribute to the maintenance of internalizing problems in this population.
Keywords: extremely low birth weight, internalizing disorder, adolescent, adult, longitudinal studies
Introduction
Just over 11% of all infants born world-wide in 2010 were preterm, (Blencowe et al., 2013), with risks of almost 10% in the United States (2015; Purisch & Gyamfi-Bannerman, 2017) and nearly 8% in Canada (2013; Statistics Canada, 2016) and the United Kingdom (1996–2008; Zeitlin et al., 2013). The smallest and most vulnerable of these infants are born at extremely low birth weight (ELBW; <1000 g), and are exposed to significant prenatal (e.g., undernutrition, maternal stress) and postnatal stresses (e.g., life-saving neonatal intensive care procedures) that are associated with an increased risk of mental and physical morbidity (Behrman & Butler, 2007). Research suggests that ELBW survivors are at increased risk for mental health problems in childhood and adolescence, and that this risk may remain elevated in adulthood (Mathewson et al., 2017).
Our knowledge of the psychiatric sequelae of preterm birth comes almost exclusively from cross-sectional studies of individuals born in different countries and different eras, who experienced diverse risk and resilience exposures during development (e.g., healthcare, education systems). By their nature, cross-sectional studies cannot capture dynamic changes, nor identify the progression of disease states or their environmental influences. To analyze change over time, a longitudinal approach is required, especially if early experiences may set the stage for maladaptive development (e.g., Nelson, Bos, Gunnar, & Sonuga-Burke, 2011), or chronic health problems in adulthood (e.g., the developmental origins of health and disease [DOHaD], Gluckman, Hanson & Buklijas, 2010). To date, longitudinal studies of psychological functioning in individuals born extremely or very preterm are rare, and most examine changes over short periods (e.g., 2- to 6-years. For exceptions, see Jaekel, Baumann, Bartmann & Wolke, 2017, and Breeman, Baumann, Bartmann & Wolke, 2015).
Typically, both internalizing and externalizing problems increase in early adolescence (e.g., Costello, Egger & Angold 2005; Odgers et al., 2008), and then subside in adulthood (e.g., Galambos, Barker & Krahn 2006; Rawana & Morgan, 2014). Whether exposure to significant perinatal adversity influences these trajectories is unknown. Reports of ongoing cognitive (Breeman et al., 2015), social (Johnson & Marlow, 2014), and health problems (Hack et al., 2002) in adulthood suggest that ELBW survivors may not simply ‘grow out’ of any psychological problems they face in adolescence.
In this study, we compared the developmental trajectories of internalizing and externalizing problems from adolescence (ages 12–16) to young adulthood (ages 22–26) and adulthood (ages 30–35) in individuals born at ELBW and their normal birth weight (NBW) peers. We also sought to determine whether group differences were mediated by problems common to preterm survivors in childhood (e.g., depressed maternal mood; Vigod, Villegas, Dennis & Ross, 2010), adolescence (e.g., low self-esteem; Grunau, Whitfield & Fay, 2004), or adulthood (e.g., poor physical health; Hack et al., 2002), and lower general intelligence (Koenen et al., 2009). We predicted that individuals born ELBW would not show the age-typical declines associated with internalizing and externalizing problems by age 30–35, consistent with longstanding changes associated with perinatal adversity.
Method
Study Design
Data from the McMaster ELBW Cohort collected at adolescence, young adulthood, and adulthood were used to create growth models that illustrated trajectories of internalizing and externalizing psychopathology in ELBW survivors and NBW control participants.
Ethical Considerations
Ethical approval was obtained from the Hamilton Health Sciences Research Ethics Board, and all participants provided written informed consent.
Study Cohort
The ELBW sample originally consisted of 397 infants born between 1977 and 1982 to parents living in central-west Ontario, Canada (Saigal, Rosenbaum, Hattersley & Milner, 1989). They weighed 500–1000 g at birth and were born at 23–34 weeks gestational age. Of these, 179 (45%) survived to hospital discharge and 13 subsequently died, leaving 166 survivors. One hundred and forty-one ELBW survivors participated in the adolescent assessment (age 12–16), with 149 at the young adult assessment (age 22–26), and 100 at the adult assessment (age 30–35). Among ELBW participants, 26.8% (n=40) had significant neurosensory impairment (defined as cerebral palsy, blindness, deafness, and/or microcephaly diagnosed by a developmental paediatrician).
A group of 145 normal birth weight control participants was recruited when both birth weight groups were 8 years old. These children were randomly selected from local school boards and matched with ELBW survivors on age, sex, race, and familial socioeconomic status (SES; Saigal, Szatmari, Rosenbaum, Campbell, & King, 1991). Of NBW controls, 2.3% (n = 3) had neurosensory impairment. One hundred and twenty-three control participants completed the adolescent assessment, 133 the young adult assessment, and 89 the adult assessment. Together, 151 ELBW and 137 NBW participants provided at least one outcome and were eligible to be included in growth models (Table 1).
Table 1.
Sample Characteristics
| Full Sample (N = 288) | ELBW (n =151) | NBW (n =137) | t/chi2 (p-value) | |
|---|---|---|---|---|
| Birth Weight, g | 2056.89 (1323.37) | 841.42 (123.74) | 2296.56 (480.27) | 63.12 (<0.01) |
| Age | ||||
| Adolescence | 14.22 (1.49) | 13.98 (1.61) | 14.49 (1.29) | 2.82 (<0.01) |
| Young Adulthood | 23.42 (1.11) | 23.24 (1.15) | 23.62 (1.04) | 2.85 (<0.01) |
| Adulthood | 32.26 (1.55) | 32.06 (1.68) | 32.49 (1.37) | 1.93 (<0.06) |
| Male, n (%) | 130 (45.14) | 68 (45.03) | 62 (45.26) | 0.01 (0.97) |
| Maternal Education, y | 14.52 (2.59) | 14.29 (2.57) | 14.77 (2.60) | 1.52 (0.13) |
| Married Mother, n (%) | 247 (88.9) | 125 (88.7) | 122 (89.1) | 0.01 (0.92) |
| Immigrant Mother, n (%) | 76 (29.1) | 33 (23.9) | 43 (35.0) | 3.85 (<0.05) |
| Socioeconomic Status, age 8, n (%) | 5.82 (0.21) | |||
| I (highest) | 49 (18.4) | 25 (18.0) | 24 (18.8) | |
| II | 89 (33.3) | 42 (30.2) | 47 (36.7) | |
| III | 69 (25.8) | 42 (30.2) | 27 (21.1) | |
| IV | 40 (15.0) | 23 (16.6) | 17 (13.3) | |
| V | 20 (7.49) | 7 (5.0) | 13 (10.2) | |
| Family Functioning (FAD, adolescence) | 9.71 (5.17) | 9.51 (5.10) | 9.93 (5.24) | 0.65 (0.52) |
| Self-esteem (Z-scores) | ||||
| Adolescence | 0.00 (1.00) | 0.01 (1.00) | −0.01 (1.00) | 0.15 (0.88) |
| Young Adulthood | 0.00 (1.00) | −0.12 (1.02) | 0.13 (0.97) | 2.02 (<0.05) |
| Adulthood | 0.00 (1.00) | −0.18 (1.06) | 0.20 (0.89) | 2.65 (<0.01) |
| Maternal Depressed Mood | ||||
| Childhood (age 8) | 2.35 (1.70) | 2.35 (1.86) | 2.35 (1.53) | 0.00 (1.0) |
| Adolescence | 2.46 (1.75) | 2.46 (1.75) | 2.46 (1.77) | 0.00 (1.0) |
| Young Adulthood | 2.50 (1.70) | 2.57 (1.84) | 2.42 (1.54) | 0.74 (0.46) |
| Chronic Health Conditions, n (%) | ||||
| Adolescence | 187 (69.3) | 116 (81.1) | 71 (55.9) | 20.08 (<0.01) |
| Young Adulthood | 219 (79.4) | 127 (88.8) | 92 (69.2) | 16.22 (<0.01) |
| Adulthood | 140 (74.1) | 82 (82.0) | 58 (65.2) | 6.95 (<0.01) |
| No. of Chronic Conditions | ||||
| Adolescence | 1.48 (1.47) | 2.01 (1.63) | 0.89 (0.96) | 6.74 (<0.01) |
| Young Adulthood | 2.01 (1.79) | 2.43 (1.90) | 1.56 (1.54) | 4.16 (<0.01) |
| Adulthood | 2.06 (2.09) | 2.57 (2.34) | 1.49 (1.59) | 3.65 (<0.01) |
| Intelligence | ||||
| FSIQ | 97.97 (15.22) | 91.66 (15.38) | 104.13 (12.29) | 7.38 (<0.01) |
| Internalizing Problems | ||||
| Adolescence | 10.83 (6.72) | 10.79 (7.30) | 10.88 (6.02) | 0.10 (0.92) |
| Young Adulthood | 10.30 (7.94) | 11.58 (8.78) | 8.93 (6.72) | 2.79 (<0.01) |
| Adulthood | 10.30 (8.07) | 11.91 (8.56) | 8.49 (7.11) | 2.96 (<0.01) |
| Externalizing Problems | ||||
| Adolescence | 4.09 (3.71) | 3.91 (3.86) | 4.30 (3.54) | 0.85 (0.40) |
| Young Adulthood | 2.35 (2.46) | 2.32 (2.57) | 2.39 (2.35) | 0.25 (0.80) |
| Adulthood | 1.84 (2.31) | 1.87 (2.38) | 1.80 (2.25) | 0.21 (0.83) |
Notes: Data are reported as mean (SD), unless indicated otherwise.
FAD, McMaster Family Assessment Device.
FSIQ, Wechsler Full-Scale IQ.
Sample sizes given reflect the number of participants who provided at least one outcome datum for trajectory modelling, (i.e., completed at least one internalizing or externalizing measure).
Measures
Outcome Scales
Internalizing and externalizing problems in adolescence were self-reported using the Ontario Child Health Study-Revised (OCHS-R) scales (Boyle et al., 1993). These scales were derived from the original OCHS scales (Boyle et al., 1987), and the Child Behavior Checklist, (CBCL, Achenbach & Edelbrock, 1981). Young adult and adult participants completed the Young Adult Self-Report (YASR; Achenbach, 1997). The Achenbach scales are comparable across development (from childhood to adulthood), and the high degree of overlap between the OCHS-R and YASR makes them ideal for longitudinal study. Items from all scales asked about functioning over the previous 6 months. Responses were scored 0, (not true or never true), 1, (somewhat or sometimes true), or 2, (very true or often true). Self-reported responses for 48 identical items were available from all three assessments.
Subscale Development
These 48 items were divided (by authors RVL and LAS) into 2 broad syndrome scales related to internalizing (21 items, 13 representing depression and 8 anxiety), and externalizing (13 items, 10 representing conduct and 3 oppositional problems) psychopathology, which were confirmed by factor analysis. Internalizing (Kendler, Prescott, Myers, & Neale, 2003) and externalizing (Krueger & South, 2009) constructs have been well-validated in adult samples. The remaining 14 items were not used.
Our internalizing scale reflected seven of nine DSM-5 criteria for major depressive disorder, and six symptoms of generalized and social anxiety. The 13 externalizing items tapped aggression (4 items), destructiveness (3), deceitfulness/theft (3), and oppositionality (3).
Both scales exhibited concurrent validity with full YASR empirical and DSM scales at the 22–26 (internalizing (rs >.94); externalizing (rs >.90)) and 30–35-year (internalizing (rs >.94); externalizing (rs >.90)) assessments and showed good reliability (Cronbach’s alpha=0.88–0.92 for internalizing and 0.72–0.82 for externalizing). Assumptions of linearity, normality, and homoscedasticity of the outcome variables used in the trajectory analysis were satisfied. (See online Table S1 and Figures S1 and S2).
Covariates
We aimed to isolate perinatal effects on psychopathology risk by adjusting for sex, parental immigrant status, familial SES, and family functioning, factors linked to preterm birth and later psychopathology. Levels of internalizing and externalizing problems are known to differ by sex (Nolen-Hoeksema, 2012). Higher risks for poor mental health in immigrant mothers (Vang, Sigouin, Flenon & Gagnon, 2015), may adversely affect their offspring (Pearson et al., 2013). Socioeconomic disadvantage, measured using the Hollingshead 2-factor index at age 8 (Hollingshead, 1969), can also increase risk (Jefferis, Power, & Hertzman, 2002). Poor family functioning has previously been linked to psychological problems (Sourander et al., 2006).
Problems in family functioning were assessed at age 8 using the McMaster Family Assessment Device (Epstein, Baldwin, & Bishop., 1983), a twelve-item scale indexing six dimensions of family life (e.g. problem solving, communication, etc.) on a four-point scale ranging from 1 to 4. Higher scores indicated worse family functioning.
Analyses were not adjusted for differential effects of neurosensory impairment, because this factor was collinear with birth weight status.
Mediators
Four mediators were tested for associations with birth weight status and psychopathology risk. Self-esteem was assessed at the adolescent, young adult, and adult assessments, using the 5-item Global Self-Worth subscale of the Harter Self-Perception Profile for Adolescents (1988), the 10-item Rosenberg Self-Esteem Scale (Rosenberg, 1965), and the 25-item Coopersmith Self-Esteem Inventory (Johnson, Redfield, Miller, & Simpson, 1983), respectively. All showed good internal consistency in our sample (α=0.89–0.92). Scale scores from the three assessments were normalized (Z-scored) before entry in analyses.
Maternal depressed mood was assessed at the childhood, adolescent, and young adult interviews using the 5-item negative mood index of the Bradburn Affect Balance Scale (Bradburn, 1969). Higher scores indicated greater negative affect. Internal consistency (α=0.58–0.67) was comparable to previous reports (Larsen, Diener, & Emmons, 1985).
Counts of current physical health problems were self-reported at each wave and may be considered reliable if they are current rather than retrospective (Baumeister, Kriston, Bengel, & Härter, 2010).
Finally, the full-scale IQ score from the Wechsler Intelligence Scale for Children, Revised (WISC-R; Wechsler, 1974) at age 8 (Saigal et al., 1991) defined intellectual ability.
Statistical Analysis
Bivariable analyses (t-tests and χ2 tests) were used to compare characteristics between birth weight groups. Trajectories of internalizing and externalizing in each group were estimated using multilevel modeling (Singer & Willett, 2003). Our data were structured as a 2-level hierarchy, with individual outcomes at each age (Level 1), nested within individual participants (Level 2). These analyses yield effects represented by baseline values (intercepts) and change in outcomes over time (slopes).
For each outcome, we first specified an unadjusted model, containing birth weight status (to test for group differences in internalizing or externalizing), time (participant age), and their interaction (to test for associations of birth weight status with symptom change over time (slope)). In adjusted models, we controlled for effects of sex, immigrant status, SES, and family functioning. Predictors were grand-mean centered at the adult assessment.
In subsequent analyses, potential mediating effects of self-esteem, maternal depressed mood, physical health problems, and IQ were investigated within the multilevel model framework using the product of coefficients and 95% confidence intervals (MacKinnon & Luecken, 2008). Separate models determined whether self-esteem, maternal depression, physical health, or IQ mediated longitudinal associations between birth weight status and internalizing or externalizing. Data from all three occasions were used for all mediators except IQ (measured only at 8 years). The statistical significance of mediators was determined using the Sobel test (Sobel, 1982). Hypothesis tests were two-sided with α=0.05. Trajectories and mediating effects were calculated using SAS 9.2 (SAS Institute Inc.) and measurement invariance with Mplus 6.11 (Muthén & Muthén).
Measurement invariance of outcome scales
Despite differences between preterm and term survivors, measurement invariance is rarely examined in studies comparing these groups (Van Lieshout, Boyle, Schmidt, Saigal, & Ferro 2015). Here, we established measurement invariance between ELBW and NBW groups for internalizing and externalizing scales using the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). Adequate model fit was defined using CFI>0.95 and RMSEA<0.06 (Cheung & Rensvold, 2002). Invariance was present if the difference in model fit between more versus less constrained models met the following thresholds: CFI difference ≤0.010 or RMSEA difference ≥0.015 (Chen, 2007). Similarly, measurement invariance was examined across developmental periods using strict models with factor loadings, item thresholds and items residuals constrained across all three groups.
Results
Sample characteristics are shown in Table 1. The mean age (SD) of individuals at each assessment was 14.2 (1.5), 23.4 (1.1), and 32.3 (1.6) years, and males comprised 45%, 45%, and 39% of the sample at each assessment, respectively. Although chronic physical conditions increased over time in both groups, the number was higher among ELBW survivors (ps<.001) at each assessment. The overall difference in the age distribution between groups was small (<6 months) but statistically significant.
Female sex (OR=0.40, p<.001, 95% CI = 0.25–0.65), higher IQ (OR=0.97, p<.002, 95% CI=0.96–0.99), and less maternal depression (OR=1.17, p<.04, 95% CI=1.01–1.35) were predictors of complete data. (See online Table S2).
Model fit across birth weight groups was adequate for both scales (Internalizing: CFI=0.950; Externalizing: CFI=0.999) and both were measurement invariant (Internalizing, factor loadings: ΔCFI=0.008; item residuals: ΔCFI=0.008; Externalizing, factor loadings: ΔCFI=0.001; item residuals: ΔCFI=0.002). Acceptable model fit across developmental periods provided indirect evidence of measurement invariance across age groups (Internalizing: CFI=0.953; Externalizing: CFI=0.972). (See online Table S3).
At the adolescent visit, the proportions of those with clinically-relevant scores (at the 80th percentile or higher) for internalizing (ELBW: 19.6%; NBW: 20.8%) and externalizing (ELBW: 20.3%; NBW: 23.3%) did not differ between groups, χ2<1.0, ps>.55. Given that these problems are known to increase during adolescence even in typically-developing populations (e.g., Costello et al., 2005), these results are not unexpected. However, at the young adult visit, the proportion of ELBW survivors (25.4%) with internalizing scores at the 80th percentile or higher was marginally higher than for NBW controls (17.3%), χ2=2.65, p=.10, and at the adult visit, significantly more ELBW survivors (28.0%) than NBW controls (13.5%) still had internalizing scores at the 80th percentile or higher, χ2=5.95, p<.02.
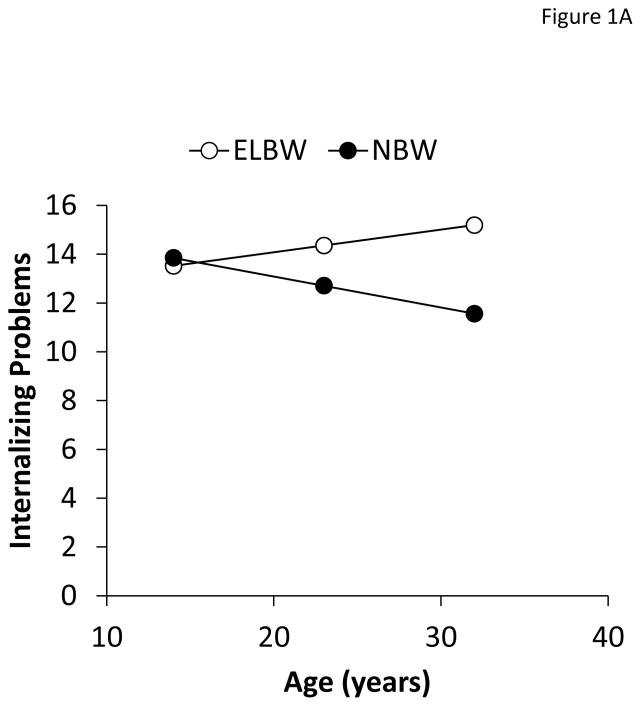
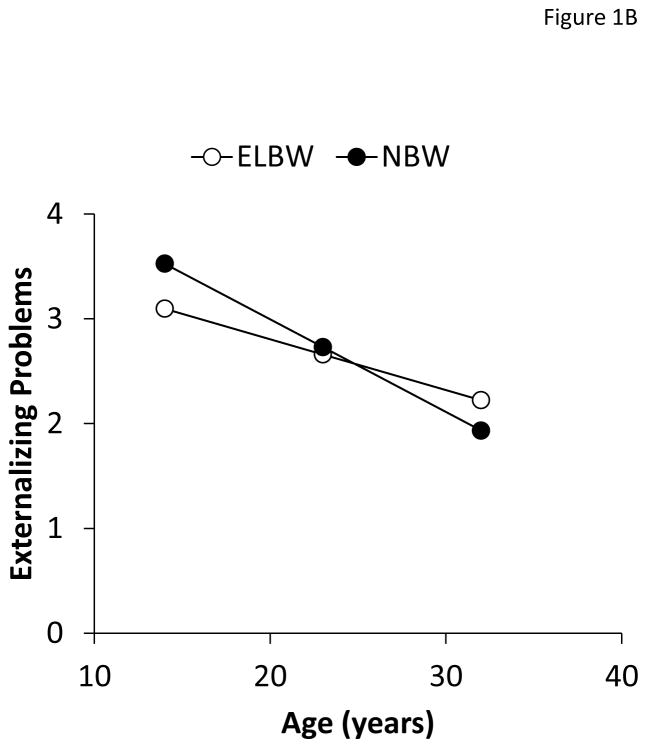
Multilevel analyses are shown in Table 2 and group trajectories in Figures 1A and 1B. After adjustment for sex, immigrant status, SES, and family functioning, ELBW status was associated with more internalizing difficulties, β=3.63 (1.17), p<.01, and an increase over time relative to NBW controls’ decline, resulting in a significant interaction (β=0.22 (0.07), p<.01).
Table 2.
Multilevel Models of Internalizing and Externalizing Problems
| Internalizing | Externalizing | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Fixed Effects | ||||
| Final Status | ||||
| Intercept | 8.03 (0.78)*** | 7.80 (0.83)*** | 1.61 (0.22)*** | 1.37 (0.23)*** |
| ELBW | 3.58 (1.08)** | 3.63 (1.17)** | 0.03 (0.31) | 0.29 (0.32) |
| Sex | 1.76 (1.18) | −0.30 (0.33) | ||
| SES | −0.28 (0.52) | −0.06 (0.14) | ||
| Immigrant | 0.30 (1.29) | 0.35 (0.35) | ||
| FAD | 0.15 (0.12) | 0.08 (0.03)* | ||
| Rate of Change | ||||
| Age (slope) | −0.15 (0.05)** | −0.18 (0.05)*** | −0.15 (0.02)*** | −0.15 (0.02)*** |
| ELBW x Age | 0.18 (0.07)** | 0.22 (0.07)** | 0.03 (0.03) | 0.04 (0.03) |
| Sex x Age | −0.01 (0.07) | 0.06 (0.03)* | ||
| SES x Age | −0.02 (0.03) | −0.01 (0.01) | ||
| Immigrant x Age | 0.07 (0.07) | 0.02 (0.03) | ||
| FAD x Age | 0.00 (0.01) | 0.00 (0.00) | ||
| Variance Components | ||||
| Intra-individual | 25.92 (2.62)*** | 25.59 (2.68)*** | 4.83 (0.46)*** | 5.12 (0.51)*** |
| Intercept | 45.68 (7.29)*** | 45.22 (7.68)*** | 1.20 (0.65)* | 0.35 (0.63) |
| Slope | 0.06 (0.03)* | 0.06 (0.03)* | 0.01 (0.01) | 0.00 (0.01) |
| Goodness-of-Fit | ||||
| −2LL | 4777.3 | 4140.0 | 3482.4 | 2995.7 |
| BIC | 4822.9 | 4227.4 | 3528.0 | 3083.1 |
Notes: FAD, McMaster Family Assessment Device.
Variables included in the model were grand-mean centered at the adult assessment.
p<.05,
p<.01,
p<.001
Figure 1.
Change trajectories for A) internalizing and B) externalizing problems between adolescence and adulthood in ELBW survivors and NBW controls.
Note: Mean age differed between consecutive assessments by 9 years in each case (adolescent to young adult, young adult to adult).
Externalizing problems declined over time, β=−0.15 (0.02), p<.001, but this did not differ by birth weight.
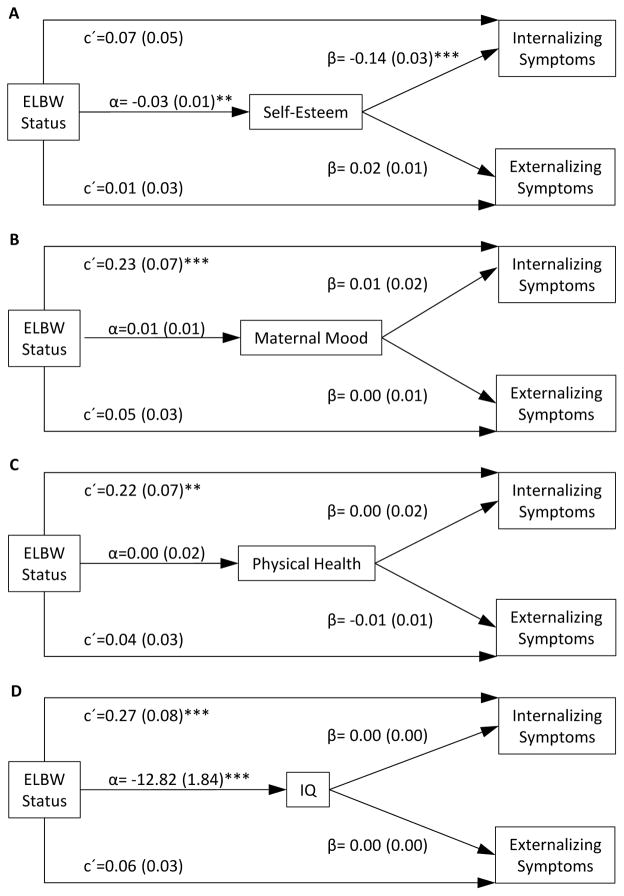
Self-esteem partially mediated the association between ELBW status and internalizing problems, αβ=0.004 (0.00), p<.05, accounting for 5.1% of the variance (Figure 2). Maternal depression, physical health problems, and intelligence did not mediate the association between ELBW status and internalizing. None was a significant mediator of externalizing problems, ps>.05.
Figure 2.
Mediation of associations between birth weight status and internalizing by self-esteem, maternal depressed mood, physical health, and intellectual functioning.
Discussion
The normative, age-related decline in depression and anxiety between adolescence and adulthood was absent in adults born at ELBW: whereas adolescent internalizing problems decreased over time in NBW control participants, internalizing psychopathology in the ELBW group remained high and virtually unchanged for two decades. This pattern did not appear to be accounted for by potential confounders, nor was it mediated by maternal depressed mood, health problems, or IQ. The results suggested that ELBW survivors may not simply grow out of the internalizing difficulties they face in adolescence but continue to struggle with these problems through their thirties. Conversely, both groups showed a modest decline in externalizing problems over time.
These are important findings for ELBW survivors, their families, and healthcare providers. Processes that exacerbate and prolong negative emotions (e.g., rumination) may simply not diminish with maturity to the same degree in ELBW survivors, resulting in higher levels of mood and anxiety problems than in general adult population samples. In addition, personality-related differences in the perception, interpretation, and reaction to acute and chronic environmental stress may contribute to psychopathology in adults born at ELBW (e.g., Schmidt, Miskovic, Boyle, & Saigal 2008). Although our older cohort may be more vulnerable than cohorts born since the widespread adoption of significant advances in neonatal care (around 1990; Hack & Costello, 2008), effects of birth era on mental health outcomes may be minimal (Mathewson et al., 2017).
Alternatively, failure to experience the normative age-related decline in internalizing may be related to neurodevelopmental changes associated with premature birth (Volpe, 2009). Studies of adolescents and children born preterm have linked increased vulnerability to mental health problems such as internalizing and attention deficits to structural brain abnormalities (e.g., Skranes et al., 2007). Birth-related injuries in cerebral white matter tracts and periventricular regions during what would have been the third trimester of pregnancy may interfere with the exuberant neurodevelopment taking place during this period (Luciana, 2003; Volpe, 2009). While cerebral damage may be focal or diffuse, the imprecise nature of mental health problems is most consistent with diffuse damage or diminished connectivity among cortical and subcortical regions.
Fetal adaptation to adverse perinatal conditions may set the stage for maladaptive development (Nelson et al., 2011) or chronic health problems in adulthood (Gluckman et al., 2010). Adverse early exposures appear to establish a more “plastic” fetal state that increases the individual’s sensitivity to postnatal influences later in life (O’Donnell & Meaney, 2016). Human fetal regulatory systems may be particularly sensitive to conditions that promote the secretion of glucocorticoids, including maternal stress (e.g., Davis & Sandman, 2012), nutritional deprivation (e.g., Brown, van Os, Driessens, Hoek & Susser, 2000), and maternal infection (e.g., Bilbo & Schwartz, 2009). Prenatal exposure of the developing human brain to high levels of endogenous or exogenous glucocorticoids can influence activity of the HPA axis (Entringer, Kumsta, Hellhammer, Wadhwa, & Wüst, 2009; Grunau et al., 2007; Van den Bergh, 2011), the autonomic nervous system (Seckl & Meaney 2004), and the limbic and prefrontal neurocircuitry involved in emotional and cognitive coping (Jacobson & Sapolsky, 1991).
Our findings are consistent with the notion that being born at ELBW may delay or impede the normal resolution of anxiety and depression. However, they differ from those recently reported by Jaekel and colleagues (2017), which suggested no persistent risk of internalizing problems between childhood and young adulthood in individuals born at VLBW. Differences in cohort vulnerability (birthweights ≤1000 g versus ≤1500 g), or age of follow-up (to the mid-thirties versus mid-twenties) may partly account for the discrepant findings. Methodological and analytical differences may also explain significant variation in outcomes (Achenbach, Rescorla, & Ivanova, 2012), as we used a dimensional rather than categorical approach to the assessment of internalizing that may be particularly useful for measuring change in mental health trajectories over time (Sala, Granero, & Ezpeleta, 2005). Although the VLBW findings were not statistically robust, the direction of effects in both studies was the same.
Limitations
First, sample attrition over 30 years reduced our statistical power. However, adjusting the multilevel analyses performed here for variables predicting attrition may reduce its impact. Second, for reasons relating to scale selection in adolescence, we utilized subsets of items from better known rating scales (e.g., YASR). Nonetheless, each construct was assessed using identical indicators on three evenly-spaced measurement occasions, and established the reliability, validity, and measurement invariance of our scales. Third, internalizing and externalizing were assessed with respect to the preceding six-month period, rather than over years, which could produce temporal gaps not covered by our measures. Fourth, despite our efforts, unmeasured confounding variables (e.g., genetic differences) may contribute to the differential trajectories of internalizing psychopathology in ELBW survivors. Fifth, the modest internal consistency of the maternal depression scale may have affected our mediation finding for this outcome. We acknowledge that we will better understand the generalizability of our findings in this population as further mental health data become available.
Conclusions
Extreme prematurity appears to result in a persistent vulnerability that blunts the normal decline seen in internalizing problems from adolescence to adulthood. This vulnerability may have its origins in enduring physiological responses to perinatal exposures in key regulatory pathways, or in the neural circuitry involved in emotional and cognitive processing.
On a practical level, our results suggest that ELBW survivors continue to struggle with depression and anxiety into their thirties. The persistence of these problems highlights the need for ongoing awareness among survivors and their healthcare providers that early detection and intervention may be warranted, and that a continuity of care beyond the traditional pediatric period may be required to optimize mental health of this growing segment of the population.
Supplementary Material
Diagnostic Plots for Externalizing.
Table S1. Descriptive Statistics for the Internalizing and Externalizing Scales by Group.
Table S2. Characteristics Associated with Missing Data.
Table S3. Measurement Invariance of the Internalizing and Externalizing Scales across Birth Weight Groups and Developmental Periods.
Diagnostic Plots for Internalizing.
Key Points.
Longitudinal trajectories of internalizing problems between adolescence and adulthood are altered in those born at ELBW such that these individuals manifest a persisting vulnerability to depression and anxiety through the fourth decade of life.
By their mid-thirties, ELBW survivors fail to show the normative, age-related decline in internalizing problems between adolescence and adulthood, after adjusting for sex, immigrant and socioeconomic status, and family functioning.
Our findings illustrate the need for a continuity of care beyond the traditional pediatric period in this group.
Acknowledgments
This research was supported by grants from the Canadian Institutes of Health Research (CIHR) awarded to LS (CIHR Team Grant: TMH-103145) and the National Institute of Child Health and Human Development (NICHD: 1-R01HD40219) awarded to SS. RVL and MF had full access to all the data in the study and take responsibility for the integrity and accuracy of the data analysis. Study concept and design: RVL, MF. Acquisition, analysis, or interpretation of data: RVL, MF, LS, MB, KMM, KJM, SS. Statistical analysis: MF. Drafting of the manuscript: KJM, RVL, MF. Critical revision of the manuscript for intellectual content: All authors. Obtained funding: LS, SS. Administrative, technical, or material support: Lorraine Hoult, Barbara Stoskopf, Vivian Vaughan Williams. Data collection: Nicole Folland, Sue McKee, Jordana Waxman, Shirien Yunus. Supervision: LS, RVL, SS. The authors also wish to thank the many participants and their families for their continued participation in the study. Funding/Support: Conflict of Interest Disclosures: The authors have declared that have no competing or potential conflicts of interest.
Footnotes
Conflict of interest statement: No conflicts declared.
Additional Supporting Information may be found in the online version of this article
References
- Achenbach TM. Manual for YASR and YABCL. Burlington, Vermont: University of Vermont, Department of Psychiatry; 1997. [Google Scholar]
- Achenbach TM, Edelbrock CS. Behavioral problems and competencies reported by parents of normal and disturbed children aged 4 through 16. Monograph of the Society for Research in Child Development. 1981;46:1–78. [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA, Ivanova MY. International epidemiology of child and adolescent psychopathology I: diagnoses, dimensions, and conceptual issues. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(12):1261–1272. doi: 10.1016/j.jaac.2012.09.010. [DOI] [PubMed] [Google Scholar]
- Baumeister H, Kriston L, Bengel J, Härter M. High agreement of self-report and physician-diagnosed somatic conditions yields limited bias in examining mental-physical comorbidity. Journal of Clinical Epidemiology. 2010;63(5):558–565. doi: 10.1016/j.jclinepi.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. National Academies Press; 2007. [PubMed] [Google Scholar]
- Bilbo SD, Schwarz JM. Early-life programming of later-life brain and behavior: a critical role for the immune system. Frontiers in Behavioral Neuroscience. 2009;3(14):1–14. doi: 10.3389/neuro.08.014.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, … Lawn J. Born too soon: the global epidemiology of 15 million preterm births. Reproductive Health 2013. 2013;10(Suppl 1):S2. doi: 10.1186/1742-4755-10-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle MH, Offord DR, Hofmann HG, Catlin GP, Byles JA, Cadman DT, Crawford JW, Links PS, Rae-Grant NI, Szatmari P. Ontario Child Health Study: I. Methodology. Archives of General Psychiatry. 1987;44(9):826–831. doi: 10.1001/archpsyc.1987.01800210078012. [DOI] [PubMed] [Google Scholar]
- Boyle MH, Offord DR, Racine YA, Fleming JE, Szatmari P, Sanford MN. Evaluation of the revised Ontario Child Health Study Scales. Journal of Child Psychology and Psychiatry. 1993;34(2):189–213. doi: 10.1111/j.1469-7610.1993.tb00979.x. [DOI] [PubMed] [Google Scholar]
- Bradburn NM. The Structure of Psychological Well-being. Aldine; Chicago, III: 1969. [Google Scholar]
- Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Preterm cognitive function into adulthood. Pediatrics. 2015;136(3):415–423. doi: 10.1542/peds.2015-0608. [DOI] [PubMed] [Google Scholar]
- Brown AS, van Os J, Driessens C, Hoek HW, Susser ES. Further evidence of relation between prenatal famine and major affective disorder. American Journal of Psychiatry. 2000;157(2):190–195. doi: 10.1176/appi.ajp.157.2.190. [DOI] [PubMed] [Google Scholar]
- Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling. 2007;14(3):464–504. [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9(2):233–255. [Google Scholar]
- Costello EJ, Egger H, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(10):972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- Davis EP, Sandman CA. Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology. 2012;37(8):1224–1233. doi: 10.1016/j.psyneuen.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entringer S, Kumsta R, Hellhammer DH, Wadhwa PD, Wüst S. Prenatal exposure to maternal psychosocial stress and HPA axis regulation in young adults. Hormones and Behavior. 2009;55(2):292–298. doi: 10.1016/j.yhbeh.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9(2):171–180. [Google Scholar]
- Galambos NL, Barker ET, Krahn HJ. Depression, self-esteem, and anger in emerging adulthood: seven-year trajectories. Developmental Psychology. 2006;42(2):350–365. doi: 10.1037/0012-1649.42.2.350. [DOI] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA, Buklijas T. A conceptual framework for the developmental origins of health and disease. Journal of Developmental Origins of Health and Disease. 2010;1(1):6–18. doi: 10.1017/S2040174409990171. [DOI] [PubMed] [Google Scholar]
- Grunau RE, Haley DW, Whitfield MF, Weinberg J, Yu W, Thiessen P. Altered basal cortisol levels at 3, 6, 8 and 18 months in infants born at extremely low gestational age. Journal of Pediatrics. 2007;150(2):151–156. doi: 10.1016/j.jpeds.2006.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunau RE, Whitfield MF, Fay TB. Psychosocial and academic characteristics of extremely low birth weight (≤ 800 g) adolescents who are free of major impairment compared with term-born control subjects. Pediatrics. 2004;114(6):e725–e732. doi: 10.1542/peds.2004-0932. [DOI] [PubMed] [Google Scholar]
- Hack M, Costello DW. Trends in the rates of cerebral palsy associated with neonatal intensive care of preterm children. Clinical Obstetrics and Gynecology. 2008;51(4):763–774. doi: 10.1097/GRF.0b013e3181870922. [DOI] [PubMed] [Google Scholar]
- Hack M, Flannery DJ, Schluchter M, Cartar L, Borawski E, Klein N. Outcomes in young adulthood for very-low-birth-weight infants. New England Journal of Medicine. 2002;346(3):149–157. doi: 10.1056/NEJMoa010856. [DOI] [PubMed] [Google Scholar]
- Harter S. Self-Perception Profile for Adolescents. Denver, CO: University of Denver Press; 1988. [Google Scholar]
- Hollingshead AB. Two-factor index of social position [mimeograph] New Haven, CT: Yale University; 1969. [Google Scholar]
- Jacobson L, Sapolsky R. The role of the hippocampus in feedback regulation of the hypothalamic-pituitary-adrenocortical axis. Endocrine Reviews. 1991;12(2):118–134. doi: 10.1210/edrv-12-2-118. [DOI] [PubMed] [Google Scholar]
- Jaekel J, Baumann N, Bartmann P, Wolke D. Mood and anxiety disorders in very preterm/very low–birth weight individuals from 6 to 26 years. Journal of Child Psychology and Psychiatry. 2017 doi: 10.1111/jcpp.12787. [DOI] [PubMed] [Google Scholar]
- Jefferis BJ, Power C, Hertzman C. Birth weight, childhood socioeconomic environment, and cognitive development in the 1958 British birth cohort study. British Medical Journal. 2002;325(7359):1–6. doi: 10.1136/bmj.325.7359.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BW, Redfield DL, Miller RL, Simpson RE. The Coopersmith self-esteem inventory: A construct validation study. Educational and Psychological Measurement. 1983;43(3):907–913. [Google Scholar]
- Johnson S, Marlow N. Growing up after extremely preterm birth: Lifespan mental health outcomes. Seminars in Fetal & Neonatal Medicine. 2014;19(2):97–104. doi: 10.1016/j.siny.2013.11.004. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, … Caspi A. Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. American Journal of Psychiatry. 2009;166(1):50–57. doi: 10.1176/appi.ajp.2008.08030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, South SC. Externalizing disorders: cluster 5 of the proposed meta-structure for DSM-V and ICD-11. Psychological Medicine. 2009;39(12):2061–2070. doi: 10.1017/S0033291709990328. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, Diener ED, Emmons RA. An evaluation of subjective well-being measures. Social Indicators Research. 1985;17(1):1–17. [Google Scholar]
- Luciana M. Cognitive development in children born preterm: implications for theories of brain plasticity following early injury. Development and Psychopathology. 2003;15(4):1017–1047. doi: 10.1017/s095457940300049x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychology. 2008;27(2S):S99. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathewson KJ, Chow CTH, Dobson KG, Pope EI, Schmidt LA, Van Lieshout RJ. Mental health of extremely low birth weight survivors: A systematic review and meta-analysis. Psychological Bulletin. 2017;143(4):347–383. doi: 10.1037/bul0000091. [DOI] [PubMed] [Google Scholar]
- Nelson CA, Bos K, Gunnar MR, Sonuga-Barke EJ. The neurobiological toll of early human deprivation. Monographs of the Society for Research in Child Development. 2011;76(4):127–146. doi: 10.1111/j.1540-5834.2011.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annual Review of Clinical Psychology. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- Odgers CL, Moffitt TE, Broadbent JM, Dickson N, Hancox RJ, Harrington H, … Caspi A. Female and male antisocial trajectories: From childhood origins to adult outcomes. Development and Psychopathology. 2008;20(2):673–716. doi: 10.1017/S0954579408000333. [DOI] [PubMed] [Google Scholar]
- O’Donnell KJ, Meaney MJ. Fetal origins of mental health: The developmental origins of health and disease hypothesis. American Journal of Psychiatry. 2016;174(4):319–328. doi: 10.1176/appi.ajp.2016.16020138. [DOI] [PubMed] [Google Scholar]
- Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, … Stein A. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70(12):1312–1319. doi: 10.1001/jamapsychiatry.2013.2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purisch SE, Gyamfi-Bannerman C. Epidemiology of preterm birth. Seminars in Perinatology. 2017;41(7):387–391. doi: 10.1053/j.semperi.2017.07.009. [DOI] [PubMed] [Google Scholar]
- Rawana JS, Morgan AS. Trajectories of depressive symptoms from adolescence to young adulthood: the role of self-esteem and body-related predictors. Journal of Youth and Adolescence. 43(4):597–611. doi: 10.1007/s10964-013-9995-4. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the Adolescent Self-image. Princeton, New Jersey: Princeton University Press; 1965. [Google Scholar]
- Saigal S, Rosenbaum P, Hattersley B, Milner R. Decreased disability rate among 3-year-old survivors weighing 501 to 1000 grams at birth and born to residents of a geographically defined region from 1981 to 1984 compared with 1977 to 1980. Journal of Pediatrics. 1989;114(5):839–846. doi: 10.1016/s0022-3476(89)80150-7. [DOI] [PubMed] [Google Scholar]
- Saigal S, Szatmari P, Rosenbaum P, Campbell D, King S. Cognitive abilities and school performance of extremely low birth weight children and matched term control children at age 8 years: a regional study. Journal of Pediatrics. 1991;118(5):751–760. doi: 10.1016/s0022-3476(05)80043-5. [DOI] [PubMed] [Google Scholar]
- Sala R, Granero R, Ezpeleta L. Dimensional analysis of a categorical diagnostic interview: the DICA-IV. Psicothema. 2006;18(1):123–129. [PubMed] [Google Scholar]
- Schmidt LA, Miskovic V, Boyle MH, Saigal S. Shyness and timidity in young adults who were born at extremely low birth weight. Pediatrics. 2008;122(1):e181–e187. doi: 10.1542/peds.2007-3747. [DOI] [PubMed] [Google Scholar]
- Seckl JR, Meaney MJ. Glucocorticoid programming. Annals of the New York Academy of Sciences. 2004;1032(1):63–84. doi: 10.1196/annals.1314.006. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Skranes J, Vangberg TR, Kulseng S, Indredavik MS, Evensen KAI, Martinussen M, … Brubakk AM. Clinical findings and white matter abnormalities seen on diffusion tensor imaging in adolescents with very low birth weight. Brain. 2007;130(3):654–666. doi: 10.1093/brain/awm001. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociology and Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Sourander A, Pihlakoski L, Aromaa M, Rautava P, Helenius H, Sillanpää M. Early predictors of parent-and self-reported perceived global psychological difficulties among adolescents. Social Psychiatry and Psychiatric Epidemiology. 2006;41(3):173–182. doi: 10.1007/s00127-005-0013-3. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. [Accessed November 7, 2017];Health Fact Sheets: Preterm live births in Canada, 2000 to 2013. 2016 Available at http://www.statcan.gc.ca/pub/82-625-x/2016001/article/14675-eng.htm.
- Van Den Bergh BR. Developmental programming of early brain and behaviour development and mental health: a conceptual framework. Developmental Medicine and Child Neurology. 2011;53(s1):19–23. doi: 10.1111/j.1469-8749.2011.04057.x. [DOI] [PubMed] [Google Scholar]
- Van Lieshout RJ, Boyle MH, Schmidt LA, Saigal S, Ferro MA. Measurement invariance across parent and self-ratings of extremely low birth weight survivors and normal birth weight controls in childhood and adolescence on the Child Behavior Checklist and Youth Self-Report. Journal of Pediatric Psychology. 2015;40(8):825–833. doi: 10.1093/jpepsy/jsv043. [DOI] [PubMed] [Google Scholar]
- Vang Z, Sigouin J, Flenon A, Gagnon A. The healthy immigrant effect in Canada: A systematic review. Population Change and Lifecourse Strategic Knowledge Cluster Discussion Paper Series/Un Réseau stratégique de connaissances Changements de population et parcours de vie Document de travail. 2015;3(1):4. [Google Scholar]
- Vigod SN, Villegas L, Dennis CL, Ross LE. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurology. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. WISC-R, Wechsler Intelligence Scale for Children, revised. Psychological Corporation; 1974. [Google Scholar]
- Zeitlin J, Szamotulska K, Drewniak N, Mohangoo AD, Chalmers J, Sakkeus L, … Blondel B. Preterm birth time trends in Europe: a study of 19 countries. BJOG. 2013;120(11):1356–1365. doi: 10.1111/1471-0528.12281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnostic Plots for Externalizing.
Table S1. Descriptive Statistics for the Internalizing and Externalizing Scales by Group.
Table S2. Characteristics Associated with Missing Data.
Table S3. Measurement Invariance of the Internalizing and Externalizing Scales across Birth Weight Groups and Developmental Periods.
Diagnostic Plots for Internalizing.