Abstract
Introduction:
Scrotal orchidopexy for palpable undescended testicle (UDT) has received attention in the last decade due to its lower morbidity. This study was conducted to determine the frequency and factors related to the use of the scrotal approach in the surgical treatment of palpable UDT among surgeons.
Methods:
An observational cross-sectional study was carried out using an online survey, which was sent to different pediatric urologists, pediatric surgeons, and urologists groups. The survey consisted of questions on demographics as well as surgeons opinions and experience toward scrotal orchidopexy.
Results:
Of 163 respondents, 57 (35.0%) were pediatric surgeons, 98 (60.1%) were pediatric urologists, and 8 (4.9%) were urologists. There were 86 respondents (52.8%) who used the scrotal orchidopexy approach for UDT at any time in their practice. Pediatric urologists tended to use the scrotal orchidopexy approach for UDT more significantly than others (P < 0.001). There were significantly more scrotal orchidopexies for UDT performed by the pediatric urologists throughout their practice and per year compared to others, respectively (P < 0.001). Fifty-two respondents (31.9%) claimed that scrotal orchidopexy is not a good option for their patients, while seven respondents (4.3%) claimed that the procedure was hard to perform.
Discussion:
Based on the results of this study, we believe that there is a discrepancy in the reported advantages and success rate of scrotal orchidopexy in the published literature and the utilization of such an approach among surgeons managing palpable UDT in children.
Conclusion:
Scrotal orchidopexy is an underutilized approach in the management of palpable UDT in children. Only 52.8% of our respondents used it for UDT. One of the main reasons why scrotal orchidopexy is underutilized is due to the surgeons’ perception that scrotal orchidopexy is not the procedure of choice for their patients and their unfamiliarity with the procedure.
Keywords: Cryptorchidism, scrotal orchidopexy, surgical approach, undescended testis
INTRODUCTION
Cryptorchidism is the most common genitourinary disorder during childhood.[1] The testis descends to the scrotum in 75% of full-term neonates and 90% in premature newborns.[2,3] There are two surgical approaches to correct palpable undescended testicle (UDT) – first, there is the traditional inguinal approach, and second, there is the scrotal orchidopexy approach, which was introduced in 1989 by Bianchi and Squire although it is still not a popular choice as far as surgeons are concerned.[4] The scrotal approach was found to have a lower morbidity rate, with a shorter hospital stay, shorter operation times, and less-associated pain. It is also deemed to be more cosmetically feasible in comparison with the traditional inguinal approach.[5]
Scrotal orchidopexy procedures that were performed on patients with testes located within the inguinal canal and testes located beyond the external inguinal ring were found to have a success rate of 97.6%.[6] Moreover, in terms of long-term outcomes, the scrotal orchidopexy approach was found to be more efficient and safe when compared to the traditional approach.[7] The incidence of wound infection; testicular atrophy and testicular reascent are very low after surgery using the scrotal orchidopexy approach.[8]
Cuda et al. observed a declining in the trend in the standard inguinal approach usage for the treatment of UDT and increase of single scrotal incision from approximately 15% to a high of 63%.[9] The question as to why pediatric urologists and pediatric surgeons either utilize or do not utilize the scrotal approach over the traditional inguinal approach is an important aspect of this study, especially in view of the fact that the scrotal approach has been found to be a safe and efficient method in treating palpable UDT. This interesting disparity in approach, therefore, warrants investigation.[8] Thus, this study was conducted to determine the use of the scrotal approach in the surgical treatment of palpable UDT and to identify the factors related to such an approach seeing as it is a frequently used procedure amongst pediatric surgeons and pediatric urologists from different institutions.
METHODS
This is a quantitative (observational) cross-sectional study, which looks at the utilization of scrotal orchidopexy among surgeons. An online self-administered questionnaire was sent in July 2017 to all the members of the: Canadian Pediatric Urology Group, the Society for Pediatric Urology, Saudi Pediatric Urology Group, Arab Pediatric Surgery Group and the Pediatric urology E-mail listing group. The inclusion criteria for those participating in the survey were that they should be either a pediatric urologist, a pediatric surgeon, or a urologist.
The questionnaire comprised two parts, which were as follows [Figure 1]: The first section queried the demographics of the surgeons as well as their surgical experience. The second section was concerned with their opinions and experience toward scrotal orchidopexy. In addition, the questionnaire was designed to assess the surgeons’ conceptual understanding of the reasons for not practicing the scrotal approach.
Figure 1.
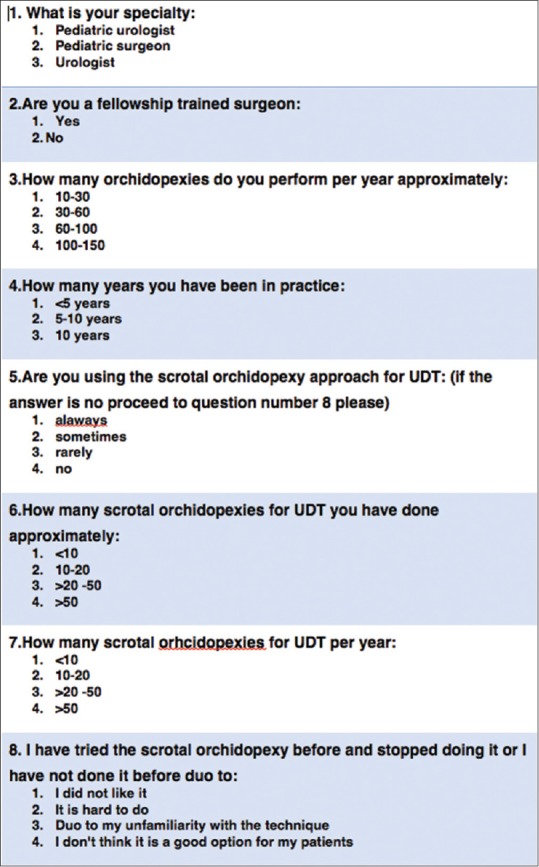
Utilization of scrotal orchidopexy for palpable undescended testes among surgeons survey
All statistical analyses were performed using the SPSS® statistical software package for social studies, version 22.0 (SPSS Inc., Chicago, IL, USA) for Windows®. Chi-square statistics and odds ratios were calculated to correlate demographic factors and surgical experience along with reasons for practicing the preferred surgical approach for cryptorchidism. P ≤0.05 was considered to be statistically significant. Ethical Board Approval for this study was obtained by our institution.
RESULTS
There were 163 respondents to our survey, 57 (35.0%) were pediatric surgeons, 98 (60.1%) were pediatric urologists and 8 (4.9%) were general urologists [Table 1]. When we looked at the number of orchidopexies performed per year by the surgeons participating in the study we discovered that the number was variable with only 17.5% of the surgeons conducting <30 orchidopexies per year. The number of years spent in practice also varied with 95 (58%) of the surgeons have been in practice for more than 10 years [Table 1]. Incidentally, there were significantly more fellowship-trained pediatric urologists (91/141, 64.5%) compared to pediatric surgeons (44/141, 31.2%) and urologists (6/141, 4.3%), P = 0.014 [Figure 2].
Table 1.
Demographic profile of the 163 respondents
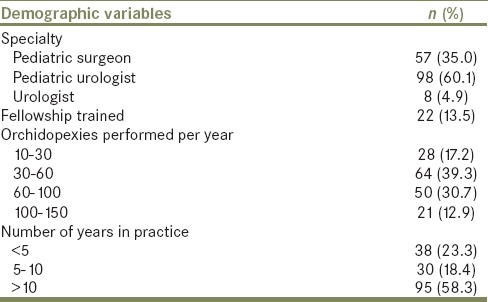
Figure 2.
Percentage of fellowship training by specialty
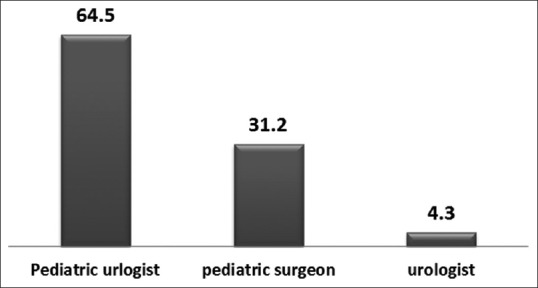
There were only 86 respondents (52.8%) who used the scrotal orchidopexy approach for UDT. Of the 86 positive responses, 11 (6.7%) said that they used scrotal orchidopexy “always,” whereas the remaining 75 (46.0%) used scrotal orchidopexy “sometimes.” Significantly, however, the pediatric urologists used the scrotal orchidopexy approach for UDT more frequently than the pediatric surgeons and urologists (65.3% vs. 38.6% vs. 0%, P < 0.001). In fact, their response to the question of whether they carried out the procedure or not was “always” and “sometimes.” There were significantly more scrotal orchidopexies for UDT performed by the pediatric urologists throughout their practice compared to the pediatric surgeons and urologists (81.6% vs. 49.1% vs. 62.5%, P < 0.001) [Figure 3]. In addition, there were significantly more scrotal orchidopexies for UDT performed per year among pediatric urologists compared to pediatric surgeons and urologists (P = 0.001) [Figure 4].
Figure 3.

Percentages of all scrotal orchidopexies performed by different specialties
Figure 4.
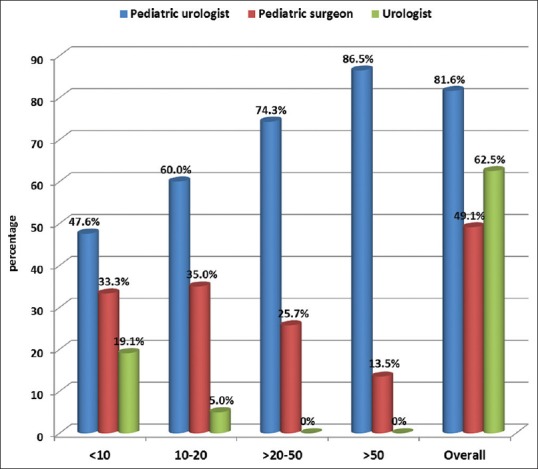
Percentage of scrotal orchidopexies performed per year according to specialties
When we examined the reasons why surgeons were not using scrotal orchidopexy often or not using the procedure at all we discovered that 97/163 (60%) of physicians were not using it due to different reasons including their unfamiliarity with the technique, and their disliking the idea of changing their approach from the previously mentioned classical technique. They also reported that they feared the prospect of facing various technical difficulties while performing scrotal orchidopexy [Table 2].
Table 2.
Responses to questions about the use of scrotal orchidopexy for cryptorchidism among 163 respondents
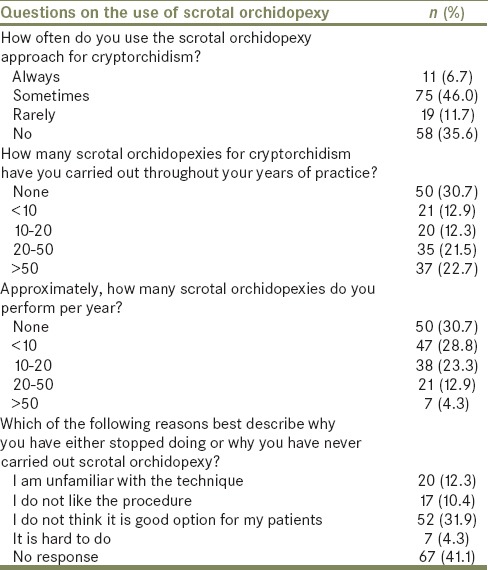
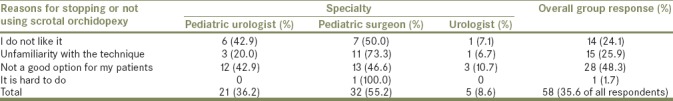
There were 58 respondents (35.6%) who claimed that they “do not use” scrotal orchidopexy for UDT, and 19 (11.7%) of the surgeons who were surveyed claimed that they “rarely” used scrotal orchidopexy for UDT. Of the 58 respondents, who claimed that they “do not use” scrotal orchidopexy for UDT, 28 (48.3%) claimed that the approach is not a good option for their patients, whereas 15 (25.9%) claimed they were unfamiliar with the technique. Moreover, 14 (24.1%) did not like the procedure at all, and 1 (1.7%) respondent even claimed that the approach was hard to perform. There were no significant differences in the reasons why the respondents had not performed scrotal orchidopexy and their different subspecialties (P = 0.675) [Table 3].
Table 3.
Reasons for stopping doing scrotal orchidopexy or reasons why respondents have not carried out scrotal orchidopexy
DISCUSSION
This study aimed to answer the question of if whether surgeons utilize the scrotal orchidopexy approach for palpable UDT over the traditional inguinal approach and to analyze the factors that play a role in determining which approach is chosen. Notably, in the past, the scrotal approach was rarely used in patients with UDT. However, given the abundance of publications concerning scrotal orchidopexy as well as ample reports of the use of the procedure with similar success rates to the classic inguinal approach we were surprised that it is not as yet a popular choice among surgeons.
Regarding the frequency of the use of scrotal orchidopexy for UDT, this study has shown that 22.7%, 21.7%, 12.3%, and 12.9% of the respondents have performed this approach for UDT for >50 times, 20–50 times, 10–20 times, and <10 times, respectively, throughout their practice. On the other hand, 30.7% of the respondents have never used scrotal orchidopexy for UDT during their practice. This reflects the underutilization of this particular surgical approach. While assessing the reasons why the scrotal approach is not being utilized more frequently, it was discovered that 31.9% of the surgeons surveyed believed that it is not a good option for their patients and 4.3% claimed that the procedure was hard to do. The other reasons for surgeons not using the scrotal approach are discussed in Table 3. In fact, two prominent reasons for the nonimplementation of the procedure were cited, which were, specifically, that the approach was “not a good option for my patients” and also that it was “hard to do.” These reasons, therefore, reflect a negative perception of the procedure either due to a lack of information and evidence-based practice guidelines, or a lack of practice and training in relation to carrying out the procedure of scrotal orchidopexy.
The frequency of using the scrotal orchidopexy for UDT is evident in the results of this study. Of the three specialties, the pediatric urologists perform scrotal orchidopexy significantly more than the pediatric surgeons and urologists regardless of their years of training and the duration of practice. The pediatric urologists use the scrotal orchidopexy approach for UDT considerably more in comparison to the pediatric surgeons and urologists (65.3% vs. 38.6% vs. 0%, P < 0.001), and have performed more scrotal orchidopexies for UDT throughout their practice compared to the pediatric surgeons and urologists (81.6% vs. 49.1% vs. 62.5%, P < 0.001) [Figure 3]. However, despite this, 65.3% of the pediatric urologists who use the scrotal orchidopexy approach for UDT, as well as those who either refrained or stopped using this approach altogether claimed that the scrotal approach is “not a good option” for their patients (12/28, 42.9%), or that they were unfamiliar with the technique (3/15, 20.0%). Nevertheless, in general, there were more pediatric urologists who favored the use of scrotal orchidopexy and were familiar with the technique compared to the number of pediatric surgeons and the urologists who were either unfamiliar with the practice or against it [Table 3].
Some studies have shown that the choice and selection of a surgical procedure is not only dependent on the overall success and outcome of the procedure but also hinges on a lower incidence of postoperative complications, fewer failure rates, and ease of surgical approach.[10] This is true whether the UDT is palpable or not, where, generally speaking, the choice of approach tends to be open orchidopexy for palpable UDT while the laparoscopic approach is favored in cases of nonpalpable UDT.[1,11] However, there was a published report that recommended using single scrotal incision orchidopexy even in impalpable UDT.[12] The same study further stated that the reasons for choosing scrotal orchidopexy over other approaches were due to the shorter operative time involved and a more cosmetically desirable appearance, along with apparently less pain being experienced by the patient.[1,12]
This study has highlighted the fact that there is a current underutilization of scrotal orchidopexy in the surgical management of UDT. In fact, the most common reason for not conducting scrotal orchidopexy amongst our respondents was that “it is not a good option for our patients.” Although, in retrospection, it would have been better if we had asked the respondents why they thought that “it was not a good option.” This study has also highlighted the fact that despite the statistically nonsignificant difference in the number of years of practice of our respondents, the use of scrotal orchidopexy is still underutilized. Another limitation of this study was that we were not able to highlight which particular type of UDT the surgeons were managing, i.e., palpable or nonpalpable. Interestingly, however, it seems to be common knowledge among surgeons that impalpable UDT is usually managed using the laparoscopic and inguinal approach rather than the scrotal incision orchidopexy approach. One of the other limitations of this study is that there seems to be a recall bias when it comes to accurately documenting the number of procedures that have actually been performed but this is compensated for by the surgeons’ beliefs and preferences in their day-to-day practice.
Based on the results of this study, we believe that there is a discrepancy in the reported advantages and success rate of scrotal orchidopexy in the published literature surrounding this topic and in the utilization of such an approach among surgeons managing palpable UDT.
CONCLUSION
Scrotal orchidopexy is an underutilized approach in the management of UDT. There are more pediatric urologists who use this approach compared to pediatric surgeons and urologists. The main reasons why scrotal orchidopexy is underutilized include the surgeons’ perception that scrotal orchidopexy is not the procedure of choice for their patients and their unfamiliarity with the procedure. Despite the recording of good results pertaining to scrotal orchidopexy in the literature, its use is not widespread and therefore, there is a need to familiarize surgeons with it and expose our trainees to different surgical techniques in their training.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Novaes HF, Carneiro Neto JA, Macedo A, Jr, Barroso U., Júnior Single scrotal incision orchiopexy – A systematic review. Int Braz J Urol. 2013;39:305–11. doi: 10.1590/S1677-5538.IBJU.2013.03.02. [DOI] [PubMed] [Google Scholar]
- 2.Abacı A, Çatlı G, Anık A, Böber E. Epidemiology, classification and management of undescended testes: Does medication have value in its treatment? J Clin Res Pediatr Endocrinol. 2013;5:65–72. doi: 10.4274/Jcrpe.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hensel KO, Caspers T, Jenke AC, Schuler E, Wirth S. Operative management of cryptorchidism: Guidelines and reality – A 10-year observational analysis of 3587 cases. BMC Pediatr. 2015;15:116. doi: 10.1186/s12887-015-0429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alp BF, Irkilata HC, Kibar Y, Zorba U, Sancaktutar AA, Kaya E, et al. Comparison of the inguinal and scrotal approaches for the treatment of communicating hydrocele in children. Kaohsiung J Med Sci. 2014;30:200–5. doi: 10.1016/j.kjms.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Na SW, Kim SO, Hwang EC, Oh KJ, Jeong SI, Kang TW, et al. Single scrotal incision orchiopexy for children with palpable low-lying undescended testis: Early outcome of a prospective randomized controlled study. Korean J Urol. 2011;52:637–41. doi: 10.4111/kju.2011.52.9.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dayanç M, Kibar Y, Tahmaz L, Yildirim I, Peker AF. Scrotal incision orchiopexy for undescended testis. Urology. 2004;64:1216–8. doi: 10.1016/j.urology.2004.06.069. [DOI] [PubMed] [Google Scholar]
- 7.Dayanc M, Kibar Y, Irkilata HC, Demir E, Tahmaz L, Peker AF, et al. Long-term outcome of scrotal incision orchiopexy for undescended testis. Urology. 2007;70:786–8. doi: 10.1016/j.urology.2007.04.053. [DOI] [PubMed] [Google Scholar]
- 8.Feng S, Yang H, Li X, Yang J, Zhang J, Wang A, et al. Single scrotal incision orchiopexy versus the inguinal approach in children with palpable undescended testis: A systematic review and meta-analysis. Pediatr Surg Int. 2016;32:989–95. doi: 10.1007/s00383-016-3956-4. [DOI] [PubMed] [Google Scholar]
- 9.Cuda SP, Srinivasan AK, Kalisvaart J, Kirsch AJ. Evolution of single practice trends in the surgical approach to the undescended testicle. J Urol. 2011;185:2451–4. doi: 10.1016/j.juro.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Stec AA, Tanaka ST, Adams MC, Pope JC, 4th, Thomas JC, Brock JW, 3rd, et al. Orchiopexy for intra-abdominal testes: Factors predicting success. J Urol. 2009;182:1917–20. doi: 10.1016/j.juro.2009.03.069. [DOI] [PubMed] [Google Scholar]
- 11.Thorup J, Haugen S, Kollin C, Lindahl S, Läckgren G, Nordenskjold A, et al. Surgical treatment of undescended testes. Acta Paediatr. 2007;96:631–7. doi: 10.1111/j.1651-2227.2007.00239.x. [DOI] [PubMed] [Google Scholar]
- 12.Callewaert PR, Rahnama’i MS, Biallosterski BT, van Kerrebroeck PE. Scrotal approach to both palpable and impalpable undescended testes: Should it become our first choice? Urology. 2010;76:73–6. doi: 10.1016/j.urology.2009.09.096. [DOI] [PubMed] [Google Scholar]


