Abstract
Context:
urethral strictures commonly occur and considered difficult to manage due to high recurrence rate and wide variety of management approach.
Aims:
This study aims to identify how urologists in Saudi Arabia manage new and recurrent urethral stricture cases and to investigate their opinions regarding urethroplasty.
Settings and Design:
A cross-sectional study (Online Survey) among urologists.
Subjects and Methods:
A nationwide survey of urologists registered with the Saudi Commission for Health Specialties was performed through a mailed questionnaire. A total of 603 urologists were selected from all five regions of Saudi Arabia, of whom 216 (35.8%) completed the questionnaire.
Statistical Analysis Used:
SPSS software version 23 was used for data entry and analysis.
Results:
Most urologists (40.3%) had treated 1–5 urethral strictures in the past year. The most common procedures used to manage urethral strictures were visual urethrotomy (82.4%), cystoscopy and dilatation (62.2%), and excision and primary anastomosis (20.8%). Minimally invasive procedures were used more frequently than any open urethroplasty techniques. Most urologists (63%) did not perform urethroplasty surgery, and 21.8% were not aware of any adult reconstructive urologists in Saudi Arabia. When used, however, the most commonly performed urethroplasty surgeries were excision and primary anastomosis, dorsal buccal graft augmented urethroplasty, and ventral buccal graft augmented urethroplasty.
Conclusions:
Minimally invasive methods are easy to perform and have good short-term outcomes. As such, they are more commonly used for the management of urethral strictures. On the other hand, urethroplasty surgeries are challenging procedures that require greater experience and skill.
Keywords: Management pattern, urethra, urethral stricture
INTRODUCTION
Urethral strictures commonly occur, and their risk increases with age. They are also considered to be the most challenging and stressful problem that urologists are required to manage.[1] Indeed, urethral strictures cause >1.5 million visits to urologists’ offices annually in the US and were responsible for a financial burden of >$191 million in the year 2000.[2]
The approach to urethral stricture management has significantly changed over the past 40 years.[1] In particular, there has been a long-running debate between urologists regarding the roles of endourological procedures (i.e., internal urethrotomy or urethral dilatation) and urethroplasty.[3] Accordingly, many studies have been conducted worldwide to identify the most commonly performed procedures for urethral stricture management and to determine the importance of urethroplasty.
It has been found that for the management of both newly diagnosed and recurrent cases in the UK, urethrotomy is the most commonly used procedure, followed by dilatation then urethroplasty.[4] In the US, dilatation is the most common procedure, followed by urethrotomy, endourethral stent insertion, then urethroplasty. Furthermore, the most common urethroplasty procedure in the US is end-to-end anastomotic urethroplasty.[5] Overall, published data suggest that the minimally invasive methods of urethrotomy and dilatation are the most commonly used procedures in the management of urethral strictures worldwide.[6] However, despite being less common, urethroplasty has a much higher long-term success rate and better outcomes in terms of recurrence rate than dilatations and urethrotomies.[7,8] This thus suggests that for the definitive correction of urethral strictures, urethroplasty is the most effective method and should generally be considered the gold standard for treatment.[9,10]
In this study, we aimed to identify how urologists in Saudi Arabia manage patients with urethral stricture and to determine whether there is a discrepancy between government and private sector recommendations regarding management procedures and opinions toward urethroplasty.
SUBJECTS AND METHODS
A nationwide study was conducted among urologists (including registrars, senior registrars, and consultants) registered with the Saudi Commission for Health Specialties in all 5 regions of the Kingdom of Saudi Arabia. The survey was conducted from December 2016 to May 2017 as a mailed questionnaire. Along with the survey, each participant received information regarding the objectives of our study and a copy of the approval letter from the institutional review board.
The questionnaire consisted of 15 close-ended questions [Appendix 1] eliciting information on respondent demographics, the number of urethral strictures treated in the past year, commonly used procedures, urethral stricture management strategies, opinions toward urethroplasty, preferred minimally invasive methods of management, and awareness of adult reconstructive surgery availability in Saudi Arabia.
SPSS software version 23 (SPSS Inc., Chicago, Illinois, USA) was used for data entry and analysis.
RESULTS
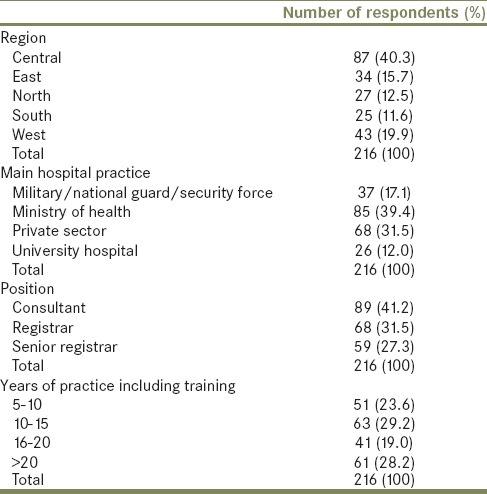
Of the 603 urologists contacted for our survey, 216 (35.8%) responded. The characteristics of these respondents are summarized in Table 1.
Table 1.
Respondent characteristics
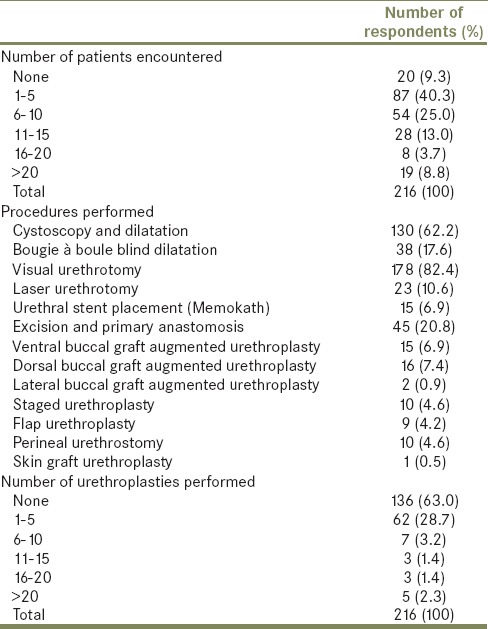
In terms of case numbers treated, we found that most urologists surveyed had treated 1–5 urethral strictures in the past year. The most common procedures used in descending order were visual urethrotomy, cystoscopy and dilatation, excision and primary anastomosis, and bougie à boule-blind dilatation. Minimally invasive methods were performed more commonly than any open urethroplasty techniques, with most urologists not performing any urethroplasty procedures. Of those who did, most performed 1–5 procedures, and only few performed more. The most commonly performed urethroplasty procedures in descending order were excision and primary anastomosis, dorsal buccal graft augmented urethroplasty, ventral buccal graft augmented urethroplasty, staged urethroplasty, and perineal urethrostomy. These results are summarized in detail in Table 2.
Table 2.
Number of urethral stricture patients encountered and stricture management procedures performed over the past year
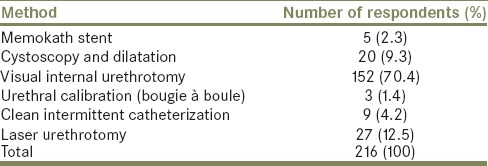
Regarding preferred management procedures for newly diagnosed patients with 1-cm urethral strictures, most urologists indicated that they would choose to treat the patient with endourological management (i.e., internal urethrotomy or cystoscopy and dilatation) and half would opt for urethroplasty. For first recurrences in the same patient, 67.1% and 18.1% of urologists indicated that they would opt for endourological management and urethroplasty, respectively. For second recurrences in the same patient and beyond, however, the proportion of urologists opting for endourological management progressively fell, while the proportion of urologists opting for urethroplasty progressively rose. These results are summarized in detail in Table 3. Regarding preferred minimally invasive procedures, most urologists preferred to perform visual internal urethrotomy [Table 4].
Table 3.
Preferred strategies for the management of urethral strictures
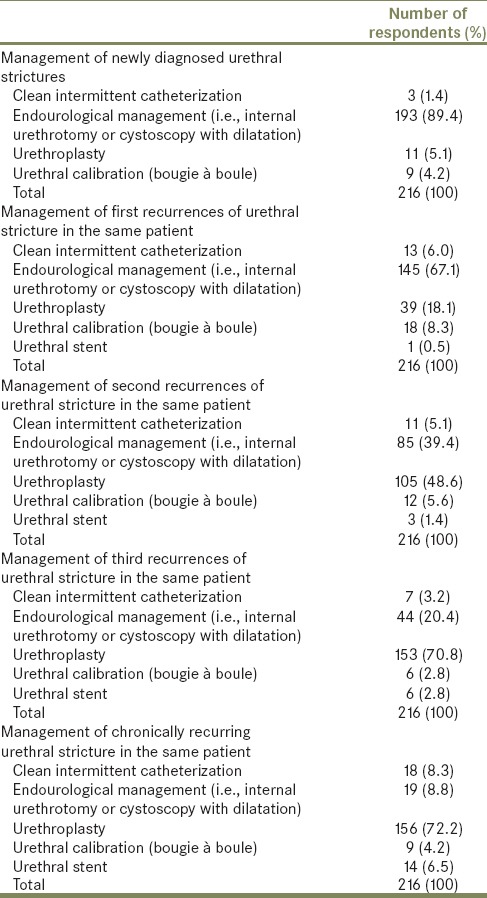
Table 4.
Preferred minimally invasive methods for the management of urethral strictures
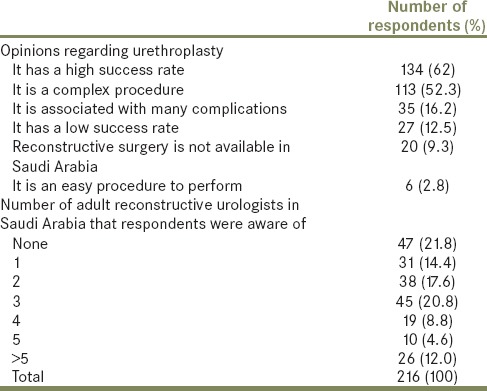
Finally, with respect to opinions toward urethroplasty, we found that large proportions of surveyed urologists regarded it as having a high success rate and being a complex procedure. Furthermore, a substantial proportion was unaware of any adult reconstructive urologists in Saudi Arabia. These results are summarized in detail in Table 5.
Table 5.
Opinions regarding urethroplasty and awareness of adult reconstructive urologists available in Saudi Arabia
DISCUSSION
Over the past 40 years, the management of urethral strictures has undergone significant changes. Currently, minimally invasive methods are the most commonly used,[1] which is in line with findings from our survey of urologists in Saudi Arabia. For example, we found that internal urethrotomy and dilatation were the most commonly performed procedures in the past year. These results are similar to those of nationwide surveys of urologists in the Netherlands, Italy, and Turkey,[11,12,13] as well as those of a survey demonstrating that dilatation and internal urethrotomy are the most commonly used procedures in the US. Regarding other procedures used for managing urethral strictures, we found that 6.9% of urologists surveyed had used urethral stents in the past year, which is also similar to the results of other studies.[11,12,13]
Although internal urethrotomy and dilatation differ procedurally, it has been suggested that they have similar recurrence rates.[14] Direct visual internal urethrotomy (DVIU), which was first described in 1974 by Sachse, has, in particular, become a widely popular and safe procedure that is frequently used for the primary management of urethral strictures.[15] However, studies examining recurrence rates of DVIU over a period of 4 years found that recurrence occurred in 61% of new DVIU cases, and in 100% of second and third DVIU cases.[16,17]
We conclude from these studies that internal urethrotomy is generally considered only as an initial management option for urethral strictures although it should be noted that these studies lack long-term follow-up data.
Regarding preferred procedures for the management of urethral strictures, most urologists (70.4%) preferred visual internal urethrotomy out of the minimally invasive methods available, where minimally invasive methods fail, open urethroplasty is generally considered throughout the literature as the best and most effective option for the definitive correction of urethral strictures. This is because it has a high success rate and better long-term outcomes than internal urethrotomy.[18,19] However, in accordance with another study,[5] we observed that the majority of urologists surveyed (63%) did not perform urethroplasty and that the most common invasive procedure was excision and primary anastomosis. A particularly interesting finding of our study was that 21.8% of urologists surveyed were unaware of there being adult reconstructive urologists available in Saudi Arabia. Furthermore, when presented with a multiple choice question regarding their opinion toward urethroplasty, large proportions of surveyed urologists indicated that they believed it has a high success rate (63%) and is a complex procedure (52%). These findings support our view that urethroplasty is a complex but effective procedure requiring urologists with sufficient skill and experience.
CONCLUSIONS
Most urologists in Saudi Arabia manage urethral stricture patients with minimally invasive methods at first diagnosis and first recurrence. This is because minimally invasive methods are easy to perform and have good short-term outcomes. On the other hand, anastomotic urethroplasty and urethroplasty graft techniques are less frequently used, likely because urethroplasties are challenging procedures that require more experienced urologists. As such, some variation in standard practice across different hospitals and regions should be expected, with the availability of sufficiently experienced urologists in different centers playing a role in this variation. Finally, urology centers need to draw more attention to the availability of adult reconstructive surgery in Saudi Arabia.
Financial support and sponsorship
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank our colleagues from Research Center, Deanship of Scientific Research, College of Medicine, King Saud University who provided insight and expertise that greatly assisted the research paper.
Appendix 1: Management of urethral stricture questionnaire
REFERENCES
- 1.Chiou RK, Matamoros A, Anderson JC, Taylor RJ. Changing concepts of urethral stricture management. I: Assessment of urethral stricture disease. Nebr Med J. 1996;81:282–6. [PubMed] [Google Scholar]
- 2.Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol. 2007;177:1667–74. doi: 10.1016/j.juro.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 3.Mundy AR, Andrich DE. Urethral strictures. BJU Int. 2011;107:6–26. doi: 10.1111/j.1464-410X.2010.09800.x. [DOI] [PubMed] [Google Scholar]
- 4.Greenwell TJ, Castle C, Andrich DE, MacDonald JT, Nicol DL, Mundy AR, et al. Repeat urethrotomy and dilation for the treatment of urethral stricture are neither clinically effective nor cost-effective. J Urol. 2004;172:275–7. doi: 10.1097/01.ju.0000132156.76403.8f. [DOI] [PubMed] [Google Scholar]
- 5.Bullock TL, Brandes SB. Adult anterior urethral strictures: A national practice patterns survey of board certified urologists in the United States. J Urol. 2007;177:685–90. doi: 10.1016/j.juro.2006.09.052. [DOI] [PubMed] [Google Scholar]
- 6.Andrich DE, Mundy AR. Urethral strictures and their surgical treatment. BJU Int. 2000;86:571–80. doi: 10.1046/j.1464-410x.2000.00878.x. [DOI] [PubMed] [Google Scholar]
- 7.Naudé AM, Heyns CF. What is the place of internal urethrotomy in the treatment of urethral stricture disease? Nat Clin Pract Urol. 2005;2:538–45. doi: 10.1038/ncpuro0320. [DOI] [PubMed] [Google Scholar]
- 8.Bello JO. Impact of preoperative patient characteristics on posturethroplasty recurrence: The significance of stricture length and prior treatments. Niger J Surg. 2016;22:86–9. doi: 10.4103/1117-6806.188979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong SS, Narahari R, O’Riordan A, Pickard R. Simple urethral dilatation, endoscopic urethrotomy, and urethroplasty for urethral stricture disease in adult men. Cochrane Database Syst Rev. 2010;4:CD006934. doi: 10.1002/14651858.CD006934.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Jordan GH, McCammon KA. Surgery of the Penis and Urethra. Vol. 1. Oxford: Elsevier Saunders; 2012. pp. 956–1000. [Google Scholar]
- 11.van Leeuwen MA, Brandenburg JJ, Kok ET, Vijverberg PL, Bosch JL. Management of adult anterior urethral stricture disease: Nationwide survey among urologists in the Netherlands. Eur Urol. 2011;60:159–66. doi: 10.1016/j.eururo.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 12.Palminteri E, Maruccia S, Berdondini E, Di Pierro GB, Sedigh O, Rocco F, et al. Male urethral strictures: A national survey among urologists in Italy. Urology. 2014;83:477–84. doi: 10.1016/j.urology.2013.10.043. [DOI] [PubMed] [Google Scholar]
- 13.Akyuz M, Sertkaya Z, Koca O, Caliskan S, Kutluhan MA, Karaman MI, et al. Adult urethral stricture: Practice of Turkish urologists. Int Braz J Urol. 2016;42:339–45. doi: 10.1590/S1677-5538.IBJU.2014.0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steenkamp JW, Heyns CF, de Kock ML. Internal urethrotomy versus dilation as treatment for male urethral strictures: A prospective, randomized comparison. J Urol. 1997;157:98–101. [PubMed] [Google Scholar]
- 15.Sachse H. Treatment of urethral stricture: Transurethral slit in view using sharp section. Fortschr Med. 1974;92:12–5. [PubMed] [Google Scholar]
- 16.Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: Long-term followup. J Urol. 1996;156:73–5. [PubMed] [Google Scholar]
- 17.Heyns CF, Steenkamp JW, De Kock ML, Whitaker P. Treatment of male urethral strictures: Is repeated dilation or internal urethrotomy useful? J Urol. 1998;160:356–8. doi: 10.1016/s0022-5347(01)62894-5. [DOI] [PubMed] [Google Scholar]
- 18.Barbagli G, Palminteri E, Lazzeri M, Guazzoni G, Turini D. Long-term outcome of urethroplasty after failed urethrotomy versus primary repair. J Urol. 2001;165:1918–9. doi: 10.1097/00005392-200106000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Andrich DE, Dunglison N, Greenwell TJ, Mundy AR. The long-term results of urethroplasty. J Urol. 2003;170:90–2. doi: 10.1097/01.ju.0000069820.81726.00. [DOI] [PubMed] [Google Scholar]


