ABSTRACT
Background
Panel management is emphasized as a subcompetency in internal medicine graduate medical education. Despite its importance, there are few published curricula on population medicine in internal medicine residency programs.
Objective
We explored resident experiences and clinical outcomes of a 5-month diabetes and obesity ambulatory panel management curriculum.
Methods
From August through December 2016, internal medicine residents at the University of Vermont Medical Center reviewed registries of their patients with diabetes, prediabetes, and obesity; completed learning modules; coordinated patient outreach; and updated gaps in care. Resident worksheets, surveys, and reflections were analyzed using descriptive and thematic analyses. Before and after mean hemoglobin A1c results were obtained for patients in the diabetic group.
Results
Most residents completed the worksheet, survey, and reflection (93%–98%, N = 42). The worksheets showed 70% of participants in the diabetic group had appointments scheduled after outreach, 42% were offered referrals to the Community Health Team, and 69% had overdue laboratory tests ordered. Residents reported they worked well with staff (95%), were successful in coordinating outreach (67%), and increased their sense of patient care ownership (66%). In reflections, identified successes were improved patient care, teamwork, and relationship with patients, while barriers included difficulty ensuring follow-up, competing patient priorities, and difficulty with patient engagement. Precurricular mean hemoglobin A1c was 7.7%, and postcurricular was 7.6% (P = .41).
Conclusions
The curriculum offered a feasible, longitudinal model to introduce residents to population health skills and interdisciplinary care coordination. Although mean hemoglobin A1c did not change, residents reported improved patient care. Identified barriers present opportunities for resident education in patient engagement.
What was known and gap
Panel management is emphasized in primary care but has not been studied in depth in the setting of graduate medical education.
What is new
A prospective study of a panel management curriculum in an internal medicine residency assessed resident perceptions, successes and barriers, and impact on clinical outcomes.
Limitations
Single site study limits generalizability; instruments lack validity evidence.
Bottom line
The curriculum was feasible, and while mean hemoglobin A1c did not change, residents reported improved patient care.
Introduction
Panel management is an integral component of the Chronic Care Model,1–6 a quality improvement framework that systematically addresses gaps in care for chronic illness. Panel management is a proactive, structured process in which physicians use dedicated time to direct patient care, work with primary care teams to use technology/information to identify care gaps, and provide outreach to patients.6 The Accreditation Council for Graduate Medical Education (ACGME) has practice-based learning and improvement and systems-based practice competencies that require internal medicine residents to use quality improvement methods to analyze their practice and implement changes in an interprofessional team to improve patient care.7 Panel management curricula in residency have the potential to meet population needs while addressing core competencies and training future physician team leaders.8–10 Reports of residency panel management curricula have been encouraging, with statistically significant improvements in glycemic control, low-density lipoprotein, and blood pressure11,12; more frequent completion of quality metrics13; and improved self-reported practice behaviors among residents.13,14 The optimal approach to integrating panel management into graduate medical education has not been determined.
We integrated a prediabetes, diabetes, and obesity panel management curriculum into the didactic ambulatory curriculum in an internal medicine residency clinic. We hypothesized this would increase residents' sense of ownership of patient care; promote teamwork among staff and residents, patient outreach, and self-management goal setting with patients; and improve glycemic control among clinic patients with diabetes.
Methods
Setting and Participants
Internal medicine residents (postgraduate years 1–3) at the University of Vermont Medical Center were required to participate in the ambulatory panel management curriculum. Residents have their primary continuity clinic at a university-based practice in Burlington, Vermont. The practice is a National Committee for Quality Assurance Level 3 Patient-Centered Medical Home serving approximately 3671 patients. The 42 residents (31 categorical and 11 primary care residents) were divided into 5 cohorts and rotated through the clinic every fifth week (4 + 1 block schedule). Each resident has 80 to 100 patients in his or her continuity panel. There are typically 2 faculty preceptors staffing the clinic each half day, and 4 medical assistants (MAs) or licensed practical nurses (LPNs) responsible for providing patient rooms, reviewing chronic disease registries, and following protocols for ordering laboratory tests. Two registered nurses (RNs) triage telephone calls, and 3 medical staff are responsible for scheduling and clerical support.
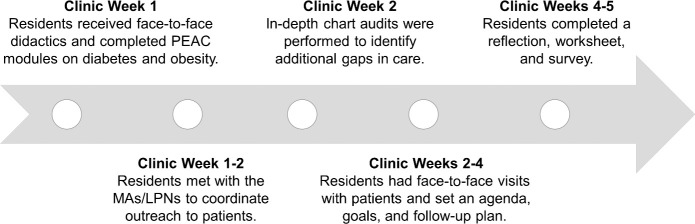
Curricular Intervention
As each cohort rotated into their clinic week in August or September 2016, residents participated in a didactic lecture about panel management and received, via e-mail, detailed panel management instructions specific to diabetes and obesity. Residents dedicated 1 half day each clinic week to the panel management curriculum over a 5-month period through December 2016 (Figure) and were asked to complete the Physician Education and Assessment Center (PEAC) learning modules on diabetes and obesity.15,16 Residents received a list of their patient panel who had at least 1 of the following conditions: prediabetes (hemoglobin A1c [HbA1c], 5.7–6.4), diabetes (HbA1c ≥ 6.5), or obesity (body mass index ≥ 30). All patients needed to have an encounter within the past year (telephone, order, or appointment) to ensure they were an active patient of the clinic and a resident listed as their primary care provider in the electronic health record. Registries were generated by the information technology team. Residents met with their team MA/LPN to identify and schedule patients for appointments and order overdue laboratory tests. The MAs/LPNs were given separate instructions for reviewing charts in preparation for the meetings with the residents. Residents were encouraged to set self-management goals with their patients regarding behavior changes and to refer patients, as needed, to a multidisciplinary Community Health Team (CHT) staffed by diabetes educators, social workers, dietitians, and health coaches. Two designated faculty leaders (A.R.L. and H.G.S.) were available for questions about panel management as needed.
Figure.
Panel Management Curriculum Timeline (August–December 2016)a
a Due to the 4 + 1 block schedule, it was a total of 4 to 5 clinic weeks over a course of 5 months.
Residents were required to complete a worksheet for the diabetes portion of the registry that asked them to log whether follow-up visits were scheduled after outreach, CHT services were offered, self-management goals were set, and laboratory tests were ordered or updated. Residents completed a 10-item survey about the curriculum that utilized a 5-point Likert scale (strongly agree to strongly disagree) and a reflection consisting of 2 open-ended questions about what was successful about the experience and what barriers occurred in closing gaps in chronic disease management. The curriculum and the panel management instructions, worksheet, reflection, and survey (provided as online supplemental material) were developed in an iterative fashion by the authors. The survey was not tested for validity evidence.
The study was approved by the University of Vermont Institutional Review Board.
Data Collection and Analysis
Descriptive analysis was used to summarize the worksheet and survey responses. Analysis of residents' open-ended reflections was performed by the authors using a grounded theory process17 to identify common themes in the successes and barriers of the curriculum. The mean HbA1c of residents' patients with diabetes was obtained prior to the curricular intervention in August 2016 and compared with the mean HbA1c obtained from February through September 2017 using a paired t test. Agreement of survey responses was compared between the primary care and categorical track residents using a 2-tailed Fisher's exact test.
Results
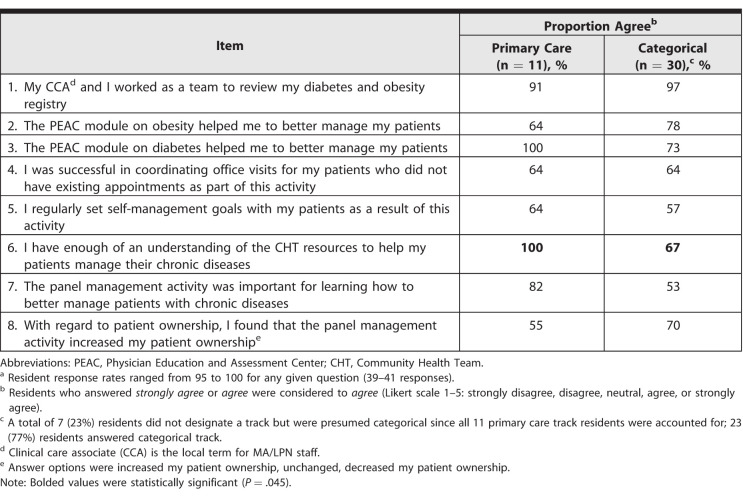
Of 42 residents, 39 (93%) completed the activity worksheet, 41 (98%) completed the curriculum survey, and 40 (95%) completed the reflection. In their worksheets, residents reported that 70% (149 of 213) of patients in the diabetic group had follow-up appointments scheduled after outreach, 42% (89 of 213) were offered referral to the CHT, and 69% (147 of 213) had follow-up laboratory tests ordered. In the responses, most residents indicated the curriculum successfully promoted ownership of patient care, teamwork, patient outreach, and goal setting (Table 1). The only significant difference between the primary care and categorical responses was that primary care residents reported a better understanding of CHT resources (100%, 11 of 11) compared with categorical residents (67%, 20 of 30; P = .04). On average, a resident panel had 24 patients who were obese (77%, 788 of 1017) and/or prediabetic (30%, 303 of 1017) or diabetic (18%, 183 of 1017) based on HbA1c values. Data were analyzed for 119 patients who had values in both precurriculum and postcurriculum periods. The mean HbA1c did not change from baseline (7.7%) to follow-up (7.6%, P = .41).
Table 1.
Resident Survey Responses to Panel Management Activity (N = 41)a
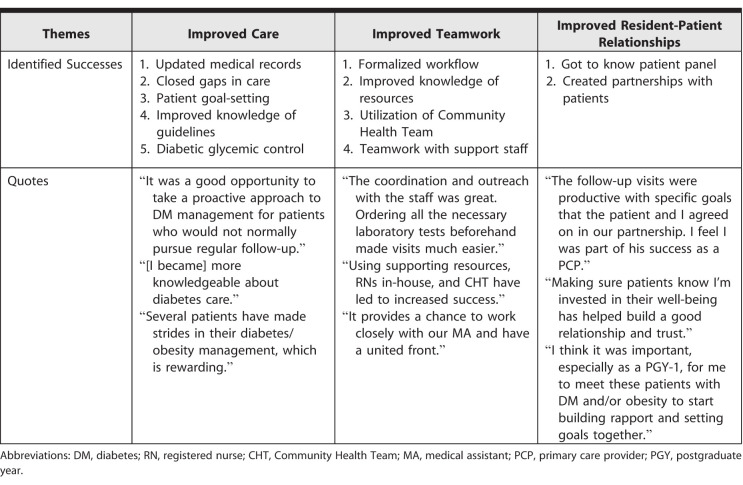
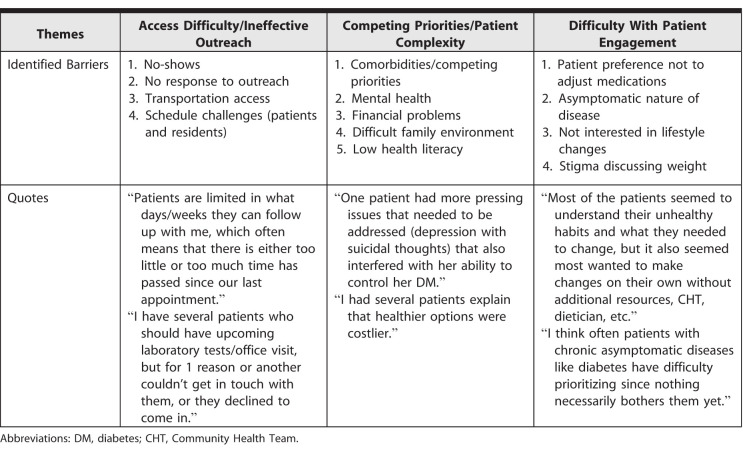
In residents' reflections, major themes emerged as successes (Table 2) and barriers (Table 3) to improving care for empaneled patients. One resident noted, “Having objectives and going through the modules reminded me to set goals and provide more consistent and recommended care.” Despite often citing difficulty with patient engagement, residents demonstrated resiliency in their reflections. One resident noted, “It has been overall a very welcoming experience and taught me to always practice patience because there are things I cannot control, so all I can do is keep trying to help my patients and hope/believe they will get there someday.”
Table 2.
Major Themes for Successes Based on Resident Responses
Table 3.
Major Themes for Barriers Based on Resident Responses
Discussion
Our findings suggest that, from the residents' perspective, the panel management curriculum increased ownership of patient care, interdisciplinary teamwork, and self-management goal-setting. Average HbA1c values remained unchanged. The worksheet data demonstrated a relatively high rate of appointments scheduled, laboratory tests ordered, and CHT referrals offered, and reflections allowed identification of successes and barriers of the curriculum.
Few studies have looked at panel management curricula in residency.11–14,18 Most focused on clinical outcomes based on health metrics and processes of care measures, such as completion of laboratory tests, vaccinations, or visits.11–14 In our study, residents reported increased processes of care, which is concurrent with previous work.11–14 Our findings were not consistent with the majority of studies that showed modest improvements in quality metrics, such as glycemic, lipid, and blood pressure control.11,12,14 The lack of improvement in HbA1c may have been due to the small sample of patients who had HbA1c values in both the pre- and postintervention periods, the relatively low baseline mean HbA1c limiting room for improvement, and potentially inadequate amount of time until follow-up to show meaningful change in these values. Additionally, we collected HbA1c data for this analysis based on the presence of diabetes on patient problem lists, which may have underrepresented the true population in our resident clinic.
To our knowledge, this is the first study to identify major themes for successes and barriers of a panel management curriculum from a resident perspective. Previous studies have assessed learner outcomes, consisting of self-reported improvements in panel management skills, confidence in chronic care delivery, self-management goal-setting, and/or sustained behavior change, but most studies did not elaborate about what residents felt was successful about the curricula.13,14,18 Our thematic analysis of residents' reflections on successes and barriers can inform further work by identifying particularly strong elements of a panel management curriculum as well as elements that may need improvement. In our case, the teamwork element of the curriculum and the positive effect on resident-patient relationships were key strengths identified by residents. This may be attributable to the longitudinal, 5-month structure of our curriculum, which also differs from others.11–14,18
Our panel management curriculum meets ACGME core competencies in patient care and practice-based learning and improvement in the Chronic Care Model, and it successfully engages residents in this work. The curriculum was well received by residents. This type of positive clinic experience may promote career choices in primary care, which are likely important given the role of primary care in improving population health.19,20 Previous research has suggested that physicians tend to close gaps in performance and strive for standardized care when they are aware of those gaps.21–23 The curriculum can be integrated into existing didactic core ambulatory curricula, and the panel management support staff role can be filled by an MA, LPN, or RN. The model is adaptable to program structures and is transferrable to other chronic diseases and preventative health metrics. Since the introduction of the curriculum, we have continued the same longitudinal model for 2 years on these topics: chronic obstructive pulmonary disease/asthma/smoking, hypertension, and shared decision making in prostate cancer screening. As residency programs across the country work to integrate panel management and quality improvement skills into graduate medical education, our curriculum and findings can provide valuable guidance and insight into execution of similar education initiatives.
Limitations of our study included the lack of assessment of resident behavior change over time and the fact that our survey, worksheet, and reflection materials were without evidence of validity. Additionally, the findings of this single institution study may not generalize to other residency programs with differing scheduling systems, support staff resources, or patient populations. The feasibility of implementation of our curriculum across other programs may also be limited by accessibility to electronic health records and the ability to run patient registries. Lastly, we were unable to show significant differences between the primary care and categorical residents' responses, except for categorical residents feeling less familiar with CHT resources.
Further investigation with larger samples and multiple institutions may help to distinguish whether differences exist between primary care and categorical residents' perspectives on panel management curricula. The access barriers cited by residents present opportunities for innovation in resident clinic schedules and further community-based creativity in addressing social determinants of health and patient-centered research on alternative forms of outreach and connection.24 Residents cited difficulty with patient engagement as limiting their success in improving their patients' health; further panel management curricular work could include measuring patient engagement and resident education in tools and techniques, such as motivational interviewing to better equip residents.25 We plan to incorporate assessment of resident knowledge and behavior change as we study ongoing iterations of our curriculum.
Conclusion
Our panel management curriculum promoted resident skills in multiple ACGME core competencies and fostered ownership of patient care and interdisciplinary teamwork in a resident diabetic and obese clinic patient population. Although mean HbA1c remained unchanged, residents reported improved patient care. The curriculum was feasible, acceptable to residents, and has continued for 2 years with quality metrics.
Supplementary Material
References
- 1.Berwick DM, Noland TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the Chronic Care Model, part 2. JAMA. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 4.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality of improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–2261. doi: 10.1016/S0140-6736(12)60480-2. [DOI] [PubMed] [Google Scholar]
- 5.[AHRQ] Agency for Healthcare Research and Quality. Practice Facilitation Handbook. Module 20. Facilitating Panel Management. Rockville, MD: AHRQ; http://www.ahrq.gov/professionals/prevention-chronic-care/improve/system/pfhandbook/mod20.html Published May 2013. Accessed August 1, 2018. [Google Scholar]
- 6.Neuwirth EE, Schmittdiel JA, Tallman K, et al. Understanding panel management: a comparative study of an emerging approach to population care. Perm J. 2007;11(3):12–20. doi: 10.7812/tpp/07-040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.[ACGME] Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in internal medicine. http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/140_internal_medicine_2017-07-01.pdf?ver=2017-06-30-083345-723 Published July 1, 2009. Updated July 1, 2017. Accessed August 1, 2018.
- 8.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29(5):799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T, Willard-Grace R. Teamlets in primary care: enhancing the patient and clinician experience. J Am Board Fam Med. 2016;29(1):135–138. doi: 10.3122/jabfm.2016.01.150176. [DOI] [PubMed] [Google Scholar]
- 10.Wagner EH, Flinter M, Hsu C, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract. 2017;18(1):13. doi: 10.1186/s12875-017-0590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiPiero A, Dorr DA, Kelso C, et al. Integrating systematic chronic care for diabetes into an academic general internal medicine resident-faculty practice. J Gen Intern Med. 2008;23(11):1749–1756. doi: 10.1007/s11606-008-0751-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salem JK, Jones RR, Sweet DB, et al. Improving care in a resident practice for patients with diabetes. J Grad Med Educ. J Grad Med Educ. 2011;2011;33(3)(2):446. 196–202. doi: 10.4300/JGME-D-10-00113.1. published correction appears in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janson SL, Cooke M, McGrath KW, et al. Improving chronic care of type 2 diabetes using teams of interprofessional learners. Acad Med. 2009;84(11):1540–1548. doi: 10.1097/ACM.0b013e3181bb2845. [DOI] [PubMed] [Google Scholar]
- 14.Holmboe ES, Prince L, Green M. Teaching and improving quality of care in a primary care internal medicine residency clinic. Acad Med. 2005;80(6):571–577. doi: 10.1097/00001888-200506000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Sisson SD. (2017) Diagnosis and management of type 2 diabetes mellitus. http://www.peaconline.org Accessed August 1, 2016.
- 16.Gudzune K, Chaudhry ZW, Clark JM. Obesity module for PEAC. (2017) http://www.peaconline.org Accessed August 1, 2016.
- 17.Green J, Thorogood N. Beginning data analysis. In: Green J, Thorogood N, editors. Qualitative Methods for Health Research 3rd ed. London, England: Sage; 2014. pp. 209–217. [Google Scholar]
- 18.Kaminetzky CP, Beste LA, Poppe AP, et al. Implementation of a novel panel management curriculum among interprofessional health care trainees. BMC Med Educ. 2017;17(1):264. doi: 10.1186/s12909-017-1093-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peccoralo LA, Tackett S, Ward L, et al. Resident satisfaction with continuity clinic and career choice in general internal medicine. J Gen Intern Med. 2013;28(8):1020–1027. doi: 10.1007/s11606-012-2280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laponis R, O'Sullivan PS, Hollander H, et al. Educating generalists: factors of resident continuity clinic associated with perceived impact on choosing a generalist career. J Grad Med Educ. 2011;3(4):469–474. doi: 10.4300/JGME-D-10-00227.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duffy FD, Holmboe ES. Self-assessment in lifelong learning and improving performance in practice: physician know thyself [comment] JAMA. 2006;296(9):1137–1139. doi: 10.1001/jama.296.9.1137. [DOI] [PubMed] [Google Scholar]
- 22.Hildebrand C, Trowbridge E, Roach MA, et al. Resident self-assessment and self-reflection: University of Wisconsin-Madison's five-year study. J Gen Intern Med. 2009;24(3):361–365. doi: 10.1007/s11606-009-0904-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyers FJ, Weinberger SE, Fitzgibbons JP, et al. Alliance for Academic Internal Medicine Education Redesign Task Force. Redesigning residency training in internal medicine: the consensus report of the Alliance for Academic Internal Medicine Education Redesign Task Force. Acad Med. 2007;82(12):1211–1219. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 24.Lee PT, Friedberg MW, Bowen JL, et al. Training tomorrow's comprehensive primary care internists: a way forward for internal medicine education. J Grad Med Educ. 2013;5(2):187–191. doi: 10.4300/JGME-D-12-00134.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunhill D, Schmidt S, Klein R. Motivational interviewing interventions in graduate medical education: a systematic review of the evidence. J Grad Med Educ. 2014;6(2):222–236. doi: 10.4300/JGME-D-13-00124.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.