Abstract
Objectives:
This study aimed to develop a scale that can measure the role competency of oncology nurses during shared decision-making process.
Methods:
A total of 226 oncology nurses who actively provide direct care to patients from inpatient and outpatient oncology units in the Midwest and Pacific Northwest completed the online or mail survey. Exploratory factor analysis and parallel analysis showed the multidimensionality of the role competency scale on shared decision-making nurses.
Results:
The role competency scale on shared decision-making nurses revealed four dimensions: knowledge, attitudes, communication, and adaptability. The 22 items have excellent internal consistency with a Cronbach’s alpha of 0.91. The four subscales also have adequate reliability with Cronbach’s alpha >0.70 as well as greater than 0.70 Spearman–Brown’s correlation coefficients in split-half reliability testing for each subscale.
Conclusion:
The new scale has the potential to be used as a clinical tool to assess the need for shared decision-making education and training in oncology nurses.
Keywords: Shared decision-making, role competency, psychometric properties, oncology, hematology, nursing
The Agency for Health Care Quality and Research1 described shared decision-making (SDM) as a health care delivery model that requires the clinician to involve the patient in decisions about health care thereby fostering patient-centered care. The Institute of Medicine (IOM) defined patient-centered care as providing care that respects and responses to individual patient preferences, needs, and values, and ensures patient values as the primary guide in all clinical decisions.2 SDM has been considered the crux of patient-centeredness in health care delivery. In hematology–oncology practice setting, the roles of the oncology nurse in SDM have been recently examined and described as evolving, and these roles include key team member roles.3,4
In recent years, oncology care has emerged into a new era of significant patient participation during cancer treatment decision-making as exemplified by the SDM model of care delivery. According to SDM model, patient is at the center of care delivery. The SDM model of care has replaced the paternalistic (doctor knows everything mantra), physician-driven health care delivery model in contemporary oncology practice.5 Patients with cancer and their families are now encouraged to participate with members of the health care team in planning and deciding their treatment course.6,7 Two systematic literature reviews revealed that SDM is preferred by patients diagnosed with cancer.8,9
The SDM model of care delivery is embedded in the 2010 Affordable Care Act10 and is engineered to empower patients by placing them at the center of health care delivery. As health care clinicians, nurses must recognize that an engaged patient is an important component of excellent nursing care.11 According to the Oncology Nursing Society (ONS), an essential core competency for the oncology nurse is to advocate for the delivery of high-quality, patient-centered cancer care.12 The SDM care delivery model positioned the patient in the middle of all decision-making processes.13
Little is known on the oncology nurses’ knowledge, attitudes, and skills (KAS) on SDM. KAS are among the top constructs of competency.14 One study found that oncology nurses value their participation and contribution to the cancer treatment SDM process, and they believed having an influence on the final cancer treatment decisions, though at varying degrees.15 In response to IOM’s paper2 that highlighted SDM as a model for 21st century health care, oncology nursing experts pointed out that oncology nurses are front and center in the SDM care delivery model, and are well situated to empower patients to communicate their needs, values, and preferences.11 A recent study examined the roles of the oncology nurses in SDM and found that patient education, information giving to multidisciplinary team, psychological support, side-effect management, and patient advocacy are at the top of the list of these roles.16
In today’s climate of SDM care delivery model, the oncology nurse’s role competency in the SDM process is critical to acquire and evaluate. Nurses spend more time with patients diagnosed with cancer than other care clinicians and are a trusted source of information for patients and their families.17 Nurses are not silent bystanders in the cancer treatment decision-making process. They are reliable and fierce advocates, particularly when patients cannot advocate for themselves.16 SDM is underutilized in clinical practice18 and nurses can enhance SDM process for patients.
SDM measurement tools for clinicians have been developed in other disciplines, but none of them address the nursing role in SDM.19 The three most frequently used SDM questionnaires, namely, the OPTION (observing patient involvement) scale developed by Elwyn et al.,20 COMRADE, a patient-based outcome measure21 and the SDM-Q-9 scale (9-item SDM questionnaire) are focused on measuring the patient involvement in the context of patient–physician relationship.22 Similarly, the Decision Analysis System-Oncology (DAS-O) tool focused on identifying and rating the quality of SDM in breast cancer consultations with physicians23 while the Decision Support Analysis Tool (DSAT) focused on the evaluation of clinicians’ use of decision support and related communication skills.24
To date, there is no existing SDM tool specifically developed to measure the nurse’s involvement in the oncology SDM process. In the United Kingdom, clinicians including nurses have expressed the need for more guidance and clarity on what is SDM25 and the roles that oncology nurses play in the SDM process need to be elucidated. Hence, this study is aimed at developing an instrument that can measure the role competency of oncology nurses throughout the SDM process. The research question for this study was what are the factors that are statistically related for latent variables of SDM competency such as KAS among practicing oncology nurses?
A validated and reliable role competency instrument for SDM in nurses (SDM-N) will allow administrators and researchers to measure areas of strengths and weaknesses on nurses’ role competency in terms of their KAS on SDM process, which can identify opportunities for tailored education and training on SDM.
Theoretical frameworks
SDM care delivery model
Charles et al.26,27 defined SDM as a model of health care delivery requiring a dyadic relationship where the clinician and the patient are closely interacting, listening, and exchanging information including patient-specific personal preferences. This SDM dyad demonstrated the benefits associated with mutually agreeable treatment decisions such as increased patient satisfaction and adherence to therapy.5 Charles et al.27 posited that SDM is a dynamic process that is valued by both the clinician and the patient.
Recognizing that SDM is a dynamic process involving many individuals and can continue to evolve throughout the decision-making continuum, Charles et al.26 published a follow-up paper 2 years later with a revised framework which outlined the following elements of the revised SDM model:
Different analytic steps in the treatment decision-making process;
A dynamic view of treatment decision-making by recognizing that the approach adopted at the outset of a medical encounter may change as the interaction evolves;
Identifies SDM as a decision-making approach situated between paternalistic and informed model of care delivery;
Practical applications for clinical practice (with non-physician clinicians’ involvement in SDM process), research, and medical education.
The revised framework emphasized that SDM is a process that happens over time and requires flexibility on the clinician to respect patient preferences. Factors involved with the clinician and patient play into this process, including the clinician’s choices based on system barriers, clinician’s preference, and available clinical data, as well as the patient’s choices based on personal values, preferences, and influences.26
Since the inaugural publication of SDM model by Charles et al.27 in 1997, which critically examined what SDM really means, many other SDM models of care delivery have been proposed such as the Communication Model of SDM in 2005,28 the Integrative SDM Model for Medical Encounters in 2006,29 the Interprofessional Model of SDM in 2011,30 the revised Three-Talk Model for SDM in 2017,31 and most recently, the SDM Model for Nursing Practice in 2018.32 The majority of aforementioned proposed models of SDM is mostly theoretical and lack validation of structural constructs and concepts in actual practice.
The evolving role in SDM process: nursing framework
Over the span of time, the SDM process evolved to include nurses in this SDM care delivery model in the cancer setting. With the shift to patient-centered care, oncology nurses have greater involvement during pivotal periods of the decision-making process. Oncology nurses function in many roles which include assessing, supporting, evaluating outcomes, providing information, and advocating for the patient during the SDM process.3 With the SDM model of care delivery, oncology nurses have evolving roles that indicate a higher level of participation throughout the SDM process.
Work cultures, clinical experience, knowledge, skills, and negative attitudes are barriers that can impact the nurses’ role competency in the SDM process.3 Nurses must be aware of these barriers and be cognizant of their roles throughout the entire SDM process. Awareness of these barriers and the delineation and development of nurse’s role in SDM can improve the nurse’s role competency during the SDM process, resolving some of the barriers to SDM. Consequently, increasing nurses’ participation at various time points of the SDM process can lead to better patient outcomes.3 Measuring KAS of the nurses within the context of SDM process can help nurse administrators and nurse educators design interventions or training that can improve nurses’ role competency on SDM process as described in the updated paper on SDM by Charles et al.26
Methods
Design
This study utilized an instrument development design with the use of an online survey to collect the data for establishing the psychometric properties of the role competency scale in SDM among oncology nurses.
Participants
A sample of 226 oncology nurses participated in this study. They were stratified using four educational level strata, namely, associate, bachelor, master, and doctorate. The sample frame was composed of three large ONS chapters in the Midwest and Pacific Northwest regions of the States. The ONS chapter members were recruited to participate in the study through the individual chapter’s email listserv. The sample was stratified by educational level to obtain a representative sample of ONS members who provide direct care to patients with a cancer diagnosis. The sampling calculations were based on the overall membership data provided by the Director of Membership, ONS Headquarter in Pittsburgh, PA.
Sample size
Exploratory factor analysis (EFA) requires that at least 10 subjects should be accounted for each variable and this has served as the basis for determining the study sample size.33 Given that the SDM-N has a total of 22 initial items (22 × 10 = 220), 220 became the study sample accrual goal. A total of 226 oncology nurses were successfully enrolled in this study (N = 226).
Inclusion and exclusion criteria
All study participants met the following inclusion criteria: at least 18 years of age, able to give consent, speak and understand English language, and actively provide direct patient care. The exclusion criteria include non-English speaker due to lack of available interpreter for the SDM-N scale and nurses who provide indirect patient care (e.g. nurse educator, pharmaceutical nurse liaison or nursing administrators who have no direct patient care responsibilities). The demographic questionnaire asked potential participants whether they are practicing nurses and how many years they have been practicing as nurses to verify eligibility for study participation.
Procedures and materials
The online survey was distributed to the members of three large chapters of the ONS, the professional organization of oncology nurses in the United States. The study participants completed the online survey through Qualtrics, an online research enterprise platform,34 at home or at work where a computer was available. To ensure an adequate sample size, snowball sampling was also employed. ONS members who received the survey link of the Qualtrics online survey were allowed to forward the survey link via email or share the mailed paper-based SDM-N instrument directly to oncology nurses who are actively providing direct care to patients with cancer to achieve the study accrual goal. Due to unknown number of ONS members who opted out of email listserv or US postal mail service from their chapters, the overall survey response rate cannot be estimated.
Instrument
The role competency scale for SDM-nurses also known as SDM-N scale (Supplementary Appendix A) and the sociodemographic questionnaire (Supplementary Appendix B) were sent to three ONS large chapter members via an online survey platform called Qualtrics. The 22 initial items in the SDM-N instrument have been generated and developed using two theoretical frameworks: the SDM model of care delivery26,27 and the evolving role of the nurse in SDM nursing framework.3 Each item in the scale was deductively generated from the constructs of these two models to ensure validity, reliability, and utility of future study results.35 Items in the Attitudes subscale were generated from earlier work of McCarter et al.16 on barriers and promoters of SDM among oncology nurses. The SDM-N scale is designed (a priori) to measure KAS within the context of SDM process because KAS are considered as key constructs of competency according to Hay Group, Inc.14
Recruitment and data collection procedures
The ONS protocol for survey participant selection and stratification by educational attainment was followed in order to achieve a research study sample that best represents the overall ONS membership.36 The sample for this study consisted of oncology nurses who were stratified based on educational level (a representative sample of overall ONS membership with diploma), associate and bachelor degrees (118 participants), and an oversampled advanced practice nurses (APNs) with master degrees (87 participants) and doctoral degrees (19 participants). Oversampling of APNs with master degree and doctoral degrees is needed to have a representative sample of these ONS members.36
A University Institutional Review Board (IRB) Committee approval was obtained prior to recruitment. A mailed survey was sent after the Qualtrics online survey launch because over 300 members in one of the three ONS chapters opted out the email listserv system. The President of the three large ONS chapters sent out the web link for the online Qualtrics survey containing the SDM-N scale (Supplementary Appendix A) and the sociodemographic questionnaire (Supplementary Appendix B) to their members. The paper-based SDM-N scale and sociodemographic questionnaire along with pre-paid, self-addressed return envelopes were sent out by the principal investigator and study research personnel via the US postal mail service.
Ethical considerations
The principal investigator and research personnel completed the online Collaborative Institutional Training Initiative at the University of Miami’s Human Subjects Research training program. IRB approval was obtained from a University IRB Committee. The online and paper-based questionnaires did not contain any personal identifiable information. All printed records were kept in a locked cabinet in a secured room of the principal investigator. Electronic records from Qualtrics online survey platform were kept on a computer that is password protected at all times.
Data analytic procedures
Initial content validity
Initial content validity of SDM-N was completed by an expert panel of six oncology nurses (one with a doctorate degree, four with master’s degrees, and one with a bachelor’s degree in nursing). The content experts comprehensively graded the 22 individual Likert-type survey questions in the SDM-N scale using the content validity index for scales.37 Each item was graded for clarity, relevance, simplicity, and consistency using a 10-point Likert-type scale. Clarity: score of 1 = unclear, score of 10 = very clear; Relevance: score of 1 = not relevant, score of 10 = high relevance; Simplicity: score of 1 = very complex and confusing, score of 10 = simple and easy to understand; Consistency: score of 1 = inconsistent, score of 10 = high consistency. The initial content validity results were deemed satisfactory and they are shown in Table 1.
Table 1.
Expert panel’s initial content validity of the 22 pool items.
| Domain | Clarity | Relevancy | Simplicity | Consistency |
|---|---|---|---|---|
| Knowledge | 87.70 | 94.37 | 88.95 | 93.33 |
| Attitudes | 90.83 | 96.87 | 93.12 | 96.45 |
| Skills | 91.00 | 97.33 | 91.33 | 96.00 |
Face validity
After the initial content validity was established by the study researchers, 10 practicing oncology nurses were asked to read the 22 items in SDM-N scale and they were asked to answer one question: How well do you think the SDM-N scale measures KAS of the oncology nurse throughout the SDM process? A 4-point Likert-type scale was used: 1 = not at all, 2 = very little, 3 = somewhat, 4 = to a great extent. Eight respondents rated the SDM-N as 4. The average time to complete the SDM-N was 20 min based on the data obtained during face validity.
Construct validity
Data were analyzed for construct validity using EFA. Parallel analysis (PA) was used to determine how many factors should be retained for the final model that best represents the SDM-N scale. EFA was performed to analyze the 22 items in the SDM-N to see if there are identifiable groups of variables that are statistically related and make conceptual sense to group together. EFA is widely applied to both the development of scale and the development of theory.38 The principal axis factoring approach and PA techniques were used in deciding how many factors will be retained, as it is the most evidence-based and most accurate method of determining the number of factors to retain in EFA.38,39 Oblique rotation strategy was employed as it is more consistent with reality.38
Reliability testing procedures
Cronbach’s alpha coefficient
All items in the subscales were individually assessed for evidence of internal consistency using Cronbach’s alpha coefficient.40 The reliability of the four subscales of SDM-N (Knowledge, Attitudes, Communication, and Adaptability subscales) was deemed reliable if the Cronbach’s alpha is ⩾0.7.40
Split-half reliability
In order to further assess the reliability of SDM-N scale, a series of split-half reliability tests were performed on the SDM-N subscales as suggested by DeVellis.40 Split-half reliability is indicated when a scale does not have any alternate form (to the best of the authors’ knowledge, this is the first instruments designed to measure KAS during SDM-N). It can be performed by dividing the set of items in a subscale into two subsets and correlating the subsets to assess reliability.40 These split-half reliability tests examined the extent to which the SDM-N scale is consistent within itself. Essentially, each subscale was divided into two halves and Spearman–Brown’s correlation test statistics were performed to determine whether there were circumstances where the halves were weakly correlated with each other. Theoretically, when a measure includes multiple items, split halves created from subsets of the items in a subscale should be strongly correlated with each other.40 According to DeVellis,40 the threshold for split-half reliability using Spearman-Brown’s equal length coefficient should be ⩾0.70.40
Descriptive analysis
Sociodemographic data were entered into IBM SPSS version 19. Descriptive statistics such as frequencies, percentages, and cumulative percents were used to examine and describe the study participants’ characteristics. The means, standard deviations, and percentages of extreme values (i.e. 1 = strongly disagree and 5 = strongly agree) for each item of the SDM-N scale were examined for any floor (extremely low responses) or ceiling (extremely high responses) effect.
Results
Demographics of study participants
A total of 226 oncology nurse participants who provide direct care to patients with cancer completed the online or mailed questionnaire known as the SDM-N scale. Of which, 95% of study participants were women (n = 213) and 5% were men (n = 12), 83% worked full time (n = 184) and 17% were persons of minority and mixed race. Out of the 226 participants, 47% (n = 105) had a bachelor’s degree in nursing and 52% had 21 years or more clinical experience. Only 8.5% were between the age of 20 and 29 years.
Table 2 shows the sociodemographic features of study participants. The representativeness of study sample was adequate after comparing the sociodemographic descriptive statistics of the study sample and the population of interest (i.e. overall ONS membership). No extreme discordance was seen in terms of gender, employment status, age groupings, and ethnicity between the study participants (N = 226) and the overall ONS membership (N = 37,650) based on previous data reported by Doorenbos et al.36 Oversampling of the ONS members with doctoral and master’s degrees coupled with aggressive recruitment using online and regular US mail survey approaches yielded a representative sample of the study population of interest.
Table 2.
Demographics of study participants (N = 226).
| Variables | Frequency | % |
|---|---|---|
| Gender | ||
| Female | 213 | 94.7 |
| Male | 12 | 5.3 |
| Age groups (years) | ||
| 50–59 | 71 | 31.7 |
| 60 and above | 52 | 23.2 |
| 40–49 | 42 | 18.8 |
| 30–39 | 40 | 17.9 |
| 20–29 | 19 | 8.5 |
| Missing | ||
| Employment status | ||
| Full time | 184 | 83.3 |
| Part time | 33 | 14.9 |
| Per Diem | 4 | 1.8 |
| Missing | ||
| Years of oncology experience (years) | ||
| 21+ | 116 | 51.8 |
| 11–15 | 35 | 15.6 |
| 0–5 | 29 | 12.9 |
| 6–10 | 28 | 12.5 |
| 16–20 | 16 | 7.1 |
| Highest nursing degree attained | ||
| Bachelor’s degree | 105 | 46.9 |
| Master’s degree | 87 | 38.8 |
| Doctoral degree | 19 | 8.5 |
| Associate’s degree | 13 | 5.8 |
| Diploma | 0 | 0 |
| Missing | ||
| Ethnicity (n = 329) | ||
| Caucasian | 187 | 83.5 |
| Asian | 22 | 9.8 |
| Hispanic | 8 | 3.6 |
| Black | 4 | 1.8 |
| Mixed | 3 | 1.3 |
Descriptive statistics of the 22 items
Item mean scores
Descriptive statistics showed that item 11 (I have the skills to assess for the side effects of cancer treatment.) and item 12 (I advocate on behalf of my patient during the cancer treatment SDM process if needed) had the highest mean scores of 4.65, whereas item 15 (I can evaluate the outcomes of cancer treatment SDM) and item 1 (I have enough time to participate in SDM) had the lowest mean scores of 3.76 and 3.58, respectively. The mean scores for each item in the four subscales are above the neutral point (3 = neither disagree nor agree).
Floor and ceiling effect
After a careful review of the descriptive statistics of the 22 items in the SDM-N scale, no floor effect was seen. The ceiling effect was examined and observed in a few items in Knowledge and Communication subscales (i.e. more than 30% of the total respondents selected the most extreme response of “5 = strongly agree”). When ceiling effect occurs, it could lead to a reduced variance that lowers the sensitivity of the Knowledge or Communication subscales to determine whether there are mean score differences in outcome variables such as knowledge and communication skills between two groups in a research study (e.g. pre-test versus post-test group mean scores or treatment versus placebo group mean scores). If this occurs in the future use of the scale, probit analysis can overcome the ceiling effect issue.41,42
Construct validity, factorability, and reliability procedures
The Kaiser–Meyer–Olkin (KMO) measure was developed based on the assumption that controlling for the effects of other variables, the partial correlations between pairs of variables should be small if the variables share common factors.33 A KMO of 0.80 or greater means the correlation among variables is high and factor analysis (factorability) is best suited to the data obtained.33 In this study, the KMO was 0.909 indicating adequacy of sample and it confirmed EFA as a good model for the data collected in this study. In addition, Bartlett’s test of sphericity was used to test the null hypothesis that the correlation matrix has all coefficients not in the diagonal are equal to zeroes. In this study, Bartlett’s test was statistically significant (p < 0.001) and the null hypothesis was rejected indicating that all the coefficients not in the diagonal are greater or lesser than zeroes as seen in Table 3.
Table 3.
KMO and Bartlett’s test.
| Kaiser–Meyer–Olkin measure of sampling adequacy. | 0.909 | |
| Bartlett’s test of sphericity | Approximate chi-square | 2149.186 |
| df | 231 | |
| Significance | 0.000 | |
In order to test the internal consistency of all 22 items in the SDM-N, Cronbach’s alpha coefficient was calculated and the results showed an excellent Cronbach’s alpha value of 0.913.40 Table 4 shows the item-total statistics with excellent corrected item-total correlation with all correlations with other variables found in the matrix to be between 0.30 and 0.70. The corrected item-total correlation data found in Table 4 met the critical assumption of EFA that states: correlations between variables should be substantial between 0.30 and 0.70 so that each variable correlates highly with at least one other variable.33
Table 4.
Reliability and item-total statistics.
| Reliability statistics | ||||
|---|---|---|---|---|
| Overall scale Cronbach’s alpha | No. of total items | |||
| 0.913 | 22 | |||
| Item-total statistics | ||||
| Individual items | Scale mean if item deleted | Scale variance if item deleted | Corrected item-total correlation | Cronbach’s alpha if item deleted |
| I have enough time to participate in shared decision-making | 90.12 | 83.109 | 0.433 | 0.914 |
| Shared decision-making is essential in contemporary oncology nursing practice | 89.14 | 86.258 | 0.490 | 0.911 |
| I certainly feel comfortable actively participating during the shared decision-making process | 89.44 | 83.206 | 0.652 | 0.907 |
| I play crucial roles that optimize patient outcomes related to treatment decisions | 89.55 | 81.954 | 0.606 | 0.908 |
| The patient is the focus throughout the shared decision-making process | 89.40 | 84.299 | 0.541 | 0.909 |
| Patients rely on more than just the physician to help them with cancer treatment decisions | 89.20 | 86.009 | 0.420 | 0.912 |
| My opinion is valued by patients and the medical team throughout the cancer treatment shared decision-making process | 89.55 | 83.369 | 0.639 | 0.907 |
Factor loading
Factor analysis was performed to answer the main research question of this study.
The factor analysis of all the 22 initial item pool indicated that these items seemed to represent four factors. The four factors have 8.07, 1.76, 1.5 and 1.19 initial eigenvalues, respectively, accounting for the total 57.27% cumulative variance. The scree plot for eigenvalues is shown in Figure 1. According to Yong and Pearce,43 the larger the N in the study, the cut-off for factor loading can be >6.0. Using this criterion, item 13 (I am capable of providing psychological support to my patient during SDM process) and item 18 (I understand that an exchange of information including personal preference between a patient and a clinician) were removed from the initial item pool because their factor loading scores were below 6.0. The final instrument included a total of 20 items out of the 22 item pool and these 20 items are shown in Supplementary Appendix A.
Figure 1.
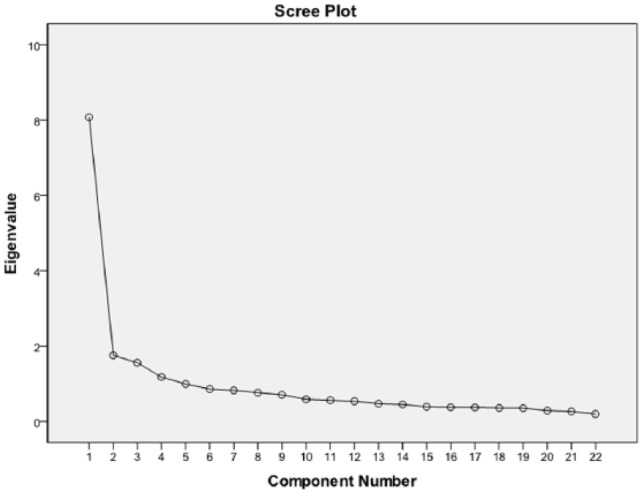
Scree plot of eigenvalues demonstrating four factors with eigenvalue greater than 1.
Subscale reliability analyses
The PA determined that there are four valid subscales in the SDM-N scale. All four subscales have adequate to very good internal consistency as evidenced by Cronbach’s alpha coefficient values of ⩾0.70. These four subscales included KAS (Communications Skills subscale and Adaptability Skills subscale). They have Cronbach’s alpha coefficients of 0.81, 0.81, 0.76 and 0.83, respectively, as shown in Table 5. A Cronbach’s alpha of 0.80 or higher indicated a very good internal consistency of all the items in the Knowledge, Attitudes, and Adaptability Skills subscales while a 0.76 alpha value in the Communication Skills subscale indicated adequate and acceptable internal consistency of items.40
Table 5.
Results of the internal consistency reliability tests for Knowledge, Attitudes, Communication, and Adaptability subscales.
| Subscale | Total no. of subscale items | Cronbach’s alpha | Spearman–Brown’s coefficients |
|---|---|---|---|
| Knowledge | 4 | 0.81 | 0.80 |
| Attitudes | 8 | 0.81 | 0.83 |
| Communication | 4 | 0.76 | 0.73 |
| Adaptability | 4 | 0.83 | 0.89 |
A series of split-half reliability tests were performed on SDM-N subscales. These tests examined the extent to which a subscale is consistent within itself. Each of four subscales had correlation coefficients that met the split-half reliability threshold of 0.70 with the following Spearman–Brown correlation coefficient results: Knowledge (0.80), Attitudes (0.83), Communication Skills (0.73) and Adaptability Skills (0.90) as seen in Table 5. Given the results of Cronbach’s alpha and Spearman–Brown’s correlation statistical tests, we concluded that the items in the four SDM-N subscales have internal consistency and are therefore reliable measures.
Discussion
The SDM delivery model of care has evolved from a patient–physician model to one that involves the healthcare team. Oncology nurses have roles throughout the SDM process. To date, there has not been a role competency scale specifically developed to measure the KAS of the oncology nurse during the SDM process. The SDM-N described here is a self-report scale that describes the roles and measures the nurse’s competency in these roles throughout the SDM process. It has shown to be user-friendly (paper-based or online survey format), quick, and easy to complete (20 min average completion time) and it can be used as a reliable and valid tool to measure nurses’ KAS (communication skills and adaptability skills) as important components of competency on SDM.
The final SDM-N tool consisted of 20 items (from 22 initial items) which are organized into four subscales as identified by PA analytic procedure. All the subscales were found to have adequate internal reliability with Cronbach’s alpha and Spearman–Brown’s correlation coefficients greater than 0.70. Construct validity procedures including EFA and PA statistical tests supported the SDM-N scale as a valid instrument that can be used in measuring the oncology nurses’ KAS on the SDM process.
There was no floor effect seen, but ceiling effect should be examined each time a subscale of the SDM-N is used because it can potentially attenuate the relationships between independent and dependent variables. A special type of analysis called probit analysis, which is a method of analyzing the relationship between a dose and the quantal (all or nothing) response,42 should be used to analyze data whenever ceiling effect is observed (extreme values for the item represent ⩾30% of all responses) in order to avoid any incorrect conclusion that the dose (e.g. annual 1 h SDM education and training for nurses) has no effect on quantal response (e.g. nurses’ knowledge mean scores). The probit model analytic procedure, which is a variation of multiple regressions, is capable of producing correct inference when ceiling effects are present.41 The authors suggest the use of a probit analysis only if a ceiling effect is observed. No one can predict whether the next group of participants (e.g. urology nurses with very high rate of success on SDM implementation) will have a ceiling effect on the Knowledge or Attitude subscale. But if ceiling effect is observed, a probit analysis will be highly applicable on this instance to make meaningful conclusions.
DeVellis40 suggested that ceiling effects in survey research using Likert-type scaling can also be prevented by expanding the range of potential responses. This study has utilized the five-category response items for likelihood. A seven-category response rating scale (1 = strongly disagree, 2 = moderately disagree, 3 = mildly disagree, 4 = neither agree nor disagree, 5 = mildly agree, 6 = moderately agree and 7 = strongly agree) for Knowledge and Communication subscales may alleviate the ceiling effect seen, by giving the participants greater flexibility in choosing answers at the upper end of the response spectrum.40 Using a seven-category rating could potentially eliminate or reduce the extreme responses (5 = strongly agree), which produce the ceiling effect seen in the Knowledge and Communication Skills subscales.
Many tools are available to educate and measure physicians’ and patients’ interaction in the current SDM model of care delivery. However, no resources existed to evaluate the nurses’ role competency prior to this study. Prior research studies led to a nursing model of SDM with constructs describing several complex and evolving roles of the oncology nurse in SDM process. By combining the SDM framework from nursing3 with the SDM care delivery model by Charles et al.,26,27 the investigators’ goal of establishing a scale that can measure nurses’ role competency on SDM has been achieved.
To date, the SDM-N scale is the first and the only scale that has been developed by nurses for nurses and it is validated by practicing oncology nurses. The SDM-N scale can now be used as a clinical tool to evaluate oncology nurses’ KAS related to the SDM process. The addition of SDM-N in the array of instruments to measure SDM in medical oncology clinic encounter is a step in the right direction toward the measurement of SDM through an interdisciplinary team approach. The SDM-N will allow researchers to quantitatively report the contributions of nurses throughout the SDM process.
Participation in SDM is essential for all health care providers in today’s climate of patient-centeredness in healthcare. Nursing leaders and other healthcare administrators with vision for fully embracing the SDM care delivery model must see the need to implement valid and reliable tools that can evaluate the role competency of oncology nurses throughout the SDM process. Oncology nurses must be educated and trained on SDM in order to improve patient-reported decisional outcomes associated with SDM such as increased patient satisfaction with decision and reduced patient decisional regret43 and well as team work in the health care team.4
Scoring
Clinical researchers may want to know what score on the competency scale for SDM-N would indicate a competent level. We propose 80% of the highest possible summary score be used as the threshold score for the competency level for each subscale. This proposed threshold score is based on the scale’s rating of 4 (in a 1 to 5 Likert-type scale) as the point where self-report of competency has been reached. There are several permutations based on individual scores from each item in a subscale that can have 80% sum score. Therefore, one must be cautious in examining the sample score on each item in every subscale to avoid missing serious knowledge or skill deficits. Descriptive statistics using mean, median or mode must be examined for each item in each subscale of the SDM-N to detect significant deficits.
The SDM-N does not measure nurse’s level of involvement. However, the authors hypothesized that a highly competent nurse on SDM will likely have higher level of participation in SDM process. Higher education has been reported having a positive correlation with higher clinician’s level of participation.18 To measure the level of participation among nurses, a separate valid and reliable instrument must be developed for this specific construct on level of participation. Testing of hypothesized correlations of education with SDM-N competency score and the level of participation in SDM among nurses must be conducted in future studies to test any positive or negative associations of these variables.
Study limitations
Several limitations of this study included a small sample of oncology nurses which may limit the generalization of the findings to overall nurse populations from other nursing specialties (e.g. urology, cardiology, and orthopedic nurses). It was not possible to perform concurrent validity because there was no comparable instrument available. Subscale items with ceiling effects are also a limitation of this study, but the use of probit model of multiple regressions can overcome this limitation. The major strength of this study is the rigorous application of the most recent scale development procedures such as item development using a deductive approach as outlined by DeVellis40 and the use of the most up-to-date analytic procedures for factor analysis as described by Ledesma and Valero-Mora.39
Conclusion
The SDM-N scale was found to be a valid and reliable instrument that can be used as a clinical tool to measure the KAS of oncology nurses throughout the SDM process. A confirmatory factor analysis must be tested in future validation studies using new data set to further validate the results from this newly developed instrument. The new SDM-N instrument showed adequate psychometric properties, but further refinement of the instrument such as the use of seven category response rating and additional validation of the scale in other nursing specialties (e.g. urology, cardiology, and orthopedics) would further strengthen the validity of this new instrument.
Supplemental Material
Supplemental material, Appendix_A for Role competency scale on shared decision-making nurses: Development and psychometric properties by Joseph D Tariman, Pamela Katz, Jessica Bishop-Royse, Lisa Hartle, Katharine L Szubski, Toreend Enecio, Ima Garcia, Nadia Spawn and Katherine Jones Masterton in SAGE Open Medicine
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study has been approved by the DePaul University Institutional Review Board.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Chicago Chapter of Oncology Nursing Society.
Informed consent: All study participants have given informed consent prior to study participation.
ORCID iD: Joseph D Tariman:  https://orcid.org/0000-0002-4986-2627.
https://orcid.org/0000-0002-4986-2627.
References
- 1. Agency for Healthcare Quality and Research. Shared decision making, 2013, https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html
- 2. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: The National Academies Press, 2001. [PubMed] [Google Scholar]
- 3. Tariman JD, Szubski KL. The evolving role of the nurse during the cancer treatment decision-making process: a literature review. Clin J Oncol Nurs 2015; 19(5): 548–556. [DOI] [PubMed] [Google Scholar]
- 4. Agency for Healthcare Quality and Research. TeamSTEPPS 2.0, 2015, https://www.ahrq.gov/teamstepps/instructor/fundamentals/index.html
- 5. Kehl KL, Landrum MB, Arora NK, et al. Association of actual and preferred decision roles with patient-reported quality of care: shared decision making in cancer care. JAMA Oncol 2015; 1(1): 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kane HL, Halpern MT, Squiers LB, et al. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin 2014; 64(6): 377–388. [DOI] [PubMed] [Google Scholar]
- 7. Politi MC, Studts JL, Hayslip JW. Shared decision making in oncology practice: what do oncologists need to know? Oncologist 2012; 17(1): 91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh JA, Sloan JA, Atherton PJ, et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care 2010; 16(9): 688–696. [PMC free article] [PubMed] [Google Scholar]
- 9. Tariman JD, Berry DL, Cochrane B, et al. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol 2010; 21(6): 1145–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013; 368(1): 6–8. [DOI] [PubMed] [Google Scholar]
- 11. Ferrell B, McCabe MS, Levit L. The Institute of Medicine report on high-quality cancer care: implications for oncology nursing. Oncol Nurs Forum 2013; 40(6): 603–609. [DOI] [PubMed] [Google Scholar]
- 12. Oncology Nursing Society. Oncology nurse generalist competencies, 2016, https://www.ons.org/sites/default/files/Oncology%20Nurse%20Generalist%20Competencies%202016.pdf
- 13. Gillick MR. Guiding the guardians and other participants in shared decision making. JAMA Intern Med 2015; 175(10): 1691–1692. [DOI] [PubMed] [Google Scholar]
- 14. Hay Group, Inc. Using competencies to identify high performers: an overview of the basics, 2003, http://www.haygroup.com/downloads/uk/competencies_and_high_performance.pdf
- 15. Tariman JD, Mehmeti E, Spawn N, et al. Oncology nursing and shared decision making for cancer treatment. Clin J Oncol Nurs 2016; 20(5): 560–563. [DOI] [PubMed] [Google Scholar]
- 16. McCarter SP, Tariman JD, Spawn N, et al. Barriers and promoters to participation in the era of shared treatment decision-making. West J Nurs Res 2016; 38(10): 1282–1297. [DOI] [PubMed] [Google Scholar]
- 17. Gallup Inc. Americans rate nurses highest on honesty, ethical standards, 2014, http://news.gallup.com/poll/180260/americans-rate-nurses-highest-honesty-ethical-standards.aspx
- 18. Couet N, Labrecque M, Robitaille H, et al. The impact of DECISION+2 on patient intention to engage in shared decision making: secondary analysis of a multicentre clustered randomized trial. Health Expect 2015; 18(6): 2629–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Légaré F, Ratté S, Stacey D, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2010; 5: CD006732. [DOI] [PubMed] [Google Scholar]
- 20. Elwyn G, Edwards A, Wensing M, et al. Shared decision making: developing the OPTION scale for measuring patient involvement. Qual Saf Health Care 2003; 12(2): 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Edwards A, Elwyn G, Hood K, et al. The development of COMRADE—a patient-based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Educ Couns 2003; 50(3): 311–322. [DOI] [PubMed] [Google Scholar]
- 22. Kriston L, Scholl I, Hölzel L, et al. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns 2010; 80(1): 94–99. [DOI] [PubMed] [Google Scholar]
- 23. Brown RF, Butow PN, Juraskova I, et al. Sharing decisions in breast cancer care: development of the decision analysis system for oncology (DAS-O) to identify shared decision making during treatment consultations. Health Expect 2011; 14(1): 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guimond P, Bunn H, O’Connor AM, et al. Validation of a tool to assess health practitioners’ decision support and communication skills. Patient Educ Couns 2003; 50(3): 235–245. [DOI] [PubMed] [Google Scholar]
- 25. Staveley I, Sullivan P. We need more guidance on shared decision making. Br J Gen Pract 2015; 65(641): 663–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999; 49(5): 651–661. [DOI] [PubMed] [Google Scholar]
- 27. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997; 44(5): 681–692. [DOI] [PubMed] [Google Scholar]
- 28. Siminoff LA, Step MM. A communication model of shared decision making: accounting for cancer treatment decisions. Health Psychol 2005; 24(4S): S99–S105. [DOI] [PubMed] [Google Scholar]
- 29. Makoul G, Clayman LM. An integrative model of shared decision making in medical encounters. Patient Educ Couns 2006; 60(3): 301–312. [DOI] [PubMed] [Google Scholar]
- 30. Legare F, Stacey D, Pouliot S, et al. Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. J Interprof Care 2011; 25(1): 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Elwyn G, Durand MA, Song J, et al. A three-talk model for shared decision making: multistage consultation process. BMJ 2017; 359: j4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Truglio-Londrigan M, Slyer JT. Shared decision-making for nursing practice: an integrative review. Open Nurs J 2018; 12: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kellar SP, Kelvin EA. Munro’s statistical methods for health care research. 6th ed. Philadelphia, PA: Wolters Kluwer, 2012. [Google Scholar]
- 34. Qualtrics. Qualtrics research core, 2018, https://www.qualtrics.com/research-core/
- 35. Schmidt LA. Keeping the theory in measurement. J Nurs Educ 2013; 52(11): 603–604. [DOI] [PubMed] [Google Scholar]
- 36. Doorenbos AZ, Berger AM, Brohard-Holbert C, et al. 2008. ONS research priorities survey. Oncol Nurs Forum 2008; 35(6): E100–E117. [DOI] [PubMed] [Google Scholar]
- 37. Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health 2006; 29(5): 489–497. [DOI] [PubMed] [Google Scholar]
- 38. Fabrigar LR, Wegener DT, MacCallum RC, et al. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods 1999; 4(3): 272–299. [Google Scholar]
- 39. Ledesma RD, Valero-Mora P. Determining the number of factors to retain in EFA: an easy to use program for carrying out parallel analysis. Practical Assess Res Eval 2007; 12(2): 1–11. [Google Scholar]
- 40. DeVellis RF. Scale development: theory and application. 4th ed. Thousand Oaks, CA: SAGE, 2017. [Google Scholar]
- 41. McBee M. Modeling outcomes with floor or ceiling effects: an introduction to the Tobit model. Gifted Child Quart 2010; 54(4): 314–320. [Google Scholar]
- 42. Prentice RL. A generalization of the probit and logit methods for dose response curves. Biometrics 1976; 32(4): 761–768. [PubMed] [Google Scholar]
- 43. Yong AG, Pearce S. A beginner’s guide to factor analysis: focusing on exploratory factor analysis. Tutor Quant Methods Psychol 2013; 9(2): 79–94. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_A for Role competency scale on shared decision-making nurses: Development and psychometric properties by Joseph D Tariman, Pamela Katz, Jessica Bishop-Royse, Lisa Hartle, Katharine L Szubski, Toreend Enecio, Ima Garcia, Nadia Spawn and Katherine Jones Masterton in SAGE Open Medicine


