Abstract
Access to basic imaging and laboratory services remains a major challenge in rural, resource-limited settings in sub-Saharan Africa. In 2016, the Academic Model Providing Access to Healthcare programme in western Kenya implemented a mobile diagnostic unit (MDU) outfitted with a generator-powered X-ray machine and basic laboratory tests to address the lack of these services at rural, low-resource, public health facilities. The objective of this paper is to describe the design, implementation, preliminary impact and operational challenges of the MDU in western Kenya. Since implementing the MDU at seven rural health facilities serving a catchment of over half a million people, over 4500 chest radiographs have been performed, with one or more abnormalities detected in approximately 30% of radiographs. We observed favorable feedback and uptake of MDU services by healthcare workers and patients. However, various operational challenges in the design and construction of the MDU and the transmission and reporting of radiographs in remote areas were encountered. Our experience supports the feasibility of deploying an MDU to increase access to basic radiology and laboratory services in rural, resource-limited settings.
Keywords: radiology, diagnostic x ray, rural, sub-saharan Africa, Kenya, tuberculosis, mobile health units
Summary box.
Access to basic imaging and laboratory services in rural, resource-limited settings in sub-Saharan Africa is limited, particularly in areas facing a high burden of tuberculosis.
In 2016, the Academic Model Providing Access to Healthcare programme implemented a mobile diagnostic unit (MDU) with a generator and wireless digital radiography which has taken over 4500 X-rays to date, detecting abnormalities in approximately 30% of images.
Benefits of the MDU include high rates of detection of abnormal X-ray findings, improved patient access to radiology services and increased patient engagement; transmission of primary radiology reports is a challenge.
Implementing a mobile vehicle equipped with X-ray capabilities and basic laboratory services is a feasible and potentially scalable means to increase access to these services in resource-limited areas.
Background
Access to basic imaging and laboratory services remains a major challenge in rural, resource-limited settings in sub-Saharan Africa. In Kenya, 74% of the population live in rural areas with low population density, serviced by health outposts that lack basic radiology equipment, trained radiologists and laboratory tests.1 Moreover, 90% of Kenya’s radiologists are estimated to be working in urban settings, with 76% (80 of 105) of radiologists in Kenya concentrated in three major cities.2 Similar disparities in access to radiographic imaging services exist elsewhere in East Africa. In Uganda, for example, 56% of patients requiring imaging receive such services in urban areas compared with 10%–13% of patients in rural areas, and an estimated 90% of radiographs performed do not have an accompanying imaging report.3 The optimal strategy to increase access to radiographic imaging in these settings is not well understood.
Access to radiology services in resource-constrained settings in sub-Saharan Africa is particularly critical when one considers the unmeasured burden of tuberculosis (TB) and the major role of chest radiography in TB detection and control.4 Kenya is among 30 countries that together carry the world’s highest country-level burdens of TB.5 The 2016 Kenya TB Prevalence Survey found a national TB prevalence of 558 cases per 100 000 people, more than twice that of previous estimates by WHO.5 Moreover, more than 40% of TB cases remained undetected and untreated. TB case detection has been shown to decrease with increasing distance from a hospital, with patients living further from the facility at higher risk of more severe TB disease.6 Chest radiography is recommended by WHO as a screening tool for TB given its high sensitivity.4 However, the lack of radiographic imaging capacity in rural areas remains a major barrier to implementation of this recommendation. Several studies have described the use of mobile radiography units to address the burden of TB in rural areas.6–8
The Academic Model Providing Access to Healthcare (AMPATH) programme is a consortium of North American Universities working in collaboration with the Kenya Ministry of Health (MOH), Moi University College of Health Sciences, and Moi Teaching and Referral Hospital in western Kenya.9 By engaging in the delivery of health-promoting services to individuals and populations in low-income environments, AMPATH and its partners aim to build health systems in the public sector that deliver and sustain essential healthcare services, develop human capacity through training and education, advance research, eliminate health disparities and mutually strengthen institutions. As part of this population health strategy, AMPATH designed and implemented a truck called the mobile diagnostic unit (MDU) that was outfitted with an X-ray generator, computed radiography system and gasoline generator. The MDU was first operationalised in September of 2014. In 2016, the MDU was augmented with digital radiography and laboratory testing. Following these upgrades, the MDU has travelled daily to rural health outposts within the AMPATH network to deliver radiology and laboratory services. The objective of this paper is to describe the design, implementation, preliminary impact, and operational challenges of the AMPATH MDU in western Kenya.
Design and operation
AMPATH program
AMPATH started an HIV care and treatment program in 2001 and has since expanded to about 500 clinical sites in western Kenya that have enrolled over 200 000 patients with HIV with approximately 1500 new patients enrolling each month.10 AMPATH also supports MOH delivery of primary healthcare, chronic disease care, specialty care and supports community activities including community-run microfinance groups to help address socioeconomic determinants of health.
Setting
AMPATH is the President’s Emergency Plan for AIDS Relief–supported HIV care implementing partner in four of the seven sub-counties of Busia County, namely Butula, Bunyala, Matayos and Teso North. According to the most recent census (2009), Busia County is home to an estimated 743 946 people.11 The HIV prevalence in the county is 6.8% and the poverty level is 66%.12 Although the AMPATH-supported facilities in Busia County serve a catchment area of half a million people, they are poorly resourced, and many do not offer basic laboratory or radiology diagnostic services. Illustrating this, the major county hospital in Busia town, the capital of Busia County, had a digital X-ray unit installed in 2016 after a period of 14 months without any functional X-ray unit. Several of the facilities serviced by the MDU have only intermittent access to electricity and Internet.
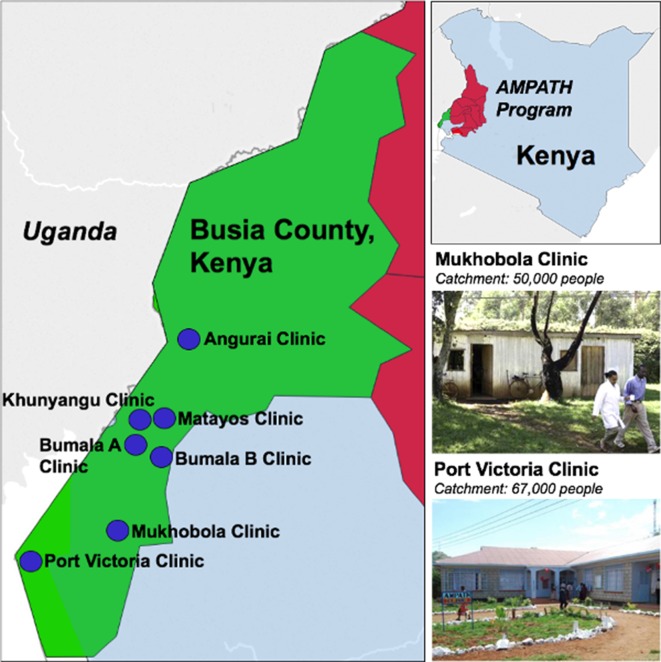
Within the four sub-counties, AMPATH supports HIV service delivery in 66 MOH facilities including one county referral, three sub-county hospitals, eight health centres, 53 dispensaries and five private owned/faith-based facilities. Two of these facilities, the county referral hospital and one sub-county hospital, currently have functional X-ray facilities. The MDU currently travels to seven AMPATH-supported MOH facilities in Busia County on the westernmost border of Kenya: Angurai, Bumala A, Bumala B, Khunyangu, Matayos, Mukhobola and Port Victoria (figure 1). On average, it takes approximately 2 hours to travel from the communities AMPATH serves to Busia County hospital, at a cost of between 500 and 1500 Kenyan shillings (US$5–15) by public transport such as a motorbike, mini-bus or shared taxi.
Figure 1.
Locations of Academic Model Providing Access to Healthcare (AMPATH) clinics served by the mobile diagnostic unit (MDU) in Busia County, Kenya. The red shaded area of the map of Kenya indicates the counties served by the AMPATH programme in the western region of the country. The green shading of the map on the left shows Busia County, where the MDU operates; blue circles indicate the locations of clinics served by the MDU. Photos of two of these clinics’ areas are shown in the lower right of the figure, along with the clinic names and catchment size.
Design
The MDU design, customisation and installation were performed locally. The MDU is a standard Isuzu canter chassis (3–4 tonnes) with a custom-designed, insulated/refrigeration box body, complete with integrally welded, mild steel radiation shielding and washable interior plastic surfaces. The body was further customised with elements including a power control system, anchoring points for equipment, roll-out drawer-mounted AC generation and fuel can. The design incorporates several elements aimed at safety including a negative pressure ventilation system, multipoint redundant electrical grounding, strategically placed mild steel radiation shielding, ample interior space and lighting, patient privacy curtain and an integrated ramp for non-ambulatory patients (figure 2). Implementing a high-frequency X-ray generator in a mobile capacity, free from mains power, was challenging. Due to a lack of detailed information regarding peak power consumption of the X-ray generator, the AC power generator was initially undersized, and the X-ray generator would not consistently fire without power alarms and failed exposures. After extensive testing, this was mitigated by engineering and installing a low-cost power factor correction device.
Figure 2.
Mobile diagnostic unit equipment placement and descriptions. (A) Anterior side view: (1) fuel can; (2) slide-out electrical generator; (3) grounding chain; (4) grounding rod (hammered into the ground at each site). (B) Posterior side view: (1) standing platform for radiologists; (2) power factor correction device; (3) shielded door for radiologists to stand behind; (4) patient access ramp; (5) onboard generator fuel can; (6) redundant grounding devices (installed at each site); (7) slide-out electrical generator. (C) (interior view, detailed): (1) fold-down bed for supine radiographs; (2) X-ray generator; (3) negative pressure ventilation; (4) digital radiography cassette; (5) radiography laptop computer; (6) onboard 230 V power and charging; (7) power control, safety and distribution systems. (D) Interior view, general layout, shown with shielding door open.
Cost
Implementation and monthly maintenance costs for the mobile diagnostic unit can be found below in tables 1 and 2.
Table 1.
Implementation costs for mobile diagnostic unit
| Equipment | KSH | US$ |
| Truck chassis | 2 850 000 | 33 139.53 |
| Truck body | 1 250 000 | 14 534.88 |
| Outfitting truck body | 556 000 | 6465.12 |
| Engineering cost | 495 000 | 5755.81 |
| Radiation testing and certification | 60 000 | 697.67 |
| Electrical generator | 226 000 | 2627.91 |
| Sedecal Dragon (X-ray generator) | 10 950.00 | |
| Digital radiography | 52 100.00 | |
| Dell server | 6182.00 | |
| 132 452.92 |
All costs in Kenyan shillings (KSH) were spent locally. Exchange rate: 86 KSH/US$.
Table 2.
Monthly maintenance costs for mobile diagnostic unit
| Expense | KSH/month | US$ (86 KSH/US$) |
| Radiographer meal allowance | 6000 | |
| Generator fuel | 10 000 | |
| Tires | 9000 | |
| Inspection | 812 | |
| Vehicle insurance | 6375 | |
| Vehicle maintenance | 8400 | |
| Fuel | 20 000 | |
| Tracking system | 1700 | |
| Technology (CDs) | 8000 | |
| Salaries | 100 000 | |
| Equipment maintenance | 10 000 | |
| 180 287 | 2096.36 |
KSH, Kenyan shilling.
Operation
A radiographer employed by the MOH in Busia County performs the studies. The schedule for the MDU is determined monthly by a Busia County–based coordinator of AMPATH services and disseminated to the clinics at the beginning of the month. The MDU travels to each site at least twice per month with additional visits to sites according to the size of their patient population and need for services. Patients are scheduled for a radiograph or laboratory test by the clinician at each facility and asked to return to clinic on the next MDU day. X-rays are performed for tuberculosis screening purposes in HIV-positive patients per WHO and Kenya MOH guidelines, and for diagnostic purposes in patients with respiratory symptoms and offered free of charge.13 14 HIV-infected patients in Kenya who are asymptomatic are also routinely screened for serum cryptococcal antigen if their CD4+ count is ≤100 cells/µL. If the radiographer notes the image to be grossly abnormal, he notifies the clinician immediately to review the image and determine any necessary management course. At the end of the day, radiographs are copied onto a CD, which is maintained at each site for review and recordkeeping. Radiographs were originally acquired with a computed radiography system (Kodak POC 140), which was replaced with a wireless digital radiography (Carestream) system in 2016 to save operator time, reduce space requirements and decrease electrical load. Images were originally transported to a central archive via DVDs burned from the computed radiography machine. While cost-effective, this mechanism was associated with delays in care and was replaced with a cellular modem to send images to a central archive, which reliably delivers the images for reading by radiologists at Moi Teaching and Referral Hospital, using a web-based application, referralPACS.15 Radiologists report using a form that captures discrete data elements about each radiograph and referralPACS generates a PDF report that is printed centrally and distributed to each site within 2 weeks of the radiograph (figures 3 and 4). The results are also uploaded to an online results portal through a secure socket shell tunnel. Our web page uses hypertext transfer protocol secure (HTTPS) encryption for all interpretations. All results are filed in the patient’s medical record.
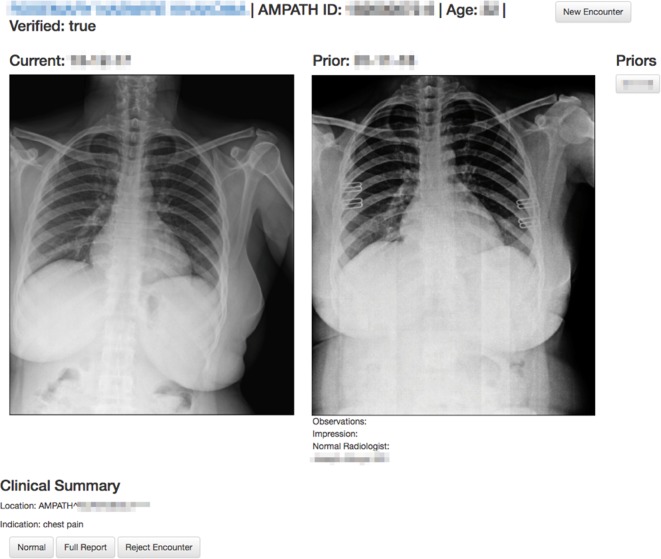
Figure 3.
Example of web-page layout for radiologist interpretation. Prior films acquired on the mobile diagnostic unit are available for comparison. A shortcut button to create a normal report is important for workflow due to the large number of normal radiographs. See figure 4 for the full report form.
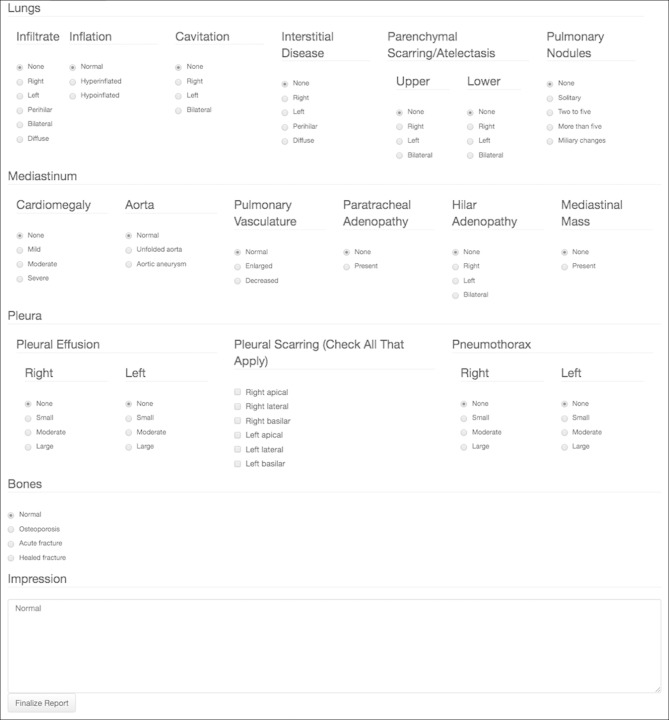
Figure 4.
Report form for abnormal radiographs. Data elements are captured discreetly in addition to a free-text impression.
Laboratory services, including testing for pregnancy (urine human chorionic gonadotropin), meningitis (cryptococcal antigen), TB (lateral flow urine lipoarabinomannan assay) and a serum basic metabolic profile are also available to patients, with or without an appointment, whenever the MDU is at the clinic. All laboratory services are performed by a certified laboratory technician employed by AMPATH and offered at the point-of-care, which enables results to be immediately made available to the patient and clinician at the time they are performed.
Implementation benefits
Our experience supports the feasibility of an MDU equipped with radiographic and basic laboratory services to address the major access gap for these health services in rural areas of Kenya. Moreover, we identify three key successes with the MDU: a high detection rate of abnormal radiographic studies, improved access to radiology/laboratory services and increased patient engagement in these services.
Laboratory findings
As of June 2017, 523 laboratory services had been provided. Pregnancy tests accounted for 183 of the MDU laboratory services, followed by basic metabolic profile (169), cryptococcal antigen (98) and rapid urine lipoarabinomannan antigen (73).
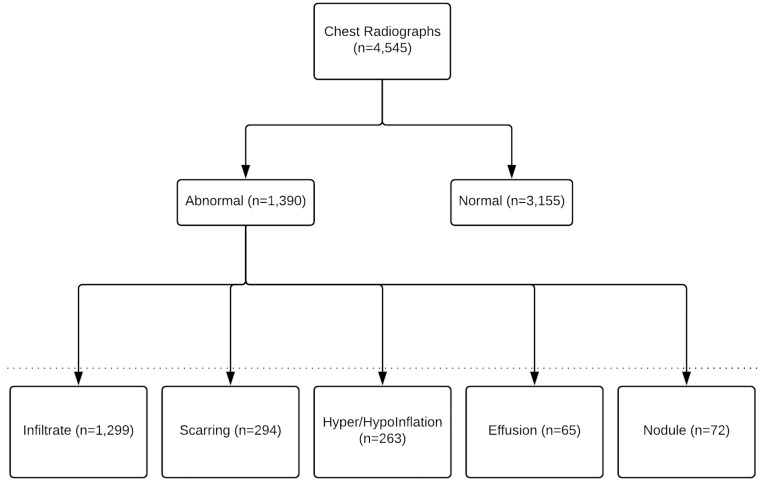
High detection rates
From April 2014 to April 2018, 4545 chest radiographs were performed by the MDU, ranging from 10 to 20 to 40–50 radiographs per day at low-volume and high-volume facilities, respectively. All radiographs were interpreted by radiologists with board-certified Kenyan medical licenses. Most X-rays performed were usable according to the radiographer’s assessment at the time of the procedure; those that were deemed unusable were simply repeated given the digital format of the film. Of these, 3155 (69%) were normal and 1390 (31%) were abnormal, demonstrating a spectrum of pathological findings (figure 5). The number of patients receiving chest radiographs each month has risen steadily each month since implementation. Our rate of detection was much higher than anticipated, as more than 30% of chest radiographs taken were abnormal. It is likely that many of these abnormalities would not have been detected in the absence of the MDU, as the areas the MDU serves do not otherwise have access to diagnostic testing. Our results also demonstrate the potential impact of the MDU in improving detection of TB and other pathologies in resource-constrained settings.
Figure 5.
Description of X-ray results. Abnormality classes are not exclusive, patients may have one or more.
Improved access
The MDU was developed as part of AMPATH’s population health strategy and seeks to increase access to radiography and laboratory services, but not to take the place of permanent healthcare facilities. Although we identified these services as priorities for the patient population at AMPATH, it is important to note that the MDU platform can accommodate multiple potential diagnostic and treatment modalities to increase access to healthcare services in resource-limited settings. Ultrasound and CT scan, for example, have been incorporated into MDUs in other settings.16 17 While AMPATH is still focused on increasing infrastructure that allows its healthcare facilities to function independently of the MDU, one of the major successes of the MDU is the ability to provide basic radiographs to a population living in remote areas. Many of the facilities the MDU services are several kilometres away from major highways and are accessible only by dirt road. Having an independent steady power source from our generator improves reliability, and digital radiography reduces cost through elimination of film and processing supplies. Furthermore, acquisition of film and processing supplies is not trivial in Kenya, and frequently leads to extended downtimes at other facilities. In addition, patients who use the MDU or seek out AMPATH services because of the services the MDU provides gain access to AMPATH’s larger network of healthcare services and programme as AMPATH patients, contrasting with companies aiming to replicate healthcare facilities through broadly capable mobile units.18 In so doing, the AMPATH MDU takes a less costly and more efficient approach that synergises with its existing infrastructure.
Patient engagement
Increased patient engagement was a benefit we were not expecting. Several of our clinicians anecdotally reported that patients are excited about access to new technology, and curious about engaging with radiographic and laboratory services, resulting in an increase in the number of patients visiting the health facilities. Similar findings were reported using MDUs for TB active case detection as well elsewhere in sub-Saharan Africa.7 This finding is important because patients who live long distances from tertiary hospitals access lower-level care locally and avoid travelling until they have advanced disease. Concerning TB, moving diagnostics closer to the patient has the potential to decrease TB burden by increasing screening chest radiographs especially for patients with newly diagnosed HIV and those who have not previously had a chest X-ray.13 14 Such screening should lead to earlier diagnosis and treatment. This is particularly important in Kenya, where an estimated 40% of TB cases are currently undetected.13
Challenges and limitations
Implementation
Although the design of the MDU came with challenges (see Design section), the majority of challenges we encountered were during the implementation of the MDU. A primary radiologist reading, which is the standard of care throughout the USA, is challenging in Kenya due to multiple factors including poor internet connectivity, too few radiologists and delivery time for paper reports. Poor internet connectivity in rural areas creates delays in archiving images for radiologist review and precludes clinicians’ access to the online results portal. To address these issues, we have ensured that the local clinic has a copy of each radiograph for immediate review by clinical officers. To increase immediate access to radiologist readings, efforts are ongoing to allow synchronisation of the imaging archive system with AMPATH’s electronic medical record system to facilitate clinicians’ access to images and formal reports at the point of care.19 We are also actively developing a computer-aided detection (CAD) system, in partnership with the National Institutes of Health, which aims to identify which radiographs contain abnormalities that need to be evaluated quickly. This CAD system is currently being implemented on the MDU (figure 6). Other possible solutions to increase efficiency include task shifting to clinical officers with escalation of more complex images to be read by a radiologist. Outsourcing or telemedicine are additional potential solutions but are also limited by Internet connectivity and significantly higher costs.
Figure 6.
Example of the National Library of Medicine (NLM) computer-aided detection system. The system confers either red or green status to each chest radiograph, shortly after acquisition.
Sustainability
Funding for equipment maintenance to continue providing radiographs is a challenge. Currently, all radiographs and laboratory tests performed by the MDU, except the basic metabolic profile, are offered free of charge due to various AMPATH funding partners. To ensure long-term sustainability of the MDU programme and other healthcare initiatives, AMPATH is focusing on enrolling patients in the National Hospital Insurance Fund, a new government insurance programme to cover healthcare costs for Kenyans. Vouchers and conditional cash transfers are other methods used to increase access to healthcare services in sub-Saharan Africa.20 Although the early diagnosis of TB and other communicable diseases is likely to have benefits in terms of patient morbidity and mortality and prevention of ongoing disease transmission in the community, we are unable to characterise the cost-effectiveness of the MDU given the lack of these patient-level clinical and outcomes data. However, the MDU programme requires that at least 10 patients to be scheduled for an X-ray at a given site for the unit to attend that site; once on site, the cost per X-ray decreases with each additional X-ray performed. Finally, we do not have data on the clinical treatment courses for patients who received X-rays and laboratory tests through our MDU and the extent to which the MDU interventions influenced patient outcomes and clinical decision-making. This information is also important in understanding the true impact and cost-effectiveness of the MDU intervention.
Future directions
Future efforts are planned to further characterise the impact of the MDU on tuberculosis diagnosis and control in the catchment area, as well as the cost-effectiveness of the MDU strategy in comparison with other strategies to scale laboratory and radiological resources in our setting.
Conclusions
The MDU provides a potential solution to resource-limited, rural areas seeking to increase access to laboratory and radiology resources in western Kenya. The MDU may serve as a model for other settings facing similar challenges, both to address the burden of rural TB and the growing need for non-communicable disease detection and management in the population.
Footnotes
Handling editor: Seye Abimbola
Contributors: The research and development for aspects of this project was supported by the Intramural Research Program of the National Library of Medicine, National Institutes of Health. The design, equipment and operation of the MDU is supported by a grant from the AbbVie Foundation. This research has also been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through USAID under the terms of Cooperative Agreement No. AID-623-A-12-0001. It is made possible through joint support of the United States Agency for International Development (USAID).
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The contents are the sole responsibility of AMPATH and do not necessarily reflect the views of USAID or the United States Government.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Moi University/Moi Teaching and Referral Hospital Institutional Research and Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data statement: No additional data are available.
References
- 1. World Bank Group , 2017. Rural population (% of total population). https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS (accessed 15 Feb 2018).
- 2. Kawooya MG. Training for rural radiology and imaging in sub-saharan Africa: addressing the mismatch between services and population. J Clin Imaging Sci 2012;2:37 10.4103/2156-7514.97747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kawooya MG, Pariyo G, Malwadde EK, et al. . Assessing the diagnostic imaging needs for five selected hospitals in Uganda. J Clin Imaging Sci 2011;1:53 10.4103/2156-7514.90035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization Chest radiography in tuberculosis detection: summary of current who recommendations and guidance on programmatic approaches. Geneva: WHO, 2016. [Google Scholar]
- 5. World Health Organization Global tuberculosis report. Geneva: WHO, 2016. [Google Scholar]
- 6. Golub JE, Mohan CI, Comstock GW. Active case finding of tuberculosis: historical perspective and future prospects. Int J Tuberc Lung Dis 2005;9:1183–203. [PMC free article] [PubMed] [Google Scholar]
- 7. Corbett EL, Bandason T, Duong T, et al. . Comparison of two active case-finding strategies for community-based diagnosis of symptomatic smear-positive tuberculosis and control of infectious tuberculosis in Harare, Zimbabwe (DETECTB): a cluster-randomised trial. Lancet 2010;376:1244–53. 10.1016/S0140-6736(10)61425-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Heuvelings CC, de Vries SG, Greve PF, et al. . Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis 2017;17:e144–58. 10.1016/S1473-3099(16)30532-1 [DOI] [PubMed] [Google Scholar]
- 9. Inui TS, Nyandiko WM, Kimaiyo SN, et al. . AMPATH: living proof that no one has to die from HIV. J Gen Intern Med 2007;22:1745–50. 10.1007/s11606-007-0437-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. AMPATH , 2018. AMPATH: leading with care. http://www.ampathkenya.org/ (accessed 20 Feb 2018).
- 11. Kenya National Bureau of Statistics Kenya—2009 Kenya Population and Housing Census. Kenya, 2009. [Google Scholar]
- 12. National AIDS Control Council Busia county HIV & AIDS strategic plan. Busia County, Kenya, 2014. [Google Scholar]
- 13. Republic of Kenya: Ministry of Health Kenya tuberculosis prevalence survey. Nairobi: Kenya, 2016. [Google Scholar]
- 14. World Health Organization Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. Geneva: WHO, 2011. [Google Scholar]
- 15. Shadowdoc , 2018. Shadowdoc/referralpacs. https://github.com/shadowdoc/referralpacs (accessed 29 Jun 2018).
- 16. Sone S, Takashima S, Li F, et al. . Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet 1998;351:1242–5. 10.1016/S0140-6736(97)08229-9 [DOI] [PubMed] [Google Scholar]
- 17. Chavez MA, Naithani N, Gilman RH, et al. . Agreement between the World Health Organization algorithm and lung consolidation identified using point-of-care ultrasound for the diagnosis of childhood pneumonia by general practitioners. Lung 2015;193:531–8. 10.1007/s00408-015-9730-x [DOI] [PubMed] [Google Scholar]
- 18. OneStopTB clinic , 2018. Delft imaging systems. https://www.delft.care/onestoptb/ (accessed 29 Jun 2018).
- 19. Tierney WM, Rotich JK, Hannan TJ, et al. . The AMPATH medical record system: creating, implementing, and sustaining an electronic medical record system to support HIV/AIDS care in western Kenya. Stud Health Technol Inform 2007;129(Pt 1):372–6. [PubMed] [Google Scholar]
- 20. Owusu-Addo E, Renzaho AMN, Smith BJ. Evaluation of cash transfer programs in sub-saharan Africa: a methodological review. Eval Program Plann 2018;68:47–56. 10.1016/j.evalprogplan.2018.02.010 [DOI] [PubMed] [Google Scholar]