Abstract
Purpose
To examine the validity of wrist acceleration cut-points for classifying moderate (MPA), vigorous (VPA) and moderate-to-vigorous (MVPA) physical activity.
Methods
Fifty-seven children (5-12y) completed 15 semi-structured activities. Three sets of wrist cut-points (>192mg, >250mg, >314mg), previously developed using Euclidian norm minus one (ENMO192+), GENEActiv software (GENEA250+) and Bandpass Filtered followed by Euclidian Norm (BFEN314+), were evaluated against indirect calorimetry. Analyses included classification accuracy, equivalence testing and Bland-Altman procedures.
Results
All cut-points classified MPA, VPA and MVPA with substantial accuracy (ENMO192+: κ = 0.72 [95% confidence interval: 0.72 – 0.73], MVPA: area under the receiver operating characteristic curve (ROC-AUC) = 0.85 [0.85 – 0.86]; GENEA250+: κ = 0.75 [0.74 – 0.76], MVPA: ROC-AUC = 0.85 [0.85 – 0.86]; BFEN314+: κ = 0.73 [0.72 – 0.74], MVPA: ROC-AUC = 0.86 [0.86 – 0.87]). BFEN314+ misclassified 19.7% non-MVPA epochs as MPA, whereas ENMO192+ and GENEA250+ misclassified 32.6% and 26.5% of MPA epochs as non-MVPA, respectively. Group estimates of MPA time were equivalent (p<0.01) to indirect calorimetry for the BFEN314+ MPA cut-point (mean bias: -1.5%, limits of agreement [LoA]: -57.5 - 60.6%), while estimates of MVPA time were equivalent (p<0.01) to indirect calorimetry for the ENMO192+ (mean bias: -1.1% [LoA: - 53.7% – 55.9%]) and GENEA250+ (mean bias: 2.2% [LoA: -56.5% – 52.2%]) cut-points. Individual variability (LoAs) was large for MPA (min: BFEN314+, -60.6% – 57.5%; max: GENEA250+, -42.0% – 104.1%), VPA (min: BFEN314+, -238.9% – 54.6%; max: ENMO192+, -244.5% – 127.4%) and MVPA (min: ENMO192+, -53.7% – 55.0%; max: BFEN314+, -83.9% – 25.3%).
Conclusion
Wrist acceleration cut-points misclassified a considerable proportion of non-MVPA and MVPA. Group level estimates of MVPA were acceptable; however, error for individual level prediction was larger.
Keywords: activity monitor, children, validation, objective measurement, GENEActiv, ActiGraph
Introduction
Accurate measurement of physical activity (PA) in children is of critical importance to monitor prevalence and trends, establish associations with health outcomes, identify determinants, and to evaluate the effectiveness of interventions to promote PA (1). Hip-mounted accelerometers have commonly been used to objectively quantify habitual PA in children (2). However, low participant compliance with accelerometry protocols have resulted in considerable non-wear time and, subsequently, loss of data (3). National biobanks such as U.K. Biobank (4), and large population surveys (5) including the National Health and Nutrition Examination Study (NHANES) 2011-2014 (6) in the U.S. incorporated wrist-worn accelerometers. Recent evidence indicates that wrist-placement results in increased wear time due to greater compliance (6–8), which has consequently caused a shift from hip-placement to wrist-placement.
Traditionally, accelerometer-based PA monitoring devices have provided proprietary units referred to as “counts” from which cut-points have been developed to classify moderate (MPA), vigorous (VPA) and moderate-to-vigorous physical activity (MVPA) and estimate time spent in MVPA. However, more recently, commonly used accelerometer-based motion sensors such as the GENEActiv (ActivInsights Ltd., Cambridge, UK) and ActiGraph GT3X+ and GT9X (ActiGraph Corporation, Pensacola Beach, FL) provide access to high frequency tri-axial acceleration data, and therefore cut-points to define PA intensity have been developed for these data collected from wrist devices. The existence of multiple cut-points makes comparisons of PA outcomes from studies that have used different cut-points challenging, and inconsistencies between studies may affect conclusions about PA prevalence, health benefits, determinants and the effectiveness of interventions. Therefore, studies are needed that simultaneously compare the validity of multiple cut-points to provide evidence upon which consensus can be reached for consistent data reduction approaches, which could increase the comparability of PA outcomes between studies.
Recent laboratory-based calibration studies (9–11) have developed three sets of PA intensity thresholds for raw acceleration output from wrist-worn devices in 6-14 year-old children using indirect calorimetry as the criterion measure. The cut-points were cross-validated and demonstrated acceptable classification accuracy. However, two studies (10, 11) applied the leave-one out cross-validation approach in the calibration sample and evaluated classification accuracy for the same MPA and VPA activities, which were predominantly ambulatory (e.g., treadmill walking and running). As such, generalizability to free living scenarios may be limited. One set of cut-points (9) was cross-validated in an independent sample of 5-8 year-olds (12), however, the sample size was small (n=15), the protocol included a limited range of activities, and the cut-points were not cross-validated in children older than 8 years.
These independent calibration studies used different data processing methodologies and have resulted in different cut-points, ranging from 192mg (11) to 314mg (10) and 696mg (11) to 998mg (10) for MPA and VPA, respectively; thus providing different PA estimates, which makes it difficult to compare outcomes between studies. Therefore, additional studies are needed to adequately cross-validate cut-points. A recent study (13) validated various data processing approaches for the wrist-worn ActiGraph in children and concluded that differences in PA estimates were caused by the use of different methods. However, because Kim et al. (13) did not include a valid criterion measure, the most accurate approach could not be determined. In agreement with best practice recommendations from Welk et al. (14), the authors suggested that the validity of different methods, along with their corresponding cut-points, should be evaluated simultaneously, relative to gold standard methods. Therefore, the aim of this study was to simultaneously evaluate the performance of three sets of wrist acceleration cut-points for classifying MPA, VPA and MVPA and estimating time spent in PA intensities, under consistent conditions, using portable indirect calorimetry as the criterion measure in 5-12 year-old children.
Methods
Participants
Fifty-seven children aged 5-12y who were without physical or health conditions that would affect participation in PA were recruited as part of an activity monitor validation study. The study was approved by the University of Wollongong Health and Medical Human Research Ethics Committee. Descriptive characteristics of participants are presented in Table 1. Written parental consent and participant assent were obtained prior to participation.
Table 1. Participant characteristics.
| Characteristics | |
|---|---|
| Age (y) | 9.2 ± 2.3 |
| Sex | |
| Boys (n) | 28 (49.1%) |
| Girls (n) | 29 (50.9%) |
| Height (cm) | 135.9 ± 14.6 |
| Body mass (kg) | 32.7 ± 10.9 |
| BMI percentile | 53.2 ± 28.6 |
| Overweight (n) | 7 (12.3%) |
| Obese (n) | 2 (3.5%) |
| Age distribution | |
| 5-7 (n=19) | 33.3% |
| 8-18 (n=24) | 42.1% |
| 11-12 (n=14) | 24.6% |
| Race | |
| Caucasian (n) | 54 (94.7%) |
| Asian (n) | 3 (5.3%) |
Characteristics of the participants are presented as mean ± SD, distributions of the sample are presented in percentages. Weight status was classified according to the 2000 Centers for Disease Control and Prevention Growth Charts for the United States (11).
Procedures
Participants were required to visit the laboratory on two occasions. Anthropometric measures were completed during the first visit using standardised procedures while children were wearing light clothing and with shoes removed. BMI (kg/m2) was calculated to categorize participants as normal weight or overweight/obese, according to the 2000 CDC Growth Charts for the United States (15). Children completed a protocol of 15 semi-structured activities (Table 2) from sedentary (lying down, TV viewing, handheld e-game, writing/coloring, computer game), light-intensity PA (LPA: getting ready for school, standing class activity, slow walk, dancing), and MVPA (tidy up, brisk walk, soccer, basketball, running, locomotor course). Activities were equally divided over 2 visits and completed in a structured order of increasing intensity for 5 min (except for lying down which was done for 10 min).
Table 2. Activity Protocol.
| Activity Type | Activity Trial | Intensity | Description of Activity Trial |
|---|---|---|---|
| Resting | Lying down | Sedentary | Lying down awake on a mattress in supine position - arms at sides - rest for 10 min. |
| Sitting | TV viewing | Sedentary | Watching a movie in a comfortable chair. Instructed to minimize body movements. |
| Handheld e-game | Sedentary | Sitting on a chair at a desk playing an e-game on a handheld device. | |
| Writing/coloring | Sedentary | Sitting on a chair at a desk, 5-8 y: coloring on paper using pencils, 9-12 y: copying words on a pad of paper using a pencil. | |
| Computer game | Sedentary | Sitting on a chair at a desk playing an educational computer game. | |
| Lifestyle | Getting ready for school | Light | Get dressed, set table, pour food, pack up, brush teeth, pack bag, leave for school. |
| Standing class activity | Light | Standing activities with minimal movement such as writing/drawing on a white board. | |
| Dancing | Light | Following a video with dance step instructions (Zumba® fitness). | |
| Tidy up | Moderate | Tidying up a 4x5 m area: pick up clothes, towels, toys and sport equipment and return them into boxes. | |
| Basketball | Moderate | Shooting a basketball using a 2.29 m adjustable hoop, chase the ball within a 4.9x4.6 m area and bounce back to the start position at the boundary line apposite from the hoop. | |
| Soccer | Vigorous | Kicking a foam soccer ball on a 5 m distance between a 1 m wide goal after dodging between a straight line of 5 cones (1 m apart). Instructed to jog back to start position after kicking the ball. | |
| Locomotor course | Vigorous | Continuously completing a course including 4x 2-foot jump, jogging and sliding between cones around a 4x9.5 m area. | |
| Ambulatory | Slow walk | Light | Walking slowly at a self-selected comfortable speed around a 45 m indoor track. Examiner regulates constant speed by recording lap times. |
| Brisk walk | Moderate | Walking briskly at a self-selected brisk comfortable speed around a 45 m indoor track. Examiner regulates constant speed by recording lap times. | |
| Running | Vigorous | Run at a self-selected comfortable speed around a 45 m indoor track. Examiner regulates constant pace by speed lap times. |
All activities are completed for 5 min, except from lying down (10 min)
Instrumentation
At each visit, children were fitted with a portable respiratory gas analysis system (MetaMax® 3B, Cortex, Biophysics, Leipzig, Germany) to provide the criterion assessment of PA energy expenditure. Children were also fitted with a GENEActiv dorsally on the non-dominant wrist.
Indirect calorimetry
Oxygen consumption (O2) was assessed using the MetaMax® 3B portable breath-by-breath respiratory gas analysis system to provide the criterion assessment of energy expenditure. The participants wore a facemask (Hans Rudolph, Kansas City, MO) covering their nose and mouth, which was held in place by a head harness. Prior to every measurement, the analyser was calibrated according to the manufacturer’s guidelines. Breath-by-breath data from indirect calorimetry were downloaded and exported using MetaSoft (version 4.3.2).
Activity monitor
The GENEActiv has a waterproof design and measures tri-axial accelerations ranging in magnitude ±8g at a sample frequency ranging from 10-100Hz. Acceleration values are digitized by a 12-bit analog-to-digital converter. Accelerometers were initialised with a sample frequency of 100Hz.
Data reduction
Energy expenditure
Volume of O2 uptake and CO2 production were averaged per 10s for every entire activity bout of 5min and converted into units of energy expenditure (kcal·min-1) using the Weir equation (16). For analytical purposes, and for consistency with the calibration studies of the cut-points (9–11), the activities were categorised in the primary analyses as non-MVPA (<3 METs), MPA (≥3 to <6 METs) or VPA (≥6 METs) based on average measured energy expenditure values. MPA and VPA were subsequently combined and classified as MVPA (≥3 METs). The participants’ measured resting energy expenditure (REE) from the lying down trial was used to define 1 MET in order to calculate MET-values for all activities. Breath-by-breath samples from the data collected between minutes 7.0 and 9.0 during the lying down trial were averaged to calculate mean REE. Metabolic data (10s epochs) from the activities were scaled to the children’s REE and converted into youth METs using customized software. Although 3 METs has widely been used as an intensity threshold to distinguish MPA from LPA, there is considerable evidence that 4 METs is more accurate for classifying MPA in children and adolescents (17) and that brisk walking, a key behavioral indicator of MPA, is associated with an energy cost of approximately 4 METs (18). It should be noted that researchers have based these estimates on either predicted REE or measured REE. As such, studies have demonstrated that MET levels for walking and other activities are somewhat contingent on the choice of the denominator (19, 20). In our sample, the larger value results in ~3 METs for brisk walking as the behavioural indicator, when based on measured REE (slow walking = 2.9 ± 0.5 METs; brisk walking = 3.4 ± 0.6 METs) (see Table, Supplemental Digital Content 1, metabolic data by activities for indirect calorimetry, http://links.lww.com/MSS/B67). However, when based on predicted REE, the value was closer to 4 METs (slow walking = 4.0 ± 0.6 METs; brisk walking = 4.7 ± 0.7 METs), which was consistent with a previous study (comfortable walking = 3.9 ± 0.6 METs; brisk walking = 4.7 ± 0.6 METs) (21). Therefore, supplementary analyses were conducted testing the consistency of the findings using a threshold of 4 METs, for which METs were calculated by dividing mean energy expenditure values by REE predicted from the participant’s sex, age, body mass, and height using Schofield’s (22) equation for children aged 3–10 or 10–18 yr.
Accelerometry
Data reduction approaches were performed according to the methods reported in calibration studies by Hildebrand et al. (11), Phillips et al. (9) and Schaefer et al. (10) for the development of the three cut-points evaluated. Raw wrist data were downloaded using the GENEActiv software version 2.2. Signal processing codes from Hildebrand et al. (11) were downloaded and applied to convert raw acceleration data into 1s epochs according to the Euclidian norm minus one (ENMO) approach. This method subtracted 1g from the Euclidian norm (EN = sqrt (x2 + y2 +z2)), after which negative values were rounded up to zero. According to the methods described by Phillips et al. (9), raw acceleration data was converted into 1s epochs using the GENEActiv post processing software, in order to create gravity-subtracted signal vector magnitude (SVMgs) data. Customized software was developed using the statistical computing language R (v.3.1.2) in order to apply a band-pass filter to the raw acceleration data (4th order Butterworth filter with ω0 = 0.2-15Hz) to remove the gravitational acceleration component as well as high-frequency sensor noise, as described by Schaefer et al. (10). EN was taken from the three resulting signals and averaged per 1s epoch. This method is referred to as Bandpass Filtered followed by Euclidian Norm (BFEN). The methods of the calibration studies resulted in sets of cut-points as described below in order of increasing acceleration magnitude, and hereafter referred to as:
Hildebrand et al. (11), ENMO192+: non-dominant wrist; MPA, 192-695 mg; VPA, ≥696 mg.
Phillips et al. (9), GENEA250+: right wrist; MPA, >275 to ≤700 mg; VPA, >700 mg, left wrist; MPA, >250 to ≤750 mg; VPA, >750 mg. Calibration procedures for these cut-points were based on the cumulative sum of gravity-based accelerations measured with a sample frequency of 80Hz, making the original cut-points frequency dependent (11). For presentation purposes, the cut-point values were converted from a time dependent unit (g.seconds) to the time independent unit mg in order to compare with values of other cut-points.
Schaefer et al. (10), BFEN314+: non-dominant wrist; MPA, 314-998 mg; VPA, ≥998 mg.
The 1s epochs for accelerometry data of all methods were averaged over 10s windows in order to align with indirect calorimetry data.
Data synchronization
At the beginning of each laboratory visit, the activity monitors and indirect calorimetry were synchronized with an internal computer clock. After applying the cut-points, predicted intensity classification for the wrist acceleration data was aligned with the ground truth energy expenditure data in order to examine classification accuracy. All valid epochs from each activity trial were included in analyses to reflect how activity monitors are applied under free-living conditions. Estimated time spent in each PA intensity using indirect calorimetry or wrist accelerometry was established by summing the 10s epochs classified for each intensity.
Statistical analyses
Normality of the data was confirmed prior to analyses. Classification accuracy for each set of cut-points (MPA, VPA, non-MVPA) was examined by calculating weighted κ statistics. Kappa coefficients were interpreted using the ratings suggested by Landis and Koch (23): poor (0 – 0.20), fair (0.21 – 0.40), moderate (0.41 – 0.60), substantial (0.61 – 0.80), and almost perfect (0.81 – 1.0). Contingency tables were applied to summarize classification accuracy and percentage of misclassified epochs for each intensity. Because of the public health focus on MVPA, the intensities of MPA and VPA were combined as one dichotomous variable MVPA and the classification accuracy was evaluated using sensitivity, specificity and area under the receiver operating characteristic curve (ROC-AUC). ROC-AUC values were defined as excellent (≥0.90), good (0.80-0.89), fair (0.70-0.79), or poor (<0.70) (24). The equivalence of time estimates between the cut-points and indirect calorimetry for each intensity was examined at the group level using the 95% paired equivalence test. In order to reject the null-hypothesis of the equivalence test, the 90% confidence interval (CI) of time spent in the intensity predicted by the monitors should fall entirely within the predefined equivalence region of ±10% (25). Measurement agreement and systematic bias for estimated time spent in intensities were evaluated at the individual level using Bland-Altman procedures (26). Analyses were performed using the statistical computing language R v.3.1.2 (The R Foundation for Statistical Computing) and SPSS v.21.0 (IBM Corporation, Armonk NY).
Results
All participants completed the protocol. For one of the visits, wrist acceleration data were unavailable for 3 children. Data from one child were entirely excluded from the analyses and data from 3 participants for a total of 8 activities were excluded because of indirect calorimetry failure. A total of 25,452 PA intensity annotated 10s epochs (94.4% of the total data) from 57 children were available for analyses.
Applying the contingency tables for classification accuracy (Table 3), ENMO192+ (κ = 0.72 [95% confidence interval (CI): 0.72 to 0.73]), GENEA250+ (κ = 0.75 [95% CI: 0.74 to 0.76]) and BFEN314+ (κ = 0.73 [95% CI: 0.72 to 0.74]) exhibited substantial agreement. The proportion of correctly classified epochs for the BFEN314+ MPA and VPA cut-points (52.0% and 93.6%, respectively) was higher than for the ENMO192+ cut-points (46.5% and 70.0%, respectively) and the GENEA250+ cut-points (45.4% and 79.9%, respectively). However, ENMO192+ and GENEA250+ classified non-MVPA (90.5% and 89.2%, respectively) more accurately than BFEN (81.7%). BFEN misclassified 19.7% of non-MVPA as MPA and 39.4% of MPA as VPA. The highest proportions of misclassification for ENMO192+ and GENEA250+ on the other hand were found for MPA misclassified as non-MVPA (ENMO192+: 32.6% epochs; GENEA250+: 26.5% epochs) and VPA misclassified as MPA (ENMO192+: 20.8% epochs; GENEA250+: 28.1% epochs). ENMO192+ and GENEA250+ misclassified 25.0% and 19.4% of VPA as MPA. Classification accuracy for MVPA was good for all cut-points (ROC-AUC: ENMO192+, 0.85 [95% CI: 0.85 to 0.86]; GENEA250+, 0.85 [95% CI: 0.85 to 0.86]; BFEN314+, 0.86 [95% CI: 0.86 to 0.87]). Although the true-positive rate (sensitivity) for BFEN314+ (0.94) was higher than for ENMO192+ (0.80) and GENEA250+ (0.81), specificity for BFEN314+ was lower (0.78) compared to ENMO192+ (0.90) and GENEA250+ (0.89).
Table 3. Contingency tables for classification accuracy of raw wrist acceleration cut-points.
| Actual Intensity | Cut-points classification of intensity | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| ENMO192+ | |||
| 1. non-MVPA | 14418 (90.5) | 1312 (8.2) | 193 (1.2) |
| 2. MPA | 2217 (32.6) | 3160 (46.5) | 1416 (20.8) |
| 3. VPA | 138 (5.0) | 684 (25.0) | 1914 (70.0) |
| GENEA250+ | |||
| 1. non-MVPA | 14208 (89.2) | 1493 (9.4) | 222 (1.4) |
| 2. MPA | 1802 (26.5) | 3081 (45.4) | 1910 (28.1) |
| 3. VPA | 20 (0.7) | 531 (19.4) | 2185 (79.9) |
| BFEN314+ | |||
| 1. non-MVPA | 12448 (78.2) | 3130 (19.7) | 345 (2.2) |
| 2. MPA | 580 (8.5) | 3535 (52.0) | 2678 (39.4) |
| 3. VPA | 8 (0.3) | 167 (6.1) | 2561 (93.6) |
The presented values indicate the proportion of epochs classified for each intensity, with percentages presented between brackets. The values in boldface indicate the proportion of epochs correctly classified for the physical activity intensity. MPA: moderate physical activity; VPA: vigorous physical activity; MVPA: moderate-to-vigorous physical activity; ENMO: cut-points developed using Euclidian norm minus one; GENEA: cut-points developed using the GENEActiv post processing software; BFEN: cut-points developed using Bandpass Filtered followed by Euclidian Norm.
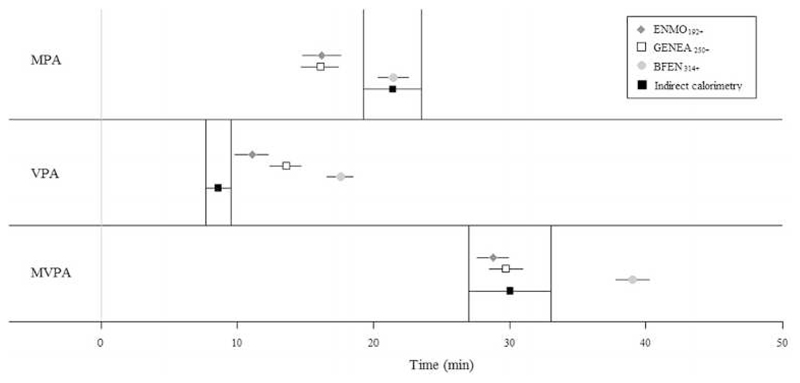
At the group level, estimated time spent in MPA was equivalent (p<0.01) to indirect calorimetry for BFEN314+ and estimated time spent in MVPA was equivalent for ENMO192+ and GENEA250+ (Figure 1). Outcomes of the Bland-Altman analyses are presented in Table 4. BFEN314+ overestimated time spent in MPA by a small margin of 1.5% (limits of agreement [LoA]: -57.5% – 60.6%), whereas ENMO192+ and GENEA250+ overestimated time spent in MPA by 30.1% (LoA: -99.6% – 39.4%) and 31.0% (LoA: -104.1% – 42.0%), respectively. Overestimation of time spent in VPA was larger for BFEN314+ (92.2% [LoA: -54.6% – 238.9%]) compared to ENMO192+ (58.5% [LoA: -127.4% – 244.5%]) and GENEA250+ (75.2% [LoA: -91.8% – 242.2%]). Mean bias for time spent in MVPA was small for ENMO192+ (-1.1% [LoA: -55.9% – 53.7%]) and GENEA250+ (2.2% [LoA: -52.2% – 56.5%]), whereas time spent MVPA was overestimated by BFEN314+ to a larger extent (29.3% [LoA: -25.3% – 83.9%]). At the individual level, LoAs were wide for all cut-points and for all intensities, especially for VPA estimates from all cut-points and for MPA estimates from the ENMO192+ and GENEA250+. Systematic bias (p<0.05) was found for time spent in all intensities estimated by all cut-points, with the exceptions of time spent in MPA estimated by BFEN314+ and GENEA250+, indicating that errors increased with increasing time spent in the intensities.
Figure 1. 95% equivalence test for raw wrist acceleration-based estimated time spent in physical activity intensities.
Times estimated by wrist-worn cut-points are equivalent to indirect calorimetry if 90% confidence intervals lie entirely within the equivalence region of indirect calorimetry. MPA: moderate physical activity; VPA: vigorous physical activity; MVPA: moderate-to-vigorous physical activity; ENMO: cut-points developed using Euclidian norm minus one; GENEA: cut-points developed using the GENEActiv post processing software; BFEN: cut-points developed using Bandpass Filtered followed by Euclidian Norm.
Table 4. Agreement analysis of raw wrist acceleration-based estimations of physical activity intensities compared to indirect calorimetry.
| Intensity | Mean bias (%) | Limits of agreement | p-value slope |
|---|---|---|---|
| ENMO192+ | |||
| MPA | 30.1 | -39.4 – 99.6 | 0.04 |
| VPA | -58.5 | -244.5 – 127.4 | 0.00 |
| MVPA | 1.1* | -53.7 – 55.9 | 0.00 |
| GENEA250+ | |||
| MPA | 31.0 | -42.0 – 104.1 | 0.05 |
| VPA | -75.2 | -242.2 – 91.8 | 0.00 |
| MVPA | -2.2* | -56.5 – 52.2 | 0.00 |
| BFEN314+ | |||
| MPA | -1.5* | -60.6 – 57.5 | 0.28 |
| VPA | -92.2 | -238.9 – 54.6 | 0.00 |
| MVPA | -29.3 | -83.9 – 25.3 | 0.00 |
MPA: moderate physical activity; VPA: vigorous physical activity; MVPA: moderate-to-vigorous physical activity; ENMO: cut-points developed using Euclidian norm minus one; GENEA: cut-points developed using the GENEActiv post processing software; BFEN: cut-points developed using Bandpass Filtered followed by Euclidian Norm. Mean bias was calculated as: measured intensity time – estimated intensity time; a positive value indicates underestimation; a negative value indicates overestimation.
Significantly equivalent to indirect calorimetry (p < 0.05).
Supplementary analyses (see Tables and Figure, Supplemental Digital Content 2, Supplementary analyses for the raw wrist acceleration cut-points using a ≥4-MET MVPA definition, http://links.lww.com/MSS/B68) indicated that classification accuracy for MPA, VPA and non-MVPA remained similar when 1 MET was defined using predicted REE and a 4-MET threshold for MPA was applied to the data (ENMO192+, κ = 0.65 [95% CI: 0.64 to 0.66], GENEA250+, κ = 0.71 [95% CI: 0.70 to 0.72], BFEN314+, κ = 0.75 [95% CI: 0.74 to 0.76]). Although ROC-AUC values for MVPA (ENMO192+, 0.85 [95% CI: 0.85 to 0.86]; GENEA250+, 0.86 [95% CI: 0.85 to 0.86]; BFEN314+, 0.87 [95% CI: 0.87 to 0.88]) were similar to the primary analyses, slightly more non-MVPA epochs were correctly classified (see Table, Supplemental Digital Content 2, 2.1: Contingency tables for classification accuracy of raw wrist acceleration cut-points using a ≥4-MET MVPA definition, http://links.lww.com/MSS/B68). Although time spent in MVPA estimated by ENMO192+ and GENEA250+ using the ≥4-MET MVPA definition was not equivalent to indirect calorimetry as they were in the primary analyses, the means and/or 90% CIs for estimated time spent in MPA and MVPA for ENMO192+ and GENEA250+ overlapped the equivalence region and thus approached equivalence. BFEN314+ overestimated time spent in MVPA for both the 3-MET (1 MET = measured REE) approach (29.3% [LoA: -25.3% – 83.9%]) and the 4-MET (1 MET = predicted REE) approach (18.3% [LoA: -13.5% - 50.2%]) (see Table, Supplemental Digital Content 2, 2.2: Agreement analysis of raw wrist acceleration-based estimations of physical activity intensities compared to indirect calorimetry using a ≥4-MET MVPA definition, http://links.lww.com/MSS/B68). Time spent in MPA estimated by BFEN314+ was no longer equivalent to the criterion measure, whereas time spent in VPA was (p<0.01) (see Figure, Supplemental Digital Content 2, 2.3: 95% equivalence test for raw wrist acceleration-based estimated time spent in physical activity intensities using a ≥4-MET MVPA definition, http://links.lww.com/MSS/B68). In contrast, when defining MVPA as ≥4-METs, fewer MPA epochs were misclassified by BFEN314+ as VPA compared to the 3-MET approach, however more VPA epochs were misclassified as MPA. The overestimation of time spent in VPA from BFEN314+ was small for the 4-MET approach (0.5% [LoA: -39.7% – 40.6%]), whereas overestimation of time spent in MPA for BFEN314+ was larger (34.4% [LoA: -20.4% – 89.1%]). At the individual level, errors for all cut-points were decreased for time spent in VPA when using the 4-MET approach, but increased for time spent in MPA, compared to outcomes from the 3-MET approach.
Discussion
Current international PA guidelines specify that children should accumulate a minimum of 60 minutes per day of MVPA (27). Therefore, the accurate measurement of MVPA is central to understanding the prevalence and patterns of PA, the dose of PA required to achieve health benefits, the determinants of PA, and the effect of PA interventions for children, which typically target MVPA. This study simultaneously cross-validated three previously published wrist acceleration cut-points for the classification of MVPA in children. ENMO192+, GENEA250+ and BFEN314+ demonstrated good classification accuracy for MVPA. However, while time spent in MVPA estimated by ENMO192+ and GENEA250+ were equivalent to indirect calorimetry, misclassification of non-MVPA as MVPA resulted in an overestimation of time spent in MVPA for BFEN314+. Although ENMO192+ and GENEA250+ classified non-MVPA more accurately than BFEN314+, these cut-points still misclassified a significant proportion of MVPA epochs as non-MVPA (37.6% and 27.2%, respectively). Findings were relatively consistent in supplementary analyses, where predicted REE was used to define 1 MET and MVPA was defined as ≥4METs. The classification accuracy of MPA, VPA and MVPA remained relatively similar for all cut-points compared to previous analyses and, although time spent in MVPA estimated by ENMO192+ and GENEA250+ were no longer equivalent to indirect calorimetry, estimates approached equivalence.
Findings from the current study were similar to findings in previous independent cross-validation studies, which demonstrated good classification accuracy for MVPA estimates from raw acceleration wrist cut-points (10, 12), and that classification for VPA is generally higher than for MPA (10–12). Even though classification of MPA, VPA and MVPA was most accurate for BFEN314+, ENMO192+ and GENEA250+ estimated time spent in MVPA more accurately than BFEN314+. Time spent in MVPA was overestimated by BFEN314+ because a relatively large proportion (19.7%) of non-MVPA was misclassified as MPA, which was in agreement with Schaefer et al.’s (10) application in free-living individuals. This misclassification could be explained by activities of light intensity that involve vigorous wrist movements. For example, BFEN314+ misclassified 66.4% of non-MVPA as MPA during the non-MVPA activity “Getting ready for school” (see Table, Supplemental Digital Content 3, Confusion matrices for the raw wrist acceleration cut-points using a ≥3-MET MVPA definition, http://links.lww.com/MSS/B69), an activity of low intensity that involved relatively high wrist motion (e.g., while getting dressed, packing a schoolbag, brushing hair etc.) The opposite effect may occur when MVPA activities involve limited wrist movement. As such, the ENMO192+ and GENEA250+ misclassified 82.3% and 77.1%, respectively, of MPA as non-MVPA during “Tidy up”, an activity of MPA intensity that may have involved limited upper body and wrist motions due to carrying objects while walking. Because of the public health focus on MVPA, misclassification by wrist cut-points of MPA as VPA and vice-versa may not represent a major measurement limitation. However, increased interest among researchers in the influence of sedentary behaviors, defined as any waking behaviors in a sitting or reclining position that require an energy expenditure of ≤1.5 METs (28), and light physical activity (1.5 to <3.0 METs), on health makes it critical to discriminate between these behaviors and MVPA. Previous studies indicate that accurate assessment of sedentary behaviors and the number of breaks in sedentary time based on a lack of wrist movement is challenging (11, 29, 30). The findings from this study confirm that the use of the magnitude of acceleration only might not be effective in distinguishing MVPA from non-MVPA. This finding is relatively consistent with previous studies using cut-points based on proprietary activity “counts” (31–33). This is likely because the association between counts or raw acceleration and energy expenditure, whether on the hip or wrist, differs for different types of physical activities, resulting in cut-points performing well for some activities and demonstrating considerable misclassification during other activities. It should be noted that the benefit of using raw acceleration-based cut-points over using count-based cut-points remains unclear, as in general cut-points result in misclassification, which was also demonstrated by the results in this study for all cut-points. Therefore, progress on alternative approaches, such as those utilizing machine learning (29, 33, 34), may be required. However, similar to the inconsistencies that occur because of the existence of multiple cut-points, the existence of different machine learning approaches and models, such as artificial neural networks (35), decision trees (36) and hidden Markov models (37), presents further challenges and evidence to reach consensus on the most accurate approach for categorizing physical activity intensities in children is required.
An additional limitation of the wrist cut-points validated in the current study is that calibration studies used different processing methodologies. While Schaefer et al. (10) used a filtering approach to remove static accelerations from the tri-axial data, Hildebrand et al. (11) and Phillips et al. (9) subtracted the value of gravity from the vector magnitude, in order to focus the outcome variable on dynamic rather than static accelerations. Hildebrand et al. (11) used the ENMO method, which rounds negative values, resulting from subtracting the vector magnitude by 1g, up to zero. Phillips et al. (9) on the other hand, replaced the negative values with their absolute values and summed the resulting values, which creates a dependency on sample frequency, and thus the cut-points should be converted when using different sample frequencies in order to compare results across studies. The ENMO192+ and BFEN314+ were developed using averaged acceleration magnitudes and can be used for different sample frequencies and epoch lengths. The different processing methods also resulted in different units for the outcomes; Hildebrand et al. (11) and Schaefer et al. (10) used gravity units in g and mg, respectively, whereas Phillips et al. (9) used gravity-based acceleration seconds. Taking all of this into account makes it complicated to compare results from the different cut-points and, as the field progresses, it is important that procedures are standardized based on evidence. Furthermore, some data indicate that raw acceleration output from the GENEActiv and ActiGraph may differ in children during common activities (11). This is likely because manufacturer specific transformations (e.g. filtering) are applied to the raw acceleration data, resulting in different outputs from different devices that may not be a representation of the actual raw acceleration signals (38). As such, our findings may only apply to the GENEActiv monitor and further evaluation across different monitor brands is required.
A strength of this study was that three recently developed sets of raw wrist acceleration cut-points were evaluated simultaneously, against a criterion measure. The study included a broad age range and an equal distribution of age and sex across the sample. Additionally, a range of tasks, beyond treadmill-based ambulatory activities, that are likely to resemble children’s free-living behaviors were included in the protocol. Although these activities reflect daily activities that children typically engage in, the findings of the present study should be confirmed under free-living conditions. A potential limitation of this study is that validation focused on MVPA and did not include light PA or sedentary behavior. Our previous cross-validation study (29) of sedentary cut-points demonstrated that, while hip-based cut-points typically misclassify light activities (e.g. standing still) as sedentary postures, wrist cut-points exhibit some misclassification of non-sedentary behaviors as sedentary and vice-versa. Therefore, it is essential to apply the most accurate intensity specific cut-points for accurate estimates of sedentary behaviors and light intensity PA. However, in order to investigate the accuracy of cut-points for distinguishing sedentary behaviors from light intensity PA, postures such as sitting and standing should be evaluated. This is typically performed using alternative criterion measures, such as direct observation, as described in our previous work (39). Another potential limitation is that acceleration signals were not calibrated to local gravity before analysis in order to minimize sensor calibration errors, as described by van Hees et al. (40). Furthermore, body accelerations and metabolic rate during the exercise bouts may not have been aligned due to lags in oxygen consumption, and true classification accuracy may have been underestimated. However, this data reduction approach reflects how cut-points are used in free-living population studies and, because the approach was applied consistently across cut-points, one cut-point was not biased over the other.
In conclusion, although raw acceleration wrist cut-points exhibited good accuracy for classifying MVPA in children, all cut-points misclassified a significant proportion of MVPA epochs as non-MVPA. While the cut-points demonstrated acceptable estimates of time spent in MPA, VPA, and MVPA at the group level, their application was less accurate for individual measures. When combined with the practical advantages of wrist worn placement, surveillance application of the raw wrist acceleration cut-points would be acceptable for group level estimates of MVPA, although alternative data processing approaches such as machine learning methods may be needed to achieve a generally higher accuracy for the assessment of PA intensities among individual children.
Supplementary Material
Acknowledgements
We would like to thank all children and their parents for their participation. We also thank Melinda Smith for her assistance with recruitment and data collection. This study was funded by the National Heart Foundation of Australia (G11S5975). DPC is supported by an Australian Research Council Discovery Early Career Researcher Award (DE140101588). ADO is supported by a National Heart Foundation of Australia Career Development Fellowship (CR11S 6099). TH is funded by a National Health and Medical Research Council Early Career Fellowship (APP1070571). UE is funded by the Research Council of Norway (249932/F20). The work of UE and SB is funded by the UK Medical Research Council (MC_UU_12015/3). ST is supported by the National Health and Medical Research Council Centre of Research Excellence on Sitting Time and Chronic Disease Prevention (APP1057608).
Footnotes
Conflict of Interest
The authors have no conflict of interest to declare. The results of the present study do not constitute endorsement by the American College of Sports Medicine. The results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- 1.Rennie KL, Wareham NJ. The validation of physical activity instruments for measuring energy expenditure: problems and pitfalls. Public Health Nutr. 1998;1(04):265–71. doi: 10.1079/phn19980043. [DOI] [PubMed] [Google Scholar]
- 2.Trost SG. State of the Art Reviews: Measurement of Physical Activity in Children and Adolescents. Am J Lifestyle Med. 2007;1(4):299–314. [Google Scholar]
- 3.Freedson PS, John D. Comment on estimating activity and sedentary behavior from an accelerometer on the hip and wrist. Med Sci Sports Exerc. 2013;45(5):962–3. doi: 10.1249/MSS.0b013e31827f024d. [DOI] [PubMed] [Google Scholar]
- 4.UK Biobank. Category 2 enhanced phenotyping at baseline assessment visit in last 100-150,000 participants. [cited 2017 Jan 21];2009 [internet] Available from: http://www.ukbiobank.ac.uk/wp-content/uploads/2011/06/Protocol_addendum_2.pdf.
- 5.da Silva IC, van Hees VT, Ramires VV, Knuth AG, Bielemann RM, Ekelund U, et al. Physical activity levels in three Brazilian birth cohorts as assessed with raw triaxial wrist accelerometry. Int J Epidemiol. 2014;43(6):1959–68. doi: 10.1093/ije/dyu203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–23. doi: 10.1136/bjsports-2014-093546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowlands AV, Rennie K, Kozarski R, Stanley RM, Eston RG, Parfitt GC, et al. Children’s physical activity assessed with wrist-and hip-worn accelerometers. Med Sci Sports Exerc. 2014;46(6):2308–16. doi: 10.1249/MSS.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 8.Fairclough SJ, Noonan R, Rowlands AV, van Hees V, Knowles Z, Boddy LM. Wear Compliance and Activity in Children Wearing Wrist and Hip-Mounted Accelerometers. Med Sci Sports Exerc. 2016;48(2):245–253. doi: 10.1249/MSS.0000000000000771. [DOI] [PubMed] [Google Scholar]
- 9.Phillips LR, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. J Sci Med Sport. 2013;16(2):124–8. doi: 10.1016/j.jsams.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Schaefer CA, Nigg CR, Hill JO, Brink LA, Browning RC. Establishing and evaluating wrist cutpoints for the GENEActiv accelerometer in youth. Med Sci Sports Exerc. 2014;46(4):826. doi: 10.1249/MSS.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hildebrand M, Van Hees VT, Hansen BH, Ekelund U. Age-group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–24. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 12.Duncan MJ, Wilson S, Tallis J, Eyre E. Validation of the Phillips et al. GENEActiv accelerometer wrist cut-points in children aged 5–8 years old. Eur J of Pediatr. 2016;175(12):2019–21. doi: 10.1007/s00431-016-2795-6. [DOI] [PubMed] [Google Scholar]
- 13.Kim Y, Hibbing P, Saint-Maurice PF, Ellingson LD, Hennessy E, Wolff-Hughes DL, et al. Surveillance of youth physical activity and sedentary behavior with wrist accelerometry. Am J Prev Med. 2017;52(6):872–9. doi: 10.1016/j.amepre.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welk GJ, McClain J, Ainsworth BE. Protocols for evaluating equivalency of accelerometry-based activity monitors. Med Sci Sports Exerc. 2012;44(1):S39–49. doi: 10.1249/MSS.0b013e3182399d8f. [DOI] [PubMed] [Google Scholar]
- 15.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 16.Weir JBV. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109(1–2):1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saint-Maurice PF, Kim Y, Welk GJ, Gaesser GA. Kids are not little adults: what MET threshold captures sedentary behavior in children? Eur J Appl Physiol. 2016;116(1):29–38. doi: 10.1007/s00421-015-3238-1. [DOI] [PubMed] [Google Scholar]
- 18.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–8. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 19.Schuna JM, Jr, Barreira TV, Hsia DS, Johnson WD, Tudor-Locke C. Youth Energy Expenditure During Common Free-Living Activities and Treadmill Walking. J Phys Act Health. 2016;13(6):S29–S34. doi: 10.1123/jpah.2015-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sasaki JE, Howe CA, John D, Hickey A, Steeves J, Conger S, et al. Energy Expenditure for 70 Activities in Children and Adolescents. Journal of Physical Activity and Health. 2016;13(6 Suppl 1):S24–S8. doi: 10.1123/jpah.2015-0712. [DOI] [PubMed] [Google Scholar]
- 21.Trost SG, Drovandi CC, Pfeiffer K. Developmental Trends in the Energy Cost of Physical Activities Performed by Youth. J Phys Act Health. 2016;13(6):S35–S40. doi: 10.1123/jpah.2015-0723. [DOI] [PubMed] [Google Scholar]
- 22.Schofield W. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39:5–41. [PubMed] [Google Scholar]
- 23.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. [PubMed] [Google Scholar]
- 24.Metz CE. Basic principles of ROC analysis. Semin Nuel Med. 1978;8(4):283–98. doi: 10.1016/s0001-2998(78)80014-2. [DOI] [PubMed] [Google Scholar]
- 25.Batterham M, Van Loo C, Charlton K, Cliff D, Okely A. Improved interpretation of studies comparing methods of dietary assessment: Combining equivalence testing with the limits of agreement. Br J Nutr. 2016;115(7):1273–1280. doi: 10.1017/S0007114516000040. [DOI] [PubMed] [Google Scholar]
- 26.Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. The statistician. 1983:307–17. [Google Scholar]
- 27.WHO. Global Recommendations on Physical Activity for Health. World Health Organization; 2010. [cited 2016 Dec 15]. [internet]. Available from: apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf. [PubMed] [Google Scholar]
- 28.Sedentary Behavior Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37:540–2. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 29.van Loo CMT, Okely AD, Batterham MJ, Hinkley T, Ekelund U, Brage S, et al. Wrist Accelerometer Cut-points for Classifying Sedentary Behavior in Children. Med Sci Sports Exerc. 2017;49(4):813–822. doi: 10.1249/MSS.0000000000001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberger ME, Haskell WL, Albinali F, Mota S, Nawyn J, Intille S. Estimating activity and sedentary behavior from an accelerometer on the hip or wrist. Med Sci Sports Exerc. 2013;45(5):964. doi: 10.1249/MSS.0b013e31827f0d9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Med Sci Sports Exerc. 2006;38(2):380–7. doi: 10.1249/01.mss.0000183848.25845.e0. [DOI] [PubMed] [Google Scholar]
- 32.Janssen X, Cliff DP, Reilly JJ, Hinkley T, Jones RA, Batterham M, et al. Predictive validity and classification accuracy of ActiGraph energy expenditure equations and cut-points in young children. PLoS One. 2013;8(11) doi: 10.1371/journal.pone.0079124. e79124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trost SG, Wong W-K, Pfeiffer KA, Zheng Y. Artificial neural networks to predict activity type and energy expenditure in youth. Med Sci Sports Exerc. 2012;44(9):1801–9. doi: 10.1249/MSS.0b013e318258ac11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hagenbuchner M, Cliff DP, Trost SG, Van Tuc N, Peoples GE. Prediction of activity type in preschool children using machine learning techniques. J Sci Med Sport. 2015;18(4):426–31. doi: 10.1016/j.jsams.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Rothney MP, Neumann M, Béziat A, Chen KY. An artificial neural network model of energy expenditure using nonintegrated acceleration signals. J Appl Physiol. 2007;103(4):1419–27. doi: 10.1152/japplphysiol.00429.2007. [DOI] [PubMed] [Google Scholar]
- 36.Bonomi AG, Plasqui G, Goris AH, Westerterp KR. Improving assessment of daily energy expenditure by identifying types of physical activity with a single accelerometer. J Appl Physiol. 2009;107(3):655–61. doi: 10.1152/japplphysiol.00150.2009. [DOI] [PubMed] [Google Scholar]
- 37.Pober DM, Staudenmayer J, Raphael C, Freedson PS. Development of novel techniques to classify physical activity mode using accelerometers. Med Sci Sports Exerc. 2006;38(9):1626–34. doi: 10.1249/01.mss.0000227542.43669.45. [DOI] [PubMed] [Google Scholar]
- 38.John D, Freedson P. ActiGraph and Actical physical activity monitors: a peek under the hood. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S86–9. doi: 10.1249/MSS.0b013e3182399f5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Loo CMT, Okely AD, Batterham M, Hinkley T, Ekelund U, Brage S, et al. Predictive validity of a thigh-worn accelerometer METs algorithm in 5-to 12-Year-old children. J Phys Act Health. 2016;13:S78–S83. doi: 10.1123/jpah.2015-0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva IC, et al. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol. 2014;117(7):738–44. doi: 10.1152/japplphysiol.00421.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.