Abstract
Objective
Ovarian cancer comprises several subtypes with widely differing levels of survival. We aimed to explore international variation in survival for each subtype to help interpret international differences in survival from all ovarian cancers combined. We also examined differences in stage-specific survival.
Methods
The CONCORD programme is the largest population-based study of global trends in cancer survival, including data from 60 countries for 695,932 women (aged 15-99 years) diagnosed with ovarian cancer during 1995-2009. We defined six histological groups: type I epithelial, type II epithelial, germ cell, sex cord-stromal, other specific non-epithelial and non-specific morphology, and estimated age-standardised 5-year net survival for each country by histological group. We also analysed data from 67 cancer registries for 233,659 women diagnosed from 2001 to 2009, for whom information on stage at diagnosis was available. We estimated age-standardised 5-year net survival by stage at diagnosis (localised or advanced).
Results
Survival from type I epithelial ovarian tumours for women diagnosed during 2005-09 ranged from 40 to 70%. Survival from type II epithelial tumours was much lower (20-45%). Survival from germ cell tumours was higher than that of type II epithelial tumours, but also varied widely between countries. Survival for sex-cord stromal tumours was higher than for the five other subtypes. Survival from localised tumours was much higher than for advanced disease (80% vs. 30%).
Conclusions
There is wide variation in survival between histological groups, and stage at diagnosis remains an important factor in ovarian cancer survival. International comparisons of ovarian cancer survival should incorporate histology.
Introduction
The CONCORD-2 study, a comprehensive study on cancer survival, showed wide variation in 5-year net survival for ovarian cancer among over 779,000 women diagnosed in 61 countries (1). Age-standardised survival from ovarian cancer for all histological groups combined was around 30-40% in most countries from 1995 to 2009, but it varied widely between countries. Most international comparisons of ovarian cancer survival include all histological groups combined (1–3). The different histological groups have unique molecular pathways and treatment, and survival also differs widely, especially for type I and type II epithelial tumours (4–7). We have examined patterns of survival for each distinct histological group in order to gain a better understanding of international differences in ovarian cancer survival.
Type I epithelial tumours include low-grade serous, endometrioid, clear cell, mucinous and transitional cell (Brenner) carcinomas, while type II epithelial tumours include high-grade serous, undifferentiated carcinoma and malignant mixed mesodermal tumours (carcinosarcoma). Type II epithelial tumours account for approximately 70% of all malignant ovarian tumours, while only 22% of ovarian tumours are type I epithelial. Type I epithelial tumours often present at an early stage and have better prognosis than Type II epithelial tumours, which typically present at an advanced stage (4). Germ cell and sex cord-stromal tumours are rarer types of ovarian cancer, but they generally have much better prognosis than type II epithelial tumours.
Stage at diagnosis also affects survival. Though most women are diagnosed at an advanced stage, stage-specific survival also differs widely between countries (2). In a comparison of one-year net survival between six high-income countries, Denmark had the highest percentage of women with advanced disease and the second lowest survival for all stages combined (2). Thus, the international variation in ovarian cancer survival may be partially explained by the distribution of stage at diagnosis.
The CONCORD-2 study on the global surveillance of cancer survival has shown the extent to which ovarian cancer survival for all histological groups combined varies worldwide (1). However, it remains unclear how much of the variation in ovarian cancer survival could be attributed to international variation in survival for each histological group. We aimed to examine survival from ovarian cancer by histological group and stage at diagnosis in order to improve understanding of international differences in ovarian cancer survival.
Material and methods
The CONCORD-2 study was based on data for over 25.7 million patients diagnosed with one of 10 cancers, contributed by 279 population-based cancer registries in 67 countries. The data included over 779,000 women diagnosed with ovarian cancer in 61 countries during the 15-year period of 1995 to 2009 (1). The CONCORD-2 protocol, ethical approvals and quality control procedures have been described (1).
We analysed data for women (aged 15-99 years) diagnosed during 1995 to 2009 with a cancer of the ovary, fallopian tube, uterine ligaments and adnexa, other specified and unspecified female genital organs, peritoneum and retroperitoneum (International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) topography codes C56.9, C57.0-C57.4, C57.7-C57.9, C48.0-C48.2) (8). Recent evidence suggests that high-grade serous carcinoma, the most common type of ovarian cancer, originates in the fallopian tube. Therefore, cancers of the fallopian tube were included in a broader definition of ovarian cancer (4). Similarly, primary peritoneal malignancies are managed in the same way as advanced-stage epithelial ovarian cancer, and they are also included (4). Tumours of the uterine ligaments and adnexa, other specified and unspecified female genital organs and retroperitoneum were included because of the close proximity of these sites to the ovaries, fallopian tubes and peritoneum. Follow-up until 31 December 2009 for vital status was available. Women diagnosed with ovarian cancer as a second or higher-order primary tumour are included in the analysis, in addition to those for whom ovarian cancer was their first cancer. Women whose cancer registration was from a death certificate or autopsy only were excluded, because their true survival time was unknown.
In ICD-O-2, some borderline tumours were coded as malignant, or with a behaviour code of 3. The behaviour code changed, however, from malignant (behaviour code of 3) to not malignant or of borderline malignancy (behaviour code of 0 or 1) in ICD-O-3. Due to this change in coding, some women diagnosed with borderline tumours were included in the data submissions. ICD-O-3 morphology codes were checked to detect borderline tumours that are now coded with behaviour codes of 0 or 1, and these tumours were then excluded from analysis because their inclusion would inflate survival estimates.
We defined six histological groups based on ICD-O-3 codes, literature (9) and clinical advice: type I epithelial, type II epithelial, germ cell, sex cord-stromal, other specific non-epithelial and non-specific morphology [Table 1]. Clear cell, endometrioid, mucinous, squamous and transitional cell (Brenner) carcinomas were classified as type I epithelial. Serous, mixed epithelial-stromal and undifferentiated or other classified epithelial carcinomas were grouped as type II epithelial. Tumours with a non-specific morphology code (8000-8004) were analysed separately. Survival for tumours with unknown morphology (0.1% of cases) is not reported. We included in the analysis all microscopically verified tumours. We also included tumours that were reported as not microscopically verified but for which we had a specific ICD-O-3 morphology code (any valid ICD-O-3 code except 8000-8004).
Table 1. Ovarian cancer histological groups and subtypesa.
| Histological group | Histological subtype | ICD-O-3 morphology code |
|---|---|---|
| Type I epithelial | Clear cell carcinoma | 8005, 8310, 8443, 9110 |
| Endometrioid carcinomab | 8380, 8382–8383, 8560, 8570 | |
| Mucinous carcinoma | 8470–8471, 8480–8482, 8490 | |
| Squamous carcinoma | 8051–8084 | |
| Transitional cell or Brenner carcinoma | 8120–8131, 9000 | |
| Type II epithelial | Serous carcinomac | 8050, 8441, 8450, 8460–8461 |
| Mixed epithelial-stromal carcinoma | 8313, 8323, 8381, 8930–8991, 9010–9030 | |
| Undifferentiated or other epithelial | 8010–8015, 8020–8046, 8090–8110, 8140–8231, 8246–8300, 8311–8312, 8314–8322, 8324–8325, 8336–8337, 8341–8375, 8384–8440, 8452–8454, 8500–8551, 8561–8562, 8571–8589 | |
| Germ cell | Germ cell | 8240–8245, 8330–8335, 8340, 9060–9105, 9380–9523 |
| Sex cord-stromal | Sex cord-stromal | 8590–8671, 8810 |
| Other specific non-epithelial | Other specific non-epithelial | 8680–8806, 8811–8921, 9040–9055, 9120–9373, 9530–9589 |
| Non-specific | Non-specific | 8000–8004 |
No information on grade was available, therefore all endometrioid tumours were classified as type I epithelial.
No information on grade was available, therefore all serous tumours were classified as type II epithelial.
Borderline tumours (ICD-O-3 codes: 8442, 8444, 8451, 8462, 8463, 8472, 8473) were excluded from the analysis of distribution of histological groups (see text).
Information on stage at diagnosis was available only from 2001; therefore, the stage-specific analysis only includes patients diagnosed between 2001 and 2009. Stage at diagnosis was categorised into localised or advanced. Registries submitted stage data coded to one of several classifications: UICC Tumour-Node-Metastasis (TNM) staging system (7th edition), the Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) system or SEER Summary Stage 2000. We received data on pathological and/or clinical T, N and M, as well as tumour size (in millimetres) and the number of positive lymph nodes. These data were used to create a final stage at diagnosis variable, prioritising pathological TNM information, supplemented with clinical TNM information where missing. Information on FIGO stage and SEER Summary Stage 2000 was used to supplement missing TNM information when both pathological and clinical TNM were missing, and if no data on tumour size or number of positive lymph nodes were available. TNM Stage I tumours are confined to the ovaries at diagnosis; and were defined as localised in these analyses. Stage II tumours are usually confined to the ovaries, but were defined as advanced in these analyses. Stage III tumours have spread to regional lymph nodes and Stage IV tumours have metastasised to other organs. TNM Stage III and Stage IV tumours were defined as advanced. Where there was no information available on stage, we classified the tumours as of unknown stage at diagnosis.
We analysed survival by histological group in each country. We analysed survival by stage at diagnosis in each country, and where possible, for each registry, separately from the analysis by histological group. Only countries with at least 10 women for a given histological group for all years combined were included in the analysis for that histological group. For the stage-specific analysis, we included registries with at least 10 women available for analysis in each stage for any given time period. If more than 30% of tumours were unknown stage at diagnosis for a given registry during 2004-2009, then that registry was excluded from the stage-specific analysis. If fewer than 10 women were available for analysis in a given registry, then the registry was excluded from the analysis by stage at diagnosis. Registries for which net survival estimates were considered as less reliable in the main CONCORD-2 analysis (1) were also excluded. Country-level survival estimates were derived by pooling data for registries that were included in the registry-specific analysis by stage at diagnosis. We only included data from countries that were included in the analysis of specific histological groups in the analysis for non-specific morphology, given that there were at least 10 women with non-specific tumours available for all years combined. If fewer than 50 women were available for survival analysis by morphological group or stage at diagnosis in a given calendar period, the data for that country were merged.
Net survival is defined as the probability of survival for cancer patients up to a given point in time after diagnosis (for example, 5 years) if death from cancer were to be the only cause of death. Net survival controls for the background mortality of competing causes of death in a population. We used the Pohar Perme estimator of net survival (10), which allows for the fact that competing risks of death increase with age. The Pohar Perme estimator was implemented using stns (11) in Stata version 14 (12).
Net survival is reported for each country and histological group, and separately for each registry and each stage at diagnosis. Survival by histological group was estimated for women diagnosed during 1995-1999, 2000-2004 and 2005-2009. The cohort approach was used for women diagnosed during 1995-1999 and 2000-2004, because five or more years of follow-up were available for all patients, while a period approach was used for 2005-2009. Stage-specific survival was estimated with a cohort approach for 2001-03 and a complete approach was used for 2004-2009.
Survival estimates for all ages combined were age-standardised, where possible, with the International Cancer Standard Survival (ICSS) weights (13). Age at diagnosis was categorised into five age groups: 15-44, 45-54, 55-64, 65-74 and 75-99 years. If an age-specific estimate could not be produced, or fewer than 10 women were available for analysis in an age group, data for adjacent age groups were pooled and the re-estimated survival used for both of the original age groups. If two or more age-specific estimates could not be produced, fewer than 10 women were available for analysis in two or more age groups, only the unstandardised estimate is reported.
Results
Data for a total of 695,932 women were available for analysis of survival by histological group [appendix Figure 1], including 98.3% with a specific morphology, 1.6% with non-specific morphology and 0.1% with unknown morphology [Table 2]. Survival by histological group was estimated for all stages combined. Most women were diagnosed with Type II epithelial tumours. The mean age at diagnosis varied between histological group, ranging from 36 years for germ cell tumours to 66 years for tumours of non-specific morphology.
Table 2. Worldwide distribution of histology and mean age at diagnosis, 1995–2009.
| Histological group | No. of patients | % | Mean age in years (SD)a |
|---|---|---|---|
| Type I epithelialb | 152,970 | 22.0 | 58 (14) |
| Type II epithelialc | 488,634 | 70.2 | 64 (14) |
| Germ cell | 13,306 | 1.9 | 36 (18) |
| Sex cord-stomal | 11,430 | 1.6 | 54 (16) |
| Other specific non-epithelial | 17,619 | 2.5 | 61 (15) |
| Non-specific tumours | 11,282 | 1.6 | 66 (17) |
| Missing morphology | 691 | 0.1 | 64 (16) |
Standard deviation.
No information on grade was available, therefore all endometrioid tumours were classified as type I epithelial.
No information on grade was available, therefore all serous tumours were classified as type II epithelial.
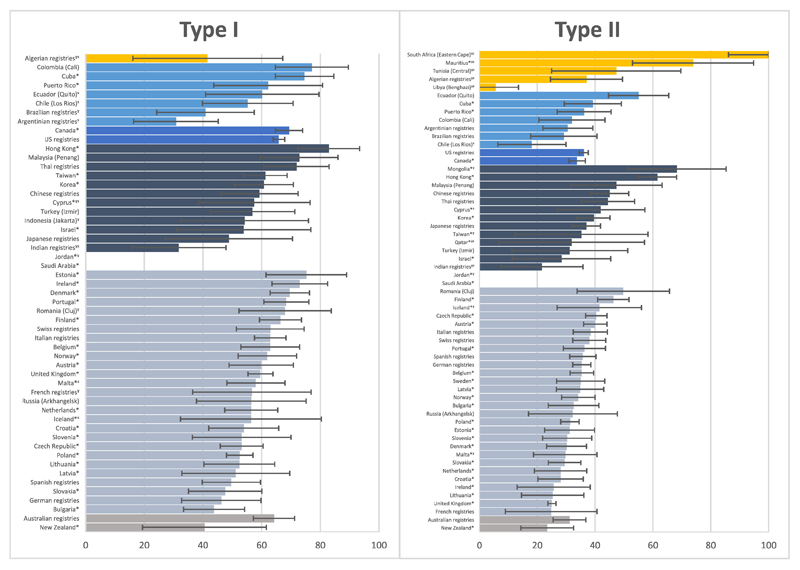
Net survival for women diagnosed with type I epithelial tumours five years after diagnosis was fairly high, generally 50-60% [Figure 1]. During 2005 to 2009, age-standardised 5-year survival for type I epithelial tumours varied widely, with the highest survival in Hong Kong (82.9%, 72.4-93.4%) and the lowest in Argentina (30.8%, 16.3-45.2%) [appendix Table 1]. Age-standardised survival from type I epithelial tumours also varied within each continent and over time. The between-country variation in survival was widest in Central and South America (from 30.8%, 16.3-45.2% in Argentina to 77.1%, 64.7-89.6% in Colombia) for women diagnosed during 2004-2009. Age-standardised net survival from type I tumours increased over time in all countries in Central and South America and North America for which data were available. In Asia, Europe, and Oceania, most countries saw an improvement in survival from type I tumours, but survival actually fell over time for some countries in these regions (from 65.5%, 59.0-72.1% to 60.8%, 50.7-70.8% in Korea and from 60.3%, 49.8-70.7% to 56.9%, 42.6-71.3% in Turkey (Izmir)) [appendix Table 1].
Figure 1.
5-year age-standardised net survival for Type 1 and Type 2 epithelial ovarian tumours by country, 2005-2009
*Data with 100% coverage of the national population.
ˠ Estimate not age-standardised.
ˢ Data for two or more calendar periods of diagnosis have been merged.
95% CI represented by error bars. Ranked from highest to lowest net survival by continent for women diagnosed in the calendar period of 2005-2009.
Survival from type II epithelial tumours five years after diagnosis was lower than that of type I epithelial tumours, around only 20-45% [Figure 1]. For women diagnosed between 2005 and 2009, the highest age-standardised survival was seen in Hong Kong (61.5%, 54.8-68.2%), compared with only 18.1% (6.3-29.9%) for women in Chile (Los Rios). Age-standardised survival from type II epithelial tumours increased over time for most countries worldwide, though there were decreases in some countries. In Cuba, for example, survival was 53.4% (45.1-61.7%) for women diagnosed during 1995-99, but only 39.2% (29.3-49.1%) during 2005-2009 [appendix Table 1]. Between-country variation was widest in Central and South America, where age-standardised 5-year survival was only 18.1% (6.3-29.9%) in Chile (Los Rios), but 55.0% (44.6-65.5%) in Ecuador (Quito). Type II epithelial was the only histological group for which survival estimates could be produced for all five African countries, but all of these estimates were not age standardised.
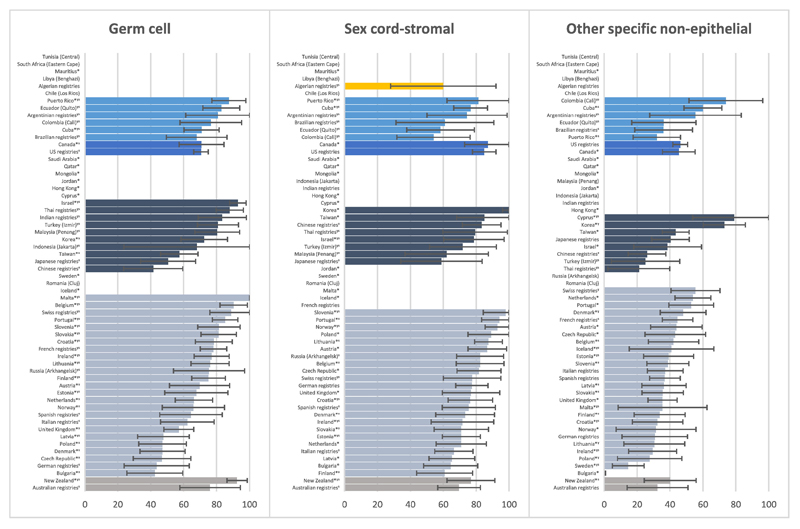
Survival from germ cell tumours could only be presented for all women diagnosed between 1995 and 2009, because these tumours are so uncommon. As a result, most survival estimates for germ cell tumours were not age standardised. This is because younger women have the highest incidence of germ cell tumours and this subtype is extremely rare in older women. Therefore, only for a few countries were enough women available in each age group to allow for age standardisation. Considering the age-standardised estimates, the highest was in Australia (76.0%, 57.6-94.5%) and the lowest in China (41.5%, 23.6-59.4%) [Figure 2; appendix Table 1].
Figure 2.
5-year age-standardised net survival for germ cell, sex cord-stromal and other specific non-epithelial ovarian tumours by country, 2005-2009
*Data with 100% coverage of the national population.
ˠ Estimate not age-standardised.
ˢ Data for two or more calendar periods of diagnosis have been merged.
95% CI represented by error bars. Ranked from highest to lowest net survival by continent for women diagnosed in the calendar period of 2005-2009.
Sex cord-stromal tumours are also rare, and survival could only be estimated in 11 countries for all three calendar periods. During 2005-2009, net survival was over 90% at 5 years after diagnosis in Korea (100.0%, 96.0-100.0%, n=207 women) and Portugal (94.1%, 83.3-100.0%, n=64 women). However, survival varied widely between countries, and the lowest survival was almost half that seen in Korea (Japan, 58.9%, 34.2-83.7%, n=63 women). Over time, survival from sex cord-stromal tumours remained either stable, or increased, in most countries [Figure 2; appendix Table 1].
Survival from other specific non-epithelial tumours was generally around 40% and slightly higher than that of type II epithelial tumours. The variation in survival was wide, ranging from only 0.3% (0.0-0.8%) in Bulgaria to 60.0% (48.4-71.5%) in Cuba [Figure 2; appendix Table 1].
Age-standardised net survival for tumours of non-specific morphology was generally lower than, that of tumours with specific morphology, with a few notable exceptions [appendix Table 2].
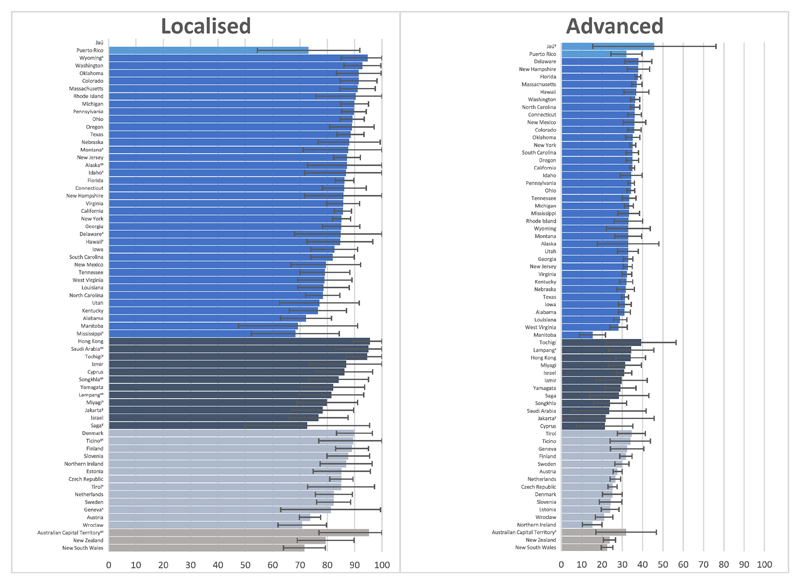
Data for 233,659 women were available from 67 registries in 25 countries for analysis of survival by stage [appendix Figure 2]. Survival by stage at diagnosis was estimated for all ovarian cancer histological groups combined. Only two Central and South American registries provided enough information on stage at diagnosis to be included in the analysis. In North America, one Canadian registry and 36 US registries provided adequate stage data. In Asia and Europe, only 12 and 13 registries, respectively, provided adequate stage data for inclusion in survival analyses. No data from African registries were available for analysis by stage at diagnosis.
Overall, 38,033 (16.3%) of these 233,659 women were diagnosed with localised ovarian cancer, 169,033 (72.3%) with advanced disease and 26,593 (11.4%) with unknown stage at diagnosis. The overall mean age was 64 years. Women diagnosed with localised ovarian cancer were the youngest (mean age 56 years), while women with an unknown stage at diagnosis were the oldest (mean age 68 years). The mean age at diagnoses for women diagnosed with advanced disease was 65 years.
Overall, 5-year age-standardised net survival for localised ovarian cancer (around 80%) was much higher than that for advanced (around 30%) and unknown stages (around 30%) [Figure 3]. For women diagnosed with localised ovarian cancer during 2004-2009, survival was much higher than for women diagnosed with advanced disease everywhere. In some countries, 5-year age-standardised survival was over 90% for localised tumours, with the highest survival in Hong Kong (95.5%, 89.4-100.0%). The lowest age-standardised survival from localised tumours was seen in Mississippi (US) (68.3%, 52.3-84.4%), however, this is still much higher than the highest survival for advanced-stage tumours during the same time period [appendix Table 3].
Figure 3.
5-year age-standardised net survival for localised-stage and advanced-stage ovarian tumours by country, 2004-2009
ˠ Estimate not age-standardised.
ˢ Data for 2001-2003 and 2004-2009 have been merged.
95% CI represented by error bars.
For advanced-stage ovarian cancer, survival was generally around 30% [Figure 3]. Age-standardised survival from advanced-stage disease diagnosed during 2004 to 2009 was highest in Tochigi, Japan (39.3%, 22.1-56.5%), while the lowest survival was in Manitoba, Canada (15.4%, 9.0-21.7%). The between-registry variation in survival for advanced-stage disease was not as wide as that of localised disease [appendix Table 3].
Survival from tumours of unknown stage at diagnosis was similar to or lower than that of advanced disease in most registries in Central and South America and North America during 2005-2009. For a few registries, survival from tumours of unknown stage was higher than that for advanced disease. In North America, survival from tumours of unknown stage at diagnosis was 43.7% (95% CI: 39.2-48.2) in Texas but only 31.3% (95% CI: 29.6-33.0%) for advanced-stage tumours. In Florida and Mississippi, survival for tumours of unknown stage was higher than that of advanced-stage disease. In contrast to other regions, age-standardised survival from tumours of unknown stage was higher than for advanced stage disease in all Asian, European and Oceanic registries [appendix Table 3].
Discussion
There are few international comparisons of survival for the various histological groups of ovarian cancer. The results from this large study show the importance of histology in comparisons of survival from ovarian cancer between countries.
The distribution of histological groups may explain some of the wide international variation in survival. In Asia, for example, type I epithelial tumours are more common than in other regions, is in part due to a higher percentage of clear cell tumours. Because survival for type I epithelial tumours is generally higher than that of type II epithelial tumours, we would expect survival for all histological groups combined to be higher in Asian countries with this larger proportion of more favourable tumours. As shown in the results, survival for all histological groups combined was generally higher in Asian countries than other regions. It is therefore important to examine survival from ovarian cancer for each histological group separately, at least in international comparisons, because survival for all histological groups combined may be influenced by a higher proportion of tumours with a more favourable outcome.
The results also confirm that survival is higher for type I epithelial, germ cell and sex cord-stromal tumours than for the more aggressive type II epithelial tumours. Survival from tumours with a non-specific morphology is also much lower than for tumours in any of these specific histological groups. We would expect survival from tumours of non-specific morphology to be even lower than that of type II tumours, because most women diagnosed with ovarian cancer for whom a specific morphology is not recorded are likely to have been too sick to undergo surgery, which is required for pathological examination and morphological classification of the tumour. However, tumours recorded as unknown morphology or non-specific morphology, may be recorded as such due to lack of or incomplete pathological information reported to registries.
Survival for localised tumours was much higher than for either advanced tumours or tumours of unknown stage. Early diagnosis of ovarian cancer is thus pathologically important. The result for tumours of unknown stage is not surprising, because accurate staging can only be achieved if a woman has undergone surgery. Women with significantly advanced disease are less likely to have surgery and are therefore less likely to be staged appropriately at diagnosis. Furthermore, women with higher comorbidity, some of whom will also have advanced-stage disease, may not be healthy enough for surgery and may also not have their tumours staged appropriately.
In some countries, however, survival from tumours of unknown stage was higher than that for advanced-stage tumours. In these countries, it seems more likely that unknown stage at diagnosis may be due to lack of reporting stage to registries or incomplete staging at diagnosis.
Some cancer registries do not routinely collect data on tumour grade, and no information on grade was available for this study. Therefore, some serous tumours may have been misclassified, because grade is required to classify these tumours appropriately. Only high-grade serous tumours are considered as type II epithelial, but we included all serous tumours in our definition of type II epithelial, because grade was not available. We feel confident that the effect on survival is small, because only a small proportion (5%) of serous tumours are of low grade (14).
We have classified all endometrioid tumours as type I epithelial, despite this subtype being previously sub-divided into type I and type II epithelial tumours (4). If grade had been available, only low-grade endometrioid tumours would have been classified as type I epithelial while high-grade endometrioid tumours should have been classified as type II epithelial based on previous definitions of type I and type II epithelial tumours (4). As with low-grade serous tumours, however, high-grade endometrioid tumours are rare, so the inclusion of these tumours in the type I epithelial group should not greatly affect the survival estimate by histological group (14). An update in 2016 to the classification of endometrioid tumours into type I and type II epithelial tumours now classifies all endometrioid tumours as type I regardless, of tumour grade (15). A sensitivity analysis was conducted to determine how the survival estimates varied between the two possible classifications for endometrioid tumours. Survival for both type I and type II epithelial increased when endometrioid tumours were included in each group separately. Because survival from endometrioid tumours was generally high when examined separately, we feel confident that including these tumours with the less-aggressive type I epithelial subtypes is preferable.
Tumour stage is not routinely collected by cancer all registries; therefore, the analysis by stage at diagnosis could only include data from 25 countries. Additionally, changes in coding of stage at diagnosis in the US (72.7% of women included in the analysis) from the Summary Staging Guide 1977 to SEER Summary Stage 2000 meant that only data from 2001 forward could be included from the US.
The quality and comparability of morphology data between countries may be limited due to differences in diagnostic techniques, morphological classification and transfer of data to the cancer registry. Almost all tumours submitted by Sweden were type II epithelial, the majority of which were unspecific epithelial carcinomas. Given that previous studies show a wider distribution of histological subtypes (16), it is unlikely that almost all tumours from Sweden included in our analysis would have been true type II epithelial tumours. Additionally, Hong Kong only submitted epithelial ovarian cancers when submitting data for the CONCORD-2 study. Therefore, the survival comparison is limited to type I and type II epithelial tumours for Hong Kong.
Our analysis was limited to tumours that had been reported by the registry as morphologically verified, though we also included tumours with specific ICD-O-3 morphology codes regardless of the reported basis of diagnosis. Morphological verification requires a tumour biopsy, thus, may not be performed if the woman presents with advanced-stage disease and is older or has a high number of comorbidities. Additionally, morphological verification may be difficult in low resource settings, where survival may be lower. Therefore, limiting our analysis to morphologically verified tumours may overestimate survival. However, given that 92.7% of tumours were morphologically verified, the bias would be small.
Data on treatment are not routinely collected by all cancer registries, and the registries included in the CONCORD programme were not asked to submit data on treatment. Therefore, we were unable to evaluate the impact of treatment, or lack thereof, on survival estimates for each histological group or stage at diagnosis.
The method of follow-up for obtaining the vital status of registered patients varied between cancer registries. Around 60% of registries reported using only passive follow-up, 2% reported only using active follow-up and 38% reported using both methods. The majority of patients were followed until death or at least five years after diagnosis. The data for this analysis come from the main CONCORD-2 data (n=779,302), in which only 0.6% of women were lost to follow-up and only 0.6% were censored, or diagnosed from 1995-2004 and a vital status of “alive”, but with less than five years of follow-up (1).
This is the largest international population-based study of survival for ovarian cancer by histological group and stage at diagnosis. The large number of women included allowed for comparison of survival from epithelial and non-epithelial tumours, which are usually studied separately, complicating comparisons of survival between populations or over time. The differences in survival between the histological groups emphasise the need to focus future international comparisons of ovarian cancer survival on the various subtypes, rather than analysing ovarian cancer as a single homogenous group. The results from this analysis also emphasise the need for further development of high-quality population-based cancer registries in low-income countries, and the continued improvement of the quality and completeness of cancer registry data in all countries.
Supplementary Material
Acknowledgements
We would like to thank Mr. John Butler for proposing the idea for the manuscript and Dr Martin Gore for helpful advice on classification of ovarian tumours. This work was funded by the Canadian Partnership Against Cancer, Cancer Focus Northern Ireland, Cancer Institute New South Wales, Cancer Research UK (C1336/ A16148), US Centers for Disease Control and Prevention (CDC; 12FED03123, ACO12036), Swiss Re, Swiss Research foundation, Swiss Cancer League, and the University of Kentucky (3049024672-12-568). Salmerón's work was supported by the Séneca Foundation Programme "Jiménez de la Espada".
*.
CONCORD Working Group
Africa—Algeria: S Bouzbid (Registre du Cancer d'Annaba); M Hamdi-Chérif*, Z Zaidi (Registre du Cancer de Sétif); Gambia: E Bah, R Swaminathan (National Cancer Registry); Lesotho: SH Nortje, DC Stefan (Children’s Haematology Oncology Clinics - Lesotho); Libya: MM El Mistiri (Benghazi Cancer Registry); Mali: S Bayo, B Malle (Kankou Moussa University); Mauritius: SS Manraj, R Sewpaul-Sungkur (Mauritius Cancer Registry); Nigeria: A Fabowale, OJ Ogunbiyi* (Ibadan Cancer Registry); South Africa: D Bradshaw, NIM Somdyala (Eastern Cape Province Cancer Registry); Sudan: M Abdel-Rahman (University of Khartoum); Tunisia: L Jaidane, M Mokni (Registre du Cancer du Centre Tunisien).
America (Central and South)—Argentina: I Kumcher, F Moreno (National Childhood Cancer Registry – National Cancer Institute); MS González, EA Laura (Registro Regional de Tumores del Sur de la Provincia de Buenos Aires); SB Espinola, GH Calabrano (Registro Poblacional de Tumores de la Provincia del Chubut); B Carballo Quintero, R Fita (Registro Provincial de Tumores de Córdoba); DA Garcilazo, PL Giacciani (Entre Rios Cancer Registry); MC Diumenjo, WD Laspada (Registro Provincial de Tumores de Mendoza); MA Green, MF Lanza (Registro de Cáncer de Santa Fe); SG Ibañez (Cancer Registry of Tierra del Fuego Province); Brazil: CA Lima, E Lobo de Oliveira (Registro de Câncer de Base Populacional de Aracaju); C Daniel, C Scandiuzzi (Cancer Registry of Distrito Federal); PCF De Souza, CD Melo (Registro de Câncer de Base Populacional de Cuiabá); K Del Pino, C Laporte (Registro de Curitiba); MP Curado, JC de Oliveira (Registro de Goiânia); CLA Veneziano, DB Veneziano (Registro de Câncer de Base Populacional de Jahu); TS Alexandre, AS Verdugo (Registro de Câncer de São Paulo); G Azevedo e Silva* (University of Rio de Janeiro); Chile: JC Galaz, JA Moya (Registro Poblacional de Cáncer Region de Antofagasta); DA Herrmann, S Vargas (Registro Poblacional Region de Los Rios); Colombia: VM Herrera, CJ Uribe (Registro Poblacional de Cáncer Area Metropolitana de Bucaramanga); LE Bravo (Cali Cancer Registry); NE Arias-Ortiz (Registro Poblacional de Cáncer de Manizales); DM Jurado, MC Yépez (Registro Poblacional de Cáncer del Municipio de Pasto); Cuba: YH Galán, P Torres (Registro Nacional de Cáncer de Cuba); Ecuador: F Martínez-Reyes, ML Pérez-Meza (Cuenca Tumor Registry); L Jaramillo, R Quinto (Guayaquil Cancer Registry); P Cueva, JG Yépez (Quito Cancer Registry); Puerto Rico: CR Torres-Cintrón, G Tortolero-Luna (Puerto Rico Central Cancer Registry); Uruguay: R Alonso, E Barrios (Registro Nacional de Cáncer).
America (North)—Canada: C Nikiforuk, L Shack (Alberta Cancer Registry); AJ Coldman, RR Woods (British Columbia Cancer Registry); G Noonan, D Turner* (Manitoba Cancer Registry); E Kumar, B Zhang (New Brunswick Provincial Cancer Registry); FR McCrate, S Ryan (Newfoundland and Labrador Cancer Registry); H Hannah (Northwest Territories Cancer Registry); RAD Dewar, M MacIntyre (Nova Scotia Surveillance and Epidemiology Unit); A Lalany, M Ruta (Nunavut Department of Health and Social Services); L Marrett, DE Nishri* (Ontario Cancer Registry); C McClure, KA Vriends (Prince Edward Island Cancer Registry); C Bertrand, R Louchini (Registre Québécois du Cancer); KI Robb, H Stuart-Panko (Saskatchewan Cancer Registry); S Demers, S Wright (Yukon Government); USA: JT George, X Shen (Alabama Statewide Cancer Registry); JT Brockhouse, DK O'Brien (Alaska Cancer Registry); KC Ward (Georgia Comprehensive Cancer Registry; Metropolitan Atlanta Registry); L Almon (Metropolitan Atlanta Registry); J Bates (California State Cancer Registry); R Rycroft (Colorado Central Cancer Registry); L Mueller, C Phillips (Connecticut Tumor Registry); H Brown, B Cromartie (Delaware Cancer Registry); AG Schwartz, F Vigneau (Metropolitan Detroit Cancer Surveillance System); JA MacKinnon, B Wohler (Florida Cancer Data System); AR Bayakly (Georgia Comprehensive Cancer Registry); CA Clarke, SL Glaser (Greater Bay Area Cancer Registry); D West (Cancer Registry of Greater California); MD Green, BY Hernandez (Hawaii Tumor Registry); CJ Johnson, D Jozwik (Cancer Data Registry of Idaho); ME Charlton, CF Lynch (State Health Registry of Iowa); B Huang, TC Tucker* (Kentucky Cancer Registry); D Deapen, L Liu (Los Angeles Cancer Surveillance Program); MC Hsieh, XC Wu (Louisiana Tumor Registry); K Stern (Maryland Cancer Registry); ST Gershman, RC Knowlton (Massachusetts Cancer Registry); J Alverson, GE Copeland (Michigan State Cancer Surveillance Program); DB Rogers (Mississippi Cancer Registry); D Lemons, LL Williamson (Montana Central Tumor Registry); M Hood (Nebraska Cancer Registry); GM Hosain, JR Rees (New Hampshire State Cancer Registry); KS Pawlish, A Stroup (New Jersey State Cancer Registry); C Key, C Wiggins (New Mexico Tumor Registry); AR Kahn, MJ Schymura (New York State Cancer Registry); G Leung, C Rao (North Carolina Central Cancer Registry); L Giljahn, B Warther (Ohio Cancer Incidence Surveillance System); A Pate (Oklahoma Central Cancer Registry); M Patil, SS Schubert (Oregon State Cancer Registry); JJ Rubertone, SJ Slack (Pennsylvania Cancer Registry); JP Fulton, DL Rousseau (Rhode Island Cancer Registry); TA Janes, SM Schwartz (Seattle Cancer Surveillance System); SW Bolick, DM Hurley (South Carolina Central Cancer Registry); J Richards, MA Whiteside (Tennessee Cancer Registry); LM Nogueira (Texas Cancer Registry); K Herget, C Sweeney (Utah Cancer Registry); J Martin, S Wang (Virginia Cancer Registry); DG Harrelson, MB Keitheri Cheteri (Washington State Cancer Registry); S Farley, AG Hudson (West Virginia Cancer Registry); R Borchers, L Stephenson (Wisconsin Department of Health Services); JR Espinoza (Wyoming Cancer Surveillance Program); HK Weir* (Centers for Disease Control and Prevention); BK Edwards* (National Cancer Institute).
Asia—China: N Wang, L Yang (Beijing Cancer Registry); JS Chen (Changle City Cancer Registry); GH Song (Cixian Cancer Registry); XP Gu (Dafeng County Center for Disease Control and Prevention); P Zhang (Dalian Centers for Disease Prevention and Control); HM Ge (Donghai County Center for Disease Prevention and Control); DL Zhao (Feicheng County); JH Zhang (Ganyu Center for Disease Prevention and Control); FD Zhu (Guanyun Cancer Registry); JG Tang (Haimen Cancer Registry); Y Shen (Haining City Cancer Registry); J Wang (Jianhu Cancer Registry); QL Li (Jiashan County Cancer Registry); XP Yang (Jintan Cancer Registry); J Dong, W Li (Lianyungang Center for Disease Prevention and Control); LP Cheng (Henan Province Central Cancer Registry); JG Chen (Qidong County Cancer Registry); QH Huang (Sihui Cancer Registry); SQ Huang (Taixing Cancer Registry); GP Guo (Cancer Institute of Yangzhong City); K Wei (Zhongshan City Cancer Registry); WQ Chen*, H Zeng (National Central Cancer Registry China); Cyprus: AV Demetriou, P Pavlou (Cyprus Cancer Registry); Hong Kong: WK Mang, KC Ngan (Hong Kong Cancer Registry); India: R Swaminathan (Chennai Cancer Registry); AC Kataki, M Krishnatreya (Guwahati Cancer Registry); PA Jayalekshmi, P Sebastian (Karunagappally Cancer Registry); SD Sapkota, Y Verma (Population Based Cancer Registry, Sikkim); A Nandakumar* (National Centre for Disease Informatics and Research; National Cancer Registry Programme); Indonesia: E Suzanna (Jakarta Cancer Registry); Israel: L Keinan-Boker, BG Silverman (Israel National Cancer Registry); Japan: H Ito, H Nakagawa (Aichi Cancer Registry); M Hattori, Y Kaizaki (Fukui Cancer Registry); H Sugiyama, M Utada (Hiroshima Prefecture Cancer Registry); K Katayama, H Narimatsu (Kanagawa Cancer Registry); S Kanemura (Miyagi Prefectural Cancer Registry); T Koike (Niigata Prefecture Cancer Registry); I Miyashiro (Osaka Cancer Registry); M Yoshii (Saga Prefectural Cancer Registry); I Oki (Tochigi Prefectural Cancer Registry); A Shibata (Yamagata Cancer Registry); T Matsuda* (National Cancer Center); Jordan: O Nimri (Jordan National Cancer Registry); Malaysia: A Ab Manan, N Bhoo Pathy (Penang Cancer Registry); Mongolia: O Chimedsuren, S Tuvshingerel (Cancer Registry of Mongolia); Qatar: AHM Al Khater, MM El Mistiri (Qatar Cancer Registry); Saudi Arabia: H Al-Eid (Saudi National Cancer Registry); South Korea: KW Jung, YJ Won (Korea Central Cancer Registry); Taiwan: CJ Chiang, MS Lai (Taiwan Cancer Registry); Thailand: K Suwanrungruang, S Wiangnon (Khon Kaen Provincial Registry); K Daoprasert, D Pongnikorn (Lampang Cancer Registry); SL Geater, H Sriplung (Songkhla Cancer Registry); Turkey: S Eser, CI Yakut (Izmir Cancer Registry).
Europe—Austria: M Hackl (Austrian National Cancer Registry); H Mühlböck, W Oberaigner (Tyrol Cancer Registry); Belarus: AA Zborovskaya (Belarus Childhood Cancer Subregistry); OV Aleinikova (Belarusian Research Center for Pediatric Oncology, Hematology and Immunology); Belgium: K Henau, L Van Eycken (Belgian Cancer Registry); Bulgaria: N Dimitrova, Z Valerianova (Bulgarian National Cancer Registry); Croatia: M Šekerija (Croatian National Cancer Registry); Czech Republic: M Zvolský (Czech National Cancer Registry); Denmark: G Engholm, H Storm* (Danish Cancer Society); Estonia: K Innos, M Mägi (Estonian Cancer Registry); Finland: N Malila, K Seppä (Cancer Society of Finland); France: J Jégu, M Velten (Bas-Rhin General Cancer Registry); E Cornet, X Troussard (Registre Régional des Hémopathies Malignes de Basse Normandie); AM Bouvier, J Faivre (Burgundy Digestive Cancer Registry); AV Guizard (Calvados General Cancer Registry); V Bouvier, G Launoy (Calvados Digestive Cancer Registry); P Arveux (Côte-d'Or Gynaecologic Cancer Registry); M Maynadié, M Mounier (Côte-d'Or Haematopoietic Malignancies Registry); E Fournier, AS Woronoff (Doubs and Belfort Territory General Cancer Registry); M Daoulas (Finistère Cancer Registry); J Clavel (National Registry of Childhood Haematopoietic Malignancies); S Le Guyader-Peyrou, A Monnereau (Gironde Haematopoietic Malignancies Registry); B Trétarre (Hérault General Cancer Registry); M Colonna (Isère General Cancer Registry); A Cowppli-Bony, F Molinié (Loire-Atlantique-Vendée Cancer Registry); S Bara, D Degré (Manche General Cancer Registry); O Ganry, B Lapôtre-Ledoux (Somme General Cancer Registry); P Grosclaude (Tarn General Cancer Registry); J Estève (Hospices Civils de Lyon); F Bray*, M Piñeros* (International Agency for Research on Cancer); F Sassi (Organisation for Economic Co-operation and Development); Germany: R Stabenow (Common Cancer Registry of the Federal States); A Eberle (Bremen Cancer Registry); C Erb, A Nennecke (Hamburg Cancer Registry); J Kieschke, E Sirri (Epidemiological Cancer Registry of Lower Saxony); H Kajueter (North Rhine Westphalia Cancer Registry); K Emrich, SR Zeissig (Rhineland Palatinate Cancer Registry); B Holleczek (Saarland Cancer Registry); N Eisemann, A Katalinic (Schleswig-Holstein Cancer Registry); H Brenner (German Cancer Research Center); Gibraltar: RA Asquez, V Kumar (Gibraltar Cancer Registry); Iceland: EJ Ólafsdóttir, L Tryggvadóttir (Icelandic Cancer Registry); Ireland: H Comber, PM Walsh (National Cancer Registry); H Sundseth* (European Institute of Women’s Health); Italy: E Devigili, G Mazzoleni (Registro Tumori Alto Adige); A Giacomin (Registro Tumori Biella); F Bella, M Castaing (Integrated Cancer Registry of Catania-Messina-Siracusa-Enna); A Sutera (Registro Tumori Catanzaro); G Gola (Registro Tumori della Provincia di Como); S Ferretti (Registro Tumori della Provincia di Ferrara); D Serraino, A Zucchetto (Registro Tumori del Friuli Venezia Giulia); R Lillini, M Vercelli (Registro Tumori Regione Liguria); S Busco, F Pannozzo (Registro Tumori della Provincia di Latina); S Vitarelli (Registro Tumori della Provincia di Macerata); P Ricci (Registro Tumori Mantova); C Pascucci (Registro Tumori Marche Childhood); M Autelitano (Registro Tumori Milano); C Cirilli, M Federico (Registro Tumori della Provincia di Modena); M Fusco, MF Vitale (Registro Tumori della ASL Napoli 3 sud); M Usala (Nuoro Cancer Registry); R Cusimano, W Mazzucco (Registro Tumori di Palermo e Provincia); M Michiara, P Sgargi (Registro Tumori della Provincia di Parma); MM Maule, C Sacerdote (Piedmont Childhood Cancer Registry); R Tumino (Registro Tumori della Provincia di Ragusa); E Di Felice, M Vicentini (Registro Tumori Reggio Emilia); F Falcini (Registro Tumori della Romagna); L Cremone (Registro Tumori Salerno); M Budroni, R Cesaraccio (Registro Tumori della Provincia di Sassari); ML Contrino, F Tisano (Registro Tumori Siracusa); AC Fanetti, S Maspero (Registro Tumori della Provincia di Sondrio); G Candela, T Scuderi (Registro Tumori Trapani); MA Gentilini, S Piffer (Registro Tumori Trento); S Rosso, L Sacchetto (Registro Tumori Piemonte Città di Torino); A Caldarella (Registro Tumori della Regione Toscana); F La Rosa, F Stracci (Registro Tumori Umbro di Popolazione); P Contiero, G Tagliabue (Registro Tumori Lombardia, Provincia di Varese); AP Dei Tos, M Zorzi (Registro Tumori Veneto); R Zanetti* (International Association of Cancer Registries); P Baili, F Berrino*, G Gatta, M Sant* (National Cancer Institute); R Capocaccia*, R De Angelis (National Centre for Epidemiology); Latvia: E Liepina, A Maurina (Latvian Cancer Registry); Lithuania: G Smailyte (Lithuanian Cancer Registry); Malta: D Agius, N Calleja (Malta National Cancer Registry); Netherlands: S Siesling, O Visser (Comprehensive Cancer Centre of the Netherlands); Norway: S Larønningen, B Møller (The Cancer Registry of Norway); Poland: A Dyzmann-Sroka, M Trojanowski (Greater Poland Cancer Registry); S Góźdż, R Mężyk (Cancer Registry of Kielce); M Grądalska-Lampart, AU Radziszewska (Podkarpackie Cancer Registry); JA Didkowska, U Wojciechowska (National Cancer Registry); J Błaszczyk, K Kępska (Lower Silesian Cancer Registry); M Bielska-Lasota, K Kwiatkowska (National Institute of Public Health - NIH); Portugal: G Forjaz, RA Rego (Registo Oncológico Regional dos Açores); J Bastos, MA Silva (Registo Oncológico Regional do Centro); L Antunes, MJ Bento (Registo Oncológico Regional do Norte); A Mayer-da-Silva, A Miranda (Registo Oncólogico Regional do Sul); Romania: D Coza, AI Todescu (Cancer Institute I. Chiricuta); Russian Federation: MY Valkov (Arkhangelsk Regional Cancer Registry); Slovakia: J Adamcik, C Safaei Diba (National Cancer Registry of Slovakia); Slovenia: M Primic-Žakelj, T Žagar (Cancer Registry of Republic of Slovenia); J Stare (University of Ljubljana); Spain: E Almar, A Mateos (Registro de Cáncer de Albacete); JR Quirós (Registro de Tumores del Principado de Asturias); J Bidaurrazaga, N Larrañaga (Basque Country Cancer Registry); JM Díaz García, AI Marcos (Registro de Cáncer de Cuenca); R Marcos-Gragera, ML Vilardell Gil (Registre de Càncer de Girona); E Molina, MJ Sánchez (Registro de Cáncer de Granada); P Franch Sureda, M Ramos Montserrat (Mallorca Cancer Registry); MD Chirlaque, C Navarro (Murcia Cancer Registry); EE Ardanaz, CC Moreno-Iribas (Registro de Cáncer de Navarra); R Fernández-Delgado, R Peris-Bonet (Registro Español de Tumores Infantiles (RETI-SEHOP)); J Galceran (Tarragona Cancer Registry); Sweden: S Khan, M Lambe (Swedish Cancer Registry); Switzerland: B Camey (Registre Fribourgeois des Tumeurs); C Bouchardy, M Usel (Geneva Cancer Registry); SM Ess (Cancer Registry Grisons and Glarus); C Herrmann (Cancer Registry Grisons and Glarus; Cancer Registry of St Gallen-Appenzell); JL Bulliard, M Maspoli-Conconi (Registre Neuchâtelois des Tumeurs); H Frick (Cancer Registry of St Gallen-Appenzell); CE Kuehni, M Schindler (Swiss Childhood Cancer Registry); A Bordoni, A Spitale (Registro Tumori Cantone Ticino); A Chiolero, I Konzelmann (Registre Valaisan des Tumeurs); SI Dehler, KL Matthes (Krebsregister der Kantone Zürich und Zug); United Kingdom: J Rashbass, C Stiller* (Public Health England); D Fitzpatrick, A Gavin (Northern Ireland Cancer Registry); F Bannon (Queens University, Belfast); RJ Black, DH Brewster (Scottish Cancer Registry); DW Huws, C White (Welsh Cancer Intelligence & Surveillance Unit); P Finan (Leeds General Infirmary); C Allemani*, A Bonaventure, H Carreira, MP Coleman*, V Di Carlo, R Harewood, K Liu, M Matz, L Montel, M Nikšić, B Rachet*, N Sanz, D Spika (London School of Hygiene & Tropical Medicine); R Stephens* (National Cancer Research Institute, London); M Peake (University of Leicester).
Oceania—Australia: E Chalker, L Newman (Australian Capital Territory Cancer Registry); D Baker, MJ Soeberg (NSW Cancer Registry); J Aitken, C Scott (Queensland Cancer Registry); BC Stokes, A Venn (Tasmanian Cancer Registry); H Farrugia, GG Giles (Victorian Cancer Registry); T Threlfall (Western Australian Cancer Registry); D Currow*, H You (Cancer Institute NSW); New Zealand: J Hendrix, C Lewis (New Zealand Cancer Registry).
*CONCORD Steering Committee
Footnotes
Conflict of Interest
The authors declare there are no conflicts of interest.
References
- 1.Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385(9972):977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maringe C, Walters S, Butler J, Coleman MP, Hacker N, Hanna L, et al. Stage at diagnosis and ovarian cancer survival: evidence from the International Cancer Benchmarking Partnership. Gynecologic Oncology. 2012;127(1):75–82. doi: 10.1016/j.ygyno.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 3.De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE--5-a population-based study. Lancet Oncol. 2014;15(1):23–34. doi: 10.1016/S1470-2045(13)70546-1. [DOI] [PubMed] [Google Scholar]
- 4.Kurman RJ, Shih Ie M. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34(3):433–43. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurman RJ, Shih Ie M. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer--shifting the paradigm. Hum Pathol. 2011;42(7):918–31. doi: 10.1016/j.humpath.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCluggage WG. My approach to and thoughts on the typing of ovarian carcinomas. J Clin Pathol. 2008;61(2):152–63. doi: 10.1136/jcp.2007.049478. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee S, Kaye SB. New strategies in the treatment of ovarian cancer: current clinical perspectives and future potential. Clin Cancer Res. 2013;19(5):961–8. doi: 10.1158/1078-0432.CCR-12-2243. [DOI] [PubMed] [Google Scholar]
- 8.Fritz AG, Percy C, Jack A, Shanmugaratnam K, Sobin LH, Parkin DM, et al., editors. International Classification of Diseases for Oncology (ICD-O) 3rd ed. Geneva: World Health Organization; 2000. [Google Scholar]
- 9.Trent Cancer Registry: National Cancer Intelligence Network. Overview of Ovarian Cancer in England: Incidence, Mortality and Survival. London: National Cancer Intelligence Network; 2012. [Google Scholar]
- 10.Pohar Perme M, Henderson R, Stare J. An approach to estimation in relative survival regression. Biostatistics. 2009;10:136–46. doi: 10.1093/biostatistics/kxn021. [DOI] [PubMed] [Google Scholar]
- 11.Clerc-Urmès I, Grzebyk M, Hédelin G. Net survival estimation with stns. Stata Journal. 2014;14:87–102. [Google Scholar]
- 12.StataCorp. STATA statistical software. 14 ed. College Station TX: Stata Corporation; 2015. [Google Scholar]
- 13.Corazziari I, Quinn MJ, Capocaccia R. Standard cancer patient population for age standardising survival ratios. European Journal of Cancer. 2004;40:2307–16. doi: 10.1016/j.ejca.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Kurman RJ, Carcangiu ML, Herrington CS, Young RH, editors. WHO Classification of Tumours of Female Reproductive Organs. 4th ed. Geneva: WHO; 2014. [Google Scholar]
- 15.Kurman RJ, Shih Ie M. The Dualistic Model of Ovarian Carcinogenesis: Revisited, Revised, and Expanded. Am J Pathol. 2016;186(4):733–47. doi: 10.1016/j.ajpath.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oberaigner W, Minicozzi P, Bielska-Lasota M, Allemani C, de Angelis R, Mangone L, et al. Survival for ovarian cancer in Europe: the across-country variation did not shrink in the past decade. Acta Oncol. 2012;51(4):441–53. doi: 10.3109/0284186X.2011.653437. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.