Abstract
Research progress in diseases of the exocrine pancreas (chronic pancreatitis, pancreatogenic diabetes mellitus and pancreatic cancer) has been hampered by the disorders’ heterogeneity, the limitations of previous small cross-sectional studies, the inability to safely obtain pancreatic tissue for study, and the lack of structured epidemiology tools, genetic testing, and biomarker development. Mechanism-based research of these diseases has suffered from the lack of systematically collected clinical measures in longitudinal cohort studies linked with biospecimens. Given the increasing incidence and prevalence of chronic pancreatitis and its association to the development of pancreatic cancer, its complications, high mortality rate, and associated health care cost, National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Cancer Institute funded the Consortium for the study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer (CPDPC) to identify research gaps and foster multidisciplinary collaborations to better diagnose, characterize and manage CP and its sequelae. The CPDPC structure, governance and research objectives is described in this article. Studies undertaken by the CPDPC are described in other articles in this journal’s issue.
Keywords: chronic pancreatitis; pancreatic cancer; New Onset Diabetes (NOD); Consortium for the study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer; PROCEED Study; INSPPIRE
INTRODUCTION
The spectrum of pancreatic diseases, including recurrent and chronic pancreatitis, pancreatic adenocarcinoma ancreatic cancer) and diabetes associated with these pancreatic diseases, referred to as Type 3c diabetes mellitus, represent some of the most challenging medical disorders of our time. Based on input from patient advocacy groups, oncological and gastroenterological professional societies and from Advisory Councils to the National Cancer Institute (NCI) and the National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK), a Consortium for the study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer (CPDPC) was established by NCI and NIDDK as a unique multidisciplinary research program designed to accelerate progress in these complex disorders.
WHAT LED TO CREATION OF CPDPC?
The key impetus behind creation of the CPDPC is the lack of effective therapy for these diseases. Pancreatic cancer has an extremely high fatality rate and is the third leading cause of cancer death in the US with some estimates that it will become the second leading cause of cancer death by the year 2020.1,2 The incidence of pancreatic cancer in the US has been increasing for more than a decade, in parallel with the rates of pancreatitis, and both are likely driven by the epidemic of obesity and diabetes mellitus.3 Chronic pancreatitis (CP), which may result from repeated episodes of acute pancreatitis (recurrent acute pancreatitis [ARP]), is the strongest identified risk factor for pancreatic cancer and increases the risk at least 13.3 fold.4 Pancreatitis and pancreatic cancer often exist in a disease continuum. Patients with an episode of acute pancreatitis have a 20–30% likelihood of one or more recurrent episodes, with progression to chronic pancreatitis in ~10% of the recurrent cases.3,5,6 Glucose intolerance and pancreatogenic diabetes (referred to as Type 3c diabetes) are observed in up to 80% of individuals during the course of this continuum.7 Importantly, the risk for pancreatic cancer in patients with both pancreatitis and Type 3c diabetes is increased 33 fold.6
No medical therapy (except abstinence from alcohol and tobacco) has been found to alter the course of the disease, and early diagnosis of both chronic pancreatitis and pancreatic cancer is problematic due to the absence of biomarkers of early disease. Therefore, it is imperative to develop tools for effectively managing patients with these diseases and to design interventions that can decrease the incidence of these diseases in vulnerable populations to address a currently unmet major public health problem. Preventing both pancreatitis progression and diabetes are critical goals, as is early identification of pancreatic cancer in a treatable stage.
The conceptual origin of the CPDPC represents the combined efforts of NIDDK and NCI, patient-based non-profit and professional organizations and many dedicated clinicians and scientists. A NIDDK sponsored workshop was held in June 2012 where lead scientists reviewed the state of the art and identified areas of research gaps in pancreatitis. These experts stressed the need for further basic and translational studies in chronic pancreatitis to identify strategies and therapeutic targets to reduce the burden of disease.8 Another workshop, co-sponsored by NCI and NIDDK, was held in June 2013 and highlighted the risk factors which link chronic pancreatitis, diabetes, and pancreatic cancer. Several themes emerged from the workshop. First, the complex relationship between pancreatitis, diabetes and PDAC. Second that CP can cause diabetes by destruction of the islets (Type 3c) and third that the risks of T3cDM and CP are additive in hereditary pancreatitis, but the specific PDAC risk of T3cDM in epidemiology studies is not known because it has not been specifically measured. It was proposed that pursuing these themes is best achieved by large consortium studies.6
The Recalcitrant Cancer Research Act of 2012 (Public Law 112–239, §1083)9 called upon the NCI to “develop scientific frameworks” to assist in making “progress against recalcitrant or deadly cancers.” Pancreatic ductal adenocarcinoma is a recalcitrant cancer as defined by its five-year relative survival rate of less than 5 percent. The limited early diagnostic or therapeutic approaches for patients with pancreatic ductal adenocarcinoma has provided a stimulus for the evaluation of new and missed opportunities that could now be applied to the existing portfolio of pancreatic cancer research to make more substantial progress. In February 2014, NCI published a Scientific Framework for Pancreatic Ductal Adenocarcinoma10 which gave specific recommendations. These were based in part on the recommendations from a panel of extramural scientists convened by NCI in October 2012 and from an interdisciplinary meeting on June 2013 co-sponsored by NCI, NIDDK, and the Pancreatic Cancer Action Network, the NIDDK-NCI Pancreatitis-Diabetes-Pancreatic Cancer Workshop.6 These recommendations included: 1. Determine the relationship between pancreatogenic diabetes (type 3c diabetes) and the development of pancreatic cancer; 2. Understand the relationship between pancreatic cancer and diabetes and chronic pancreatitis and; 3. Evaluate longitudinal screening protocols for patients at high risk of developing pancreatic cancer because of genetic background or the presence of mucinous pancreatic cysts.
To address the recommendations of these workshops and meetings, the NCI and NIDDK published two Request for Applications (RFAs, RFA-DK-14–02711 and RFA-DK-14–02812) for the establishment of a multidisciplinary consortium formed by a Coordination and Data Management Center (CDMC) and multiple clinical centers (CC) of excellence that would collect a cohort of patients and biospecimens suitable for mechanistic studies and pilot trials. These RFAs were designed to fill specific high priority needs not adequately met by any other programs at NIDDK or NCI. The major area of focus was chronic pancreatitis, diabetes, and the factors which increase the risk of pancreatic cancer in patients with chronic pancreatitis or diabetes.
The objectives of the RFAs were to form multi-disciplinary teams composed of members from the CCs and CDMC to undertake a comprehensive clinical, epidemiological, and biological characterization of patients with CP (including adults and children with ARP) to gain insight into the pathophysiology of chronic pancreatitis and its sequela: chronic pain, pancreatic exocrine and endocrine insufficiency, T3cDM and the diabetes/pancreatic cancer association. Another objective was to undertake studies on the development of pancreatic cancer in newly diagnosed diabetic patients.
In addition, a major collaborative effort within the Consortium will be the establishment of an annotated repository of bio-specimens (blood, pancreatic and duodenal juice, stool, saliva and when feasible pancreatic tissue) to allow for the identification and validation of biomarkers for risk stratification and/or early detection.
Through the acquisition of a cohort of well-characterized patients and associated biospecimens, the proposed clinical research network will provide the resources and collaborative opportunities necessary for achieving many of the research objectives identified in the strategic plans of the participating institutes.
In response to RFA-DK-14–027 and RFA-DK-14–028, based on Study Section review, NCI and NIDDK program staff evaluations and with the concurrence of both NCI and NIDDK Advisory Councils a Consortium for the study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer (CPDPC) was created with the following investigators (centers in alphabetical order):
Clinical Centers
Baylor College of Medicine, Houston, Texas (Fisher, William E)
Cedars-Sinai Medical Center, Los Angeles, Calif (Pandol, Stephen J; Goodarzi, Mark O.)
Indiana University, Indianapolis, Ind (Fogel, Evan L.)
Kaiser Foundation, Oakland, Calif (Van Den Eeden, Stephen K.)
Mayo Clinic, Rochester, Minn (Chari, Suresh T; Topazian, Mark)
Ohio State University, Columbus, Ohio (Conwell, Darwin L; Hart, Phil A; Steen, Hanno)
Stanford University, Palo Alto, Calif (Park, Walter G.; Habtezion, Aida; Kim, Seung K)
University of Florida, Gainesville, Fla (Forsmark, Christopher E; Cusi, Kenneth; Hughes, Steven J)
University of Iowa, Iowa City, Iowa (Uc, Aliye)*
University of Pittsburgh, Pittsburgh, Penn (Whitcomb, David C; Yadav, Dhiraj)
Coordination and Data Management Center (CDMC):
MD Anderson Cancer Center, Houston, Texas (Feng, Ziding; Maitra, Anirban)
*Pediatric clinical center, serving as point of contact for a network of 18 pediatric centers across the United States, Canada, Australia, and Israel.
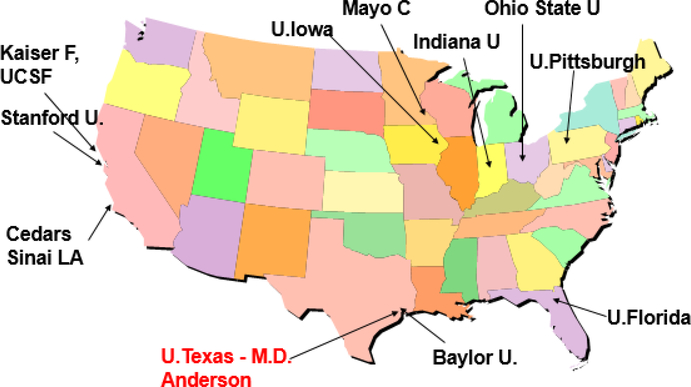
The selected investigators represent the largest accumulation of pancreatic research expertise in the US, working from top academic clinical centers distributed across the US, providing a comprehensive “catchment” area to bring diverse patient population to the studies of the CPDPC (Fig. 1).
FIGURE 1.
Geographical distribution of the CPDPC members.
ORGANIZATION OF THE CPDPC CONSORTIUM
The CPDPC consists of the following entities: the NIDDK and NCI, ten Clinical Centers (CCs), a Coordination and Data Management Center (CDMC), an Executive Committee, a Steering Committee and its subcommittees, a Data and Safety Monitoring Board (DSMB), and other committees as needed.
The NIDDK and NCI, are responsible for organizing and providing support for the CPDPC and are involved substantially with the awardees as a “partner,” consistent with the Cooperative Agreement mechanism. The NIDDK and NCI Project Scientists, provide programmatic oversight, monitor subject recruitment and study progress, ensure disclosure of conflicts of interest and adherence to NIDDK and NCI policies. The NIDDK/NCI appointed Chairperson(s) of the Steering Committee and all members of the DSMB.
All individual CCs are required to participate in a cooperative and interactive manner with one another, with the CDMC, and with the NIDDK and NCI in all aspects of the Consortium (for proposing protocols, participating in their overall development, conducting the research, and disseminating research findings).
The CDMC provides administrative and logistic support for the consortium, including developing and maintaining public and secured consortium website, supporting conference calls and in person meetings, establishing and managing subawards for each CC. The CDMC also provides coordination for each consortium collaborative study, including protocol development and management, study database, study monitoring for regulatory compliance and data quality, data analyses and DSMB reports. The CDMC provides statistical support for all consortium collaborative studies in study design and data interpretation and develops new statistical methodology if necessary to meet study needs.
CPDPC STUDY GOVERNANCE
Steering Committee
The Steering Committee is composed of the Principal Investigator (PI) of each CC, the CDMC, the NCI and NIDDK Project Scientists is the main governing body of the CPDPC and has primary responsibility for the general organization of the Consortium and approval of publications and ancillary studies. The Steering Committee is responsible for the conduct and monitoring of studies and reporting study results. Topics for investigational and treatment protocols are proposed and prioritized by the Steering Committee. Other subcommittees of the Steering Committee are established and operate as necessary, such as publications, ancillary, protocol, bio-specimens and radiology, etc.
Executive Committee
The Executive Committee is comprised of the CPDPC Study Co-Chairs, the PI of the CMDC, the NIDDK/NCI Project Scientists, convenes to effect management decisions required between Steering Committee meetings, as required for the function of the network.
Data and Safety Monitoring Board
An independent Data and Safety Monitoring Board has been established by the NIDDK in consultation with the NCI to review protocols and monitor patient safety and performance of each study. As a part of its responsibilities, the DSMB submits recommendations to the NIDDK/NCI regarding the continuation of each study. The DSMB is responsible for final approval of the Data and Safety Monitoring Plan developed by the CDMC. All protocols or changes to protocols are approved by Institutional Review Boards, the Steering Committee, the CPDPC Data and Safety Monitoring Board, the NIDDK and NCI before initiation.
RESEARCH OBJECTIVES AND PLANS OF THE CPDPC
In pursuing the research objectives of the CPDPC, as outlined in the published RFAs, the investigators organized themselves into 4 working groups around the main research objectives:
Adult Chronic Pancreatitis Working Group (Chairs: D.L. Conwell; D. Yadav)
Pediatric Chronic Pancreatitis Working Group (Chairs: A. Uc; M.E. Lowe)
DM PDAC Working Group (Chairs: S.T. Chari, A. Maitra)
Type3c DM Working Group (Chairs: M. Goodarzi, A. Habtezion)
With significant cross-fertilization across the four working groups, the consortium’s investigators have developed 3 major longitudinal studies, two cross-sectional studies to standardize the diagnosis and to characterize type 3c Diabetes, and multiple ancillary studies.
As the activities of the 4 working groups is described in other articles in this issue of Pancreas, here we provide a list of the main longitudinal studies (A, B, C):
Prospective Evaluation of Chronic Pancreatitis for Epidemiologic and Translational Studies (PROCEED).
Pediatric Longitudinal Cohort Study of Chronic Pancreatitis (The International Study Group of Pediatric Pancreatitis: In Search for a Cure (INSPPIRE 2).
A Prospective Study to Establish a New Onset Diabetes (NOD) Cohort.
In addition to the three longitudinal studies, the consortium will undertake two additional studies to define and characterize pancreatogenic Diabetes (Type 3cDM);
Evaluation of a mixed meal test for Diagnosis and characterization of Pancreatogenic Diabetes secondary to pancreatic cancer and chronic pancreatitis (DETECT).
Detailed Physiologic Characterization of the Insulin Axis in Type 3c Diabetes versus Type 2 Diabetes (DEPICT 3v2).
The Consortium also provides an environment that fosters internal and external collaborations through ancillary studies which in the future will provide new information on the epidemiology, pathogenesis and treatment of chronic pancreatitis and its sequelae, in both in children and adults as well as diabetes and pancreatic cancer.
In conclusion the Consortium for the study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer represents a significant joint effort of the NIDDK and NCI to support a comprehensive research program for clinical, epidemiological, and biological characterization of patients with chronic pancreatitis (including those with acute recurrent pancreatitis), diabetes associated with exocrine pancreatic disease (Type 3c) and pancreatic cancer, and patients with early stage pancreatic cancer to gain insight into the pathophysiology and relationships between these pancreatic diseases; and to develop better methods (and biomarkers) for diagnosis, prevention, monitoring, early detection, and therapy. The results will identify strategies for more effective care and targeted interventions for patients with these challenging conditions.
ACKNOWLEDGMENTS
The authors would like to acknowledge all the members participating in the Consortium for the study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer (CPDPC):
A. Investigators and Coordinators for Adult Pancreas studies (PROCEED, DETECT, NOD studies)
1) Co-investigators, Collaborators:
Baylor College of Medicine: Mohamed O. Othman; Mandeep Bajaj; Carlos A. Farinas; George Van Buren, II; Douglas S. Fishman; Joseph Petrosino; Eric J Silberfein; Barbara W. Trautner
Cedars Sinai Medical Center: Marc T. Goodman; Christie Y. Jeon; Srinivas Gaddam; Maxim S. Petrov; Joseph Pisegna; Sofiya Reicher; Bechien U. Wu; Laith Jamil; Simon K. Lo; Michael Stanley Lewis
Indiana University: Kieren J. Mather; Temel Tirkes; Stuart Sherman; Murray Korc
Kaiser Foundation: Margaret A. Tempero; Suraj Gupta; Kareem Mawad; Craig A. Munroe; Terry L. Jue; Assiamira Ferrara; Scott Oakes; Mark Anderson; Mattias Hebrok; Charles Quesenberry
Mayo Clinic: Yogish Kudva; Naoki Takahashi; Sudhakar Venkatesh; Gloria M. Petersen; Aleksey Matveyenko; Ayush Sharma; Tonya Palermo; Timothy B. Gardner; Yu-Xiao Yang
Ohio State University: Melena D. Bellin; David Bradley; Zobeida Cruz-Monserrate; Amy Hosmer; Luis Lara; Gregory Lesinski; Somashaker Krishna; Thomas Mace; Sean McCarthy: Zarine Shah; Sebastian Strobel; Jon Walker
Stanford University: Zachary M. Sellers; Marina Basina; Bryant Lin; Shreyas Vasanawala.
University of Florida: Joseph R. Grajo; Patricia P. Moser; Amer S. Abouhamze
University of Texas MD Anderson Cancer Center: Liang Li; Ying Yuan
University of Pittsburgh: Adam Slivka; Georgios I. Papachristou; Randall E. Brand; Anil Dasyam; Jennifer Chennat; Kevin McGrath; Gong Tang; Anna E. Phillips; Aatur Singhi.
2) Coordinators and Research Associates:
Baylor College of Medicine: Delrose A. Jones; Amy McElhany; Jose E. Mendez-Reyes; Martha Navarro Cagigas; Linda H. Nguyen
Cedars Sinai Medical Center: Cindy Miao; Phoebe Chang; Yunhee Choi-Kuaea
Indiana University: Sheryl Lynch; Vanessa Patrick; Alicia Winters; Gail McNulty; Suzette Schmidt
Kaiser Foundation: Amethyst D. Leimpeter; Erica H. Kerezsi; Jun Shan; Desiree Goldstein; Keeli McClearnen
Mayo Clinic: Vincent Anani; Natasha Kanwar
Ohio State University: Emily Bowns; Alejandra Cervantes; Brianna Conley; Casey McClurkin
Stanford University: Judith Chuang; Christina Vu; Yujun Yang; Sangbin Park
University of Florida: Amber Bouton; April A. Goddard; Danielle Poulton
University of Texas MD Anderson Cancer Center: Ria Ghosh; Noemy Contreras; Lavinia Padmore; Savitri Appana
University of Pittsburgh: Laura Mathews; Kelley Woods; Kimberly Stello; Nicole Komara; Melissa Saul; Melanie Mays; Phil Greer; Juan Castaneda; Amanda Kirshkaln; Mark Batistick
B. Investigators and Coordinators in Pediatric Pancreas study (INSPPIRE)
1) Co-investigators, Collaborators:
Baylor College of Medicine: Douglas Fishman
Cedars Sinai Medical Center: Quin Liu
Children’s Hospital Los Angeles: Yuhua Zheng
Children’s Hospital of Philadelphia: Asim Maqbool; Maria Mascarenhas
Cincinnati Children’s Hospital: Maisam Abu-El-Haija, Jaimie Nathan, Tom K. Lin
Hadassah University Hospital: Michael Wilschanski
Hospital for Sick Children, Toronto, Canada: Tanja Gonska
Indiana University: Brian McFerron
Massachusetts General Hospital: Uzma Shah
Medical College of Wisconsin; Steven Werlin; Praveen Goday
Montreal Children’s Hospital: Veronique D. Morinville
Nationwide Children’s Hospital: Cheryl Gariepy
Primary Children’s Hospital: John Pohl
Seattle Children’s Hospital: Matthew Giefer
Stanford University: Zachary M. Sellers
Sydney Children’s Hospital: Chee Y. Ooi
University of California, San Francisco: Mel Heyman; Emily Perito
University of Minnesota: Sarah Jane Schwarzenberg; Melena D. Bellin
University of Pittsburgh: Sohail Husain; Kate Ellery
University of Texas Southwestern Medical Center: David M. Troendle; Bradley Barth
Washington University: Mark E. Lowe
2) Coordinators and Research Associates:
Children’s Hospital Los Angeles: Roy Leong
Children’s Hospital of Philadelphia: Lucia Sanchez
Cincinnati Children’s Hospital: Tyler Thompson
Hadassah University Hospital: Batya Vertsman; Geulah Cramel-Fink
Massachusetts General Hospital: Ana Fernandes; Francine Molay
Medical College of Wisconsin; Adriane Mueller; Sydnee Rausch
Montreal Children’s Hospital: Veronique D. Morinville
Nationwide Children’s Hospital: Ling Fan; Mohammad Ovais
Primary Children’s Hospital: Cameron Tear; Cynthia Jones; Richard Drake
Seattle Children’s Hospital: Stephanie Lammers; Kara Cooper
Sydney Children’s Hospital: Sandra Lowe
University of California, San Francisco: Melissa Zerofsky
University of Iowa: Gretchen Cress; Karen Scudiero
University of Minnesota: Cathy Kneeland
University of Pittsburgh: Kathleen Calabro; Adam Kufen
University of Texas Southwestern Medical Center: Amber Crabb; Lauren Plummer
Washington University: Ashley Simpson
The CPDPC Consortium is cofunded by the National Cancer Institute and the National Institute of Diabetes and Digestive and Kidney Diseases: grants U01DK108334; U01DK108314; U01DK108288; U01DK108300; U01DK108326; U01DK108323; U01DK108320; U01DK108332; U01DK108327; U01DK108306 and U01DK108328. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1.Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014,74:2913–2921. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014,64:9–29. [DOI] [PubMed] [Google Scholar]
- 3.Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raimondi S, Lowenfels AB, Morselli-Labate AM, et al. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best Pract Res Clin Gastroenterol. 2010;24:349–358. [DOI] [PubMed] [Google Scholar]
- 5.Whitlock TL, Tignor A, Webster EM, et al. A scoring system to predict readmission of patients with acute pancreatitis to the hospital within thirty days of discharge. Clin Gastroenterol Hepatol. 2011;9:175–180; quiz e18. [DOI] [PubMed] [Google Scholar]
- 6.Andersen DK, Andren-Sandberg Å, Duell EJ, et al. Pancreatitis-diabetes-pancreatic cancer: summary of an NIDDK-NCI workshop. Pancreas. 2013;42:1227–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malka D, Hammel P, Sauvanet A, et al. Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology. 2000;119:1324–1332. [DOI] [PubMed] [Google Scholar]
- 8.Pasca di Magliano M, Forsmark C, Freedman S, et al. Advances in acute and chronic pancreatitis: from development to inflammation and repair. Gastroenterology. 2013;144:e1–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.§SEC. 1083. Scientific Framework for Recalcitrant Cancers. Available at https://www.gpo.gov/fdsys/pkg/PLAW-112publ239/html/PLAW-112publ239.htm. Accessed July 12, 2018.
- 10.National Cancer Institute. Scientific Framework for Pancreatic Ductal Adenocarcinoma (PDAC). Available at https://deainfo.nci.nih.gov/advisory/ctac/workgroup/pc/pdacframework.pdf Accessed July 12, 2018.
- 11.Consortium for the Study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer Clinical Centers (CSCPDPC -CCs) (U01). Available at https://grants.nih.gov/grants/guide/rfa-files/RFA-DK-14-027.html. Accessed July 12, 2018.
- 12.Consortium for the Study of Chronic Pancreatitis, Diabetes and Pancreatic Cancer Coordination and Data Management Center (CSCPDPC- CDMC) (U01). Available at https://grants.nih.gov/grants/guide/rfa-files/RFA-DK-14-028.html. Accessed July 12, 2018.