Abstract
Introduction:
Acute Appendicitis is the most common emergent abdominal surgery worldwide. diagnosis based on clinical assessment, laboratory and radiological investigations and appendectomy is the treatment of choice. Removing a normal appendix is a relatively common surgical issue, defined as negative appendectomy (NA). Multiple risk factors contribute to NA; female gender, normal WBC, normal CRP count, and CT scan unavailability. However, recently NA is decreasing in incidence after CT scan and Alvarado scoring.
Aim:
We aimed to estimate the rate of negative appendectomy, and determine possible risk factors among King Abdulaziz University Hospital.
Patients and Methods:
Article has a retrospective character and included non-incidental 441 patients who undergo an appendectomy, during period 2008 to 2018.
Results:
Negative Appendectomy incidence (9.5%) was higher among females at (64.3%). Gynecological complaints were seen in (22.2%) of cases with a sign for Negative Appendectomy. Surgery reports documented (29.6%) of female ovarian cyst diseases. Alvarado scoring at presentation was less than 7 in (69%) of cases with statistical significance value. Normal WBC count (50%), for automated neutrophil (45.2%) was high, and same number were recorded with the normal neutrophil count, all of them have statically significant relation with NA.
Conclusion:
Proper clinical evaluation involves documenting Alvarado score, using CRP, efficient radiological utilization. Also, considering more referrals to gynecological specialists of similar presentation especially females at reproductive age. Investing in time and equipment for proper clinical assessment can avoid the unnecessary burden and save our resources for better use.
Keywords: Appendectomy, Acute Appendicitis, Leukocytes, C-Reactive Protein
1. INTRODUCTION
Appendicitis is the most common emergent surgical operation worldwide, account for 7% lifetime risk. Nowadays, it is starting to increase in incidence in developing countries; an appendectomy is the treatment of choice (1-3).
Appendicitis present usually with anorexia, and tenderness with localized rigidity in the right lower quadrant over Mc Burney’s point (4). Upon the new guidelines released in 2010, the current diagnosis is based on patient history, clinical examination and supported by imaging and Biomarkers such as WBC count and CRP (5, 6). Alvarado score include symptoms, signs, and laboratory investigations are considered as a diagnostic strategy (7).
CT scan and US imaging are used for the diagnosis and make it more accurate. CT scan is more sensitive and specific than the US and it’s associated with a smaller number of negative appendectomy (8, 9).
Sometimes, an appendectomy done to a normal appendix, it has known as a negative appendectomy (NA) (10). Recently, there has been a consistent decline in NAR in the United States because of better diagnostic imaging tools (11). In adult clinically suspected patients, acute appendicitis was excluded if WBC count and CRP were normal at admission and during follow up period; normal WBC count is a risk factor to perform an NA (12).
Patients who undergone NA had more hospitalization stay and costs, and higher morbidity when compared with no perforated PA. NA could be decreased by doing more observation and investigation for clinically suspected patients and not send them for surgery directly (13, 14).
Aim: To estimate the rate of negative appendectomy, and determine possible risk factors among King Abdulaziz University Hospital.
2. AIM
The aim of the study was to estimate the rate of negative appendectomy, and determine possible risk factors among King Abdulaziz University Hospital.
3. MATERIAL AND METHODS
A retrospective review study was done at King Abdulaziz university hospital (KAUH) in the western region of Saudi Arabia, Jeddah in June 2018 by using medical records (Phoenix). All patients who underwent appendectomy from January 2008 to June 2018 under the department of general surgery were included in the study. We excluded eleven incidental appendectomy cases and fifty-three files couldn’t be reached (Inactive paper files). A sample size of five hundred and five patients was included in the study, four hundred forty-one files reached. The variables include demographic data (age, nationality), vitals (pulse & body temperature), clinical presentation, laboratory tests (WBC count, neutrophil count, CRP test). Alvarado score, imaging (CT, US), surgery notes, histopathology result, duration of hospitalization and outcomes. Data entry was performed by using Microsoft Excel 2016 and statistically analyzed by SPSS 21 using descriptive statistic, chi-square was estimated for the significance between NA and presenting complaint, the examination finding, Alvarado score, referrals, lab tests, and imaging. The t-test was estimated for the significance between NA, TLC mean and automated neutrophils mean. For all tests the p value was considered statistically significant if it was <0.05.
4. RESULTS
Four hundred and forty one patients underwent appendectomy were studied; out of them 275 (62.4%) males and 166 (37.6%) females.
Positive appendectomy (PA) was proven in 399 cases (90.3%), while 42 cases (9.5%) had negative appendectomy (NA). In NA sample, 15 cases (35.7%) were males and 27 cases (64.3%) were females. Significant relation between NA and gender (P=0.000179). Most admissions were in the young age group between 13-30 year, significant relation was reported between NA and age groups (P=0.015) (Table 1).
Table 1. Number of appendectomies for each age group and gender.
| Gender | Age-group | Total appendectomies | NA | NAR | p-value |
|---|---|---|---|---|---|
| Female | Children | 34 | 1 | 3.7% | 0.037 |
| Young age | 109 | 24 | 88.9% | ||
| Middle age | 17 | 2 | 7.4% | ||
| Seniors | 6 | 0 | 0% | ||
| Male | Children | 69 | 3 | 20% | 0.312 |
| Young age | 169 | 12 | 80% | ||
| Middle age | 37 | 0 | 0% | ||
| Seniors | 9 | 0 | 0% |
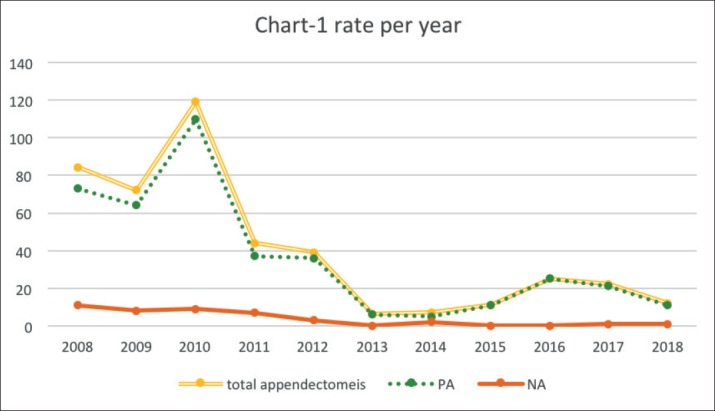
Appendectomy procedure rate was highest in 2010 by (26.9%) and reach its lowest in 2013 to be (1.4%). While, NAR was most common in 2008 (26.2%) and the minimum rate was zero during 2013, 2015 and 2016 (Figure 1).
Figure 1. Rate per year.
Among all patients who underwent appendectomies the most common symptom was abdominal pain 408 cases (92.5 %), (29%) of patients reported migration of pain, most of the cases pain was localize at right lower quadrant 245 case (55.6%), 2nd most common symptom was vomiting 290 cases (65.8%), followed by nausea 183 cases (41.5%), fever 158 cases (35.8 %), anorexia 140 cases (31.7%), diarrhea 55 cases (12.5%), urology complains 31 cases (7%), constipation 25 cases (5.7%) and gynecological complains 15 cases (3.4%) (Table 2).
Table 2. History part of clinical evaluation and reported referrals.
| PA | NA | P-value | ||
|---|---|---|---|---|
| Chief complaint | Abdominal pain (91.7%) | Abdominal pain (92.9%) | 0.743820 | |
| Vomiting (2%) | Fever (2.4%) | |||
| Pain localization | RLQ (55.9%) | RLQ (52.4%) | 0.806564 | |
| periumbilical (20.3%) | Periumbilical (33.3%) | |||
| epigastric area (5.5%) | - | |||
| other (10.2%) | other (7.2%) | |||
| Abdominal pain | (2.9%) | (2.5%) | 0.8947 | |
| Vomiting | (66.4%) | (59.5%) | 0.340648 | |
| Nausea | (40.4%) | (52.4%) | 0.145391 | |
| Fever | (36.8%) | (26.2%) | 0.142718 | |
| Anorexia | (31.1%) | (38%) | 0.396018 | |
| Diarrhea | (13.5%) | (2.4%) | 0.035428 | |
| Urology complains | (7%) | (7.1%) | 0.996250 | |
| Constipation | (5%) | (11.9%) | 0.071614 | |
| Gynecological complains | (5.5%) | (22.2%) | 0.00237 | |
| Referral | yes | 12 cases (3%) | 3 cases (7.1%) | 0.128 |
| no | 307 cases (79.9%) | 27 cases (64.3%) | ||
| Referred To | - | Ob/gyn: 2cases (4.8%) | 0.001 | |
| Fetal-medicine: 1cases (0.3%) | - | |||
| Endocrine: 1cases (0.3%) | - | |||
| Infectious: 1cases (0.3%) | - | |||
| Cardiology: 1cases (0.3%) | - | |||
In NA patients particularly the most common symptom was abdominal pain 40 cases (95.2%), (28.6%) of patients reported migration of pain, followed by vomiting 25 cases (59.5%), nausea 22 cases (52.4%) anorexia 16 cases (38.1%), fever 11 cases (26.2%), gynecological complains 6 cases (22.2%) of females, constipation 5 cases (11.9%), urology complains 3 cases (7.1%), and diarrhea 1 case (2.4%).
Significant relation with NA and both gynecological complains (P=0.00237) and diarrhea (P=0.0354). In NA 25 cases (59.5%) presented after days of symptoms started, followed by hours in 4 cases (9.5%) and weeks in 3 cases (7.1%). although, NA cases reported that duration of illness extended till months (4.8%) the difference is statistically significant (P=0.003). While in PA 72.2% presented after days of symptoms started, followed by hours (11%), weeks (2.3%) and months in (1%). Chronic illnesses of PA patients were 10 cases (2.3%) DM, 8 cases (1.8%) HTN, 4 cases (1.1%) CVD, 24 cases (5.4%) other. No chronic illnesses in all NA cases, except one case known to have chronic bronchial asthma.
At presentation in emergency department. 114 cases (25.9%) of the patients recorded fever (Temperature≥37.3). Meanwhile, 6 cases (14.3%) of NA had fever. Right iliac fossa tenderness was reported positively in 340 cases (85.2%) of PA. While, 33 cases (78.6%) of NA patients had RIF tenderness (Table 3). Similarly, rebound tenderness was positive in 250 cases (62.7%) of PA patients and 22 cases (52.4%) of the patients who underwent NA had positive rebound tenderness. In addition, Alvarado scoring was estimated for all cases, patients who underwent NA revealed scores less than 7 (69%), percentage for patient scored more than 7 (31%) statistical significance was prove (P=0.008). Referrals to gynecological clinic was documented in 2 cases (0.5%) of all females who underwent appendectomy, both of them were NA. statistically significant (P=0.001).
Table 3. Temperature, examination, Alvarado score (Unit=cases).
| PA(n=399) | NA(n=42) | P-value | ||
|---|---|---|---|---|
| Normal Temperature | 174 (43.6%) | 20 (47.6%) | 0.123 | |
| Hyperthermia | 107 (26.8%) | 6 (14.3%) | ||
| Alvarado >7 | 210 (52.6%) | 13 (31%) | 0.008 | |
| Alvarado <7 | 189 (47.4%) | 29 (69%) | 0.008 | |
| RIF Tenderness | yes | 340 (85.2%) | 33 (78.6%) | 0.420 |
| no | 11 (2.8%) | 2 (4.8%) | ||
| Rebound Tenderness | yes | 250 (62.7%) | 22 (52.4%) | 0.513 |
| no | 97 (24.3%) | 11 (26.2%) | ||
Along the 42 cases of NA, 21 cases (50%) exhibited normal TLC (4.5-11.5k/uL), while 18 cases (42.9%) of NA had high count (TLC>11.6k/uL), and three 3 cases (7.1%) had low count (TLC<4.4k/uL). For automated neutrophil count 19 cases (45.2%) was high (>7.6k/uL), same number were recorded with normal count (2-7.5k/uL). 50 cases (11.3%) of total sample had CRP test, 49 cases (11.1%) had high CRP test, only 1 case had normal CRP test (0.2%), while in NA 5 cases (11.8%) had CRP all of them was high. Of all 166 females, pregnancy test was applied for 66 cases. all of them was negative except in four females, two of pregnant females had NA (Table 4).
Table 4. laboratory results, and the radiological report (Unit=cases).
| PA(n=399) | NA(n=42) | P-value | ||
|---|---|---|---|---|
| TLC Mean | 14.70±6.54 | 11.25±5.99 | 0.001157 | |
| Automated Neutrophils Mean | 13.50±11.80 | 8.26±6.34 | 0.004795 | |
| Pregnancy-test | +ve | 2 (3.8%) | 2 (15.4%) | 0.115888 |
| -ve | 51 (96.2%) | 11 (84.6%) | ||
| x-ray | +ve | 15 (3.8%) | 1 (2.4%) | 0.633 |
| -ve | 53 (13.3%) | 6 (14.3%) | ||
| ultrasonography | +ve | 85(21.3%) | 9 (21.4%) | 0.055 |
| -ve | 65 (16.3%) | 16 (38.1%) | ||
| Computed-tomography | +ve | 70 (17.5%) | 3 (7.1%) | 0.35 |
| -ve | 8 (2%) | 1 (2.4%) | ||
Histopathological examination showed 24 cases (57.1%) with no pathological diagnosis, 10 cases (23.8%) lymphoid follicle, fecalith 3 cases (7.1%), fibrous obliteration 2 cases (4.8%), food impaction 1 case (2.4%). Although, out of 42 NA cases US was obtained for 25 cases (59.5%), 9 cases (21.4%) showed positive signs of inflammation and negative signs were reported in 16 cases (38.1%). While, from the 4 patients who performed CT scan one case revealed negative appendicular inflammatory signs (2.4%), and for the other three cases appendicitis signs were positive (7.1%).
Surgery reports in NA patients documented 10 cases (37.04%) of females exhibited gynecological diagnosis as ovarian cyst 5 cases (18.5%), ruptured ovarian cyst 3 cases (11.1%), fallopian tube adhesions 1 case (3.7%) and fallopian tube torsion 1 case (3.7%). out of all NA surgery findings notes were gross inflammation 23 cases (54.8%), Adhesions 2 cases (4.8%), clear free fluid 4 cases (9.5%). Besides that, 3 cases (7.1%) didn’t reveal any gross inflammatory signs.
Mean length of hospitalization for patient who underwent PA was 3±0.2 days which is slightly higher than the patients who had NA 2.5±0.2 days. In the same manner, mean time of antibiotic intake were 4.992±12.1157 days for PA patients while for NA patients was 4±0.45 days.
5. DISCUSSION
Surgical excision of a normal appendix exposes patients to unnecessary anesthesia and surgical complications, it can be due to improper clinical assessment, unavailability of diagnostic modalities, or to prevent the possible adverse effect of AA, which delays the identification of the accurate diagnosis. Many diseases resemble AA presentations. So, more effort should be directed toward decreasing NAR and its complications on patients and hospitals (15).
A significant relation between NA and female gender (P=0.000182), 35.7% males and (64.3%) females. This was approved by other study revealed (22.9%) of cases were NA, (65%) of them was females and (35%) males (16). Our study results documented higher incidence at the reproductive age group, as teaching hospital we should have to expect lower NA rate (14).
Studies done in the United States, California University, NA rate was (9%). In Saudi Arabia, Arar central hospital NA rate was (3%), and In Jeddah KAUH 2012 NAR was (6.4%) (17-19). A study was done in Riyadh, in the period 1998-2003 found those 23±8.67 years is the mean age-associated more with NA (20). A privately insured patient was considered as a risk factor also (17).
Through our NA data females with known gynecological conditions were (25%) and with associated gynecological presentation were (24%) for NA and (5.5%) for PA cases with the statistically significant difference (p=0.00237). Although, not all of them were referred to the Gynecology clinic. Just as important, in another study Gynecological, referral was sought in (57.1%) of females who were suspected to have AA; nearly all of them have underlying gynecological cause for acute abdomen, and appendicitis was ruled out (21). Therefore, to reduce NAR among young age females, the transvaginal ultrasound was needed in addition to abdominal ultrasound in suspected gynecological disease (22).
In the United States, NAR is more in females than in males. There are many gynecological diseases similar to AA, and NA is more frequent among reproductive-age women (11, 17). NA was found to be higher among females at Arar Central Hospital in the Northern Border Province of Saudi Arabia (18).
In our study, the primary presenting complaint in NA patients is abdominal pain, followed by vomiting, nausea, anorexia, and fever, none of the associated symptoms show statistical significance. Similarly, abdominal pain was the most frequent symptom in other researches followed by vomiting (62.1%), anorexia (58.6%), nausea (48.3%), and fever (24.1%). Vomiting showed significant difference p=0.072 (19).
The challenge of AA diagnosis is the atypical presentation, variation of presenting complaint severity and subjective factors as the description of pain course and nature. However, (80%) of diagnosing AA depends on clinical assessment (23). Despite, from our total patients (48.1%) presented to the hospital had normal body temperature; (51.3%) of them had NA and (47.8%) PA, no statistical significance was proven. Conversely, other researches proved that normal temperature was significant in relation to appendectomy (p=0.016) (22). Only (3.7%) of their PA patients had a normal body temperature. While fever was recorded in (96.1%) of PA patients (24). Furthermore, our study showed that Alvarado score is statically significant (p=0.008), with NA patients score > seven in (31%) of cases, that may indicate emergent surgery for the normal appendix. This goes with another study, where (41%) of NA patients their Alvarado score was > 7 (p=0.0001). For this reason, it’s advisable to do CT scan along with Alvarado score to limit this rate (16).
While literature (25,26) had proven the significance of diagnostic imaging, our study did not favor the same. We found that X-ray, CT, US are insignificant in relation to NA. Although, US used in half of NA cases it revealed positive inflammatory signs in (21.4%) cases and negative signs in (38.1%) cases. Moreover, CT percentage of usage among NA cases was (9.5%), positive signs appeared in (7.1%), and no signs of inflammation were shown in (2.4%). Comparable study perceived similar results, for instinct King Khalid University Hospital, (5.5%) of their patients had NA in spite of performing preoperative CT scan, which means that CT scan does not conclusively improve the outcome of misguided diagnosis (11, 20).
In the western region of Saudi Arabia, imaging and laboratory findings are very helpful in starting the diagnosis of AA if atypical presentation were found (18).
Previous studies consistently demonstrated that preoperative imaging coincides with reductions in the NAR (27) and the escalated concerns over diagnostic errors highly recommend incorporation of US, CT, and X-ray implantation while establishing AA as the diagnosis (6).
Variation in performing radiological investigation for AA through initial evaluation might be due to multiple factors, such as availability of equipment and expertise, institutional preference and the alleged need for diagnosis confirmation (28). Nevertheless, we believe that low utilization of diagnostic imaging is the risk factor that exposes patients to NA.
Mean TLC is (14.70±6.54k/ uL) in PA and (11.25±5.99k/uL) in NA, with proven statistical significance (P=0.001157). Besides, automated neutrophils are lower in NA cases 8.26±6.34 than PA cases 13.50±11.80 (P=0.004795). Other study showed the mean of TLC which was high in PA 13.91±4.04, while in NA WBC count was 11.43±3.78 (p=0.0001). Accordingly, delaying an appendectomy in patients with TLC in ranges between (9-8k/uL) would reduce the NAR (15). Similarly, CRP which has moderate diagnostic value as the inflammatory marker (24), (11.3%) of our patients had CRP marker done, in another study CRP show statically significant difference (P < 0.001) between PA and NA count for (73%), (46%) respectively.
Our judge for NA based on inflammatory cells infiltration present under microscope on histopathology lab (29), in our study, histopathological examination of NA reports no pathological diagnosis (60%), lymphoid follicle (25%), fibrous obliteration (5%), fecalith (7.5%) and food impaction (2.5%) with no inflammatory cells have been noted. In contrast, to study done in Egypt, the obstructed lesion has evidence of inflammation represent as fecalith (9.6%) and fruit seeds (1.2%) (30).
KAUH surgeons consider 23 out of 42 cases of NA inflamed grossly during the surgery, such disagreement between surgeons and pathologists was reported in similar studies in Riyadh, 11 of the 43 NA patients looked inflamed grossly as will (26, 31). Other findings are documented as an ovarian cyst, fallopian tube torsion, likewise with previous study findings, which can be a reason for the NA to be higher in female (18).
NA duration of hospitalization and duration of antibiotics course both were lower than PA. Controverting to our results, previous studies documented that average cost of hospitalization is higher for NA cases in median cost per admission than PA cases. Although the cost of hospitalization in our hospital couldn’t be obtained, we are sure it is considered a burden in different ways. For example, availability of beds, equipping staff, financially costing the hospital administration (14).
Limitations: Fifty-three files were inactive. Also, detailed history, physical examination, and radiological reports data were not adequately documented in 2008-2012. Alvarado score was not calculated in the patient’s file, and we calculate a patient’s score by the available data in the profile.
6. CONCLUSION
On the whole, NAR was (9.5 %), with significant risk factors for the female gender, TLC, WBC left shift, gynecological complaints, and gynecology referrals. For these reasons, we urge proper clinical evaluation involve documenting Alvarado score, using CRP, efficient radiological utilization. Also, considering more referrals to gynecological specialists in patients with similar presentation. Moreover, about the literature with holding appendectomy is recommended if WBC is within the normal range. Investing in time and equipment for proper clinical assessment can avoid the unnecessary burden and save our resources for better use.
Acknowledgements:
We would like to thank road of change summer school. And students who participated as a data collector: Fatheya Adam and Noor Shibriq.
Authors contributions:
YFA did substantial contribution to conception and design. YFA, AMA, RHA, SNF, EHA, OJA were involved in substantial contribution to acquisition of data and substantial contribution to analysis and interpretation of data. YFA, HAR, MRA were involved in critically revising the article for important intellectual content and final approval of the version to be published. All authors revised and approved the manuscript before submission.
Conflict of interest:
none declared.
REFERENCES
- 1.Townsend CM, Beauchamp RD, Evers BM, Mattox KL. Sabiston Textbook of Surgery E-Book. Elsevier Health Sciences. 2016 Apr 22; [Google Scholar]
- 2.Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, Ansaloni L, Coccolini F, Vijayan D, Abbas A, Abongwa HK, Agboola J. Prospective observational study on acute appendicitis worldwide (POSAW) World Journal of Emergency Surgery. 2018 Dec;13(1):19. doi: 10.1186/s13017-018-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sulu B, Gunerhan Y, Palanci Y, et al. Epidemiological and demographic features of appendicitis and influences of several environmental factors. Ulusal Travma Acil Cerrahi Derg. 2010;16:38–42. [PubMed] [Google Scholar]
- 4.World Health Organization. Surgical care at the district hospital. World Health Organization; 2003. [Google Scholar]
- 5.Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. British Journal of Surgery. 2013 Feb 1;100(3):322–329. doi: 10.1002/bjs.9008. [DOI] [PubMed] [Google Scholar]
- 6.Florence M, Flum DR, Jurkovich GJ, Lin P, Steele SR, Symons RG, Thirlby R. Negative appendectomy and imaging accuracy in the Washington state surgical care and outcomes assessment program. Annals of surgery. 2008 Oct 1;248(4):557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 7.Vaghela K, Shah B. Diagnosis of Acute Appendicitis Using Clinical Alvarado Scoring System and Computed Tomography (CT) Criteria in Patients Attending Gujarat Adani Institute of Medical Science–A Retrospective Study. Polish journal of radiology. 2017;82:726. doi: 10.12659/PJR.902246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosen MP, Ding A, Blake MA, Baker ME, Cash BD, Fidler JL, Grant TH, Greene FL, Jones B, Katz DS, Lalani T. ACR Appropriateness Criteria® right lower quadrant pain–suspected appendicitis. Journal of the American College of Radiology. 2011 Nov 1;8(11):749–755. doi: 10.1016/j.jacr.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Webb EM, Nguyen A, Wang ZJ, Stengel JW, Westphalen AC, Coakley FV. The negative appendectomy rate: who benefits from preoperative CT? American Journal of Roentgenology. 2011 Oct;197(4):861–866. doi: 10.2214/AJR.10.5369. [DOI] [PubMed] [Google Scholar]
- 10.Ruffolo C, Fiorot A, Pagura G, Antoniutti M, Massani M, Caratozzolo E, et al. Acute appendicitis: What is the gold standard of treatment? World J Gastroenterol. 2013;19(47):8799–8807. doi: 10.3748/wjg.v19.i47.8799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, Cornwell EE, Chang DC, Siram SM. Negative appendectomy: a 10-year review of a nationally representative sample. The American Journal of Surgery. 2011 Apr 1;201(4):433–437. doi: 10.1016/j.amjsurg.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Bates MF, Khander A, Steigman SA, Tracy TF, Luks FI. Use of white blood cell count and negative appendectomy rate. Pediatrics. 2014 Jan 1;133(1):e39–44. doi: 10.1542/peds.2013-2418. [DOI] [PubMed] [Google Scholar]
- 13.Çavuşoğlu YH, Erdoğan D, Karaman A, Aslan MK, Karaman I, Tütün ÖÇ. Do not rush into operating and just observe actively if you are not sure about the diagnosis of appendicitis. Pediatric surgery international. 2009 Mar 1;25(3):277–282. doi: 10.1007/s00383-009-2331-0. [DOI] [PubMed] [Google Scholar]
- 14.Lu Y, Friedlander S, Lee SL. Negative appendectomy: clinical and economic implications. The American Surgeon. 2016 Oct 1;82(10):1018–1022. [PubMed] [Google Scholar]
- 15.Joshi MK, Joshi R, Alam SE, Agarwal S, Kumar S. Negative Appendectomy: an Audit of Resident-Performed Surgery. How Can Its Incidence Be Minimized? Indian Journal of Surgery. 2015 Dec 1;77(3):913–917. doi: 10.1007/s12262-014-1063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kryzauskas M, Danys D, Poskus T, Mikalauskas S, Poskus E, Jotautas V, Beisa V, Strupas K. Is acute appendicitis still misdiagnosed? Open Medicine. 2016 Jan 1;11(1):231–236. doi: 10.1515/med-2016-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGory ML, Zingmond DS, Nanayakkara D, Maggard MA, Ko CY. Negative appendectomy rate: influence of CT scans. The American surgeon. 2005 Oct 1;71(10):803–808. [PubMed] [Google Scholar]
- 18.Jat MA, Al-Swailmi FK, Mehmood Y, Alrowaili M, Alanazi S. Histopathological examination of appendicectomy specimens at a district hospital of Saudi Arabia. Pakistan journal of medical sciences. 2015 Jul;31(4):891. doi: 10.12669/pjms.314.7453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-gaithy ZK. Clinical value of total white blood cells and neutrophil counts in patients with suspected appendicitis: retrospective study. World Journal of Emergency Surgery. 2012 Dec;7(1):32. doi: 10.1186/1749-7922-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khairy G. Acute appendicitis: is removal of a normal appendix still existing and can we reduce its rate? Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association. 2009 Jul;15(3):167. doi: 10.4103/1319-3767.51367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi MK, Joshi R, Alam SE, Agarwal S, Kumar S. Negative Appendectomy: an Audit of Resident-Performed Surgery. How Can Its Incidence Be Minimized? Indian Journal of Surgery. 2015 Dec 1;77(3):913–917. doi: 10.1007/s12262-014-1063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for non obstetric conditions: algorithms and radiation dose considerations. Radiographics. 2007 Nov-Dec;27(6):1705–1722. doi: 10.1148/rg.276075002. [DOI] [PubMed] [Google Scholar]
- 23.Shirah BH, Shirah HA, Alhaidari WA, Elraghi MA, Chughtai MA. The role of preoperative graded compression ultrasound in detecting acute appendicitis and influencing the negative appendectomy rate. Abdominal Radiology. 2017 Jan 1;42(1):109–114. doi: 10.1007/s00261-016-0862-0. [DOI] [PubMed] [Google Scholar]
- 24.Msolli MA, Beltaief K, Bouida W, Jerbi N, Grissa MH, Boubaker H, Boukef R, Nouira S. Value of early change of serum C reactive protein combined to modified Alvarado score in the diagnosis of acute appendicitis. BMC emergency medicine. 2018 Dec;18(1):15. doi: 10.1186/s12873-018-0166-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park JH LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. Journal of Korean medical science. 2014 Sep 1;29(9):1308–1316. doi: 10.3346/jkms.2014.29.9.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drake FT, Flum DR. Improvement in the diagnosis of appendicitis. Advances in surgery. 2013;47:299. doi: 10.1016/j.yasu.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paulson EK, Kalady MF, Pappas TN. Erratum: Suspected appendicitis (New England Journal of Medicine (Journal 16, 2000) 348 (236-242)) New England Journal of Medicine. 2003 Jul 17;349(3):305. doi: 10.1056/NEJMcp013351. [DOI] [PubMed] [Google Scholar]
- 28.Zosimas D, Lykoudis PM, Leung P, Strano G, Shatkar V. Is ultrasound a reliable diagnostic tool for acute appendicitis? A single centre experience. Annali italiani di chirurgia. 2017 Nov;6 [PubMed] [Google Scholar]
- 29.Shrestha R, Ranabhat SR, Tiwari M. Histopathologic analysis of appendectomy specimens. Journal of pathology of Nepal. 2012 Jan 1;2(3):215–219. [Google Scholar]
- 30.Hedya MS, Nasr MM, Ezzat H, Hamdy HM, Hassan AM, Hammam O. Histopathological findings in appendectomy specimens: a retrospective clinicopathological analysis. J Egypt Soc Parasitol. 2012 Apr;42(1):157–164. doi: 10.12816/0006303. [DOI] [PubMed] [Google Scholar]
- 31.Andersson R, Hugander A, Thulin A, Nystrom PO, Olaison G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ. 1994 Jan 8;308(6921):107–110. doi: 10.1136/bmj.308.6921.107. [DOI] [PMC free article] [PubMed] [Google Scholar]



