Case Report
A 78-year-old-man with chronic mild hypertension, treated with losartan, and uncomplicated, adult-onset diabetes mellitus, treated with metformin, developed increasing abdominal pain associated with serum lactate (6.9 mmol/L) 24 hours after treatment with 30 g orally administered sodium polystyrene sulfonate (SPS) with sorbitol for hyperkalemia (initial potassium 7.3 mmol/L, normal: 3.5-5.2 mmol/L). The patient had presented 1 day earlier with 8 voluminous, watery, non-bloody bowel movements per day for 7 days. Physical examination revealed blood pressure 109/46 mm Hg, pulse 62 beats/minute, temperature 36.4°C, dry mucous membranes, minimal abdominal tenderness, and guaiac-negative stool. Laboratory findings included hemoglobin 11.8 g/dL, leukocytes 12,400 × 106/L, glucose 206 mg/dL, blood urea nitrogen 91 mg/dL, and creatinine 6.6 mg/dL.
Hyperkalemia was associated with normal serum troponin levels and no electrocardiogram abnormalities. The potassium level quickly normalized after also receiving 18 U insulin and 50 mEq sodium bicarbonate; dialysis was not required. Stool cultures for bacteria and stool examination for ova and parasites were negative. Computed tomography of the abdomen and pelvis revealed colonic mural thickening consistent with colitis. Esophagogastroduodenoscopy revealed 3 small, non-bleeding, prepyloric ulcers. Histopathologic examination of biopsies from the ulcer margins revealed nonspecific reactive changes, no dysplasia, no Helicobacter pylori, and no crystal deposits. Colonoscopy performed 3 days after receiving SPS was highly consistent with ischemic colitis in the descending colon to cecum (Figure 1).1 Histopathology revealed inflamed and ulcerated colonic mucosa and basophilic, non-polarizable, angulated, intramucosal crystals, highly consistent with SPS-induced ischemic colitis (Figure 2).2 Extensive evaluation revealed no other etiologies for ischemic colitis. The patient recovered well.
Figure 1.
(A and B) Colonoscopy revealing acute purulent whitish-yellow exudate, edema, and mucosal friability in distal colon. Numerous small superficial ulcers in the proximal colon and multiple round, smooth, soft, and friable nodules in the mid-colon, which are endoscopic features of hemorrhagic nodules, are complementary to radiologic findings of thumbprinting and are highly characteristic of ischemic colitis.
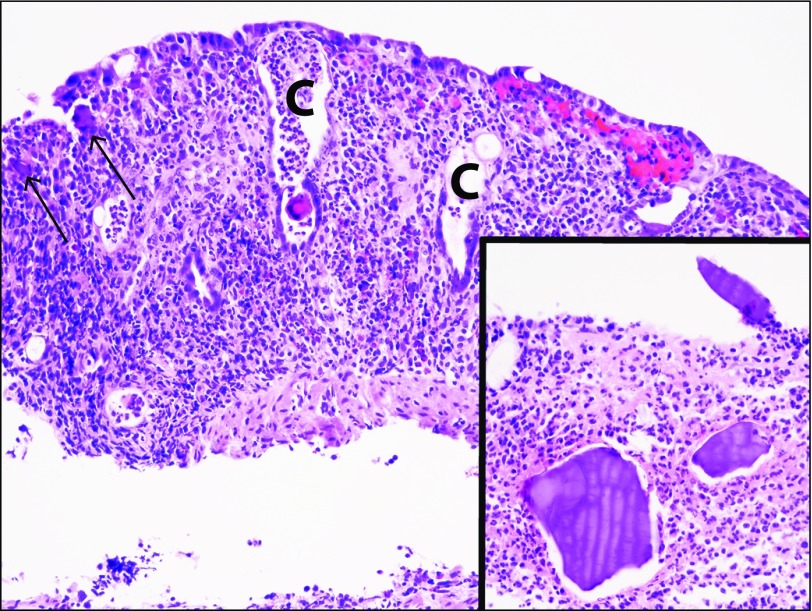
Figure 2.
Medium-powered hematoxylin and eosin stain of colonic mucosa biopsy showing atrophic crypts (C labels) and crypt dropout in the presence of moderately severe acute inflammation, which are compatible with ischemic colitis. Small sodium polystyrene sulfonate (SPS) crystals are embedded within colonic mucosa (arrows), which are better delineated at higher magnification in the surface inflammatory exudate (inset). The basophilic staining, angulated shape, and non-polarizable behavior of these crystals are characteristic for SPS in the absence of cholestyramine ingestion.
Hyperkalemia was most likely from acute renal failure and dehydration. SPS, an ion-exchange resin, reduces hyperkalemia by exchanging sodium ions for potassium ions in the colon. SPS is associated with approximately 60 cases of colonic injury and ischemic colitis, attributed to rapid osmotic shifts or vasospasm of intestinal vessels, possibly mediated by hyperreninemia.3 One third of cases have been fatal,3 often from colonic ischemia causing septicemia or colonic perforation.4
Our patient presented with typical symptoms of acute abdominal pain and diarrhea, laboratory abnormalities of leukocytosis, azotemia, and hyperlacticacidemia, and colonoscopic findings of acute mucosal exudates, ulcers, friability, and hemorrhagic nodules. Histopathologic findings of angulated, non-polarizable, and basophilic crystals within the colonic mucosa are characteristic.3 Cholestyramine causes histologically similar crystal deposition, but this was excluded by patient history. Kidney injury is strongly associated with SPS toxicity.3 Our patient had gastric ulcers, which are associated with SPS ingestion, but the current association was likely coincidental because SPS crystals were absent in the gastric biopsies.5
Disclosures
Author contributions: AI Edhi and M. Amin wrote the initial draft of the manuscript. MS Cappell, N Sharma, and A Patel edited the manuscript. A Patel, AI Edhi, and MS Cappell share first authorship. MS Cappell is the article guarantor.
Financial disclosure: MS Cappell is a member of the speaker’s bureau for AstraZeneca and Daiichi Sankyo, received one-time consulting fees from Mallinckrodt and Shire, and is a consultant for the US FDA Advisory Committee for Gastrointestinal Drugs.
Informed consent was obtained for this case report.
References
- 1.Cappell MS. Intestinal (mesenteric) vasculopathy II. Ischemic colitis and chronic mesenteric ischemia. Gastroenterol Clin North Am. 1998;27(4):827–60. [DOI] [PubMed] [Google Scholar]
- 2.Parfitt JR, Driman DK. Pathological effects of drugs on the gastrointestinal tract: A review. Hum Pathol. 2007;38(4):527–36. [DOI] [PubMed] [Google Scholar]
- 3.Harel Z, Harel S, Shah PS, Wald R, Perl J, Bell CM. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: A systematic review. Am J Med. 2013;126(3):264.e9–24. [DOI] [PubMed] [Google Scholar]
- 4.Dunlap RH, Martinez R. Total colectomy for colon perforation after Kayexalate administration: A case report and literature review of a rare complication. J Surg Case Rep. 2016;2016(10):rjw167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abraham SC, Bhagavan BS, Lee LA, Rashid A, Wu TT. Upper gastrointestinal tract injury in patients receiving kayexalate (sodium polystyrene sulfonate) in sorbitol: Clinical, endoscopic, and histopathologic findings. Am J Surg Pathol. 2001;25(5):637–44. [DOI] [PubMed] [Google Scholar]