Abstract
Hydrogen peroxide (H2O2) is an oxidizing agent found in many household products. It is a clear liquid at room temperature, allowing it to be mistaken for water if unlabelled. Ingestion of H2O2 can have serious sequelae even in low volumes and concentrations.We present a case study of H2O2 poisoning and discuss the pertinent radiographical findings.
Summary
Hydrogen peroxide (H2O2) is an oxidizing agent found in many household products. It is a clear liquid at room temperature, allowing it to be mistaken for water if unlabelled. Ingestion of H2O2 can have serious sequelae even in low volumes and concentrations. We present a case study of H2O2 poisoning and discuss the pertinent radiographical findings.
Clinical presentation
A healthy 21-year-old male unintentionally ingested approximately one mouthful of 3% H2O2 stored in his relative’s refrigerator. He presented to the emergency department with vomiting and pain in his mouth, throat and epigastrium. He was tachycardic (100 beats min−1) and mildly hypertensive (155/100 mmHg) but not hypoxic (SpO2 97% on room air). A clinical examination revealed dysphonia with mild erythema and oedema of the oropharynx and uvula; the abdominal and respiratory examinations were otherwise unremarkable. Blood and biochemical investigations were also normal.
Imaging findings
A CT scan was performed to exclude gastrointestinal perforation, which demonstrated pneumatosis and mucosal thickening throughout the stomach and proximal duodenum, as well as extensive portal venous gas (Figures 1–3).
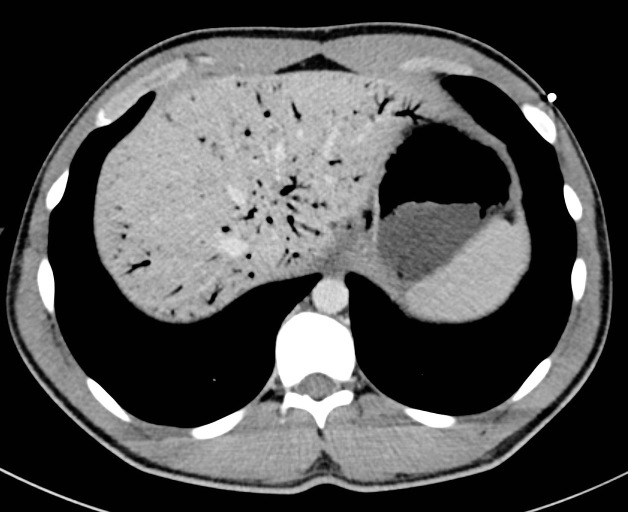
Figure 1.
Axial portal venous phase CT image showing gastric mucosal thickening with portal venous gas.
Figure 3.
Coronal portal venous phase CT image showing gastric mucosal thickening and pneumatosis with portal venous gas.
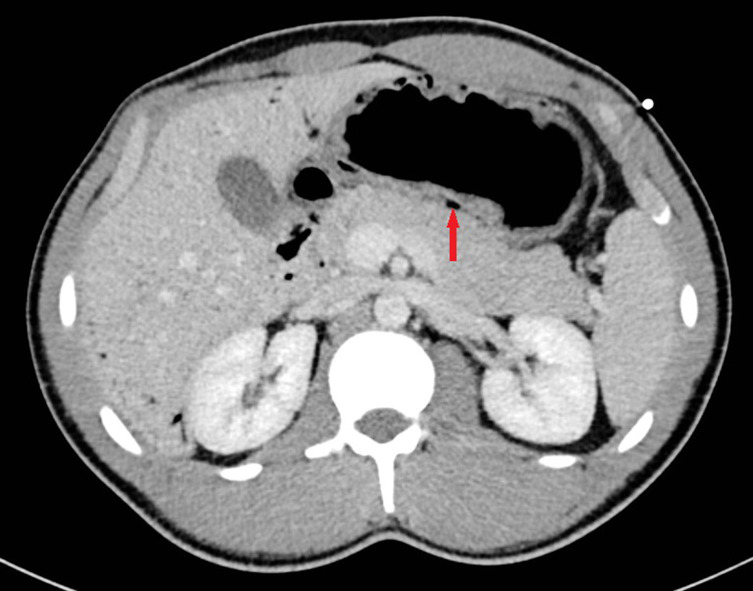
Figure 2.
Axial portal venous phase CT image showing gastric mucosal thickening and pneumatosis (arrow).
Treatment
The patient was intubated owing to concerns for developing airway involvement and gastrointestinal perforation, and conservative treatment with intravenous piperacillin/tazobactam 4.5 g four times daily and intravenous pantoprazole infusion at 8 mg hour−1 was commenced prior to transfer to a tertiary intensive care unit.
Outcome
An upper endoscopy performed 3 days after the ingestion was normal, with no evidence of mucosal injury. A repeat CT scan at this time revealed interval partial resolution of the bowel wall thickening and complete resolution of the pneumatosis and portal venous gas (Figure 4). The patient was discharged 3 days after presentation on oral pantoprazole and antibiotic therapy, and made a full recovery.
Figure 4.
Coronal CT image with intravenous and oral contrast showing interval resolution of pneumatosis and portal venous gas.
Discussion
H2O2 is an oxidizing agent that is available in concentrations ranging from 3% to 90%.1 It is found in numerous household products, including disinfectants, hair dyes, bleaches and stain removers. It is a clear, colourless liquid at room temperature,2 allowing it to be mistaken for water if unlabelled, as in this case. Recently, H2O2 has also been sold for consumption in small volumes following promotion of its purported natural health benefits,3 despite multiple documented fatalities from its ingestion2 and no evidence to demonstrate health benefits of any kind. Upon contact with the enzyme catalase in the gastric mucosa, H2O2 undergoes rapid decomposition into oxygen and water (2H2O2 → 2H2O + O2 + heat).4 If the amount of oxygen liberated exceeds the maximum solubility of blood, bubbles migrate through the epithelial interstices and gas embolism may occur, manifesting as pneumatosis3 or gas within the portal venous system,5 brain6 and coronary arteries.7 Toxicity is also caused by direct caustic injury to the gastric mucosa, resulting in gastritis and potential rupture, as well as cytotoxicity from lipid peroxidation.1 This particular case is unusual because gas embolism usually only occurs with ingestion of the stronger 35% H2O2 solution, with only a few other published case reports of portal venous gas following ingestion of the 3% solution. 8,9
Learning points
Ingestion of H2O2, a common household item, can have serious sequelae even in low volumes and concentrations.
Radiographical findings may include gastritis, pneumatosis, perforation and portal venous gas.
Contributor Information
Evyn Arnfield, Email: evyn.arnfield@uqconnect.edu.au.
Hemant Bhardwaj, Email: Hemant.bhardwaj@health.qld.gov.au.
Nicholas Brown, Email: nibrown@tpg.com.au.
Michael Handy, Email: Michael.Handy@health.qld.gov.au.
Perry Cleland, Email: Perry.Cleland@health.qld.gov.au.
References
- 1. Watt BE, Proudfoot AT, Vale JA. Hydrogen peroxide poisoning. Toxicol Rev 2004; 23: 51–7. [DOI] [PubMed] [Google Scholar]
- 2. Caraccio TR, McGuigan MA. Hydrogen peroxide In: Dart RC, Medical toxicology. 3rd edn. London, UK: Lippincott Williams & Wilkins; 2004. pp. 1253–5. [Google Scholar]
- 3. Pritchett S, Green D, Rossos P. Accidental ingestion of 35% hydrogen peroxide. Can J Gastroenterol 2007; 21: 665–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cina SJ, Downs JC, Conradi SE. Hydrogen peroxide: a source of lethal oxygen embolism. Case report and review of the literature. Am J Forensic Med Pathol 1994; 15: 44–50. [PubMed] [Google Scholar]
- 5. French LK, Horowitz BZ, McKeown NJ. Hydrogen peroxide ingestion associated with portal venous gas and treatment with hyperbaric oxygen: a case series and review of the literature. Clin Toxicol (Phila) 2010; 48: 533–8. [DOI] [PubMed] [Google Scholar]
- 6. Rider SP, Jackson SB, Rusyniak DE. Cerebral air gas embolism from concentrated hydrogen peroxide ingestion. Clin Toxicol (Phila) 2008; 46: 815–18. [DOI] [PubMed] [Google Scholar]
- 7. Islamoglu Y, Cil H, Atilgan Z, Elbey MA, Tekbas E, Yazici M. Myocardial infarction secondary to unintentional ingestion of hydrogen peroxide. Cardiol J 2012; 19: 86–8. [DOI] [PubMed] [Google Scholar]
- 8. Moon JM, Chun BJ, Min YI. Hemorrhagic gastritis and gas emboli after ingesting 3% hydrogen peroxide. J Emerg Med 2006; 30: 403–6. [DOI] [PubMed] [Google Scholar]
- 9. Tanaka Y, Yoshioka T, Kusaka T. Hydrogen peroxide ingestion: a rare case of portal venous gas. Gastrointest Endosc 2014; 79: 835–7. [DOI] [PubMed] [Google Scholar]