Abstract
Objectives:
The aim of this systematic review was to answer the focus question: “In subjects with degenerative joint disease (DJD) of the temporomandibular joint (TMJ), what is the diagnostic validity of CT or cone-beam CT (CBCT) compared with clinical protocols”?
Methods:
DJD should be assessed through clinical diagnosis according to RDC/TMD or DC/TMD. Search strategies were specifically developed to the following electronic databases: Cochrane, Latin American And Caribbean Health Sciences (LILACS), PubMed (including Medline), Scopus and Web of Science. Furthermore, partial grey literature search through Google Scholar, OpenGrey and ProQuest was performed. The risk of bias was evaluated using the second version of Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS-2).
Results:
The databases search revealed 454 records. After applying the eligibility criteria, four studies were included in this review. All studies were methodologically acceptable, although none of the them fulfilled all criteria of risk of bias according to QUADAS-2. Despite there were some high values for sensitivity and specificity, they were not homogeneous between studies. Regarding specificity outcomes, there were three studies with poor values and only one considered as excellent.
Conclusions:
CBCT could be a good image to evaluate DJD progression over time, but should not be used as a screening tool in healthy individuals.
Introduction
Temporomandibular disorder (TMD) is an umbrella term, embracing conditions which involve the temporomandibular joint (TMJ), masticatory muscles and/or associated structures.1 Disk displacement, TMJ sounds, congenital malformation, degenerative joint disease (DJD) are possible conditions affecting TMJ. DJD is characterized by deterioration and abrasion of TMJ hard and soft tissues and concomitant remodeling of the underlying subchondral bone.1 DJD has a multifactorial etiology that presents some risk factors such as age, genetics, trauma, muscle or joints disturbances, and systemic conditions.1 Clinical symptoms can include pain, joint sounds, such as crepitus, joint stiffness, and/or restriction of mandibular movement.1–3
Many efforts have been made along the past years to develop standardized criteria for TMD diagnosis. The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD), is a largely used research protocol to evaluate TMD. In 2014, a revised version has been published as the Diagnostic Criteria (DC/TMD), with the objective to be feasible for clinicians as well. In the first validation paper, TMJ imaging was optional for diagnostic, while the latter recommends it to proper evaluation.3–5
Nowadays, there are many imaging modalities to investigate TMJ, such as CT, cone-beam CT (CBCT), MRI, plain radiography, ultrasound, pantomograph (commonly named “panoramic”), arthrography, among others.5, 6 The literature is still unclear when a TMD patient should undergo a TMJ image, especially when a DJD diagnosis is proposed. There is no clear association between condyle morphology and DJD.7, 8 In addition, there is no statistical association between TMJ pain intensity and condylar severity of resorption.9
The RDC/TMD has a protocol of examination that suggests three types of images: pantomograph, MRI, and CT/CBCT. Using the RDC/TMD as the reference standard, Ahmad et al found that while CT images detected 75% of OA, MRI detected 40% and panoramic radiographs 0%.10 The use of CT/CBCT was thought to be the image reference standard to evaluate DJD.5, 11 According to the RDC/TMD, DJD is present when there is a coarse crepitus in the TMJ. If it is accompanied by self-report of pain in the TMJ region and during palpation it is considered as diagnosis IIIb, of osteoarthritis. If not, no pain in the TMJ is present, it is considered diagnosis IIIc, of osteoarthrosis. According to the DC/TMD, DJD is present when there is self-report during consultation or history of TMJ noise and examinations findings show crepitus during maximum active opening, passive opening, right lateral, left lateral or protrusive movement(s) detected by examiner. Diagnostic confirmation could be done with a CT image.4, 12
There is no systematic review in the literature that addresses the subject mentioned in vivo, which extols the scientific importance of the present study. Based on the above, the aim of this systematic review was to answer the following focus question: “In subjects with DJD, what is the diagnostic validity of CT or CBCT compared to clinical protocol”?
Methods and materials
Protocol and registration
This systematic review has followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analysis checklist (PRISMA).13 The systematic review protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42017057531.
Eligibility criteria
The studies selected in this review were those evaluating the diagnostic validity of CT and CBCT to assess DJD in subjects over 16 years old. DJD should be assessed through clinical diagnosis according RDC/TMD14 or DC/TMD.4 No sex, language or time restrictions were applied.
The following exclusion criteria were applied: (1) Studies with children or subjects under 16 years old; (2) Studies with syndromic patients; (3) Studies assessing patients with muscular TMD only or mixed TMD; (4) Studies assessing DJD in rheumatoid arthritis or juvenile idiopathic arthritis patients; (5) Studies in vitro, with animals or autopsy based; (6) Studies assessing DJD with other image rather than CT or CBCT; (7) Studies with different diagnostic protocols other than RDC/TMD or DC/TMD; (8) Studies that do not present validity measurements (sensitivity and specificity), did not present enough data to calculate them or authors could not provide them; and (9) Reviews, letters, conferences abstracts, personal opinions.
Information sources
Search strategies, appropriate truncation and word combinations were specifically developed for the following electronic database: Cochrane, Latin American And Caribbean Health Sciences (LILACS), PubMed (including Medline), Scopus and Web of Science. More information on the search strategies is provided in the online version of this article, in Supplementary Material 1(Supplementary material available online).
Furthermore, partial grey literature search through Google Scholar, OpenGrey and ProQuest was performed. Lastly, a hand-search of the references of the included studies was performed. References were managed and duplicates were removed by using EndNote® X7 (Thomson Reuters, Philadelphia, PA). Both grey literature searches and electronic database searches were conducted from their starting coverage date to October 8th, 2016. Updated search was performed on April 15th, 2017.
Study selection
The selection was completed in two phases. In phase-one, two reviewers (PBHS and DVB) independently examined the titles and abstracts of all identified electronic database citations. The studies that did not fulfill the inclusion criteria were discarded. The same 2 reviewers (PBHS and DVB) independently participated in phase-two of full-text reading. The reference lists of all included articles were critically assessed. Any disagreement in either phase was resolved by discussion and agreement. A third author (JSN) was involved when controversy arose in the process of reaching a final decision. Final selection was always based on the full-text of the publication.
Data items and data collection process
Two reviewers (PBHS and DVB) collected the required information from the included articles. The following data were collected from each article: study characteristics (authors, year of publication, country, design), population characteristics (sample size, age of participants, sex), diagnostic characteristics (RDC/TMD, DC/TMD, CT, CBCT) and outcome characteristics (findings and main conclusions). Again, any disagreement in either phase was resolved by discussion and agreement between the two reviewers. A judged author (ALP) was involved, when required, to enable formulation of the final decision. In many cases, the required data were not available, attempts were made to contact the authors by e-mail, every 2–3 days, to retrieve any pertinent unpublished information.
Risk of bias in individual studies
The methodology of selected studies was evaluated using the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS-2).15 QUADAS-2 is based on the 4-stage approach proposed by Moher et al16: (1) define the scope; (2) review the evidence base; (3) hold a face-to-face consensus meeting; and (4) refine the tool through piloting. Two reviewers (PBHS and DVB) independently scored the risk of bias as “low risk,” “high risk,” or “unclear risk.” and assess the quality of each included study. Disagreements between the two reviewers were resolved by a consensus. When they did not reach a consensus, a third author (JSN) made the final decision about each question.
Summary measures
Sensitivity and specificity of the diagnostic tests were the main outcomes evaluated. Positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), negative likelihood ratio (LR−) and diagnostic odds ratio (DOR) were secondary outcomes.
Synthesis of results
The individual results were planned to be combined by means of a meta-analysis following the appropriate Cochrane Collaboration guidelines.16, 17 Clinical, methodological, and statistical heterogeneity were explored.
Meta-analysis data may be performed using random-effect models, with restricted maximum-likelihood (REML) estimation and the DerSimonian pooled method. A random effects meta-analysis allows for differences on diagnostic measurements from study to study.
Validity measurements described in data items were transformed to draw receiver operating characteristic (ROC) curves, and forest plots with the aid of Review Manager 5.3 (RevMan 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark). Heterogeneity within studies was evaluated either by considering clinical (differences about participants, index test, and results) or methodological (design and risk of bias). A significance level of 5% was adopted.18
Results
Studies selection
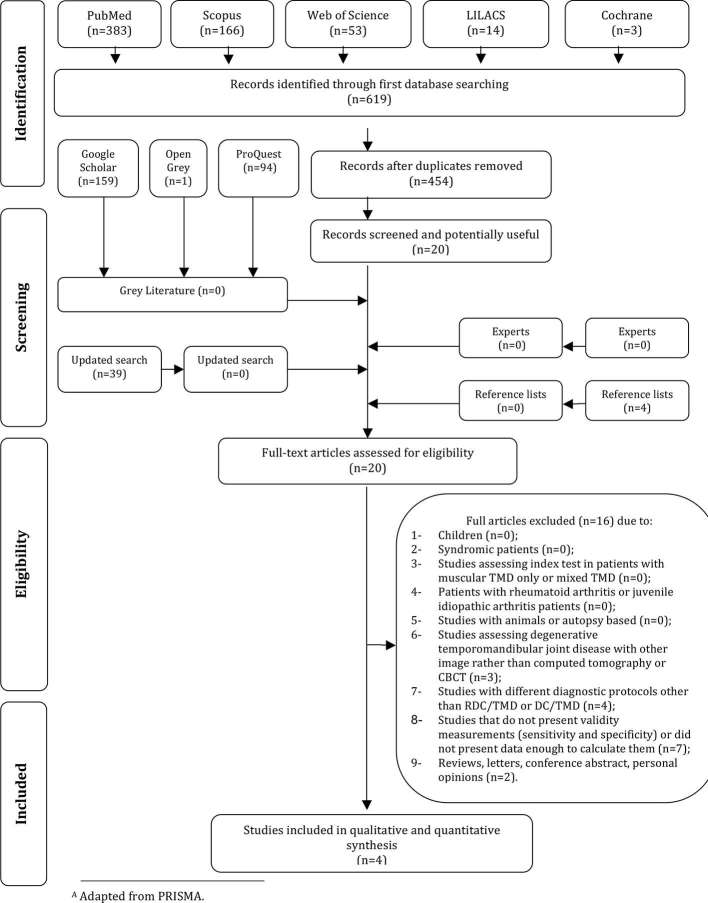
In Phase-1, the final electronic search on databases revealed 454 records after removing the duplicates. A comprehensive evaluation of titles and abstracts was performed, and 434 articles were excluded, resulting in a final number of 20 potentially useful articles. There were 254 additional studies from grey literature search, but none of these were included. Thereafter, 20 full-text articles from databases were screened according to the inclusion and exclusion criteria. The reference lists of these studies were screened, no additional studies were included. One expert suggested one article; however, it did not meet the inclusion criteria. Finally, after full-text reading, 16 studies were excluded due to multiple reasons (Supplementary Material 2) and 4 studies were included in this review. A flowchart of the process of identification, inclusion and exclusion of studies is shown in Figure 1.
Figure 1. .
Flow diagram of literature search and selection criteria.A
Study characteristics
The total sample size comprised 1224 subjects. The four selected studies were all published recently, between 201419 and 2016,20 each on a different country: Brazil,21 Korea,20 United Arab Emirates22 and USA.19 All of them have used the RDC/TMD protocol for DJD diagnosis as reference test (Groups IIIb/IIIc), three have used CBCT19, 21,22 and one CT20 as index test. Sample sizes ranged from 4521 to 103820 subjects. From the total sample size (n = 1,224), 73% were females. However, data from 508 patients (1016 TMJs) were included in the quantitative analysis, because only patients with TMJ osteoarthritis (IIIb) and osteoarthrosis (IIIc), diagnosed according to the RDC/TMD were included as study groups. Those with different diagnosis, such as I and II from RDC/TMD were not included. As control group, patients TMD symptom free,22 healthy controls19 and with arthralgia (IIIa) and/or other muscular disorders (I) or disk displacements (II) were included.20, 21 A summary of the descriptive characteristics of included articles is provided in Table 1.
Table 1.
Summary of descriptive characteristics of studies in included articles (n = 4)
| Author, year, country | Sample (n and sex) | Age in years (mean or range) | Clinical diagnosis | CT/CBCT diagnosis | CT/CBCT aquisions | Results | Conclusions |
| Cevidanes et al19, 2014, USA | 28 females (long-term TMJ OA); 12 females (initial diagnosis of OA) and 12 female controls | Long-term OA 39.39 (±16) Initial diagnosis of OA 47.4 (±16.1) Control Group 41.8 (±12.2) | OA (IIIb/IIIc) according to RDC/TMD | Morphological bone changes | CBCT: 300 axial cross-sectional slices with voxels reformatted to an isotropic 0.5 × 0.5 × 0.5 mm. Construction of surface models with ITK-SNAP 2.4 software | Agreement between RDC/TMD clinical diagnosis and CBCT was 80.4% for long term TMJ OA group; 70.8% for initial diagnosis TMJ OA group. For control group, CBCT TMJ OA diagnosis was observed in 41.7% joints | Bone resorption was more prominent at the articular surface at initial diagnosis of TMJ OA, comparing to healthy controls. A progression of bone resorption was noticed between initial and long term DJD. |
| Dias et al21, 2015, Brazil | 45 females | 43.0 (±6.2) | TMD according to RDC/TMD (Groups I, II and III) | Healthiness, planning, erosion, osteophytes and sclerosis | CBCT: i-Cat Next Generation system (Imaging Sciences International, Hatfield, PA); TV: 120 kV; TC: 3 to 8 mA; ST: 0.25 mm; ET: 26.9 | Agreement between RDC/TMD clinical diagnosis and CBCT was 100% for OA Group (III); and 100% for TMD Groups I and II | The prevalence of degenerative bone changes was high among TMJ OA patients. |
| Kim et al20, 2016, Korea | 1038 subjects (741 females/297 males) | Females: 34.0 (±16.2) Males: 31.1 (±17.4) | TMD according to RDC/TMD (Groups I, II and III) | Erosion, subcortical cyst, osteophyte, sclerosis and/or loose joint body | CT: SOMATOM Sensation 10 (Siemens, Munich, Germany) SC: 0.75 mm; TV: 120kV; TC: 100mA; RT: 19.0 s; ST: 1 mm | Agreement with RDC/TMD clinical diagnosis and CBCT was 79% for OA Group (III); and 81% for TMD Groups I and II | Arthrosis/arthritis diagnosis based on RDC/TMD shows high risk of OA changes on CT. |
| Talaat et al22, 2015, UAE | 89 subjects (56 females/33 males) | 34.0 (±21.0) | TMD according to RDC/TMD (IIb, IIc and III) | Osteophyte, flattening and irregularities of the superior surface of the condyle, cyst, joint space | CBCT: GALILEOS 3-D X-ray systems (SIRONA Dental Systems) TV: 85 kV; RT: 3 s; TC: 7 mA; ED: 75 μSv; vs : 150 µm; ST: 1 mm | Agreement with RDC/TMD clinical diagnosis and CBCT was 100% for OA Group (III); and 69.23% for TMD Groups IIb and IIc | CBCT findings are significantly associated with the clinical diagnosis of TMJ OA. Osteophytes and flattening are the most common features of OA. |
CBCT, cone beam CT; ED, effective dose; OA, osteoarthritis/osteoarthrosis; RD, radiation time; RDC/TMD, The Research Diagnostic Criteria for Temporomandibular Disorders; RT, rot time; SC, slice collimation; ST, slice thickness; TC, tube current; TMD, temporomandibular disorders; TMJ, temporomandibular joint; TV, tube voltage; UAE, United Arab Emirates; VS, voxel size; I, muscular disorders; II, disk displacement; IIa, disk displacement with reduction; IIb, disk displacement without reduction, with limited opening; IIc, disk displacement without reduction, without limited opening; III, arthralgia, arthritis, arthrosis; IIIa, arthralgia; IIIb, TMJ osteoarthritis; IIIc, TMJ osteoarthrosis.
Results of individual studies
All the selected studies used CBCT or CT scans to confirm the clinical diagnostic test, the RDC/TMD for DJD. However, they all had other results regarding more specific issues investigated. This review will focus only the results that are in accordance with the scope of this review.
Cevidanes et al19 have focused on 3D morphological evaluations and biomarkers profiles of patients with DJD. 52 patients were evaluated with CBCT scans and arthrocentesis was performed in 12 DJD patients and 12 controls. It was concluded that bone resorption of the lateral pole surface of the condyle was associated with initial phase of DJD.
Dias et al21 evaluated the presence of DJD in 45 patients with bruxism. Patients were diagnosed with or without DJD according to the RDC/TMD and underwent CBCT scans of TMJ. Although there was a high prevalence (53,1%) of DJD among bruxism patients, it was not a statistically significant association (p = 0.277).
Kim et al20 performed a retrospective study with 1038 TMD patients. Those with DJD according to the RDC/TMD underwent CT examination for diagnostic confirmation. From those 1038 patients, 354 were diagnosed with DJD, but only 237 (22.8% of the sample) had a CT scan. It was concluded that bone changes are common in young and old patients with DJD, despite these findings do not have any correlation with TMJ pain or noise.
Another study, from Talaat et al22 aimed to compare CBCT results with clinical diagnosis in 89 subjects. From those, there were 20 patients with DJD and 43 non-TMD controls. From those 40 TMJ diagnosed with DJD according to RDC/TMD criteria IIIb/IIIc, 36 had at least one degenerative change in CBCT image. It was concluded that CBCT findings are statistically associated with clinical diagnosis of DJD (p = 0.000).
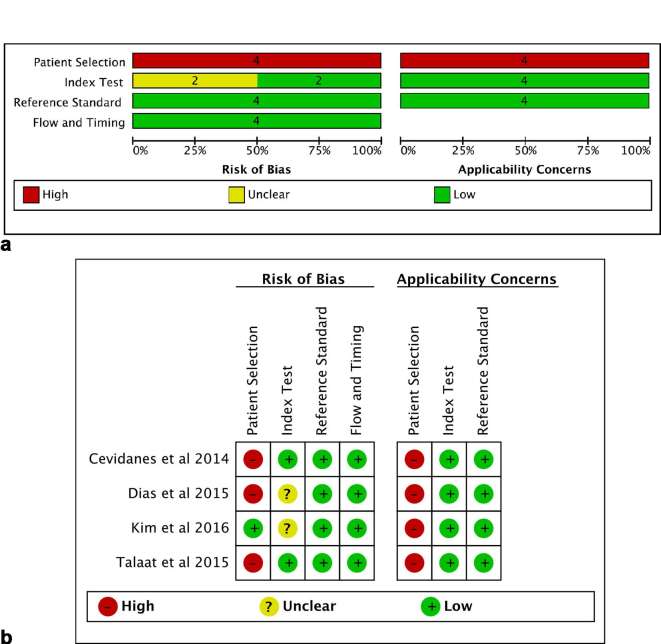
Risk of bias within studies
The complete analysis of quality assessment items list is presented in Supplementary Material 3. All studies were methodologically acceptable, although none of the them fulfilled all criteria of risk of bias according to QUADAS-2.15 The main methodological limitation of the studies was related to the poor reporting of patient selection and also because there were some concerns about applicability of results due to the fact that the selected studies were not purely diagnostic ones (domain 1). Two studies20, 21 (50%) had unclear information about the index test (domain 2). All studies showed low risk of bias in domains 3 and 4 (“reference standard” and “flow and timing”) (Figure 2).
Figure 2. .
Risk of bias and applicability concerns graph: review authors’ judgements about each domain presented as percentages across included studies. (a) Risk of bias graph; (b) risk of bias summary.
Synthesis of results
Most of data were obtained emailing the corresponding authors. Only one article19 provided full true/false positive and true/false negative variables. All data were obtained by joint, and not by patient. Sensitivity and specificity data from each article are shown in Table 2. Sensitivity rates ranged from 0.5321 to 0.90.22 Specificity rates ranged from 0.3520 to 0.93.21 Despite there were some relevant values for sensitivity and specificity, they were not homogeneous between studies. Two studies showed interesting values for sensitivity, from “good”19 to “excellent”,22 while others presented “poor” values,20, 21 according to the test indicators presented on Supplementary Material 4. Regarding specificity outcomes, there were three studies19, 20,22 with “poor” values and only one considered as “excellent”,21 which is a very discrepant result. Figure 3 presents ROC curve results. It was not possible to conclude if one study was better than another, because of the heterogeneity of the results, with a great variation between sensitivity and specificity values among the selected articles, as presented previously.
Table 2.
Prevalence, sensitivity, specificity, PPV, NPV, LR+, LR− and DOR values from each selected article
| Prevalence | True positive | False positive | False negative | True negative | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | LR+ | LR− | DOR | |
| Cevidanes et al19 | 0.76 | 62 | 10 | 18 | 14 | 78.00 | 58.00 | 73.58 | 63.73 | 1.85 | 0.37 | 4.89 |
| Dias et al21 | 0.40 | 10 | 2 | 9 | 26 | 53.00 | 93.00 | 88.33 | 66.42 | 7.57 | 0.50 | 14.98 |
| Kim et al20 b | 0.41 | 180 | 278 | 129 | 152 | 58.00 | 35.00 | 47.15 | 45.45 | 0.89 | 1.20 | 0.74 |
| Talaat et al22 | 0.31 | 36 | 31 | 4 | 55 | 90.00 | 64.00 | 71.42 | 86.48 | 2.50 | 0.15 | 16.00 |
DOR, diagnostic odds ratio; LR, likelihood ratio; NPV, negative predicative value; PPV, positive predicative value.
studies using CBCT.
study using CT.
Figure 3. .
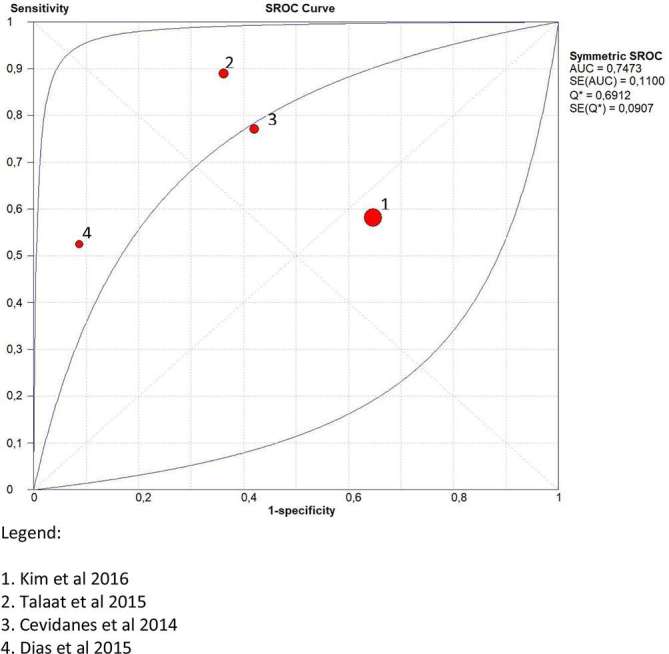
ROC curves representing the diagnostic accuracy of CT/CBCT for each study. CBCT, cone-beam CT; ROC, receiver operating characteristic.
As secondary outcomes, LR+, LR− e DOR values were obtained for each selected study, as shown in Table 2. Dias et al21 presented the best LR + value, of 7.57, considering CBCT a good diagnostic test. On the other hand, the study from Kim et al20 had the worst LR + value, of 0.89 for CT images.
Risk of bias across studies
A methodological limitation of the studies selected was related to the interpretation of index test results. In two studies20, 21 it was unclear whether the examiner’s interpretation of TMJ images could have introduced bias to the results. For example, if images examiner was aware of patient’s clinical diagnosis prior to image analysis and/or if the patient examiner was the same image examiner. A limitation across studies was related to poor reporting of sensitivity and specificity data. To get sufficient information for this review, it was necessary to contact the corresponding authors of three20–22 of the selected studies. It is important to declare that none of the selected studies had as main objective to evaluate the diagnostic validity of TMJ images for DJD. Instead, they aimed to evaluate the incidence or prevalence of TMJ bony changes in osteoarthritic joints.
Discussion
The scope of this systematic review was to evaluate the diagnostic validity of CT or CBCT, which are the image reference standards,10 in subjects older than 16 years old compared with clinical examination protocols from RDC/TMD and DC/TMD to evaluate TMJ degenerative disorder. We found four studies which met all eligibility criteria. Sensitivity and specificity values were mainly obtained directly with corresponding author. The results from this systematic review have shown a great variation between values, which reflects the lack of a standardized protocol to evaluate the TMJ through images.
In 2009, Ahmad et al10 have developed an image analysis criteria and examiner reliability for image analysis combined to RDC/TMD diagnosis of DJD. From the four included studies, only two20, 21 seemed to have used this mentioned methodology to classify the bone surfaces of mandibular condyle and articular eminence. Curiously, those were the studies with the worst sensitivity results, for CT and CBCT respectively. As they had used established criteria for imaging evaluation, we could say that their results are the most reliable, once this measure is for diagnostic accuracy.
Although TMJ images may play an important role in the diagnostic process,5 it is not consensual when a patient should undergo an imaging procedure, specially a CT or a CBCT, which have radiation safety concerns. There has been an overuse of TMJ imaging which has led to the critical thinking of which modality and when to use an image as a diagnostic tool. According to Hussain et al23 an image should be ordered considering history, clinical signs and symptoms. De Boer et al24 have evaluated the value of CBCT in clinical decision-making in 128 patients with TMD. About 58% of them had their diagnosis and management changed after the CBCT examination, which is a good reason justifying the image. Radiological examination should be considered just if it will add information to the therapy planning.5
For many years, scientific research has dealt with the difficulty to compare results from TMD patients studies due to the lack of a clinical diagnostic protocol. After the RDC/TMD and more recently DC/TMD publication, it has been easier, but not completely solved, because there still are many studies not using these instruments. In our search, from 16 excluded studies, 25% were due to the different diagnostic protocols other than RDC/TMD or DC/TMD. These instruments were established to standardize TMD diagnosis and present values for sensitivity and specificity for each diagnostic modality. As an example, DC/TMD sensitivity and specificity values for degenerative joint disease are 55 and 61%, respectively.12 Similar sensitivity results were found by two studies, 5321 and 58%;20 these same two studies mentioned were the only ones that have used a diagnostic criteria10 to evaluate TMJ images. However, it is worth to mention that solely the study performed by Kim et al20 has used CT as reference test, while Dias et al21 has used CBCT.
Regarding specificity results, similar values with DC/TMD were presented by other two studies showing 5825 and 64%.22 Unlike DC/TMD, both studies have used CBCT as reference test, which can compromise and make the comparison of these specific results unfeasible to the point where some conclusion can be drawn about the use of CT or CBCT for diagnosing DJD. Meanwhile, the use of CT and CBCT benefits immensely in the diagnosis of TMD.
The sensitivity and specificity results of the present study were hard to compare with other published studies, there is a lack of specific information in the literature. Researchers need very well established criteria to sample selection to provide reliable information for clinicians. Investigators should also be experienced and calibrated, and image examiner should be blinded for clinical diagnosis. An interesting comparison could be made with the results from Paveda-Roda et al26 that evaluated the diagnostic validity of panoramic X-rays compared to the use of MRI and RDC/TMD. When using clinical index as reference standard, the authors found a sensitivity of 61.6% and specificity of 57.9% when the analysis was made per joint. These values are not so different than those obtained in this systematic review neither from those from the clinical index DC/TMD.12 This comparison should contribute to the indication of the clinical index as the best cost-effective way of diagnosing DJD once the clinical index has no radiation exposure and is less expensive to the patient.
An impeccable diagnostic procedure has the potential to completely discriminate subjects with and without disease. Unfortunately, such perfect test does not exist in “real life” and therefore, diagnostic procedures can only make partial distinction between subjects with and without disease. Even though, the diagnostic efficacy of CBCT in the detection of morphologic changes of the osseous components of the TMJs has been found to be very good,22, 27,28 indicating its use for long-term patient follow-up. A recent systematic review with ex vivo studies, has found pooled sensitivity and specificity results of 67 and 87%, respectively.28 Those are higher values when compared to those from the present study; however autopsy-based researches do not consider the clinical diagnosis as an inclusion criteria. So, this may lead to results that must be interpreted as CBCT being a good tool for viewing TMJ osseous changes, but not to be used as the only diagnostic method.
The present results had shown that the study from Tallat et al22 had the best sensitivity result, which is an indication of a good diagnostic tool to those who have the disease. While the study from Dias et al21 was the best to diagnose healthy individuals, due to the best specificity results.
Overall, there is poor agreement between expected and actual radiographic findings.29 There is a poor correlation between the presence of clinical TMJ signs and symptoms with the presence of osseous changes in a TMJ image.9, 30,31 This is in agreement with the findings of the present systematic review when we consider the high false positive values found. Representing a scenario where the patient has a positive image, compatible with DJD, however, does not present any clinical sign or symptom of disease.
Results show that the study from Kim et al20 had poor sensibility and specificity values, pointing out that CT should not be the first-choice image examination to diagnose DJD. Besides the fact that the amount of radiation is not justifiable for the benefits in the diagnosis, it is worth to mention that this was the only study that evaluated DJD through CT and not CBCT. Sensibility values found by Tallat et al22 and Cevidanes et al25 may also indicate the preferred use of CBCT for diagnosing DJD. CBCT shows a high capacity of detecting bone abnormalities in TMJ, but its accuracy is comparable with CT, and varies among studies. It is not consensual in the literature whether CBCT provides TMJ images with better quality,11 which could consequently improve the sensitivity and specificity values of this diagnostic test. Another possible influence on the results of this study is the calibration and blinding of examiners. Also, results may not indicate the use of CT as a diagnostic tool for DJD, because the test cannot be considered a good indicative of disease. LR-values had shown a poor contribution of CT and CBCT to ruling-out the diagnosis. Exception is made for one study,22 which presented a 0.18 LR-value. Regarding DOR, the study from Talaat et al22 had the higher value of 16.00. The study from Dias et al21 had shown a DOR value of 14.98. This could be an indicative that CBCT may have some diagnostic accuracy for DJD. On the other hand, the results from another study discourage this statement, with a DOR value of 4.79.25 Further, the study from Kim et al20 have shown such a low DOR value, of 0.74, pointing to an improper test interpretation, not considering CT an accurate tool.
The use of CBCT is indicated to evaluate DJD, but mostly because it has a better cost-benefit and less radiation dose when compared to CT.5, 11,23,32 Depending on the scanner, CBCT has an effective dose radiation exposure ranging from 7.3 to 288.9 μSv while a conventional CT ranges from 1320 to 1400 μSv, depending on the protocol used.32 On this aspect, some other authors are investigating the ultrasound applicability on TMJ evaluation, it could be a radiation-free option.23, 33 Also, a systematic review performed in 2008 have pointed out that a combination of different TMJ images is indicated for better accuracy for diagnosing erosions and osteophytes.23
In this systematic review, some limitations should be mentioned. The literature in general lacks studies that use radiation, which makes difficult the accomplishment of such systematic reviews. Also, when a diagnostic test is performed, ideally the control group should be comprised of real healthy individuals. Only one19 of the selected studies had a healthy control group. This situation, added to the disparity in sample sizes, may have led to such variation in sensitivity and specificity results. In addition, we detected a sample selection bias among included studies due to patient recruitment/selection,19 the retrospective design,20 and the fact that patients were referred for treatment at a TMD and facial pain service.21, 22 Another limitation of the present study is that it was not made a distinction between gender in the results. Once our sample was 70% of females and it is known that DJD is more prevalent in females,30 it may have also introduced some bias, so they should be carefully interpreted.
Conclusion
CBCT could be a good image examination to evaluate DJD progression over time, but should not be used as a screening tool in healthy individuals, because of its poor specificity results.
Contributor Information
Priscila Brenner Hilgenberg-Sydney, Email: priscilabhs@me.com.
Danielle Veiga Bonotto, Email: danidaniveiga@gmail.com.
José Stechman-Neto, Email: consultorioatm@gmail.com.
Liete Figueiredo Zwir, Email: lfzwir@gmail.com.
Camila Pachêco-Pereira, Email: cppereir@ualberta.ca.
Graziela De Luca Canto, Email: delucacanto@gmail.com.
André Luís Porporatti, Email: andreporporatti@yahoo.com.br.
REFERENCES
- 1.de Leeuw R, Klasser GD. Orofacial pain: guidelines for assessment, diagnosis and management. 5th ed Hanover Park, IL: The British Institute of Radiology.; 2013. 312. [Google Scholar]
- 2.Kalladka M, Quek S, Heir G, Eliav E, Mupparapu M, Viswanath A. Temporomandibular joint osteoarthritis: diagnosis and long-term conservative management: a topic review. J Indian Prosthodont Soc 2014; 14: 6–15. doi: 10.1007/s13191-013-0321-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301–55. [PubMed] [Google Scholar]
- 4.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network* and orofacial pain special interest group†. J Oral Facial Pain Headache 2014; 28: 6–27. doi: https://doi.org/10.11607/jop.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersson A. What you can and cannot see in TMJ imaging-an overview related to the RDC/TMD diagnostic system. J Oral Rehabil 2010; 37: 771–8. doi: 10.1111/j.1365-2842.2010.02108.x [DOI] [PubMed] [Google Scholar]
- 6.Bag AK, Gaddikeri S, Singhal A, Hardin S, Tran BD, Medina JA, et al. Imaging of the temporomandibular joint: an update. World J Radiol 2014; 6: 567–82. doi: 10.4329/wjr.v6.i8.567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Ekrish AA, Al-Juhani HO, Alhaidari RI, Alfaleh WM. Comparative study of the prevalence of temporomandibular joint osteoarthritic changes in cone beam computed tomograms of patients with or without temporomandibular disorder. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 120: 78–85. doi: 10.1016/j.oooo.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 8.Cömert Kiliç S, Kiliç N, Sümbüllü MA. Temporomandibular joint osteoarthritis: cone beam computed tomography findings, clinical features, and correlations. Int J Oral Maxillofac Surg 2015; 44: 1268–74. doi: 10.1016/j.ijom.2015.06.023 [DOI] [PubMed] [Google Scholar]
- 9.Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 110–7. doi: 10.1016/j.tripleo.2010.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 844–60. doi: 10.1016/j.tripleo.2009.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol 2015; 44: 20140235. doi: 10.1259/dmfr.20140235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schiffman E, Ohrbach R. Executive summary of the diagnostic criteria for temporomandibular disorders for clinical and research applications. J Am Dent Assoc 2016; 147: 438–45. doi: 10.1016/j.adaj.2016.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–9. doi: 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 14.Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W, et al. The research diagnostic criteria for temporomandibular disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 2010; 24: 63–78. [PMC free article] [PubMed] [Google Scholar]
- 15.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–36. doi: 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Schulz KF, Simera I, Altman DG. Guidance for developers of health research reporting guidelines. PLoS Med 2010; 7: e1000217. doi: 10.1371/journal.pmed.1000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y. Chapter 10: analysing and presenting results : Deeks JJ, Bossuyt PM, Gatsonis C, Cochrane handbook for systematic reviews of diagnostic test accuracy version 1 0. The British Institute of Radiology.; 2010. 1–61. [Google Scholar]
- 18.Bossuyt P, Davenport C, Deeks J, Hyde C, Leeflang M, Scholten R. Chapter 11: interpreting results and drawing conclusions : Deeks JJ, Bossuyt PM, Gatsonis C, Cochrane handbook for systematic reviews of diagnostic test accuracy version 0 9. The British Institute of Radiology.; 2013. 1–31. [Google Scholar]
- 19.Cevidanes LH, Walker D, Schilling J, Sugai J, Giannobile W, Paniagua B, et al. 3D osteoarthritic changes in TMJ condylar morphology correlates with specific systemic and local biomarkers of disease. Osteoarthritis Cartilage 2014; 22: 1657–67. doi: 10.1016/j.joca.2014.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim K, Wojczyńska A, Lee JY. The incidence of osteoarthritic change on computed tomography of Korean temporomandibular disorder patients diagnosed by RDC/TMD; a retrospective study. Acta Odontol Scand 2016; 74: 337–42. doi: 10.3109/00016357.2015.1136678 [DOI] [PubMed] [Google Scholar]
- 21.Dias GM, Bonato LL, Guimarães JP, Silva JN, Ferreira LA, Grossmann E, et al. A study of the association between sleep bruxism, low quality of sleep, and degenerative changes of the temporomandibular joint. J Craniofac Surg 2015; 26: 2347–50. doi: 10.1097/SCS.0000000000002084 [DOI] [PubMed] [Google Scholar]
- 22.Talaat W, Al Bayatti S, Al Kawas S. CBCT analysis of bony changes associated with temporomandibular disorders. Cranio 2015; 34: 88–94. doi: 10.1179/2151090315Y.0000000002 [DOI] [PubMed] [Google Scholar]
- 23.Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol 2008; 37: 63–71. doi: 10.1259/dmfr/16932758 [DOI] [PubMed] [Google Scholar]
- 24.de Boer EW, Dijkstra PU, Stegenga B, de Bont LG, Spijkervet FK. Value of cone-beam computed tomography in the process of diagnosis and management of disorders of the temporomandibular joint. Br J Oral Maxillofac Surg 2014; 52: 241–6. doi: 10.1016/j.bjoms.2013.12.007 [DOI] [PubMed] [Google Scholar]
- 25.Cevidanes LH, Walker D, Schilling J, Sugai J, Giannobile W, Paniagua B, et al. 3D osteoarthritic changes in TMJ condylar morphology correlates with specific systemic and local biomarkers of disease. Osteoarthritis Cartilage 2014; 22: 1657–67. doi: 10.1016/j.joca.2014.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poveda-Roda R, Bagan J, Carbonell E, Margaix M. Diagnostic validity (sensitivity and specificity) of panoramic X-rays in osteoarthrosis of the temporomandibular joint. Cranio 2015; 33: 189–94. doi: 10.1179/2151090314Y.0000000018 [DOI] [PubMed] [Google Scholar]
- 27.Gomes LR, Gomes M, Jung B, Paniagua B, Ruellas AC, Gonçalves JR, et al. Diagnostic index of three-dimensional osteoarthritic changes in temporomandibular joint condylar morphology. J Med Imaging 2015; 2: 034501. doi: 10.1117/1.JMI.2.3.034501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma RH, Yin S, Li G. The detection accuracy of cone beam CT for osseous defects of the temporomandibular joint: a systematic review and meta-analysis. Sci Rep 2016; 6: 34714. doi: 10.1038/srep34714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiese M, Wenzel A, Hintze H, Petersson A, Knutsson K, Bakke M, et al. Osseous changes and condyle position in TMJ tomograms: impact of RDC/TMD clinical diagnoses on agreement between expected and actual findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: e52–e63. doi: 10.1016/j.tripleo.2008.03.021 [DOI] [PubMed] [Google Scholar]
- 30.dos Anjos Pontual ML, Freire JS, Barbosa JM, Frazão MA, dos Anjos Pontual A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac Radiol 2012; 41: 24–9. doi: 10.1259/dmfr/17815139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palconet G, Ludlow JB, Tyndall DA, Lim PF. Correlating cone beam CT results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac Radiol 2012; 41: 126–30. doi: 10.1259/dmfr/60489374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007; 40: 818–30. doi: 10.1111/j.1365-2591.2007.01299.x [DOI] [PubMed] [Google Scholar]
- 33.Hechler BL, Phero JA, Van Mater H, Matthews NS. Ultrasound versus magnetic resonance imaging of the temporomandibular joint in juvenile idiopathic arthritis: a systematic review. Int J Oral Maxillofac Surg 2018; 47: 83–9. doi: 10.1016/j.ijom.2017.07.014 [DOI] [PubMed] [Google Scholar]