Abstract
Objective:
Although it is well established that neuroticism increases the risk of posttraumatic stress disorder (PTSD), little is known about the mechanisms that promote PTSD in individuals with elevated levels of neuroticism. Across two studies, we examined the cognitive-affective processes through which neuroticism leads to greater PTSD symptom severity.
Method:
Community-dwelling adults with trauma histories varying widely in severity (Study 1) and clinically-diagnosed individuals exposed to DSM-IV-TR A1 criterion traumas (Study 2) completed measures of neuroticism, negative affectivity, trauma memory characteristics, and PTSD symptom severity.
Results:
Longitudinal data in Study 1 showed that individuals with higher scores on two measures of neuroticism assessed approximately three decades apart in young adulthood and midlife reported trauma memories accompanied by more intense physiological reactions, more frequent involuntary rehearsal, and greater perceived centrality to identity in older adulthood. These properties of trauma memories were in turn associated with more severe PTSD symptoms. Study 2 replicated these findings using cross-sectional data from individuals with severe trauma histories and three additional measures of neuroticism.
Conclusions:
Results suggest that neuroticism leads to PTSD symptoms by magnifying the emotionality, availability, and centrality of trauma memories as proposed in mnemonic models of PTSD.
Keywords: neuroticism, posttraumatic stress disorder, autobiographical memory, phenomenology, centrality
One consistent finding that emerges from research on personality is that neuroticism, a temperamental disposition characterized by negative affect and persistent beliefs that the world is threatening and dangerous, is the personality trait most often associated with many forms of psychopathology, including posttraumatic stress disorder (PTSD). Robust correlations have been reported between neuroticism and PTSD symptom severity across a broad range of populations, including clinical and nonclinical samples, younger and older adults, and individuals with histories of civilian and military trauma (Breslau & Schultz, 2013; Cox, MacPherson, Enns, & McWilliams, 2004; Davidson, Kudler, & Smith, 1987; Engelhard & van den Hout, 2009; Lauterbach & Vrana, 2001; Parslow, Jorm, & Christensen, 2006; Rubin, Berntsen, & Bohni, 2008; Rubin, Boals, & Berntsen, 2008; Rubin, Dennis, & Beckham, 2011; Rubin, Hoyle, & Leary, 2012; van Zelst et al., 2003). Despite the strength of empirical evidence indicating that neuroticism is a reliable predictor of PTSD diagnosis and symptom severity, the specific processes through which neuroticism leads to greater PTSD symptom severity remain understudied. The purpose of the present investigation was to identify the mechanisms through which neuroticism contributes to posttraumatic stress reactions. Specifically, we examined the extent to which neuroticism leads to elevated PTSD symptom severity through its influence on particular properties of trauma memories associated with PTSD symptoms. These phenomenological properties include the emotionality of the trauma memory as measured by ratings of cognitive and visceral aspects of emotional intensity, the frequency of trauma memory rehearsal as measured by reports of how often the memory is voluntarily and involuntarily recalled, and the perceived centrality of the trauma memory to identity.
Empirical support for the hypothesis that neuroticism contributes to PTSD by increasing the emotionality, rehearsal, and centrality of memories for traumatic events is drawn from research on individual differences in the phenomenology of autobiographical memory. Studies show that individuals with higher levels of neuroticism rate their autobiographical memories as more emotionally and viscerally intense, more frequently voluntarily and involuntarily rehearsed, and more central to identity (Rubin et al., 2011; Rubin, Boals, & Hoyle, 2014; Sutin, 2008). For instance, in a study of the phenomenological characteristics of self-defining autobiographical memories, undergraduates with higher neuroticism scores rated their self-defining memories as more emotionally intense (Sutin, 2008). Similar results were reported in a study of community-dwelling adults who rated their most-important, most-stressful, most-positive, and word-cued autobiographical memories on various phenomenological properties, including their sensory, language, and metacognitive characteristics (Rubin et al., 2011). Higher neuroticism scores were associated with ratings of greater emotional intensity, as well as more intense physiological reactions and more frequent voluntary and involuntary rehearsal when each participant’s ratings were averaged across all memory types. Likewise, Rubin et al. (2014) found that higher levels of neuroticism were consistently associated with greater ratings of the centrality of a trauma memory to one’s identity and life story across three diverse military and undergraduate samples , 5 measures of neuroticism and the related personality construct of negative affectivity, and two measures of trauma centrality. In general, the results of these three studies examining the influence of personality on the phenomenological characteristics of autobiographical memories are congruent with findings from the broader personality literature in which individuals with higher neuroticism have been found to exhibit stronger negative reactions to stress (Bolger & Zuckerman, 1995), more frequent rumination (Roelofs, Huibers, Peeters, Arntz, & van Os, 2008), and increased access to emotionally negative self-relevant information (Martin, 1985; Teasdale & Green, 2004).
Our focus on the emotionality, rehearsal, and centrality of trauma memories as the primary mechanisms through which neuroticism leads to PTSD symptoms is also supported by extensive theoretical and empirical work showing that these three properties of trauma memories predict PTSD symptoms and increase as a function of greater symptom severity (e.g., Berntsen, Rubin, & Salgado, 2015; Berntsen, Willert, & Rubin, 2003; Rubin, Boals, & Berntsen, 2008; Rubin, Feldman, & Beckham, 2004; Rubin et al., 2011; Rubin et al., 2014; Thomsen & Berntsen, 2008). Research on a wide variety of participant samples and trauma types indicates that individuals with PTSD diagnoses or elevated PTSD symptoms rate their most stressful and traumatic memories higher on measures of emotionality, rehearsal, and centrality compared to individuals without PTSD or with low symptom levels (Berntsen et al., 2003; Kleim, Graham, Bryant, & Ehlers, 2013; Rubin et al., 2003; Rubin, Boals, & Berntsen, 2008; Rubin et al., 2011). These studies also show that individuals with PTSD report higher levels of emotionality, rehearsal, and centrality for nontrauma-related memories, including their word-cued, most important, and most positive autobiographical memories, compared to individuals without PTSD. The finding that increases in emotionality, rehearsal, and centrality are observed not only for negative and stressful memories, but across a broad range of memory types in individuals with PTSD suggests that this particular pattern of responding is reflective of a general affective style that may predispose individuals to develop and maintain PTSD symptoms when exposed to a traumatic event.
The strength and consistency of findings generated over the last decade concerning the relation between trauma memory characteristics and PTSD symptom severity lead to the formulation of a mnemonic theory of PTSD, called the Autobiographical Memory Theory of PTSD (AMT; Rubin, Boals, & Berntsen, 2008). According to the AMT, PTSD symptoms arise through cognitive-affective processes that enhance the availability of the trauma memory. The specific memory availability processes that combine to promote PTSD symptoms according to the AMT are the emotional intensity of the trauma memory, the frequency of memory retrieval, and the centrality of the trauma memory to one’s life story and identity. Furthermore, the AMT proposes that individuals with different personality traits vary in their levels of these cognitive-affective processes. Although empirical support for the memory availability mechanisms of the AMT has been well documented in studies demonstrating that the phenomenological properties and perceived centrality of trauma memories correlate highly with PTSD symptom severity, little work has been devoted to examining how these cognitive-affective processes integrate with characteristics of the individual to explain PTSD symptom severity. Given the substantial heterogeneity in symptom severity observed among individuals exposed to the same event (David et al., 2006; Dyb et al., 2014; Orcutt, Bonanno, Hannan, & Miron, 2014), an integrative approach that combines factors viewed as stable characteristics of the individual (e.g., personality) with cognitive-affective processes that are viewed as reactions to traumatic events (e.g., memory characteristics, appraisals of event centrality) may be needed to understand the myriad complex factors involved in PTSD. As a test of the mediating processes described in the AMT, in the present study we examined for the first time how the cognitive-affective processes proposed by the AMT integrate with characteristics of the individual to predict PTSD symptom severity. Specifically, we investigated the extent to which neuroticism increases the emotionality, rehearsal, and centrality of memories for traumatic life events, which in turn leads to greater PTSD symptom severity.
In our investigation of this hypothesis, we first examined longitudinal data from a large sample of community-dwelling adults exposed to a range of negative and potentially traumatic events that vary widely in severity (Study 1). We then tested whether our findings replicated in a sample of clinically diagnosed individuals with histories of exposure to trauma severe enough to qualify for a potential diagnosis of PTSD (Study 2). To examine whether our results generalize to more than one measure of neurotic traits, in each study we report findings for multiple measures of neuroticism (Studies 1 and 2) and the related personality construct of negative affectivity (Study 2).
Study 1
The purpose of Study 1 was to test the mediating processes proposed by the AMT using longitudinal data from a nonclinical sample of adults with histories of potentially traumatic events ranging broadly in severity. Specifically, we examined the extent to which higher levels of neuroticism prospectively predict greater emotionality, rehearsal, and centrality of trauma memories, and whether these properties of trauma memories were in turn associated with more severe PTSD symptoms. To help ensure that our findings were not unique to a particular personality assessment, we examined neuroticism scores from two well validated personality instruments: the Minnesota Multiphasic Personality Inventory (MMPI) and the NEO Personality Inventory (NEO-PI). The MMPI and the NEO-PI were completed approximately 45 and 18 years prior to participant reports of traumatic life events and PTSD symptoms, which prevented neuroticism levels from being influenced by concurrent symptom reporting. The first two memory availability mechanisms of the AMT were measured using questions from the Autobiographical Memory Questionnaire (AMQ; Rubin, Schrauf, & Greenberg, 2003, 2004), which asks participants to rate properties of their autobiographical memories as the memories are being recalled. This procedure produces a more valid assessment of the ongoing processes than traditional retrospective reports (Ericsson & Simon, 1993). Emotionality was indexed by the AMQ measures of emotional intensity and physiological reaction, rehearsal was indexed by the AMQ measures of voluntary rehearsal and involuntary recall, and event centrality was assessed by a standardized measure of the centrality of a memory to one’s identity and sense of self, called the Centrality of Events Scale (CES; Berntsen & Rubin, 2006, 2007). Components of the CES include the extent to which the event is a core part of a person’s identity, influences interpretations of new experiences, and signals a major turning point in one’s life story.
Based on results from cross-sectional studies in which strong correlations were found between neuroticism and participant ratings of the phenomenological properties of their trauma memories (Rubin, Boals, & Berntsen, 2008; Rubin et al., 2011), we hypothesized that higher levels of MMPI and NEO neuroticism would prospectively predict trauma memories accompanied by greater emotional and physiological intensity, more frequent voluntary and involuntary recall, and greater centrality to the life story. These properties of the trauma memories were in turn expected to be related to greater PTSD symptom severity, consistent with studies showing that measures of emotionality, rehearsal, and importance to the life story increase with PTSD symptom severity.
Method
Participants and Procedure
Data were drawn from the University of North Carolina Alumni Heart Study (UNCAHS), a longitudinal mail survey study of students who entered the University of North Carolina, Chapel Hill in 1964–1966 and their spouses (Siegler et al., 1992). The recruitment procedures, participation rates, and measures of the UNCAHS are detailed elsewhere (Hooker, Hoppmann, & Siegler, 2010) and briefly described here. The UNCAHS was originally designed to examine personality as a predictor of coronary heart disease (CHD). At wave 12, the study was expanded to include measures of PTSD and lifetime trauma exposure to investigate the relations between CHD and PTSD in a non-clinical sample. A second measure of PTSD symptoms and assessments of the phenomenological properties of trauma memories were added at wave 13 (2011–2013). With 13 points of data collection now complete, the UNCAHS contains an extensive archive of data concerning personality, well-being, and disease outcomes.
All waves of the UNCAHS were approved by the Duke University Medical Center institutional review board. On the wave 13 questionnaire participants were asked to describe three traumatic events that currently bothered them most and to select a category that best described each traumatic event from the list of events included in the Traumatic Life Events Questionnaire (TLEQ, Kubany et al., 2000), a standardized broad-spectrum measure of life events demonstrated to be capable of producing PTSD symptoms according to DSM-IV-TR criteria. For each of the three traumatic events, participants completed measures of PTSD symptoms, phenomenological properties of the trauma memory, and event centrality. Ratings for the traumatic event with the most severe PTSD symptoms were included in our analyses.
Our analyses included the 1,106 respondents (71.31% of wave 13 respondents) who reported at least one potentially traumatic life event and completed measures of PTSD symptom severity, phenomenological properties of trauma memories, and event centrality at wave 13, as well as the NEO previously during the study. A subset (n = 802) also completed the MMPI upon college entry (M age = 18.28, SD = 1.69) and were included in analyses of MMPI neuroticism scores. The analysis sample was 61.30% male, with a mean age of 63.49 (SD = 2.74), and an average annual household income of $70–99,999. The sample was predominantly Caucasian (99.37%). Four participants were African American (.36%), one American Indian (.09%), one Hispanic (.09%), and one (.09%) declined to report their ethnicity. Approximately 8% had less than a college degree, 20% had Bachelor’s degrees, 21% had Bachelor’s degrees plus additional training, 29% had Master’s degrees, and 23% had advanced degrees. Analyses comparing UNCAHS respondents in the analysis sample to wave 13 respondents who were excluded due to missing data indicated that the analysis sample was slightly more educated, reported higher annual household income, and included a greater proportion of females ( s ≤ .01).
Measures
Autobiographical Memory Questionnaire (AMQ).
The AMQ (Rubin et al., 2003, 2004) measures the processes involved in remembering an event. We analyzed 4 AMQ items relevant to the AMT and that correlate consistently with PTSD symptom severity (Rubin, Boals, & Berntsen, 2008; Rubin et al., 2011; Thomsen & Berntsen, 2008), including emotional intensity (“While remembering the event, the emotions that I feel are extremely intense”), physiological reaction (“While remembering the event, I had a physical reaction: laughed, felt tense, felt sweaty, felt cramps or butterflies in my stomach, my heart pounded or raced, etc.”), voluntary rehearsal (“Since it happened, I have willfully thought back to the event in my mind and thought about it or talked about it”), and involuntary recall (“Has the memory of the event suddenly popped in your thoughts by itself – that is, without having attempted to remember it?”).
Centrality of Event Scale (CES).
The CES (Berntsen & Rubin, 2006) assesses the extent to which a trauma forms a central component of personal identity, a turning point in the life story, and a reference point for everyday inferences. Items are rated on 5-point scales (1 = totally disagree, 5 = totally agree). The 7-item short form of the scale was administered. Mean scores are reported. Cronbach’s alpha in the present study was .90.
NEO Personality Inventory (NEO-PI).
The 240 item NEO-PI (Costa & McCrae, 1992) was administered twice during midlife in the UNCAHS (Costa Herbst, McCrae, & Siegler, 2000). Average neuroticism domain scores were analyzed. Raw scores were converted to t-scores based on adult combined-sex norms. The NEO-PI has strong psychometric properties (Cronbach’s α = .92) and is well validated (Costa & McCrae, 1992). In the UNCAHS, internal consistency for the domain scales ranges from .76 to .93.
Minnesota Multiphasic Personality Inventory (MMPI).
Factor-analyzed neuroticism scores derived from the MMPI (Costa, Zonderman, McCrae, & Williams, 1985; Siegler, Zonderman, Barefoot, Williams, Costa, & McCrae, 1990) were included. The neuroticism factor has high internal consistency (Cronbach’s α = .92).
PTSD Check List - Stressor Specific Version (PCL-S).
The PCL-S (Weathers, Litz, Huska, & Keane, 1994) is a 17-item measure of PTSD symptoms in reference to a specific event. Using 5-point scales (1 = not at all, 5 = extremely), respondents indicate the extent to which a specific event produced each of the B, C, and D DSM-IV-TR symptoms of PTSD during the previous month. The PCL has strong psychometric properties (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996) and has high diagnostic agreement with diagnoses determined by clinical interviews (r = .93; Blake et al., 1990). In civilian samples, a PCL cut score for probable PTSD is between 30–35 (U.S. Department of Veterans Affairs, 2014). Approximately 28% of the current sample had PCL scores of 35 or higher.
Data Analysis
Parallel multiple mediator models using a bias-corrected bootstrapping procedure (Preacher & Hayes, 2008) were tested to examine the extent to which neuroticism leads to greater PTSD symptom severity indirectly through increases in the emotionality, rehearsal, and centrality of trauma memories. Parallel multiple mediator models were selected as the analytic method because they simultaneously test the indirect effects of each mediator while accounting for the shared association between them. This statistical procedure is recommended over other methods of testing indirect effects (e.g., Sobel test) when more than one mediator is predicted to influence the dependent variable because it increases the precision and parsimony of the model without assuming multivariate normality of the distribution of indirect effects (Hayes, 2013). Point estimates and 95% bias-corrected confidence intervals (BC CI) were generated using 10,000 bootstrap samples. Indirect effects are significant when the BC CI does not include zero.
Results
The events included in the analyses represented a wide range of potentially traumatic events assessed by the TLEQ. Prevalence rates were highest for unexpected death of a loved one (23.51%), followed by life-threatening personal illness (9.67%), life threatening or disabling accident or illness of a loved one (8.95%), motor vehicle accident that badly injured self or killed someone (5.70%), accident that badly injured self or killed someone (5.33%), natural disaster that badly injured self or killed someone (3.44%), warfare or combat (2.26%), death threat (1.54%), childhood physical abuse (1.36%), and childhood sexual abuse (1.18%). Less than 1% of the sample reported each of the following events: experiencing or witnessing an armed robbery, physical assault by a stranger, witnessing assault or murder, witnessing childhood family violence, physical assault by a partner, adulthood sexual assault, being stalked, and non-live birth pregnancy. In addition, 30.29% of participants reported a life-threatening or highly disturbing event that did not fit these categories (e.g., marital affair, unexpected loss of employment, 2008 stock market crash), 0.90% reported an experience they did not wish to name, and 1.63% did not select a category for their trauma.
Descriptive statistics for and correlations between key variables are presented in Table 1. As expected, both MMPI neuroticism and NEO neuroticism scores were positively associated with the AMQ ratings of emotional intensity, physiological reactions, voluntary rehearsal, and involuntary recall, as well as CES and PCL severity scores. Because PCL severity scores were also associated with female gender and lower annual household income (rs = .08, −.10, ps ≤ .01), gender (0 = male, 1 = female) and income were retained as covariates in the remaining analyses.
Table 1.
Descriptive Statistics and Pearson Correlations Among Predictor Variables and PTSD Symptom Severity in Study 1
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. MMPI Neuroticism a | ||||||||
| 2. NEO Neuroticism | .40*** | |||||||
| 3. Emotional intensity | .16*** | .20*** | ||||||
| 4. Physiological reaction | .14*** | .18*** | .60*** | |||||
| 5. Voluntary rehearsal | .20*** | .17*** | .47*** | .37*** | ||||
| 6. Involuntary recall | .13*** | .21*** | .51*** | .47*** | .66*** | |||
| 7. Event centrality | .16*** | .20*** | .37*** | .32*** | .46*** | .49*** | ||
| 8. PCL severity | .18*** | .31*** | .42*** | .49*** | .44*** | .54*** | .53*** | |
| Mean | 25.25 | 49.17 | 5.31 | 3.66 | 4.97 | 4.35 | 3.27 | 30.43 |
| (SD) | (12.19) | (10.35) | (1.62) | (2.08) | (1.54) | (1.81) | (1.09) | (12.84) |
Note. Gender: 0 = male, 1 = female. MMPI = Minnesota Multiphasic Personality Inventory. NEO = NEO Personality Inventory. PCL severity = PTSD Checklist symptom severity scores.
p ≤ .05,
p ≤ .01,
p ≤ .001.
n = 802.
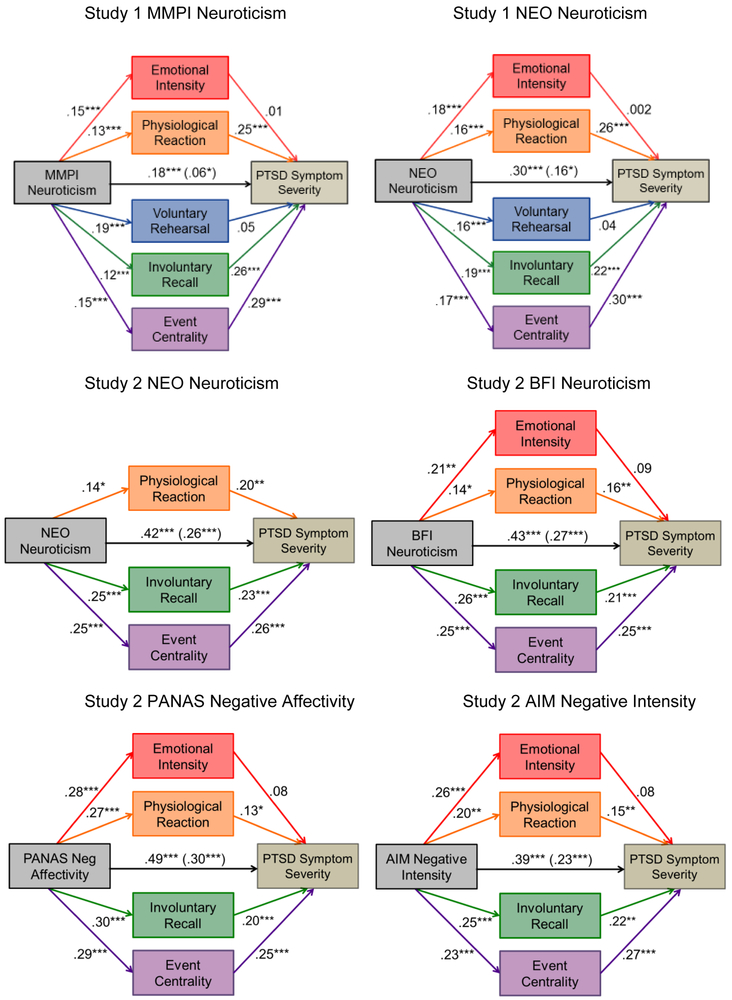
Next we examined whether neuroticism leads to increases in PTSD symptom severity indirectly through measures of emotionality, rehearsal, and centrality. Table 2 presents results from the parallel multiple mediation models. Standardized coefficients are shown in Figure 1. Consistent with our hypothesis, results for the total indirect effect indicated that the trauma memory properties as a set mediated the relation between neuroticism and PTSD symptom severity in the models for both MMPI and NEO neuroticism. Results for the specific indirect effects showed that physiological reactions to the trauma memories, the frequency of involuntary recall, and event centrality each uniquely mediated the relation between neuroticism and PTSD symptom severity, whereas the emotional intensity of the trauma memory and the frequency of voluntary rehearsal did not independently contribute to the indirect effect over and above the other memory properties. The direction of the coefficients indicated that participants with higher neuroticism scores reported more intense physiological reactions to their trauma memories, more frequent involuntary memories of their trauma, and perceived their traumas to be more central to their identity. These properties of the trauma memories were in turn related to greater PTSD symptom severity. In each model, pairwise comparisons of the specific indirect effects revealed that physiological reactions, involuntary recall, and event centrality each accounted for a statistically equivalent percentage of the indirect effect of neuroticism on PTSD symptom severity (MMPI, Bs ≤ .02, SEs ≤ .01, CIs ≤ |−.04, .02|; NEO, Bs ≤ .01, SEs ≤ .02, CIs ≤ |−.04, .02|). Significant direct effects of neuroticism on PTSD symptom severity also emerged in each model indicating that neuroticism exerted an unique effect on PTSD symptom severity independent of the indirect effects through physiological reactions, involuntary rehearsal, and event centrality (MMPI, B = .06, SE = .03, p < .05; NEO, B = .19, SE = .03, p < .001).
Table 2.
Results from Multiple Meditator Models Testing the Indirect Effects of Neuroticism and Negative Affectivity on PTSD Symptom Severity Through Properties of the Trauma Memory
| Study 1 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mediators | MMPI Neuroticism | NEO Neuroticism | ||||||||||
| Coeff. | SE | 95% BC CI | Coeff. | SE | 95% BC CI | |||||||
| Emotional intensity | .00 | .01 | [−.01, .01] | .00 | .01 | [ −.01, .01] | ||||||
| Physiological reaction | .04 | .01 | [ .02, .06] | .05 | .01 | [ .03, .08] | ||||||
| Voluntary rehearsal | .01 | .01 | [−.01, .03] | .01 | .01 | [−.003, .02] | ||||||
| Involuntary recall | .03 | .01 | [ .01, .05] | .05 | .01 | [ .03, .08] | ||||||
| Event centrality | .05 | .01 | [ .03, .07] | .06 | .01 | [ .04, .09] | ||||||
| Total indirect | .13 | .03 | [ .08, .18] | .17 | .02 | [ .13, .22] | ||||||
| Study 2 | ||||||||||||
| Mediators | NEO Neuroticism |
BFI Neuroticism |
PANAS Negative Affectivity |
AIM Negative Intensity |
||||||||
| Coeff. | SE | 95% BC CI | Coeff. | SE | 95% BC CI | Coeff. | SE | 95% BC CI | Coeff. | SE | 95% BC CI | |
| Emotional intensity | — | — | — | .37 | .29 | [−.12, 1.04] | .05 | .04 | [−.03, .12] | .06 | .05 | [−.03, .16] |
| Physiological reaction | .05 | .03 | [.004, .11] | .50 | .31 | [ .02, 1.19] | .07 | .04 | [ .01, .16] | .09 | .05 | [ .01, .20] |
| Involuntary recall | .10 | .04 | [ .04, .19] | 1.14 | .48 | [ .34, 2.21] | .13 | .05 | [ .05, .23] | .17 | .07 | [ .05, .32] |
| Event centrality | .11 | .04 | [ .05, .20] | 1.32 | .48 | [ .52, 2.40] | .15 | .05 | [ .06, .26] | .19 | .08 | [ .06, .35] |
| Total indirect | .27 | .06 | [ .15, .39] | 3.33 | .79 | [1.84, 4.96] | .40 | .07 | [ .27, .54] | .51 | .12 | [ .29, .74] |
Note. Coeff. = unstandardized coefficient. BC CI = bias-corrected confidence intervals. Full model for MMPI neuroticism (Study 1), F(8, 793) = 81.76, p < .001, R2 = .45; NEO neuroticism (Study 1), F(8, 1097) = 122.44, p < .001, R2 = .47; NEO neuroticism (Study 2), F(5, 213) = 36.14, p < .001, R2 = .46; BFI neuroticism, F(6, 214) = 31.76, p < .001, R2 = .47; PANAS negative affectivity, F(6, 214) = 33.07, p < .001, R2 = .48; AIM negative intensity, F(6, 214) = 29.22, p < .001, R2 = .45.
Figure 1.
The indirect effects of neuroticism, negative affectivity, and negative intensity on PTSD symptom severity through properties of the trauma memory in Studies 1 and 2. Values represent standardized coefficients. Path coefficients in parentheses are the effects of neuroticism on PTSD symptom severity independent of the proposed mediators.
*p < .05, **p ≤ .01, ***p ≤ .001.
Because the emotional intensity of the trauma memory, physiological reactions to the trauma memory, and involuntary recall can be viewed as related to items on the PCL, we tested models with the three PCL items related to these mediators removed from the total PCL score to ensure that our results were not driven by potential content overlap. Removal of these items did not substantially change the results: the standardized coefficients shown in Figure 1 changed < |.02|, all 18 significant paths remained significant, and all paths maintained their relative strength. In addition, we examined whether our results were moderated by the developmental timing of the trauma based on previous studies indicating that post-traumatic outcomes vary as a function of whether the trauma occurred in childhood or adulthood (e.g., Cloitre et al., 2009; Ogle, Rubin, & Siegler, 2013a; Ogle, Rubin, & Siegler, 2013b; Ogle, Rubin, & Siegler, 2015). Specifically, among the 1075 participants who reported their age at the time of their trauma, we tested the conditional indirect effect of neuroticism on PTSD symptom severity through the proposed mediators at each level of a dichotomous developmental timing moderator (early life trauma = before age 19, n = 90; adulthood trauma = age 19 or older, n = 985). Estimates of the difference between the indirect effects at each level of the moderator (i.e., the index of moderated mediation, Hayes, 2013) revealed no evidence of moderated mediation in either model (NEO, indices ≤ |.05|, SEs ≤ .04, CIs [−.14, .06]; MMPI, indices ≤ |.01|, SEs ≤ .03, CIs [−.07, .06]).
Discussion
We examined the extent to which neuroticism leads to greater PTSD symptom severity by amplifying the emotionality, rehearsal, and centrality of trauma memories. Results indicated that higher levels of NEO neuroticism in midlife predicted more intense physiological reactions to the trauma memory, more frequent involuntary recall of the memory, and greater centrality of the memory to identity approximately 15 years later. These properties of the trauma memories were in turn related to more severe PTSD symptoms in older adulthood at average age 63. No evidence was found for an effect of neuroticism on PTSD symptom severity through its influence on the emotional intensity of the trauma memory or the frequency of voluntary rehearsal. A nearly identical pattern of results emerged for neuroticism scores from the MMPI completed approximately 30 years before the NEO and 45 years prior to PTSD symptom reporting. Our finding that the observed relations between neuroticism, ratings of the phenomenological properties of trauma memories, and PTSD symptom severity were replicated across two measures of neuroticism assessed approximately three decades apart is consistent with cross-sectional and longitudinal research showing that personality is moderately stable in adulthood (McCrae & Costa, 1994; Robins, Fraley, Roberts, & Trzesniewski, 2001; Terracciano, McCrae, Brant, & Costa, 2005). Furthermore, the consistency of our findings across two measures of neuroticism assessed at different points in the life course and 15 or more years prior to participant ratings of the phenomenological properties of their trauma memories and PTSD symptoms suggests that neuroticism is a reliable longitudinal predictor of the mechanisms important to PTSD symptoms.
Study 2
The community-dwelling older adults included in Study 1 were exposed to a range of negative and potentially traumatic events that varied widely in severity. To examine whether our findings would replicate in a sample of individuals with histories of exposure to traumas severe enough to qualify for a potential diagnosis of PTSD, participants in Study 2 were required to have experienced a trauma that met the DSM-IV-TR A1 criterion, according to which the individual must have experienced, witnessed, or confronted “an event or events that involved actual or threatened death or injury, or a threat to the physical integrity of the self or others” (American Psychiatric Association, 2000, p. 467). To ensure that our findings concerning the mechanisms underlying the relation between neuroticism and PTSD symptoms extend beyond the measures of neuroticism used in Study 1, in Study 2 we report findings for the NEO as well as three additional measures of neuroticism and negative affectivity, a closely related personality construct that subsumes neuroticism broadly construed and is strongly correlated with depression and anxiety symptoms (Watson, Gamez, & Simms, 2005). Two of the three measures are subscales of standardized, well-validated personality instruments: neuroticism domain scores from the Big Five Inventory (BFI; John, Donahue, & Kentle, 1991) and negative affectivity scores from the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988). The third measure is derived from factor analysis of the Affect Intensity Measure (AIM; Larsen & Diener, 1987). The negative intensity factor of the AIM (AIM-NI) was selected for inclusion in the present study instead of the total AIM score based on studies indicating that the total AIM score does not measure a single underlying construct (e.g., Rubin et al., 2012). In addition, the AIM-NI correlates strongly with other measures of neuroticism and negative affectivity. For example, Rubin et al. (2012) reported a correlation of .72 between neuroticism and the AIM-NI suggesting that these two measures may be regarded as alternative assessments of the same or similar personality construct and that “empirically, negative intensity can not be distinguished from neuroticism” (p. 13). Additional research has shown that, of the four factors derived from factor analysis of the AIM, negative intensity is the only factor associated with PTSD symptoms (Rubin, Boals, & Berntsen, 2008). With the exception of the measure for voluntary rehearsal (described below), the measures of trauma memory properties and PTSD symptoms included in Study 2 were the same as those in Study 1. Study 2 hypotheses were also identical to those of Study 1, with the addition that results for negative affectivity and negative intensity scores were expected to mirror those from the standardized measures of neuroticism.
Method
Participants
Adults from the community were screened as part of a larger study by clinicians who were trained and worked regularly in a research setting. Participants were recruited via advertising for a study on memory for stressful or traumatic events. Exclusion criteria included current alcohol or other substance dependence/abuse measured by self-report and urine drug screen, neurological damage (i.e., head trauma, disease), and current psychotic disorder or bipolar disorder with active manic symptoms based on the Structured Clinical Interview for DSM-IV Diagnosis (SCID; First, Spitzer, Gibbon, & Williams, 1996). Nicotine dependence was allowed. To be included in the study, all participants were required to have met the DSM-IV-TR PTSD A1 criterion as determined during clinical interviews.
Participants who completed the measure of PTSD symptoms, at least one of the personality inventories, the CES, and the AMQ were selected to be included in the analysis sample (n = 221; 94.44% of the total study sample). The final analysis sample was 52.94% male, with a mean age of 42.21 (SD = 13.13), and a mean annual household income of $35–49,999. The sample was 65.16% African American, 25.79% Caucasian, 3.62% Hispanic, 3.17% multiracial, 1.36% American Indian, and 0.90% Asian. Approximately 8% did not complete high school, 31.22% earned a high school diploma or the equivalent, 42.53% attended some college, 13.12% earned a Bachelor’s degree, and 4.98% had a graduate degree.
Measures (not described in Study 1)
Autobiographical Memory Questionnaire (AMQ).
Three of the five items analyzed from the AMQ (Rubin, Schrauf, & Greenberg, 2003, 2004) were identical to those included in Study 1: emotional intensity, physiological reaction, and involuntary recall. Voluntary rehearsal was indexed by two additional items querying the frequency of voluntarily thinking and voluntarily talking about a memory (“Since it happened, I have willfully thought back to the event in my mind” and “Since it happened, I have willfully thought back to the event in my mind and talked about it”).
Big Five Inventory (BFI).
The BFI (John et al., 1991) is a 44-item measure of the broad personality domains of Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness. Each domain is assessed by eight to ten short phrases (e.g., Neuroticism: “Is emotionally stable, not easily upset” [reversed scored], “worries a lot”). The reliability of the scales is high (α = .80). Convergent and discriminant validity of the scales are well established (John & Srivastava, 1999). Neuroticism domain scores were analyzed.
Positive and Negative Affect Schedule (PANAS).
The PANAS (Watson et al., 1988) includes two 10-item subscales that measure the tendency to experience positive and negative affect. Negative affect subscale scores were included in the present study. For this subscale, participants rate the tendency to experience 10 negative feelings (distressed, upset, guilty, scared, hostile, irritable, ashamed, nervous, jittery, afraid) using 5-point scales (1 = very slightly or not at all, 5 = extremely).
Affect Intensity Measure (AIM).
The AIM (Larsen & Diener, 1987) is a 40-item questionnaire that measures individual differences in the strength and intensity of emotional experiences. Respondents are asked how often they react to situations with strong emotions (1 = never, 6 = always). The AIM has high internal consistency, test-retest reliability, and criterion related validity (Larsen & Diener, 1987). The Negative Intensity subscale of the AIM (AIM-NI; Rubin et al., 2012) includes eight items that assess the intensity of negative emotions (e.g., “My negative moods are mild in intensity”, “When I get angry it’s easy for me to still be rational and not overreact”). The AIM-NI has high internal consistency and correlates strongly with other measures of negative affectivity (Rubin et al., 2012).
Procedure
Administration of the protocol was completed individually with each participant by trained clinical research staff in a Veterans Affairs Medical Center. Participants in our sample were enrolled in a larger study for which they were compensated $500 for completing 6 total sessions. During session 1, participants were first screened for any current illicit drug use, then administered the TLEQ (Kubany et al., 2000), CAPS (Blake et al., 1990), and SCID (First et al., 1996), and finally queried about current medications and treatment history. During session 2, the AMQ (Rubin et al., 2003, 2004) was administered for 15 cue words, and participants completed a series of individual difference measures including the PANAS (Watson et al., 1988), BFI (John et al., 1991), and AIM (Larsen & Diener, 1987). During session 3, which is key to the current report, participants orally narrated their three most negative, stressful, or traumatic life events followed by their three most positive and finally their three most important life events that were not among the most traumatic or positive. After describing each event, they completed the AMQ, CES, and PCL for that event. During Session 4, participants completed the NEO. After later sessions, participants were debriefed and referred for support if necessary.
Data Analysis
Following the data analysis strategy used in Study 1, bias-corrected bootstrapped parallel multiple mediator models were used to examine the extent to which measures of emotionality, rehearsal, and centrality mediate the relation between measures of neuroticism/negative affectivity and PTSD symptom severity. Ratings for the traumatic event with the most severe PTSD symptoms were included in our analyses.
Results
Participants reported a wide range of traumatic events. Prevalence rates were highest for unexpected death of a loved one (23.53%), followed by combat (20.81%), adulthood violence (10.86%), adulthood physical or sexual assault (10.41%), childhood abuse (8.60%), accident (7.24%), domestic violence (2.26%), exposure to violence in childhood (1.81%), and natural disasters (.45%). An additional 14.03% of participants reported a life-threatening or highly disturbing event that did not fit these categories.
Descriptive statistics and inter-correlations for key variables are presented in Table 3. As expected, BFI neuroticism scores, PANAS negative affectivity scores, and AIM-NI scores were positively associated with PCL symptom severity. The measures of neuroticism and negative affectivity were also positively associated with ratings of emotional intensity, physiological reaction, involuntary recall, and event centrality. However, in contrast to results from Study 1, no associations were found between ratings of voluntary rehearsal (thinking or talking) and the measures of neuroticism, negative affectivity, and PCL symptom severity. A repeated measures ANCOVA followed by pairwise comparisons of all three measures of rehearsal (voluntary thinking, voluntary talking, and involuntary recall) revealed that voluntary talking was significantly lower than voluntary thinking and involuntary recall, whereas no differences were found between voluntary thinking and involuntary recall, F(2, 216) = 24.99, p < .001, ηp2 = .19. Thus, although the measures of voluntary rehearsal and involuntary recall did not correlate consistently with the measures of neuroticism, negative affectivity, and the PCL, the mean levels of voluntarily thinking about trauma memories and involuntarily recalling them were statistically equivalent. Given the non-significant correlations between the two ratings of voluntary rehearsal and the measures of neuroticism, negative affectivity, and PTSD symptom severity, voluntary thinking and voluntary talking were omitted from the remaining analyses. Likewise, the AMQ rating of emotional intensity was omitted from the model for the NEO because the correlation between these measures failed to reach significance (p = .06). Because PCL severity scores were correlated with age (r = .17, p < .05), age was included as a covariate in the remaining analyses.
Table 3.
Descriptive Statistics and Pearson Correlations Among Predictor Variables and PTSD Symptom Severity in Study 2
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. NEO Neuroticism a | |||||||||||
| 2. BFI Neuroticism | .73*** | ||||||||||
| 3. Negative affectivity | .59*** | .60*** | |||||||||
| 4. Negative intensity | .57*** | .64*** | .54*** | ||||||||
| 5. Emotional intensity | .13 | .21*** | .29*** | .27*** | |||||||
| 6. Physiological reaction | .15* | .15* | .27*** | .21** | .53*** | ||||||
| 7. Voluntary thinking | .07 | .01 | −.01 | .07 | .23** | .18* | |||||
| 8. Voluntary talking | .04 | .00 | −.07 | .05 | .13 | .12 | .60*** | ||||
| 9. Involuntary recall | .25*** | .26*** | .30*** | .24*** | .42*** | .33*** | .40*** | .27*** | |||
| 10. Event centrality | .25*** | .25*** | .29*** | .23*** | .44*** | .37*** | .22*** | .18* | .41*** | ||
| 11. PCL severity | .42*** | .44*** | .50*** | .41*** | .45*** | .42*** | .06 | .02 | .46*** | .50*** | |
| Mean | 47.63 | 2.96 | 22.33 | 30.77 | 6.21 | 5.33 | 4.96 | 4.15 | 4.86 | 3.89 | 49.29 |
| (SD) | (10.53) | (.87) | (8.82) | (6.01) | (1.13) | (1.88) | (1.87) | (2.01) | (1.84) | (1.10) | (18.48) |
Note. Gender: 0 = male, 1 = female. BFI = Big Five Inventory. NEO = NEO Personality Inventory. PCL severity = PTSD Checklist symptom severity scores.
p < .05,
p ≤ .01,
p ≤ .001.
n = 219.
Table 2 presents results from the mediation models testing whether high neuroticism and negative affectivity lead to greater PTSD symptom severity indirectly through the emotionality, rehearsal, and centrality of trauma memories. Standardized coefficients are shown in Figure 1. Consistent with our hypothesis, results from the two models of standardized neuroticism measures, the NEO and the BFI, revealed significant total indirect effects indicating that the trauma memory properties as a set mediated the relation between neuroticism and PTSD symptom severity for both NEO and BFI neuroticism scores. Results for the specific indirect effects indicated that participants with higher neuroticism scores reported more intense physiological reactions while remembering their traumas, more frequent involuntary memories of their traumas, and greater perceptions of their trauma memories as central to their identity. These trauma memory characteristics were in turn related to greater PTSD symptom severity. In the model for BFI neuroticism scores, the emotional intensity of the trauma memories did not independently contribute to the indirect effect over and above the other memory properties. Pairwise comparisons of the specific indirect effects revealed that physiological reactions, involuntary recall, and event centrality each accounted for a statistically equivalent percentage of the indirect effect of neuroticism on PTSD symptom severity (NEO: Bs ≤ .07, SEs ≤ .05, CIs ≤ [−.13, .10]; BFI: Bs ≤ .98, SEs ≤ .71, CIs ≤ [−1.68, 1.14]). The significant direct effects of neuroticism on PTSD symptom severity found in both models indicated that neuroticism exerted an unique effect on PTSD symptom severity independent of the indirect effects through physiological reactions, involuntary recall, and event centrality (NEO: B = .47, SE = .09, CI [.29, .65]; BFI: B = 5.83, SE = 1.11, CI [3.65, 8.01]).
The models testing PANAS negative affectivity and AIM-NI scores were nearly identical to the findings for the standardized neuroticism measures. In each model, the trauma memory properties mediated the effects of negative affectivity and negative intensity on PTSD symptom severity. Specific indirect effects were found for physiological reactions, involuntary recall, and event centrality, but not emotional intensity. Pairwise comparisons of the specific indirect effects in each model indicated that physiological reactions, involuntary recall, and event centrality each accounted for a statistically equivalent percentage of the effect of negative affectivity and negative intensity on PTSD symptom severity (PANAS NA, Bs ≤ .11, SEs ≤ .08, CIs ≤ [−.19, .12]; AIM-NI, Bs ≤ .13, SEs ≤ .11, CIs ≤ [−.18, .28]). The significant direct effects of PANAS negative affectivity and AIM-NI further indicated that these personality constructs predicted PTSD symptom severity independently of their influence through the trauma memory properties (PANAS NA, B = .63, SE = .11, CI [.41, .85]; AIM-NI, B = .74, SE = .17, CI [.41, 1.06]).
Because the emotional intensity of the trauma memory, physiological reactions to the trauma memory, and involuntary recall can be viewed as related to items on the PCL, we tested models with the three PCL items related to these mediators removed from the total PCL score to ensure that our results were not driven by potential content overlap. Removal of these items did not substantially change the results: the standardized coefficients shown in Figure 1 changed by ≤ |.03|, all but one of the 31 significant paths remained significant, and all paths maintained their relative strength compared to the model testing the total PCL score. In addition, we tested whether the paths from the personality predictors to each memory property shown in Figure 1 were moderated by the developmental timing of the trauma among the 154 participants who reported their age at the time of their trauma (early life trauma = before age 19, n = 34; adulthood trauma = age 19 or older, n = 120). No evidence of moderated mediation was found (NEO, indices ≤ |.07|, SEs ≤ .13, CIs [−.22, .17]; BFI, indices ≤ |2.03|, SEs ≤1 .21, CIs [−1.05, 3.48]; PANAS NA, indices ≤ |.17|, SEs ≤ .13, CIs [−.12, .44]; AIM-NI, indices ≤ |.18|, SEs ≤ .19, CIs [−.34, .42]).
Discussion
Across two studies, we investigated the extent to which individuals with higher levels of neuroticism are more likely to report greater PTSD symptom severity as a result of higher levels of cognitive-affective processes that increase the availability of their trauma memories. In Study 1, longitudinal data from a large community-dwelling sample of adults with histories of negative and potentially traumatic events indicated that individuals with higher levels of neuroticism collected at two different points in the lifespan reported more intense physiological reactions to their trauma memories, experienced more frequent involuntary memories of their traumas, and perceived their traumas to be more central to their identity. These properties of the trauma memories were in turn related to greater PTSD symptom severity. Moreover, a test of the equality of the indirect effects showed that each of these memory properties accounted for a statistically equivalent percentage of the explained variance in PTSD symptom severity. Our use of two standardized and well-validated measures of neuroticism collected approximately 30 years apart and 15 or more years before symptom reporting strengthens support for our finding that neuroticism is prospectively related to more severe PTSD symptoms via greater intensity, rehearsal, and centrality of trauma memories among individuals exposed to negative and potentially traumatic events ranging in severity.
To determine whether our findings replicate in individuals exposed to severe, life-threatening traumas that would qualify for a diagnosis of PTSD, in Study 2 we tested individuals with histories of traumatic events that met the DSM-IV-TR A1 criterion. In addition to the NEO, we included three new measures of neuroticism and the closely related construct of negative affectivity to examine whether the findings from Study 1 generalize to additional measures of personality. The same pattern of results found in the community dwelling adults tested in Study 1 emerged for all four measures of neuroticism and negative affectivity tested in individuals exposed to severe trauma in Study 2. Collectively, our findings suggest that neuroticism contributes to PTSD symptoms in part by magnifying the emotionality, rehearsal, and centrality of memories for traumatic events.
Overall our results extend empirical support for the processes involved in the development of PTSD symptoms according to the AMT. Specifically, the AMT proposes that individuals with different personality traits vary in their levels of cognitive-affective processes that increase the availability of trauma memories. These individual differences in memory availability mechanisms are thought to in turn explain the observed heterogeneity in individuals’ reactions to traumatic events. Consistent with the AMT, prior cross-sectional studies have shown that neuroticism is associated with greater emotionality, rehearsal, and centrality of autobiographical memories (Rubin, Boals, & Berntsen, 2008; Rubin et al., 2011), and that measures of the emotionality, rehearsal, and centrality of autobiographical memories predict greater PTSD symptom severity (Berntsen et al., 2003; Rubin, Boals, & Berntsen, 2008; Rubin et al., 2004; Rubin et al., 2011; Rubin et al., 2014). In addition to replicating these findings, we add to the empirical support for the AMT by examining the pathways between neuroticism and the cognitive-affective processes and testing their direct and indirect effects on PTSD symptom severity using longitudinal data in Study 1 and cross-sectional data from a clinically-diagnosed sample in Study 2. Although additional prospective studies are needed to further understand the mechanisms through which other personality factors contribute to PTSD, our results indicated that individuals with higher neuroticism and negative affectivity are at an elevated risk of PTSD symptoms in part as a result of higher levels of cognitive-affective mechanisms that increase the accessibility of their trauma memories in mind.
Several features of the current investigation strengthen our ability to draw conclusions about the processes through which elevated levels of neuroticism lead to greater PTSD symptom severity. First, Study 1 included data from two measures of neuroticism using well-validated personality tests that were administered approximately three decades apart which allowed us to examine the longitudinal stability of neuroticism in predicting properties of trauma memories and PTSD symptom severity. Second, the personality assessments included in Study 1 were completed approximately 45 and 18 years prior to symptom reporting, which limited potential bias of trauma-related distress on the measures of neuroticism. Third, the replication of our findings from a community-dwelling sample of adults ranging widely in symptom severity in Study 1 to a clinically diagnosed sample of adults with histories of severe, life-threatening traumas in Study 2 suggests that the processes through which neuroticism leads to greater PTSD symptom severity are consistent across clinical and non-clinical samples and that our findings are not explained by variations in the severity of the trauma. Fourth, we demonstrated that our results generalize to more than one measure of neurotic traits by examining five different measures of neuroticism and the closely related concepts of negative affectivity and affect intensity across Studies 1 and 2. Despite the variety of measures used, our analyses revealed substantial convergence in showing that neuroticism increased PTSD symptom severity in part by amplifying the emotionality intensity of the trauma memory, the frequency of memory rehearsal, and the centrality of the memory to identity.
Although the findings from Studies 1 and 2 were generally consistent, one difference that emerged concerned the relation between voluntary rehearsal and PTSD symptoms. Although the frequency of voluntary rehearsal was positively correlated with neuroticism and PTSD symptom severity in Study 1, voluntary rehearsal did not independently contribute to the indirect effect of neuroticism on PTSD symptom severity over and above the other trauma memory properties. In contrast, among individuals with histories of severe trauma in Study 2, the measures of voluntary rehearsal (i.e., voluntarily thinking or talking about one’s trauma memory) were not significantly associated with neuroticism, negative affectivity, or PTSD symptom severity. Thus, voluntary rehearsal was not consistently related to the measures of neuroticism and PTSD symptom severity across Studies 1 and 2. However, a comparison of the three rehearsal measures included in Study 2 (i.e., voluntarily thinking, voluntarily talking, involuntary recall) indicated that the frequency of voluntarily thinking about and involuntarily recalling one’s trauma memories were statistically equivalent. This finding combined with the Study 1 results suggest that although voluntary rehearsal of trauma memories occurred as frequently as involuntary recall, voluntary rehearsal is a less reliable correlate of PTSD severity and a less reliable mechanism underlying the relation between neuroticism and PTSD symptoms in the samples we tested.
The absence of a linear relation between voluntary rehearsal and PTSD symptom severity among individuals with severe trauma histories in Study 2 may also reflect the inherent tension between efforts to avoid reminders of the trauma and re-experiencing symptoms that is reflected in the diagnostic symptom clusters of PTSD. Fluctuations between thinking and talking about the trauma and efforts to avoid reminders of the trauma may obscure detectable relations between voluntary rehearsal and symptom severity or impede individuals’ ability to accurately remember and report the frequency of voluntary rehearsal. Consistent with this idea, in a sample of undergraduates selected on the basis of extreme scores on the PCL, Rubin, Boals, and Berntsen (2008) reported a correlation of .01 between voluntary rehearsal of negative memories and PTSD symptom severity in individuals with high PCL scores. The correlation for the full sample, which included individuals with high and low PCL scores, was .23. Taken together, these results suggest that the frequency of voluntarily talking about and thinking about one’s trauma may not contribute to PTSD symptom severity among individuals with histories of severe trauma.
Several limitations of the present study should be noted and addressed in future research. First, the ability to draw conclusions about the direction of causality among the constructs and symptoms examined in Study 2 is limited by our use of cross-sectional data. However, the purpose of Study 2 was to replicate the longitudinal analyses in Study 1 using a clinically diagnosed sample. The consistency of the findings across Studies 1 and 2 lends support for our theoretical model despite our use of cross-sectional data in Study 2. Nonetheless, replication of our findings in additional prospective datasets is needed. Second, our measures of memory rehearsal required individuals to retrospectively report the frequency of voluntary and involuntary rehearsal of their trauma memories, which may be vulnerable to memory errors. However, studies that utilized ecological momentary assessment and electronic diary methodologies to examine properties of trauma memories as they are recalled in everyday life have found patterns of relations between trauma memory characteristics and PTSD symptom severity similar to those in the current study. For instance, in Rubin et al. (2011), community-dwelling adults, approximately half of whom had PTSD diagnoses, rated properties of their involuntary autobiographical memories as they occurred over a 2 week period on electronic handheld devices. For each involuntary memory reported, participants were asked to recall a voluntary memory from the same time period. Compared to the control group, participants with PTSD reported memories accompanied by greater emotional intensity, more intense physiological reactions, more frequent voluntary rehearsal and involuntary recall, and greater centrality to the life story. Similar results from a nonclinical sample of college students varying in PTSD symptom severity were reported by Rubin, Boals, and Berntsen (2008). The consistency of findings from Rubin et al. (2011), Rubin, Boals, and Berntsen (2008), and the present study suggests that our results concerning the role of memory rehearsal in the relation between neuroticism and PTSD symptom severity are not explained by the specific methodology used to elicit reports of the frequency of memory rehearsal.
Within the context of these limitations, the present study provides new information on the processes through which personality influences individuals’ vulnerability to PTSD symptoms. Our results indicate that neuroticism confers risk for PTSD symptoms by amplifying a constellation of phenomenological properties of the current trauma memory that increase the availability of the memory in mind. Given that no clinical treatments currently exist to alter personality traits through the course of therapy and that evidence of individuals’ ability to volitionally change personality is limited (Hudson & Fraley, 2015), the clinical implications of our findings are instead that treatments targeted at diminishing the emotionality, rehearsal, and centrality of trauma memories may be effective methods of reducing PTSD symptom severity among individuals with higher levels of neurotic traits. For instance, our finding that neuroticism increases the intensity of individuals’ physiological reactions to memories of their trauma, which in turn is related to greater PTSD symptom severity, suggests that treatments designed to reduce fear reactions to physiological signs of arousal, such as interoceptive exposure therapy, may show promise in decreasing PTSD symptoms in individuals with high levels of neuroticism. Alternatively, treatments that incorporate affect regulation skills training may be effective at reducing PTSD symptoms among individuals with high levels of neuroticism to the extent that emotion regulation strategies decrease the emotionality, rehearsal, and centrality of trauma memories. Future research is needed to explore these possibilities.
Acknowledgments
This material is the result of work supported in part by resources and the use of facilities at the Durham, NC, Veterans Affairs Medical Center and the National Institute of Health (NIH). The contents do not represent the views of the NIH, the U.S. Department of Veterans Affairs, or the United States Government.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This manuscript was supported by Grant R01-MH066079 from the National Institute of Mental Health, the Duke Behavioral Medicine Research Center, and a VA Clinical Sciences Research and Development Career Scientist Award.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Christin M. Ogle, Duke University
Ilene C. Siegler, Duke University and Duke University Medical Center
Jean C. Beckham, Durham Veterans Affairs Medical Center and Duke University Medical Center
David C. Rubin, Duke University and Aarhus University
References
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: American Psychiatric Association. [Google Scholar]
- Berntsen D, & Rubin DC (2006). The Centrality of Event Scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behaviour Research and Therapy, 44, 219–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, & Rubin DC (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21, 417–431. [Google Scholar]
- Berntsen D, & Rubin DC, & Salgado S (2015). The frequency of involuntary autobiographical memories and future thoughts in relation to daydreaming, emotional distress, and age. Consciousness and Cognition, 36, 352–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, Willert M, & Rubin DC (2003). Splintered memories or vivid landmarks? Qualities and organization of traumatic memories with and without PTSD. Applied Cognitive Psychology, 17, 675–693. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a clinician-administered posttraumatic stress disorder scale. Journal of Traumatic Stress, 8, 75–80. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. [DOI] [PubMed] [Google Scholar]
- Bolger N, & Zuckerman A (1995). A framework for studying personality in the stress process. Journal of Personality and Social Psychology, 69, 890–902. [DOI] [PubMed] [Google Scholar]
- Breslau N, & Schultz L (2013). Neuroticism and post-traumatic stress disorder: A prospective investigation. Psychological Medicine, 43, 1697–1702. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, van der Kolk B, Pynoos R, Wang J, & Petkova E (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22, 399–408. [DOI] [PubMed] [Google Scholar]
- Costa PT, Herbst JH, McCrae RR, & Siegler IC (2000). Personality at midlife: Stability, intrinsic maturation, and response to life events. Assessment, 7, 365–378. [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Revised NEO Personality Inventory (NEO-PI-R). Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Costa PT, Zonderman AB, McCrae RR, Williams RB (1985). Content and comprehensiveness in the MMPI: An item factor analysis in a normal adult sample. Journal of Personality and Social Psychology, 48, 925–933. [Google Scholar]
- Cox BJ, MacPherson PSR, Enns MW, & McWilliams LA (2004). Neuroticism and self-criticism associated with posttraumatic stress disorder in a nationally representative sample. Behaviour Research and Therapy, 42, 105–114. [DOI] [PubMed] [Google Scholar]
- David D, Mellman TA, Mendoza LM, Kulick-Bell R, Ironson G, & Schneiderman N (1996). Psychiatric morbidity after Hurricane Andrew. Journal of Traumatic Stress, 9, 607–612. [DOI] [PubMed] [Google Scholar]
- Davidson J, Kudler H, & Smith R (1987). Personality in chronic post-traumatic stress disorder: A study of the Eysenck Inventory. Journal of Anxiety Disorders, 1, 295–300. [Google Scholar]
- Dyb G, Jensen TK, Nygaard E, Ekeberg Ø, Diseth TH, Wentzel-Larsen T, & Thoresen S (2014). Post-traumatic stress reactions in survivors of the 2011 massacre on Utøya Island, Norway. The British Journal of Psychiatry, 204, 361–367. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, & Lommen MJ (2009). Individuals high in neuroticism are not more reactive to adverse events. Personality and Individual Differences, 47, 697–700. [Google Scholar]
- Ericsson KA, & Simon HA (1993). Protocol analysis: Verbal reports as data (Rev. ed.) Cambridge, MA: MIT (Bradford Books). [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, D.C.: American Psychiatric Press, Inc. [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press. [Google Scholar]
- Hooker K, Hoppmann C, & Siegler IC (2010). Personality: Life span compass for health. Annual Review of Gerontology and Geriatrics, 30, 201–232. [Google Scholar]
- Hudson NW, & Fraley RC (2015). Volitional personality trait change: Can people choose to change their personality traits? Journal of Personality and Social Psychology, 109, 490–507. [DOI] [PubMed] [Google Scholar]
- John OP, Donahue EM, & Kentle RL (1991). The Big Five Inventory: Versions 4a and 54 Berkeley, CA: University of California, Berkeley, Institute of Personality and Social Research. [Google Scholar]
- John OP, & Srivastava S (1999). The Big-Five trait taxonomy: History, measurement, and theoretical perspectives In Pervin LA & John OP (Eds.), Handbook of personality: Theory and research (Vol. 2, pp. 102–138). New York, NY: Guilford Press. [Google Scholar]
- Kleim B, Graham B, Bryant RA, & Ehlers A (2013). Capturing intrusive re-experiencing in trauma survivors’ daily lives using ecological momentary assessment. Journal of Abnormal Psychology, 122, 998–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, & Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure. Psychological Assessment, 12, 210–224. [DOI] [PubMed] [Google Scholar]
- Larsen RJ, & Diener E (1987). Affect intensity as an individual difference characteristic: A review. Journal of Research in Personality, 21, 1–39. [Google Scholar]
- Lauterbach D, & Vrana S (2001). The relationship among personality variables, exposure to traumatic events, and severity of posttraumatic stress symptoms. Journal of Traumatic Stress, 14, 29–45. [Google Scholar]
- McCrae RR, & Costa PT (1994). The stability of personality: Observations and evaluations. Current Directions in Psychological Science, 173–175. [Google Scholar]
- Martin M (1985). Neuroticism as a predictor toward depression: A cognitive mechanism. Personality and Individual Differences, 6, 353–365. [Google Scholar]
- Ogle CM, Rubin DC, & Siegler IC (2013a). The impact of the developmental timing of trauma exposure on PTSD symptoms and psychosocial functioning among older adults. Developmental Psychology, 49, 2191–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle CM, Rubin DC, Berntsen D, & Siegler IC (2013b). The frequency and impact of exposure to potentially traumatic events over the life course. Clinical Psychological Science, 1, 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle CM, Rubin DC, & Siegler IC (2015). The relation between insecure attachment and posttraumatic stress: Early life versus adulthood traumas. Psychological Trauma: Theory, Research, Practice, and Policy, 7, 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orcutt HK, Bonanno GA, Hannan SM, & Miron L, R. (2014). Prospective trajectories of posttraumatic stress in college women following a campus mass shooting. Journal of Traumatic Stress, 27, 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parslow RA, Jorm AF, & Christensen H (2006). Associations with pre-trauma attributes and trauma exposure with screening positive for PTSD: Analysis of a community-based study of 2085 young adults. Psychological Medicine, 36, 387–395. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Robins RW, Fraley RC, Roberts BW, & Trzesniewski KH (2001). A longitudinal study of personality change in young adulthood. Journal of Personality, 69, 617–640. [DOI] [PubMed] [Google Scholar]
- Roelofs J, Huibers M, Peeters F, Arntz A, & van Os J (2008). Rumination and worrying as possible mediators in the relation between neuroticism and symptoms of depression and anxiety in clinically depressed individuals. Behaviour Research and Therapy, 46, 1283–1289. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Berntsen D, & Bohni MK (2008). A memory-based model of posttraumatic stress disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review, 115, 985–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Boals A, & Berntsen D (2008). Memory in posttraumatic stress disorder: Properties of voluntary and involuntary, traumatic and non-traumatic autobiographical memories in people with and without PTSD symptoms. Journal of Experimental Psychology: General, 137, 591–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Boals A, & Hoyle RH (2014). Narrative centrality and negative affectivity: Independent and interactive contributors to stress reactions. Journal of Experimental Psychology: General, 143, 1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Dennis MF, & Beckham JC (2011). Autobiographical memory for stressful events: The role of autobiographical memory in posttraumatic stress disorder. Consciousness & Cognition, 20, 840–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Feldman ME, & Beckham JC (2004). Reliving, emotions, and fragmentation in the autobiographical memories of veterans diagnosed with PTSD. Applied Cognitive Psychology, 18, 17–35. [Google Scholar]
- Rubin DC, Hoyle RH, & Leary MR (2012). Differential predictability of four dimensions of affect intensity. Cognition & Emotion, 26, 25–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Schrauf RW, & Greenberg DL (2003). Belief and recollection of autobiographical memories. Memory and Cognition, 31, 887–901. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Schrauf RW, & Greenberg DL (2004). Stability in autobiographical memories. Memory, 12, 715–721. [DOI] [PubMed] [Google Scholar]
- Siegler IC, Peterson BL, Barefoot JC, Harvin SH, Dahlstrom WG, Kaplan BH, … Williams RB (1992). Using college alumni populations in epidemiologic research: The UNC Alumni Heart Study. Journal of Clinical Epidemiology, 45, 1243–1250. [DOI] [PubMed] [Google Scholar]
- Siegler IC, Zonderman AB, Barefoot JC, Williams RB Jr, Costa PT Jr, & McCrae RR (1990). Predicting personality in adulthood from college MMPI scores: Implications for follow-up studies in psychosomatic medicine. Psychosomatic Medicine, 52, 644–652. [DOI] [PubMed] [Google Scholar]
- Sutin A (2008). Autobiographical memory as a dynamic process: Autobiographical memory mediates basic tendencies and characteristic adaptations. Journal of Research in Personality, 42, 1060–1066. [Google Scholar]
- Talarico JM, & Rubin DC (2003). Confidence, not consistency, characterizes flashbulb memories. Psychological Science, 14, 455–461. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, & Green HA (2004). Ruminative self-focus and autobiographical memory. Personality and Individual Differences, 36, 1933–1943. [Google Scholar]
- Terracciano A, McCrae RR, Brant LJ, & Costa PT Jr (2005). Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore Longitudinal Study of Aging. Psychology and Aging, 20, 493–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomsen DK, & Berntsen D (2008). The long-term impact of emotionally stressful events on memory characteristics and life story. Applied Cognitive Psychology, 23, 579–598. [Google Scholar]
- U.S. Department of Veterans Affairs, National Center for PTSD (2014). Using the PTSD Checklist for DSM-IV (PCL). Retrieved from http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf.
- Watson D, Gamez W, & Simms LJ (2005). Basic dimensions of temperament and their relation to anxiety and depression: A symptom based perspective. Journal of Research in Personality, 39, 46–66. [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, & Keane TM (1994). The PTSD checklist (PCL). Scale available from the National Center for PTSD. [Google Scholar]
- van Zelst WH, de Beurs E, Beekham ATF, Deeg DJH, & van Dyck R (2003). Prevalence and risk factors of posttraumatic stress disorder in older adults. Psychotherapy and Psychosomatics, 72, 333–342. [DOI] [PubMed] [Google Scholar]