Abstract
Background End-stage wrist arthritis has traditionally been treated with a total wrist fusion. There is a recent trend toward motion preserving surgery in the form of total wrist replacement.
Questions Is there a functional benefit to performing a total wrist replacement instead of a total wrist fusion in patients with end-stage wrist arthritis? Is there any difference in secondary outcome measures including pain, grip strength, and range of motion? Does the risk of adverse events and treatment failure differ between the two techniques?
Methods A systematic literature search was performed to identify studies reporting either total wrist arthrodesis or arthroplasty for end-stage wrist arthritis. Studies were systematically screened and assessed for risk of bias and quality. Data were extracted and reviewed.
Results A total of 43 studies were included in the review: 17 on arthrodesis, 24 on arthroplasty, and 2 matched cohort studies. This represented 669 index arthrodesis operations in 603 patients, and 1,371 index arthroplasty operations in 1,295 patients. A significant improvement in functional outcome was seen with both interventions. Similar improvements were seen in pain scores, and modest improvements were seen in grip strength. Range of motion following arthroplasty improved to a functional level in two studies. Complication rates were higher after arthroplasty (range: 0.2–9.5%) than those after arthrodesis (range: 0.1–6.1%; p = 0.06). Fourth-generation implants (range 0.1–2.9%) performed better than earlier designs (range: 0.2–8.1%; p = 0.002). Implant revision rates ranged from 3.5 to 52.6%. Fourth-generation prostheses survival rates were 78% at 15 years (Universal 2), 86% at 10 years (Motec), 90% at 9 years (Re-Motion), and 95% at 8 years (Maestro).
Conclusion The newer fourth-generation wrist implants appear to be performing better than earlier designs. Both wrist arthrodesis and wrist arthroplasty improve function, pain, and grip strength. The risk of complication following wrist replacements is higher than that after total wrist arthrodesis.
Keywords: wrist, arthritis, arthroplasty, arthrodesis, systematic review
Total wrist arthrodesis has been the gold standard for managing advanced inflammatory and degenerative arthritis of the wrist for many years. Some of the first techniques described to achieve wrist fusion used intramedullary pins, such as a Steinman pin with a radial bone graft by Clayton, later modified by Mannerfelt and Malsten, who used a Rush pin through the third metacarpal into the radius and two staples to prevent rotation. 1 2 The next development came from the AO (Arbeitsgemeinschaft für Osteosynthesefragen) group with the advent of dorsal plate fixation in the 1970s. Initially, a conventional dynamic compression plate was used; however, later, a dedicated wrist fusion plate was introduced. 3
Wrist arthroplasty has been compared with wrist arthrodesis through retrospective matched cohort studies by Murphy et al and Nydick et al and through a systematic review. 4 5 6 Patients in the arthroplasty group showed a trend toward better performance of certain activities such as personal hygiene. 5 Pain scores, satisfaction, and complication rates were similar in both groups. 4 5 While Nydick et al reported better functional outcomes in the arthroplasty group, this was not detected in the study by Murphy et al. 4 5 These findings were partly reflected in the systematic review by Cavaliere and Chung. 6 No or mild pain was experienced by 90% of patients in the arthroplasty group and 98% of patients in the arthrodesis group. Satisfaction appeared comparable between groups. 6 The rates of major complication were higher in the arthroplasty group (25%) compared with the arthrodesis group (13%). Newer third-generation prostheses had a lower major complication rate (21%) than older generation implants. A functional range of motion, as defined by Palmer et al, 7 was achieved by patients in only 3 of the 14 studies in the review. The systematic review by Yeoh and Tourret had similar findings, with arthroplasty having higher complication rates and functional range of motion only achieved by the Maestro implant. 7 Maintenance of a range of motion is seen as the clear advantage of wrist arthroplasty, yet this benefit is not always reflected by objective assessment. The National Institute for Health and Care Excellence (NICE) has provided cautious recommendations for the use of total wrist arthroplasty by experienced surgeons in specialist centers with special arrangements for clinical governance, consent, and audit or research. 8 National Joint Registry data are limited to Norway and Australia currently.
Since the last comparative systematic review, there have been several new publications including data on contemporary fourth-generation implants and a new matched cohort study comparing wrist arthroplasty to arthrodesis. 4 9 10 11 12 13 14 15 The availability of this new data together with previously available studies presents an ideal opportunity to revisit the ongoing debate on the efficacy of wrist arthroplasty compared with arthrodesis. The proposed research questions forming the basis for this study are as follows: “Is there a functional benefit to performing a total wrist replacement instead of a total wrist fusion in adult patients with end-stage wrist arthritis? Is there any difference in secondary measures including pain, grip strength, and range of motion? Is there a difference between the two techniques in terms of adverse events and treatment failure?”
Methods
A study protocol was created prior to undertaking this systematic review. This protocol was approved by the Brighton and Sussex Medical School Research Governance and Ethics Committee. The protocol was published on the National Institute for Health Research PROSPERO database (CRD42017067377).
Inclusion and Exclusion Criteria
Studies were included if participants were adults over the age of 16 years. The underlying clinical diagnosis was arthritis of the wrist of any type. The two intervention categories compared in this study were total wrist arthroplasty and total wrist arthrodesis. Both, studies comparing the two treatment modalities and studies focusing on only one of the treatments, were included. Studies comparing either technique to another established technique, for example, total wrist arthrodesis to partial wrist arthrodesis, were excluded. Analysis by the generation of arthroplasty implant was also performed. The studies included were at a minimum “case series,” level IV evidence but also included cohort studies and randomized control trials. Exclusion criteria included patients having undergone revision operations, studies with less than five patients, and failure to report on any of the primary or secondary outcomes. The minimum acceptable duration of follow-up was set at 1 year. Only studies published in the English language were reviewed.
The types of outcome measures chosen for the review were based on the recommendations from OMERACT (Outcome Measures for Rheumatoid Arthritis Clinical Trials) for both rheumatoid arthritis and osteoarthritis. 16 17 The primary outcome was physical function, and the secondary outcome measures were pain, grip strength, range of motion, adverse events, and implant survival.
Search Strategy
The following databases where searched: OVID Medline, OVID Embase, Cochrane Central Register of Controlled Trials, CINAHL, and BNI. Two trial registers were also searched for relevant studies: ClinicalTrials.gov and the World Health Organization Clinical trials portal. Finally, the NICE database was also searched. The primary search date for all the above was chosen as June 2, 2017. A final repeat of the search was performed on January 20, 2018. The “PICOS” elements (Population, Intervention, Comparator, and Outcomes) were used to construct an effective search strategy. However, not all the elements were used: “Outcomes,” for example, was excluded from the search as it was felt too restrictive for the primary search. Only studies published in the English language were considered, and animal or cadaveric studies were excluded. No date restrictions were applied to maximize search numbers. Search terms included arthropathy, arthritis, osteoarthritis, wrist injury, arthroplasty, joint prosthesis, replacement, arthrodesis, and fusion. The search strategies are provided in Appendices A B C D .
Appendix A. OVID Medline search strategy (dates: 1946 to January 20, 2018).
| 1 | exp Arthritis/ |
| 2 | arthri*.ti,ab. |
| 3 | Osteoarthritis/ |
| 4 | osteoarthr*.ti,ab. |
| 5 | $arthri*.ti,ab. |
| 6 | (inflam* adj3 joint*).ti,ab. |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 |
| 8 | Wrist/ |
| 9 | Wrist Injuries/ |
| 10 | Wrist Joint/ |
| 11 | wrist*.ti,ab. |
| 12 | exp Carpal Bones/ |
| 13 | carpal.ti,ab. |
| 14 | scaphoid*.ti,ab. |
| 15 | lunate.ti,ab. |
| 16 | triquetrum.ti,ab. |
| 17 | pisiform.ti,ab. |
| 18 | trapezium.ti,ab. |
| 19 | trapezoid*.ti,ab. |
| 20 | capitate.ti,ab. |
| 21 | hamate.ti,ab. |
| 22 | 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 |
| 23 | 7 and 22 |
| 24 | arthroplasty/ or arthroplasty, replacement/ |
| 25 | replac*.ti,ab. |
| 26 | exp “Prostheses and Implants”/ |
| 27 | Joint Prosthesis/ |
| 28 | prosthe*.ti,ab. |
| 29 | 24 or 25 or 26 or 27 or 28 |
| 30 | Arthrodesis/ |
| 31 | arthrodes*.ti,ab. |
| 32 | fusion*.ti,ab. |
| 33 | 30 or 31 or 32 |
| 34 | 23 and 29 and 33 |
Appendix B. OVID EMBASE search strategy (dates: 1974 to January 20, 2018).
| 1 | exp arthropathy/ |
| 2 | exp arthritis/ |
| 3 | arthr*.ti,ab. |
| 4 | exp osteoarthritis/ |
| 5 | osteoarthr*.ti,ab. |
| 6 | $arthr*.ti,ab. |
| 7 | exp wrist injury/ |
| 8 | 1 or 2 or 3 or 4 or 5 or 6 or 7 |
| 9 | exp wrist/ |
| 10 | wrist.ti,ab. |
| 11 | exp carpal bone/ |
| 12 | carpal.ti,ab. |
| 13 | scaphoid*.ti,ab. |
| 14 | lunate.ti,ab. |
| 15 | triquetrum.ti,ab. |
| 16 | pisiform.ti,ab. |
| 17 | trapezium.ti,ab. |
| 18 | trapezoid*.ti,ab. |
| 19 | capitate.ti,ab. |
| 20 | hamate.ti,ab. |
| 21 | 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 |
| 22 | 8 and 21 |
| 23 | exp arthroplasty/ |
| 24 | arthroplasty.ti,ab. |
| 25 | exp joint prosthesis/ |
| 26 | prosthe*.ti,ab. |
| 27 | replac*.ti,ab. |
| 28 | 23 or 24 or 25 or 26 or 27 |
| 29 | arthrodesis/ |
| 30 | arthrodes*.ti,ab. |
| 31 | fusion.ti,ab. |
| 32 | 29 or 30 or 31 |
| 33 | 22 and 28 and 32 |
Appendix C. CINAHL search strategy (dates: 1981 to January 20, 2018).
| 1 | exp *ARTHRITIS/ |
| 2 | (arthr*).ti,ab |
| 3 | exp *OSTEOARTHRITIS/ |
| 4 | (osteoarthr*).ti,ab |
| 5 | (inflam* ADJ3 joint).ti,ab |
| 6 | *”WRIST INJURIES”/ |
| 7 | exp *WRIST/ |
| 8 | exp *”WRIST JOINT”/ |
| 9 | “CARPAL BONES”/ |
| 10 | (carpal).ti,ab |
| 11 | exp *”ARTHROPLASTY, REPLACEMENT”/ |
| 12 | (replac*).ti,ab |
| 13 | exp *”ORTHOPEDIC PROSTHESIS”/ |
| 14 | (prosthe*).ti,ab |
| 15 | exp *ARTHRODESIS/ |
| 16 | (arthrodes*).ti,ab |
| 17 | (fusion).ti,ab |
| 18 | (1 OR 2 OR 3 OR 4 OR 5 OR 8) |
| 19 | (6 OR 7 OR 9 OR 10) |
| 20 | (11 OR 12 OR 13 OR 14) |
| 21 | (15 OR 16 OR 17) |
| 22 | (18 AND 19 AND 20 AND 21) |
Appendix D. BNI search strategy (dates: 1992 to January 20, 2018).
| 1 | exp “ARTHRITIS AND RHEUMATISM”/ |
| 2 | (arthri*).ti,ab |
| 3 | (osteoarthr*).ti,ab |
| 4 | exp “JOINT DISORDERS”/ |
| 5 | (wrist).ti,ab |
| 6 | (arthroplasty).ti,ab |
| 7 | (replacement).ti,ab |
| 8 | (prosthesis).ti,ab |
| 9 | (arthrodesis).ti,ab |
| 10 | (arthrodes*).ti,ab |
| 11 | (fusion).ti,ab |
| 12 | (1 OR 2 OR 3 OR 5) |
| 13 | (6 OR 7 OR 8) |
| 14 | (9 OR 10 OR 11) |
| 15 | (4 AND 12 AND 13 AND 14) |
Data Collection and Analysis
The basic dataset was adapted from recommendations in the Cochrane Handbook for Systematic Review of Interventions. 18 Studies were selected through two stages of screening. The first stage involved a review of the study title and abstracts to remove obviously irrelevant articles. The full text of the remaining articles was then reviewed in more detail independently by the first author (O. B.) and another qualified researcher. Disagreement was resolved by the study supervisors (S. G. and L. G.). The risk of bias in studies was assessed with the Cochrane Collaboration's Risk of Bias tool. 18 A judgment of “low risk,” “high risk,” or “unclear risk” of bias was made. The GRADE system was chosen to perform a quality appraisal of case series. 19 This system specifies four levels of quality (high, moderate, low, very low).
The results of the literature search are summarized in Fig. 1 . Of the remaining 43 articles, 17 studies reported wrist arthrodesis outcomes, 3 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 24 reported the outcomes from wrist arthroplasty, 9 10 11 12 13 14 15 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 and 2 undertook a retrospective matched cohort review of arthroplasty versus arthrodesis. 4 5
Fig. 1.
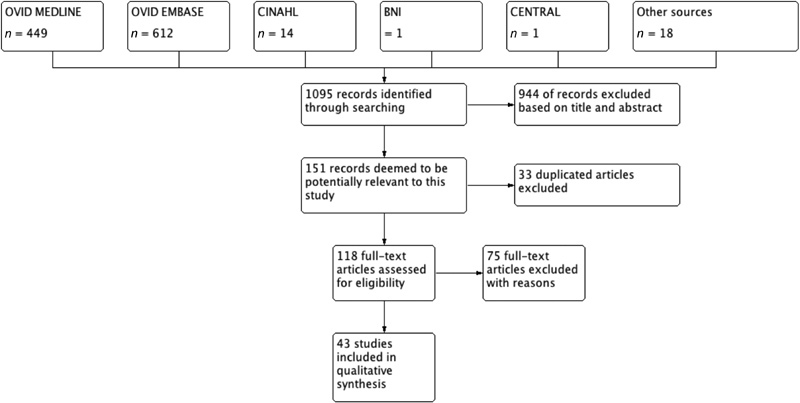
Summary of the study selection process according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Results
Table 1 summarizes the overall patient demographics. All arthrodesis studies were retrospective in nature apart from Riches et al, which was prospective. 26 Of the arthroplasty studies, seven were prospective in nature. 13 37 38 44 45 47 51
Table 1. Patient demographics.
| Total wrist arthrodesis | Total wrist arthroplasty | |
|---|---|---|
| Total number of patients | 603 | 1,295 |
| Total index operations | 669 | 1,371 |
| Male:female | 1:1.6 | 1:2.9 |
| Average age | 52.6 y | 58.4 y |
| Underlying pathology | ||
| Inflammatory arthritis | 71.6% | 72.7% |
| Rheumatoid arthritis | 70.9% | 63.2% |
| Psoriatic arthritis | 0.7% | 0.4% |
| Other | – | 0.3% |
| Not classified | – | 8.8% |
| Noninflammatory | 28.4% | 27.3% |
| Posttraumatic arthritis | 25.8% | 6% |
| Degenerative arthritis | – | 8.8% |
| Lunate AVN | 2.1% | 0.3% |
| Other | 0.5% | 0.2% |
| Not classified | 12.1% |
Abbreviation: AVN, avascular necrosis.
Note: Average age is calculated through weighted average.
A variety of wrist arthrodesis techniques were described in the studies and are summarized in Table 2 . In rheumatoid arthritis patients, Rush pin and staples were commonly used employing the technique widely advocated by Mannerfelt and Malsten. 2 20 22 29 30 32 The majority of the arthrodesis studies employed more than one surgical technique.
Table 2. A summary of the different wrist arthrodesis techniques employed by the studies included in the systematic review.
| Study | Arthrodesis technique | Underlying pathology | Number of index procedures | Length of follow-up (range) |
|---|---|---|---|---|
| Brumfield et al (1979) | Not defined | RA | 41 | 58 mo (>12 mo) |
| Vahvanen and Tallroth (1984) | Rush pin (modified from Mannerfelt and Malmsten (1971) No BG |
RA | 45 | 3.9 (1–11 y) |
| Vicar and Burton (1986) | Millender and Nalebuff (1973) technique including Darrach procedure | RA | 33 | 82 mo |
| Lee and Carroll (1994) | Intramedullary fixation with Steinman pin in third MC and K-wire second MC; ICBG | RA, n = 18; PA, n = 1 | 25 | 74 mo |
| Sauerbier et al (2000) | AO wrist fusion plate, n = 30; 3.5-mm DCP, n = 30; all with ICBG | Post-traumatic, n = 45; Kienböck's disease, n = 6 | 60 | 37 (15–120 mo) |
| Voutilainen et all (2001) | Self-reinforcing poly-L-lactide bioabsorbable implants; distal ulna resection as BG | RA, n = 17; PA, n = 1 | 21 | 5.4 (3–8 y) |
| Masada et al (2003) | Intramedullary fixation with two K-wires with ICBG; distal ulna resection | RA | 18 | 27 (13–68 mo) |
| De Smet and Truyen (2003) | Rayan (1986) technique: ICBG screw fixation, n = 24; AO/ASIF plate with ICBG, n = 12; Darrach procedure, n = 12 | Post-traumatic, n = 35; Kienböck's disease, n = 6 | 36 | 7 (4–9 y) |
| Rauhaniemi et al (2005) |
Mannerfelt and Malsten (1971),
n
= 113; Staples,
n
= 1; ICBG,
n
= 1, latter two as MC was too narrow.
Distal ulna resection in all cases Autograft (ICBG/ulna), n = 114 |
RA | 115 | 4 (1–6 y) |
| Adey et al (2005) |
Weiss and Hastings (1995): plate, 20 cases (DCP,
n
= 17; wrist fusion plate,
n
= 3; Synthes, Paoli, PA); screw arthrodesis,
n
= 2
Autograft (ICBG/ulna) in all cases |
OA (post-traumatic) | 22 | 6 (1.5–15 y) |
| Solem et al (2006) |
Mannerfelt and Malsten (1971) technique,
n
= 21; plate,
n
= 21 (AO plate,
n
= 11; Synthes plate,
n
= 9)
BG in most cases |
RA,
n
= 34; PA,
n
= 1;
Post-traumatic, n = 1; Kienböck's disease, n = 3; Unspecified, n = 1 |
42 | 10.5 (6–15 y) |
| Toma et al (2007) |
Mannerfelt and Malsten (1971) technique,
n
= 19; AO plate,
n
= 23
Distal ulna resection, n = 28/42 Autograft 40/42, allograft 2/42 |
RA | 42 | 76 (24–210 mo) |
| Lautenbach et al (2013) | Rush pin (modified from Mannerfelt and Malmsten 1971) No BG |
RA | 34 | 34 ± 28 mo |
| Fontaine et al (2014) | Rush pin and ICBG (modified from Lee and Carroll 1994) Distal ulna resection |
RA | 6 | 2.1 (1.5–3.6 y) |
| Onuma et al (2015) | Wrist fusion rod (Nakashima Medical, Okayama, Japan) Distal ulna excision as BG |
RA | 6 | 6 (2–9.2 y) |
| Owen et al (2016) | Wrist fusion plate (DePuy Synthes International; Leeds; United Kingdom) either with ICBG or distal ulna resection if DRUJ disease for BG |
RA,
n
= 24; PA,
n
= 1;
Post-traumatic, n = 38; Kienböck's, n = 3; Other, n = 2 |
68 | Median: 6 y (IQR: 3–11) |
| Riches et al (2016) | Not defined | RA | 16 | 3.5 (SD: ± 2 y) |
| Murphy et al (2003) | Dorsal wrist plate, 83%; other pin/rod fixation Autograft in most cases |
RA | 24 | 48 ± 25 mo |
| Nydick et al (2013) | Synthes wrist fusion plate (Synthes, West Chester, PA) | OA (post-traumatic) | 15 | 68 ± 36 mo |
| Total | 669 |
Abbreviations: AO, Arbeitsgemeinschaft für Osteosynthesefragen; BG, bone graft; DCP, dynamic compression plate; DRUJ, distal radioulnar joint; ICBG, iliac crest bone graft; IQR, interquartile range; K-wire, Kirschner wire; MC, metacarpal; PA, psoriatic arthritis; RA, rheumatoid arthritis; SD, standard deviation.
Table 3 provides a summary of the different implants used throughout the arthroplasty studies. There were a total of 14 different implants used, ranging from earlier second-generation prostheses, such as Volz and Motec, to contemporary fourth-generation systems such, as Universal 2 and Maestro.
Table 3. A summary of the different wrist arthroplasty implants used in the studies included in the systematic review.
| Study | Wrist arthroplasty implant | Underlying pathology | Generation of implant | Number of index procedures | Length of follow-up (range) |
|---|---|---|---|---|---|
| Menon (1987) | Volz (Howmedica, Rutherford, NJ) | RA, n = 14; PA, n = 1; OA, n = 1 | Second | 18 | 40 (24–66 mo) |
| Menon (1988) | Universal (Kinetikos Medical, San Diego, CA) | RA, n = 23; OA, n = 8 | Third | 37 | 79.4 (48–120 mo) |
| Figgie et al (1990) | Trispherical | RA | Third | 35 | 9 (5–11 y) |
| Meuli and Fernandez (1995) | MWP II Meuli | RA, n = 33; Post-traumatic, n = 12 | Second | 49 | 4.5 (2–6 y) |
| Gellman et al (1997) | Volz (Howmedica) | RA, =12; PA, n = 1; Post-traumatic, n = 1 | Second | 14 | 6.5 (3.5–11.5 y) |
| Takwale et al (2002) | Biaxial (DePuy Orthopaedics Inc, Leeds, United Kingdom) | RA | Third | 66 | 52 (12–99 mo) |
| Divelbiss et al (2002) | Universal (Kinetikos Medical) | RA | Third | 22 | 1–2 y |
| Levadoux and Legré (2003) | Destot | OA (post-traumatic) | Third | 28 | 47 (12–72 mo) |
| Rahimtoola and Rozing (2003) | RWS (Howmedica, Pfizer Hospital Products Group) | RA, n = 24; PA, n = 1; OA, n = 2 | Second | 27 | 4 (2–8 y) |
| Radmer et al (2003) | APH (Implant-Service Vertriebs-GmbH, Hamburg, Germany) | Seropositive RA, n = 36; seronegative RA, n = 4 | Third | 40 | 52 (24–73 mo) |
| Ward et al (2011) | Universal (KMI, Carlsbad, CA) | RA | Third | 19 | 7.3 (5–10.8 y) |
| Reigstad et al (2011) | Motec (Elos Medical AB, Timmersdala, Sweden) | Post-traumatic arthritis including SLAC/SNAC | Second | 8 | 7.6 (7–9 y) |
| Ferreres et al (2011) | Universal 2 (Integra Lifesciences, Plainsboro, NJ), n = 19 | Inflammatory including RA, n = 15; Psoriatic, n = 1; and other, n = 2; | Fourth | 21 | 5.5 (3–8 y) |
| Universal (KMI), n = 2 | Noninflammatory including Kienböck's disease, n = 2; other, n = 2 | Third | |||
| Krukhaug et al (2011) | Biaxial, n = 90 (80/90 uncemented) (DePuy, Warsaw, IN) |
Inflammatory (RA, PA),
n
= 116;
Noninflammatory (OA, post-traumatic, ligamentous, post-infective), n = 73 |
Third | 189 | |
| Elos, n = 23 (three versions preceding Gibbon, v1 = v2; v2 = 6; v3 = 15) | Third | ||||
| Gibbon, n = 76 (Swemac, Linkoping, Sweden, later called Motec) | Third | ||||
| Cooney et al (2012) | Biaxial, n = 16 |
RA,
n
= 29;
Post-traumatic, n = 10 |
Third | 46 | 6 (3.5–15 y) |
| Re-Motion (Small Bone Innovations Inc., Morrisville, PA), n = 22 | Fourth | ||||
| Universal 2 n = 8 | Fourth | ||||
| Ekroth et al (2012) | Biaxial, n = 6 (Biomet, Warsaw, IN) | RA | Third | 12 | 17.8 (11.7–28.3 y) |
| Volz, n = 1 (Stryker, Mahwah, NJ) | Second | ||||
| Bidwai et al (2013) | Re-Motion (Small Bone Innovations Inc.) | RA | Fourth | 13 | 33 (14–56 mo) |
| Herzberg et al (2012) | Re-Motion (Small Bone Innovations Inc.) |
RA,
n
= 129 (60%);
Non-RA, n = 86 (40%) |
Fourth | 215 | 4 (2–8 y) |
| Boeckstyns et al (2013) | Re-Motion (Small Bone Innovations Inc.) | RA, n = 50; OA, n = 6; post-traumatic, n = 8; Kienböck's disease, n = 1 | Fourth | 52 | 6.5 (5–9 y) |
| Sagerfors et al (2015) | Biaxial, n = 52 (DePuy Orthopedics, Warsaw, IN) | RA, n = 185; OA, n = 34 | Third | 219 | 7 (2–13 y) |
| Universal 2 n = 12 (Integra Lifesciences) | Fourth | ||||
| Re-Motion, n = 87 (Stryker, Kalamazoo, MI) | Fourth | ||||
| Maestro, n = 68 (Biomet) | Fourth | ||||
| Badge et al (2016) | Universal 2 (Integra Lifesciences) | RA | Fourth | 95 | 53 (24–120 mo) |
| Chevrollier et al (2016) | Universal, n = 10 (KMI) | RA, n = 6; Other, n = 1; Post-traumatic, n = 8; Kienbock's disease, n = 1, Post-septic, n = 1 | Third | 17 | 5.2 (1.1–10 y) |
| Re-Motion, n = 7 (SBI, Morrisville, PA) | Fourth | ||||
| Gil et al (2017) | Universal 2 (Integra Lifesciences) | RA, n = 29; PA, n = 1; JIA, n = 1; Degenerative OA (including post-traumatic), n = 8 | Fourth | 39 | 9 (4.8–14.7 y) |
| Reigstad et al (2017) | Motec (Swemac Orthopaedics AB, Linkoping, Sweden) | OA Degenerative | Second | 56 | 8 (5–11 y) |
| Murphy et al (2003) | Universal (KMI) | RA | Third | 27 | 26 ± 16 mo |
| Nydick et al (2013) | Maestro (Biomet) | OA (post-traumatic) | Fourth | 7 | 56 ± 10 mo |
| Total | 1,371 |
Abbreviations: JIA, juvenile idiopathic arthritis; OA, osteoarthritis; PA, psoriatic arthritis; RA, rheumatoid arthritis; SNAC, scaphoid nonunion advanced collapse; SLAC, scapholunate advanced collapse.
A common issue across most studies was the lack of blinding of study personnel, therefore creating a performance and detection bias. Several study authors were involved in product design. 38 39 42 46 47 51 while, Divelbiss et al received benefits for their work. 44 Both issues create a conflict of interest and a potential detection bias. Several studies had missing outcome data, including Owen et al, where only 59% of functional outcome data were available. 25 The GRADE quality assessment was generally very low to low, as most studies were retrospective observational studies, with no blinding, often with missing data or high patient loss to follow-up numbers. 19 Several studies, however, had a low risk of bias, and the reported outcome effect sizes were sufficient to qualify the studies as of moderate grade. 3 4 5 12 13 15 26 30 31 49 51 The GRADE assessment is summarized in Appendix E .
Appendix E. A summary of the quality of evidence of articles included in this systematic review (grading according to the GRADE system 19 ) .
| Arthrodesis study | Grade of evidence | Arthroplasty study | Grade of evidence |
| Brumfield et al (1979) | VL | Menon (1987) | VL |
| Vahvanen and Tallroth (1984) | VL | Menon (1988) | VL |
| Vicar and Burton (1986) | VL | Figgie et al (1990) | VL |
| Lee and Carroll (1994) | VL | Meuli and Fernandez (1995) | VL |
| Sauerbier et al (2000) | M | Gellman et al (1997) | VL |
| Voutilainen et all (2001) | L | Takwale et al (2002) | L |
| Masada et al (2003) | VL | Divelbiss et al (2002) | VL |
| De Smet and Truyen (2003) | M | Levadoux and Legré (2003) | VL |
| Rauhaniemi et al (2005) | VL | Rahimtoola and Rozing (2003) | L |
| Adey et al (2005) | VL | Radmer et al (2003) | L |
| Solem et al (2006) | VL | Ward et al (2011) | L |
| Toma et al (2007) | M | Reigstad et al (2011) | VL |
| Lautenbach et al (2013) | L | Ferreres et al (2011) | L |
| Fontaine et al (2014) | L | Krukhaug et al (2011) | M |
| Onuma et al (2015) | L | Cooney et al (2012) | VL |
| Owen et al (2016) | L | Ekroth et al (2012) | VL |
| Riches et al (2016) | M | Bidwai et al (2013) | VL |
| Herzberg et al (2012) | L | ||
| Boeckstyns et al (2013) | M | ||
| Sagerfors et al (2015) | M | ||
| Badge et al (2016) | VL | ||
| Chevrollier et al (2016) | M | ||
| Gil et al (2017) | VL | ||
| Reigstad et al (2017) | M | ||
| Murphy et al (2003) | M | ||
| Nydick et al (2013) | M |
Abbreviations: L, low; M, medium; VL, very low.
Is There a Functional Benefit to Performing a Total Wrist Replacement Instead of a Total Wrist Fusion in Adult Patients with End-Stage Wrist Arthritis?
Functional outcomes were poorly reported across the studies, and often nonvalidated assessment tools were used. The DASH (Disabilities of the Arm, Shoulder and Hand) functional score (range 0–100, where 0 is good function and 100 is poor function) was most commonly used, a summary of which is presented in Tables 4 and 5 . 53
Table 4. A summary of the DASH scores for the arthrodesis studies.
| Study | Arthrodesis technique | Preoperative DASH score | Postoperative DASH score (range) |
Notes |
|---|---|---|---|---|
| Sauerbier et al (2000) | AO wrist fusion plate, n = 30; 3.5-mm DCP, n = 30 | – | 51.4 | DASH part A (function) = 48.57 DASH part B (symptoms) = 61.03 |
| De Smet and Truyen (2003) | Rayan (1986) technique: ICBG screw fixation, n = 24; AO/ASIF plate, n = 12 | – | 44 (SD: 22) | |
| Adey et al (2005) | DCP, n = 17, wrist fusion plate, n = 3 (Synthes, Paoli, PA); screw arthrodesis, n = 2 | – | 25 (4–43) | Poor correlation with pain ( r = 0.36; p < 0.05) |
| Solem et al (2006) | Mannerfelt and Malsten (1971) technique, n = 21; plate, n = 21 (AO plate, n = 11; Synthes plate, n = 9) | – | Overall: 38 (2–75) Plate: 33 (5–57) Mannerfelt: 43 (2–75) |
One fused wrist: 36 (2–75) Bilateral fused wrists: 42 (18–68) All scores nonsignificant |
| Lautenbach et al (2013) | Rush pin (Modified from Mannerfelt and Malmsten 1971) | – | 63.3 ± 25.3 | Good correlation with pain ( r = 0.63) |
| Owen et al (2016) | Wrist fusion plate (Synthes, DePuy International, Leeds, United Kingdom) | Median ay 6 y: 19 (IQR: 7–45) |
Significant association of higher DASH with inflammatory arthritis (
p
= 0.005)
PRWE at 6 y: 13 (IQR: 1–31) |
|
| Murphy et al (2003) | Wrist arthrodesis (dorsal wrist plate 83%; other pin/rod fixation) vs. arthroplasty (Universal, KMI, San Diego, CA) | – | No difference between arthrodesis and arthroplasty | No difference between groups for PRWE |
| Nydick et al (2013) | Synthes wrist fusion plate (Synthes, West Chester, PA) vs. arthroplasty (Maestro, Biomet, Warsaw, IN) | Arthrodesis: 38 Arthroplasty: 29 |
No difference between groups Note: PRWE significantly better for arthroplasty ( p = 0.01) |
Abbreviations: AO, Arbeitsgemeinschaft für Osteosynthesefragen; BG, bone graft; DASH, Disabilities of the Arm, Shoulder and Hand; DCP, dynamic compression plate; ICBG, iliac crest bone graft; IQR, interquartile range; PRWE, patient-reported wrist evaluation; SD, standard deviation.
Note: DASH scores are presented as the mean (range) unless otherwise stated. r : Pearson's correlation coefficient.
Table 5. A summary of the DASH and QuickDASH scores for the arthroplasty studies.
| Study | Arthroplasty technique | Preoperative DASH score (range) | Postoperative DASH score (range) | Notes |
|---|---|---|---|---|
| Divelbiss et al (2002) | Universal | 46 |
1 y: 32.1 (
p
< 0.05)
2 y: 22.4 (8 wrists) |
Significant improvement at 1 y |
| Ward et al (2011) | Universal | 62 (42–80) | Mean: 7.8 y Median: 40 (18–80) |
|
| Reigstad et al (2011) | Motec | – | Mean 7.6 y Median: 10.3 (1.7–71.2) |
|
| Cooney et al (2012) |
Biaxial,
n
= 16
Re-Motion, n = 22 Universal 2, n = 8 |
– |
Biaxial (
n
= 8) = 48
Re-Motion ( n = 16) = 37 Universal 2 ( n = 7) = 20 |
DASH scores not available for all cases No significant difference between implants ( p = 0.07) |
| Ekroth et al (2012) |
Biaxial,
n
= 6
Volz, n = 1 |
– | 60.7 | 5/7 wrists revised to arthrodesis DASH for arthrodesis patients: 46.2 |
| Herzberg et al (2012) | Re-Motion | – | % Improvement: rheumatoid, 20; nonrheumatoid, 21 | No significant difference between rheumatoid and nonrheumatoid patients |
| Boeckstyns et al (2013) | Re-Motion | QuickDASH median: 58 (14–89) | QuickDASH median: 42 (0–84) | Significant improvement: p = 0.001 |
| Sagerfors et al (2015) |
Biaxial,
n
= 52
Universal 2, n = 12 Re-Motion, n = 87 Maestro, n = 68 |
Biaxial: 12.8 (–21.9 to 4.2) Universal 2: 13.7 (–27.1 to –6.2) Re-Motion: -12.3 (–25.5 to –1.4) Maestro: –16.8 (–29.5 to –5.3) |
Scores reported are preoperative minus postoperative at 5 y (median and interquartile range) All changes significant at p < 0.05 PRWE and COPM also significant ( p < 0.05) |
|
| Badge et al (2016) | Universal 2 | QuickDASH ( n = 40) = 61.3 (range: 16–91) | QuickDASH ( n = 59) = 45.8 (0–89) |
Significant improvement:
p
< 0.001
Wrightington wrist score also significant ( p < 0.001) |
| Chevrollier et al (2016) |
Universal,
n
= 10
Re-Motion, n = 7 |
QuickDASH = 29% (2.3–65.9%) | PRWE = 26% (range: 2–55.3%) | |
| Reigstad et al (2017) | Motec | QuickDASH 39 (SD: 18) | 25 (SD: 19) | p < 0.05 |
Abbreviations: COPM, Canadian Occupational Performance Measure; DASH, Disabilities of the Arm, Shoulder and Hand; PRWE, patient-reported wrist evaluation; SD, standard deviation.
Note: Scores are presented as the mean (range) unless otherwise stated.
In Sauerbier et al's study of wrist arthrodesis performed using either an AO wrist fusion plate or a conventional dynamic compression plate, 80% of patients reported difficulties with personal hygiene and 70% felt less capable. 3 Patients with inflammatory arthritis, in particular polyarticular disease, had a higher/poorer DASH score compared with those with noninflammatory disease ( p = 0.005). 25 A poorer DASH score has also been correlated with increased pain postoperatively ( r = 0.63). 20 Riches et al using the M-SACRAH (Modified Score for the Assessment and Quantification of Chronic Rheumatic Affections of the Hands) score reported a significant improvement in the function, stiffness, and pain domains ( p < 0.001) following arthrodesis. 26
Several arthroplasty studies reported a significant improvement in outcome scores following surgery ( Table 5 ). 12 44 51 Sagerfors et al observed this improvement up to 5 years after surgery in outcome measures also including the Canadian Occupational Performance Measure (COPM) and patient-reported wrist evaluation (PRWE). 13 In addition, Herzberg et al and Boeckstyns et al reported no statistically significant difference in the QuickDASH score for wrist arthroplasty performed in either rheumatoid or nonrheumatoid patients. 12 52
Is There Any Difference in Secondary Measures Including Pain, Grip Strength, and Range of Motion?
A statistically significant improvement in pain scores was seen in four arthrodesis studies ( Table 6 ), 3 20 26 32 and five arthroplasty studies ( Table 7 ). 12 13 14 45 50 51 Generally, postoperative scores across both arthrodesis and arthroplasty studies demonstrated a good level of pain control.
Table 6. A summary of the pre- and postoperative pain scores in the arthrodesis studies.
| Study | Arthrodesis technique | Preoperative pain score (mean unless otherwise stated) | Postoperative pain score (mean unless otherwise stated) | Pain score scale |
|---|---|---|---|---|
| Vicar and Burton (1986) | Millender and Nalebuff (1973) technique | Severe: 9 Moderate: 7 Mild: 3 None: 0 |
Severe: 0 Moderate: 0 Mild: 10 None: 22 |
|
| Lee and Carroll (1994) | Steinman pin and K-wire | 2.6, rest; 3.1, activity | 1.1 rest, 1.1 activity | 1–4 severe |
| Sauerbier et al (2000) | AO wrist fusion plate or 3.5-mm DCP | 58 | 16.5 ( p < 0.05) | 0–100 severe |
| Rauhaniemi et al (2005) | Mannerfelt and Malsten (1971); staples, n = 1; ICBG, n = 1 | 3.6 | 1 y: 1.3 (range: 1–4) ( p < 0.001) | 1–4 severe |
| Lautenbach et al (2013) | Mannerfelt and Malsten (1971) | 7.9 (range: 0–10) | 1.9 (range: 0–9) ( p < 0.01) | 0–10 severe |
| Onuma et al (2015) | Wrist fusion rod | 8 ± 1.1 | 1 ± 0.9 | 0–10 severe |
| Riches et al (2016) | Not defined | 90 ± 33 | 8 ± 12 ( p < 0.001) | 0–100 severe |
Abbreviations: AO, Arbeitsgemeinschaft für Osteosynthesefragen; DCP, dynamic compression plate; ICBG, iliac crest bone graft; K-wire, Kirschner wire.
Note: The scale of the scoring system is given unless a Likert system was used.
Table 7. A summary of the pre- and postoperative pain scores in the arthroplasty studies.
| Study | Arthroplasty technique | Preoperative pain score (mean unless otherwise stated) | Postoperative pain score (mean unless otherwise stated) | Pain score scale |
|---|---|---|---|---|
| Rahimtoola and Rozing (2003) | RWS | Moderate or Severe: 22 Mild: 4 Occasional: 1 |
Mild or Occasional: 10 Significant improvement ( p < 0.002) |
|
| Cooney et al (2012) |
Biaxial,
n
= 16
Re-Motion, n = 22 Universal 2, n = 8 |
7 | 2.3 | 0–10 severe |
| Boeckstyns et al (2013) | Re-Motion | 67 (SD: 17) | 27 (SD: 29) ( p = 0.001) | 0–100 severe |
| Sagerfors et al (2015) |
Biaxial,
n
= 52
Universal 2, n = 12 Re-Motion, n = 87 Maestro, n = 68 |
Significant improvement at rest and activity at 5 y ( p < 0.05) | 0–10 severe | |
| Badge et al (2016) | Universal 2 | 8.1 (range: 3–10) | 5.4 (range: 0–10) ( p < 0.001) | 0–10 severe |
| Gil et al (2017) | Universal 2 | 8.6 ± 1.2 | 0.4 ± 0.8 ( p < 0.001) | 0–10 severe |
| Reigstad et al (2017) | Motec | Radially rest: 34 (SD: 23) Active: 69 (SD: 20) |
Radially rest: 8 (SD: 14) Active: 20 (SD: 22) ( p < 0.05) |
0–100 severe |
Abbreviation: SD, standard deviation.
Note: The scale of the scoring system is given unless a Likert system was used.
The general trend is for an improvement in grip strength. There was a statistically significant increase in only a few studies. 12 13 14 31 51 The grip strength compared with the normal contralateral side in wrist arthrodesis ranges from 50 to 79% and in arthroplasty ranges from 58 to 72%. 3 15 31 33 38 Reigstad et al noted an average increase from 20 kg preoperatively to 24 kg on average follow-up in their series of patients undergoing wrist arthroplasty. 51 Following an arthrodesis, a good range of pronation (range: 73–83 degrees) and supination (range: 68–71 degrees) is maintained ( Table 8 ). 3 30 35 Only two studies reported a gain in range of motion to functional levels as reported by Palmer et al. 54 Levadoux and Legré, in their series of wrist arthroplasty with the Destot prosthesis, and Herzberg et al with use of the Re-Motion wrist in their nonrheumatoid patient subgroup. 39 52
Table 8. A summary of the range of motion (all measures in degrees).
| Study | Technique | Flexion | Extension | Radial deviation | Ulna deviation | Pronation | Supination | Total active range |
|---|---|---|---|---|---|---|---|---|
| Vicar and Burton (1986) | Millender and Nalebuff (1973) technique | – | – | – | 77 (30–90) | 68 (10–90) | – | |
| Sauerbier et al (2000) | AO wrist fusion plate or 3.5-mm DCP | – | – | – | – | 83 | 71 | – |
| Toma et al (2007) | Mannerfelt and Malsten (1971) technique or AO plate | – | – | – | – | 73 (45–90) | 70 (40–90) | – |
| Menon (1987) | Volz | 50.3 (15–80) | 24.7 (–80 to 50) | –0.4 (–22 to 20) | 20.3 (0–35) | – | – | – |
| Menon (1988) | Universal | 41 (SD: 15) a | 36 (SD: 16) | – | – | – | – | – |
| Figgie et al (1990) | Trispherical | – | – | 10 (0–15) | 10 (0–15) | – | – | F/E arc: 50 (0–105) |
| Meuli and Fernandez (1995) | MWP II Meuli | 30 (10–70) | 40 (20–70) | 10 (0–20) | 10 (0–30) | 85 (70–90) | 85 (75–90) | |
| Gellman et al (1997) | Volz | 18.2 (0–40) 10.3 (0–25) | 10.3 (0–25) | 7.8 (0–25) | 13.2 (5–45) | – | – | F/E arc: 26.6 (10–55) |
| Takwale et al (2002) | Biaxial | 17.4 | 28.8 | 6 | 13. | 43.5 | ||
| Divelbiss et al (2002) | Universal | 41 b | 35 b | 9 | 19 | 88 b | 80 b | – |
| Levadoux and Legré (2003) | Destot | 48 (10–70) | 41 (30–50) | 12 (5–20) | 22 (10–30) | 90 | (50–90) | – |
| Rahimtoola and Rozing (2003) | RWS | 35 (0–80; SD: 17) a | 24 (0–45; SD: 15) a | 10 (–15 to 45; SD: 12) a | 15 (–10 to 45; SD: 13) | 83 (35–90; SD: 15) | 57 (10–90; SD: 26) | 60 |
| Radmer et al (2003) | APH | 5 (–10 to 20, SD: 9) | 10 (0–30, SD: 4) | –20 (–30 to –5, SD: 7) | 25 (10–35, SD: 5) | 80 (75–90, SD: 4) | 75 (50–85, SD: 6) | – |
| Ward et al (2011) | Universal | 42 (30–55) | 20 (–20–45) | 8 (0–35) | 17 (–20–32) | 83 (60–90) b | 71 (40–90) | F/E arc: 62 (30–90) |
| Reigstad et al (2011) | Motec | – | – | – | – | – | – | F/E/R/U: 125 (100–48) |
| Ferreres et al (2011) | Universal 2 (Universal, n = 2) |
42 (SD: 10) | 26 (SD: 14) | 1 (SD: 7) | 26 (SD: 9) | F/E arc: 68 | ||
| Cooney et al (2012) | Biaxial Re-Motion Universal 2 |
30 | 38 | 8 | 20 | 75 | 70 | – |
| Ekroth et al (2012) | Biaxial Volz |
– | – | – | – | – | – | P/S arc: 133.5 |
| Bidwai et al (2013) | Re-Motion | 22.5 | 34.5 | 6.81 | 15.46 | – | – | F/E arc: 47.44 |
| Herzberg et al (2012) | Re-Motion | Rheumatoid: 29 Nonrheumatoid: 37 |
29 36 |
5 10 |
24 28 |
|||
| Boeckstyns et al (2013) | Re-Motion | 29 (SD: 19) | 31 (SD: 18) | 6 (SD: 8) | 22 (SD: 14) b | 81 (SD: 11) | 83 (SD: 12) b | – |
| Sagerfors et al (2015) | Biaxial Universal 2 Re-Motion Maestro |
No significant improvement. | Significant improvement for Biaxial and Maestro only | Significant improvement for Maestro only | Significant improvement for Maestro and Re-Motion | Significant improvement for Biaxial | Significant improvement for Re-Motion | |
| Badge et al (2016) | Universal 2 | 30.7 (0–50) a | 29.1 (0–70) b | 4 (–10–15) | 14.2 (0–30) | 81.5 (45–90) | 76.1 (20–90) | – |
| Chevrollier et al (2016) | Universal Re-Motion |
– | – | – | – | – | F/E arc: 33 (18–57) | |
| Gil et al (2017) | Universal 2 | 37 (SD: 14) | 29 (SD: 13) | |||||
| Reigstad et al (2017) | Motec | 83 (SD: 7) | 83 (SD: 11) | 126 (SD: 37) b |
Abbreviations: F/E, flexion–extension; P/S, pronation-supination; R/U, radial–ulna; SD, standard deviation.
Note: Figures in bold represent significant post-operative improvement in range.
p < 0.001.
p < 0.05.
Is There a Difference between Adverse Events and Treatment Failure?
Complications rates were higher in arthroplasty patients (range: 0.2–9.5%) than in arthrodesis patients (range: 0.1–6.1%) ( Table 9 ). This did not reach significance, however ( p = 0.1). Subgroup analysis of the newer fourth-generation implants revealed a significantly lower complication rate (range: 0.1–2.9%) compared with second- and third-generation arthroplasty cases (range: 0.2–8.1%; p = 0.002). There was no significant difference in complication rates between arthrodesis and fourth-generation wrist arthroplasty ( p = 0.06). Metalwork-related issues contributed to the majority of complications in the arthrodesis group. This included metalwork prominence requiring removal in 6.1% of cases. Osteolysis was a major issue in wrist arthroplasty, typically on the carpal side (9.5%) rather than radial side (3.2%). This is less of an issue with more recent fourth-generation implants (carpal osteolysis: 1.2%; radial osteolysis: 0.7%).
Table 9. Specific complication rates (results given in percentage).
| Complication | Arthrodesis (total cases: 669) |
All arthroplasty (total cases: 1,371) |
Second- and third-generation prosthesis (total cases: 720) | Fourth-generation prosthesis (total cases: 651) |
|---|---|---|---|---|
| Fracture | 0.1 | 1 | 0.6 | 0.4 |
| Nerve problems | 2.7 | 1.1 | 0.9 | 0.2 |
| CRPS | 0.1 | 0.2 | 0.2 | – |
| Wound problems | 2.1 | 1.4 | 1.1 | 0.3 |
| Superficial infection | 0.7 | 0.7 | 0.5 | 0.3 |
| Deep infection | 0.9 | 1.6 | 1.4 | 0.1 |
| Tendon problems | 1.8 | 1.2 | 0.7 | 0.5 |
| Impingement | 1.4 | 1.6 | 1.5 | 0.1 |
| Stiffness | 0.1 | 1.4 | 0.4 | 1 |
| Metalwork prominence | 2.3 | – | – | – |
| Metalwork breakage | 1.4 | 0.4 | 0.4 | – |
| Metalwork removal | 6.1 | – | – | – |
| Instability | – | 1.5 | 1.5 | – |
| Dislocation | – | 2.4 | 2.1 | 0.3 |
| Radiological | ||||
| Failure of arthrodesis | 2.6 | – | – | – |
| Radial osteolysis | – | 3.2 | 2.4 | 0.7 |
| Carpal/metacarpal osteolysis | 3.7 | 9.5 | 8.1 | 1.2 |
| General osteolysis | 0.9 | 8.2 | 5.5 | 2.9 |
| Implant migration | 0.6 | 1.7 | 1.7 | – |
| Other (e.g., screw loosening, malalignment, polyethylene liner wear) | – | 2.4 | 2.3 | 0.4 |
| Range | 0.1–6.1% a b | 0.2–9.5% a | 0.2–8.1% c | 0.1–2.9% b c |
| Total | 28% | 31% | 47% | 13% |
Abbreviation: CRPS, chronic regional pain syndrome.
Mann–Whitney U test: no significant difference ( p = 0.1) between arthrodesis and arthroplasty.
Mann–Whitney U test: no significant difference ( p = 0.06) between arthrodesis and fourth-generation implants.
Mann–Whitney U test: significant difference ( p = 0.002) between second- and third-generation implants and fourth-generation implants.
If the study by Radmer et al was excluded from analysis, implant revision rates ranged from 3.5 to 52.6%, and the rate of conversion to arthrodesis ranged from 0 to 42.1% ( Table 10 ). 48 The former study demonstrated a 100% revision rate to arthrodesis.
Table 10. Revision rates and conversion to arthrodesis rates for arthroplasty.
| Study | Implant | Implant generation | Revision rate (%) | Conversion to arthrodesis (%) | Length of follow-up |
|---|---|---|---|---|---|
| Menon (1987) | Volz | Second | 33 | 0 | 40 (24–66 mo) |
| Menon (1988) | Universal | Third | 26 | 5.4 | 79.4 (48–120 mo) |
| Figgie et al (1990) | Trispherical | Third | 5.7 | 5.7 | 9 (5–11 y) |
| Meuli and Fernandez (1995) | MWP II Meuli | Second | 18 | 12.2 | 4.5 (2–6 y) |
| Gellman et al (1997) | Volz | Second | 13.3 | 7.1 | 6.5 (3.5–11.5 y) |
| Takwale et al (2002) | Biaxial | Third | 7.6 | 4.5 | 52 (12–99 mo) |
| Divelbiss et al (2002) | Universal | Third | 18.2 | 4.5 | 1–2 y |
| Levadoux and Legré (2003) | Destot | Third | 14.3 | 14.3 | 47 (12–72 mo) |
| Rahimtoola and Rozing (2003) | RWS | Second | 3.7 | 3.7 | 4 (2–8 y) |
| Radmer et al (2003) | APH | Third | 100 | 100 | 52 (24–73 mo) |
| Ward et al (2011) | Universal | Third | 52.6 | 42.1 | 7.3 (5–10.8 y) |
| Reigstad et al (2011) | Motec | Second | 37.5 | 25 | 7.6 (7–9 y) |
| Ferreres et al (2011) |
Universal 2,
n
= 19
Universal, n = 2 |
Fourth | 4.8 | 0 | 5.5 (3–8 y) |
| Krukhaug et al (2011) | Biaxial, n = 90 (80/90 uncemented) | Third | 21 (Elos = 10; Gibbon = 11; Biaxial = 18) | 0 | |
| Elos, n = 23 | Third | ||||
| Gibbon, n = 76 | Third | ||||
| Cooney et al (2012) | Biaxial, n = 16 | Third | 19.6 (Biaxial = 8; Universal 2 = 1) | 13 | 6 (3.5 - 15 y) |
| Re-Motion, n = 22 | Fourth | ||||
| Universal 2, n = 8 | Fourth | ||||
| Ekroth et al (2012) | Biaxial, n = 6 | Third | 41.7 | 41.7 | 17.8 (11.7–28.3 y) |
| Volz, n = 1 | Second | ||||
| Reigstad et al (2011) | Motec | Second | 6.7 | 6.7 | 3.2 (1.1–6.1 y) |
| Bidwai et al (2013) | Re-Motion | Fourth | 7.7 | 0 | 33 (14–56 mo) |
| Herzberg et al (2012) | Re-Motion | Third | 5.1 | 2.3 | 4 (2–8 y) |
| Boeckstyns et al (2013) | Re-Motion | Fourth | 9.6 | 5.8 | 6.5 (5–9 y) |
| Sagerfors et al (2015) |
Biaxial,
n
= 52
Universal, 2 n = 12 |
Third Fourth |
8.7 | 0 | 7 (2–13 y) |
| Re-Motion, n = 87 | Fourth | ||||
| Maestro, n = 68 | Fourth | ||||
| Badge et al (2016) | Universal 2 | Fourth | 3.5 | 3.5 | 53 (24–120 mo) |
| Chevrollier et al (2016) | Universal, n = 10 | Third | 23.5 | 17.6 | 5.2 (1.1–10 y) |
| Re-Motion, n = 7 | Fourth | ||||
| Gil et al (2017) | Universal 2 | Fourth | 7.7 | 0 | 9 (4.8–14.7 y) |
| Reigstad et al (2017) | Motec | Second | 14.2 | 7.1 | 8 (5–11 y) |
| Murphy et al (2003) | Universal | Third | 3.7 | 3.7 | 26 ± 16 mo |
| Nydick et al (2013) | Maestro | Fourth | 14.3 | 14.3 | 56 ± 10 mo |
| Range a | 3.5–52.6% a | 0–42.1% a |
Excluding Radmer et al (2003).
Survival of Wrist Arthroplasty
Increasing data on implant survival are now available. Survival is defined as revision of the index procedure for any cause. Table 11 summarizes the latest figures. The worst performing implant appears to be the Biaxial, with survival as low as 50% in one study, 10 although other studies have shown survival rates of 81 to 85% at 5 to 8 years 13 43 49 and 78% at 12 years. 13 The Motec metal on metal implant, used specifically in osteoarthritic patients, is performing at 86% survival at 10 years. 51 The three other currently available implants are Universal 2 with 78% survival at 15 years, Re-Motion with 94% survival at 8 years, and Maestro with a survival of 95% at 8 years. 10 13 50
Table 11. Implant survival.
| Study | Implant | Survival | |
|---|---|---|---|
| Takwale et al (2002) | Biaxial | 83% at 8 y | |
| Krukhaug et al (2011) | 85% at 5 y | ||
| Cooney et al (2012) | 50% at 6 y | ||
| Sagerfors et al (2015) | 81% at 8 y | 78% at 12 y | |
| Levadoux and Legré (2003) | Destot | 85% 4 y | |
| Radmer et al (2003) | APH | 100% failure at 52 mo (range: 24–73) | |
| Krukhaug et al (2011) | Elos | 57% at 5 y | |
| Krukhaug et al (2011) | Gibbon | 77% at 4 y | |
| Ward et al (2011) | Universal | 75% at 5 y | 60% at 7 y |
| Chevrollier et al (2016) | 90% at 5 y | 50% at 10 y | |
| Cooney et al (2012) | Universal 2 | 97% at 6 y | |
| Badge et al (2016) | 91% at 7.8 y | ||
| Gil et al (2017) | 78% at 15 y | ||
| Cooney et al (2012) | Re-Motion | 97% at 6 y | |
| Herzberg et al (2012) | 92% at 8 y | ||
| Boeckstyns et al (2013) | 92% at 8 y | ||
| Sagerfors et al (2015) | 99% at 5 y | 94% at 8 y (est) | |
| Chevrollier et al (2016) | 100% at 6 y | ||
| Sagerfors et al (2015) | Maestro | 95% at 8 y | |
| Reigstad et al (2017) | Motec | 86% at 10 y |
Discussion
Over the recent years, there have been several new publications investigating total wrist arthrodesis and wrist arthroplasty including a new matched cohort study and data on newer fourth-generation arthroplasty implants. With the ongoing controversy on which may be the better treatment choice for end-stage wrist arthritis, an updated review may help support decision-making.
As with all systematic reviews, the synthesis of trends and patterns from the available data is dependent on the quality of the included articles. According to the GRADE assessment, the majority of articles in this review were low or very low quality retrospective case series. There was also a high degree of heterogeneity in the included studies in terms of the underlying pathology, interventions, and outcome measures.
Functional outcome following surgery was assessed with many different instruments. Pre- and postoperative scores were rarely reported in the arthrodesis studies and demonstrated significant improvement in only one study. 26 There appeared to be no significant differences between arthrodesis techniques for functional outcomes. 29 30 A higher DASH score suggesting poorer function was seen with inflammatory arthritis ( p = 0.005) 25 and was associated with higher pain levels ( r = 0.63). 20 Wrist arthrodesis patients experienced specific difficulties with certain activities such as carrying a heavy object, pushing open a heavy door (50%), and personal hygiene (80%). 3
A significant improvement in function following wrist arthroplasty was noted in several studies. 12 13 14 44 51 Sagerfors et al compared several different wrist implants in a large study of 189 patients (219 index operations) with a mean follow-up of 7 years (range: 2–13). 13 This included Universal 2, Re-Motion, Maestro, and Biaxial, all but the last being currently available. All implants demonstrated a significant improvement in function with the DASH, PRWE, and COPM tools at 5 years. There was no significant difference between the implant types. This was also reflected by Cooney et al reviewing the Biaxial, Re-Motion and Universal 2 wrist replacements in 39 patients at 6 years (range: 3.5–15). 10
Two studies provided a direct comparison between wrist arthrodesis and wrist arthroplasty in retrospective matched cohort studies. 4 5 Only Nydick et al found a significant difference between the two interventions and only with the PRWE score. 4 Following wrist arthroplasty, patients were better able to perform certain activities including cutting meat with a knife, personal activities, and household work. While the strength of this study is limited by the small numbers of patients, it is one of only two studies to compare arthrodesis and arthroplasty directly.
Although pain scores significantly improve following both interventions, patients often do not have complete pain relief, and pain scores are higher with activity. 9 13 28 38 51 The perceived advantage of wrist arthroplasty over arthrodesis is maintenance of range of motion. The reported range following arthroplasty varied widely across studies and only significantly improved following surgery in a few. This included the Universal and Universal 2 implants, RWS, Maestro, and Re-Motion. 13 14 44 45 This was not consistent in all motion planes and only reached the functional range defined by Palmer et al with the Destot prosthesis and the Re-Motion prosthesis. 39 52 54 Satisfaction rates have been studied in more detail by Cavaliere and Chung and were high for both interventions (arthroplasty 91% vs. arthrodesis 93%). 6
The complication profile between the two intervention groups differed in this review. These were generally higher for arthroplasty cases compared with arthrodesis; however, the difference was not significant (range: 0.2–9.5 vs. 0.1–6.1%; p = 0.1). Newer fourth-generation implants appeared to have lower complication rates (range: 0.1–2.9%). This difference was significant when the complication rates of second- and third-generation implants (range: 0.2–8.1%) were compared with fourth-generation implants (0.1–2.9%; p = 0.002). This is also reflected in other studies. 6 The main complication experienced with arthrodesis procedures was metalwork issues such as prominence (2.3%). Overall, metalwork removal was required in 6.1% of cases Carpal and metacarpal osteolysis was also common (3.7%), especially with the Mannerfelt and Malsten technique. 32
Carpal and metacarpal osteolysis and lucency have been major issues with arthroplasty procedures (9.5%) also. This was seen in many studies as well as in registry data from both Norwegian and Australian registers. 49 55 Our findings suggests that this appears to be improving with the newer fourth-generation implants (1.2%), which tend to have porous coatings to encourage osseointegration. 13 40 43 46 One of the reasons behind the high carpal osteolysis rates has been attributed to nonunion at the third carpometacarpal joint, which may increase stress transfer to the carpal component of the prosthesis. Intercarpal fusion to limit this was initially proposed by Menon and subsequently adopted by several others. 37 38 39 42 51
Dislocation has been well documented in second- and third-generation implants including Volz, Universal, and Biaxial. 41 42 43 44 The articular bearing shape of the Universal was modified from a toroidal to an ellipsoidal shape in the Universal 2 to counteract this problem. 56 Better soft tissue balancing and capsular repair techniques have also helped improve stability. 44
Of the current commercially available implants, the latest survival data are 86% at 10 years for Motec, 51 78% at 15 years for Universal 2, 50 90% at 9 years for Re-Motion, 12 and 95% at 8 years for Maestro. 13 Radiographic evidence of carpal component subsidence and carpal malalignment has been linked to earlier revision. 43 57 National joint registry data from Norway have found no association between the survival of wrist implants and the underlying etiology (Biaxial, Elos, and Gibbon prostheses). 49 Sagerfors et al also had similar findings. 13
In conclusion, wrist arthroplasty has evolved considerably from the first-generation implants to current prostheses that appear to have better survival and lower complication profiles. Patients are experiencing improvement in physical function, satisfaction, pain control, and grip strength. Furthermore, wrist arthroplasty is maintaining range of motion, although this was not always significant or reaching predefined functional ranges. One aspect not answered in this review is whether current wrist arthroplasty systems would be suitable in the younger, more active patient. Some data does exist; however, this was not sufficient to reach a general consensus. 51 Wrist arthrodesis remains a good option for patients with either inflammatory or noninflammatory wrist arthritis and is well established. Patients must be well informed about the risks and benefits of wrist arthroplasty compared with wrist arthrodesis to enable informed decision-making before embarking on any surgery.
Footnotes
Conflict of Interest None.
References
- 1.Clayton M L. Surgical treatment at the wrist in rheumatoid arthritis: a review of thirty-seven patients. J Bone Joint Surg Am. 1965;47:741–750. [PubMed] [Google Scholar]
- 2.Mannerfelt L, Malmsten M. Arthrodesis of the wrist in rheumatoid arthritis. A technique without external fixation. Scand J Plast Reconstr Surg. 1971;5(02):124–130. doi: 10.3109/02844317109042952. [DOI] [PubMed] [Google Scholar]
- 3.Sauerbier M, Kluge S, Bickert B, Germann G. Subjective and objective outcomes after total wrist arthrodesis in patients with radiocarpal arthrosis or Kienböck's disease. Chir Main. 2000;19(04):223–231. doi: 10.1016/s1297-3203(00)73484-6. [DOI] [PubMed] [Google Scholar]
- 4.Nydick J A, Watt J F, Garcia M J, Williams B D, Hess A V. Clinical outcomes of arthrodesis and arthroplasty for the treatment of posttraumatic wrist arthritis. J Hand Surg Am. 2013;38(05):899–903. doi: 10.1016/j.jhsa.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Murphy D M, Khoury J G, Imbriglia J E, Adams B D. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg Am. 2003;28(04):570–576. doi: 10.1016/s0363-5023(03)00182-5. [DOI] [PubMed] [Google Scholar]
- 6.Cavaliere C M, Chung K C. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg. 2008;122(03):813–825. doi: 10.1097/PRS.0b013e318180ece3. [DOI] [PubMed] [Google Scholar]
- 7.Yeoh D, Tourret L. Total wrist arthroplasty: a systematic review of the evidence from the last 5 years. J Hand Surg Eur Vol. 2015;40(05):458–468. doi: 10.1177/1753193414539796. [DOI] [PubMed] [Google Scholar]
- 8.NICE. Total wrist replacement. 2008. Available at:https://www.nice.org.uk/guidance/ipg271/evidence/overview-pdf-310832605. Accessed December 3, 2016
- 9.Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty: midterm follow-up study. J Hand Surg Am. 2011;36(06):967–973. doi: 10.1016/j.jhsa.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 10.Cooney W, Manuel J, Froelich J, Rizzo M. Total wrist replacement: a retrospective comparative study. J Wrist Surg. 2012;1(02):165–172. doi: 10.1055/s-0032-1326728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bidwai A S, Cashin F, Richards A, Brown D J. Short to medium results using the remotion total wrist replacement for rheumatoid arthritis. Hand Surg. 2013;18(02):175–178. doi: 10.1142/S0218810413500202. [DOI] [PubMed] [Google Scholar]
- 12.Boeckstyns M E, Herzberg G, Merser S. Favorable results after total wrist arthroplasty: 65 wrists in 60 patients followed for 5–9 years. Acta Orthop. 2013;84(04):415–419. doi: 10.3109/17453674.2013.823588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sagerfors M, Gupta A, Brus O, Pettersson K. Total wrist arthroplasty: a single-center study of 219 cases with 5-year follow-up. J Hand Surg Am. 2015;40(12):2380–2387. doi: 10.1016/j.jhsa.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Badge R, Kailash K, Dickson D R et al. Medium-term outcomes of the Universal-2 total wrist arthroplasty in patients with rheumatoid arthritis. Bone Joint J. 2016;98-B(12):1642–1647. doi: 10.1302/0301-620X.98B12.37121. [DOI] [PubMed] [Google Scholar]
- 15.Chevrollier J, Strugarek-Lecoanet C, Dap F, Dautel G. Results of a unicentric series of 15 wrist prosthesis implantations at a 5.2 year follow-up. Acta Orthop Belg. 2016;82(01):31–42. [PubMed] [Google Scholar]
- 16.Boers M, Tugwell P, Felson D T et al. World Health Organization and International League of Associations for Rheumatology core endpoints for symptom modifying antirheumatic drugs in rheumatoid arthritis clinical trials. J Rheumatol Suppl. 1994;41:86–89. [PubMed] [Google Scholar]
- 17.Bellamy N, Kirwan J, Boers M et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol. 1997;24(04):799–802. [PubMed] [Google Scholar]
- 18.Higgins J PT, Green S.Cochrane Handbook for Systematic Reviews of InterventionsThe Cochrane Collaboration; 2011. Available at:www.handbook.cochrane.org. Accessed December 8, 2016
- 19.Atkins D, Best D, Briss P Aet al. Grading quality of evidence and strength of recommendations BMJ 2004328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lautenbach M, Millrose M, Langner I, Eisenschenk A. Results of Mannerfelt wrist arthrodesis for rheumatoid arthritis in relation to the position of the fused wrist. Int Orthop. 2013;37(12):2409–2413. doi: 10.1007/s00264-013-2063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Voutilainen N H, Pätiälä H V, Juutilainen T J, Rokkanen P U. Long-term results of wrist arthrodeses fixed with self-reinforced polylevolactic acid implants in patients with rheumatoid arthritis. Scand J Rheumatol. 2001;30(03):149–153. doi: 10.1080/030097401300162914. [DOI] [PubMed] [Google Scholar]
- 22.Vahvanen V, Tallroth K. Arthrodesis of the wrist by internal fixation in rheumatoid arthritis: a follow-up study of forty-five consecutive cases. J Hand Surg Am. 1984;9(04):531–536. doi: 10.1016/s0363-5023(84)80105-7. [DOI] [PubMed] [Google Scholar]
- 23.Fontaine C, Mouliade S, Wavreille G, Chantelot C. Wrist arthrodesis with intercalated iliac crest graft in mutilans rheumatoid arthritis. Chir Main. 2014;33(05):336–343. doi: 10.1016/j.main.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Onuma K, Shintani R, Fujimaki H et al. Total wrist arthrodesis with wrist fusion rod in patients with rheumatoid arthritis. Eklem Hastalik Cerrahisi. 2015;26(01):41–48. doi: 10.5606/ehc.2015.10. [DOI] [PubMed] [Google Scholar]
- 25.Owen D H, Agius P A, Nair A, Perriman D M, Smith P N, Roberts C J. Factors predictive of patient outcome following total wrist arthrodesis. Bone Joint J. 2016;98-B(05):647–653. doi: 10.1302/0301-620X.98B5.35638. [DOI] [PubMed] [Google Scholar]
- 26.Riches P L, Elherik F K, Dolan S, Unglaub F, Breusch S J. Patient rated outcomes study into the surgical interventions available for the rheumatoid hand and wrist. Arch Orthop Trauma Surg. 2016;136(04):563–570. doi: 10.1007/s00402-016-2412-1. [DOI] [PubMed] [Google Scholar]
- 27.Masada K, Yasuda M, Takeuchi E, Hashimoto H. Technique of intramedullary fixation for arthrodesis of the wrist in rheumatoid arthritis. Scand J Plast Reconstr Surg Hand Surg. 2003;37(03):155–158. doi: 10.1080/02844310310007764. [DOI] [PubMed] [Google Scholar]
- 28.Lee D H, Carroll R E. Wrist arthrodesis: a combined intramedullary pin and autogenous iliac crest bone graft technique. J Hand Surg Am. 1994;19(05):733–740. doi: 10.1016/0363-5023(94)90176-7. [DOI] [PubMed] [Google Scholar]
- 29.Solem H, Berg N J, Finsen V. Long term results of arthrodesis of the wrist: a 6-15 year follow up of 35 patients. Scand J Plast Reconstr Surg Hand Surg. 2006;40(03):175–178. doi: 10.1080/02844310500453716. [DOI] [PubMed] [Google Scholar]
- 30.Toma C D, Machacek P, Bitzan P, Assadian O, Trieb K, Wanivenhaus A. Fusion of the wrist in rheumatoid arthritis: a clinical and functional evaluation of two surgical techniques. J Bone Joint Surg Br. 2007;89(12):1620–1626. doi: 10.1302/0301-620X.89B12.18880. [DOI] [PubMed] [Google Scholar]
- 31.De Smet L, Truyen J. Arthrodesis of the wrist for osteoarthritis: outcome with a minimum follow-up of 4 years. J Hand Surg Br. 2003;28(06):575–577. doi: 10.1016/s0266-7681(03)00208-0. [DOI] [PubMed] [Google Scholar]
- 32.Rauhaniemi J, Tiusanen H, Sipola E. Total wrist fusion: a study of 115 patients. J Hand Surg [Br] 2005;30(02):217–219. doi: 10.1016/j.jhsb.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 33.Adey L, Ring D, Jupiter J B. Health status after total wrist arthrodesis for posttraumatic arthritis. J Hand Surg Am. 2005;30(05):932–936. doi: 10.1016/j.jhsa.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 34.Brumfield R H, Jr, Conaty J P, Mays J D. Surgery of the wrist in rheumatoid arthritis. Clin Orthop Relat Res. 1979;(142):159–163. [PubMed] [Google Scholar]
- 35.Vicar A J, Burton R I. Surgical management of the rheumatoid wrist--fusion or arthroplasty. J Hand Surg Am. 1986;11(06):790–797. doi: 10.1016/s0363-5023(86)80224-6. [DOI] [PubMed] [Google Scholar]
- 36.Ekroth S R, Werner F W, Palmer A K. Case report of long-term results of Biaxial and Volz total wrist arthroplasty. J Wrist Surg. 2012;1(02):177–178. doi: 10.1055/s-0032-1326730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ward C M, Kuhl T, Adams B D. Five to ten-year outcomes of the Universal total wrist arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(10):914–919. doi: 10.2106/JBJS.H.01614. [DOI] [PubMed] [Google Scholar]
- 38.Reigstad A, Reigstad O, Grimsgaard C, Røkkum M. New concept for total wrist replacement. J Plast Surg Hand Surg. 2011;45(03):148–156. doi: 10.3109/2000656X.2011.579720. [DOI] [PubMed] [Google Scholar]
- 39.Levadoux M, Legré R. Total wrist arthroplasty with Destot prostheses in patients with posttraumatic arthritis. J Hand Surg Am. 2003;28(03):405–413. doi: 10.1053/jhsu.2003.50086. [DOI] [PubMed] [Google Scholar]
- 40.Gellman H, Hontas R, Brumfield R H, Jr, Tozzi J, Conaty J P. Total wrist arthroplasty in rheumatoid arthritis. A long-term clinical review. Clin Orthop Relat Res. 1997;(342):71–76. [PubMed] [Google Scholar]
- 41.Menon J. Total wrist replacement using the modified Volz prosthesis. J Bone Joint Surg Am. 1987;69(07):998–1006. [PubMed] [Google Scholar]
- 42.Menon J. Universal Total Wrist Implant: experience with a carpal component fixed with three screws. J Arthroplasty. 1998;13(05):515–523. doi: 10.1016/s0883-5403(98)90050-x. [DOI] [PubMed] [Google Scholar]
- 43.Takwale V J, Nuttall D, Trail I A, Stanley J K. Biaxial total wrist replacement in patients with rheumatoid arthritis. Clinical review, survivorship and radiological analysis. J Bone Joint Surg Br. 2002;84(05):692–699. doi: 10.1302/0301-620x.84b5.12276. [DOI] [PubMed] [Google Scholar]
- 44.Divelbiss B J, Sollerman C, Adams B D. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am. 2002;27(02):195–204. doi: 10.1053/jhsu.2002.31728. [DOI] [PubMed] [Google Scholar]
- 45.Rahimtoola Z O, Rozing P M. Preliminary results of total wrist arthroplasty using the RWS Prosthesis. J Hand Surg [Br] 2003;28(01):54–60. doi: 10.1054/jhsb.2002.0868. [DOI] [PubMed] [Google Scholar]
- 46.Figgie M P, Ranawat C S, Inglis A E, Sobel M, Figgie H E., III Trispherical total wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am. 1990;15(02):217–223. doi: 10.1016/0363-5023(90)90098-c. [DOI] [PubMed] [Google Scholar]
- 47.Meuli H C, Fernandez D L. Uncemented total wrist arthroplasty. J Hand Surg Am. 1995;20(01):115–122. doi: 10.1016/S0363-5023(05)80069-3. [DOI] [PubMed] [Google Scholar]
- 48.Radmer S, Andresen R, Sparmann M. Total wrist arthroplasty in patients with rheumatoid arthritis. J Hand Surg Am. 2003;28(05):789–794. doi: 10.1016/s0363-5023(03)00307-1. [DOI] [PubMed] [Google Scholar]
- 49.Krukhaug Y, Lie S A, Havelin L I, Furnes O, Hove L M. Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop. 2011;82(04):405–409. doi: 10.3109/17453674.2011.588858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gil J A, Kamal R N, Cone E, Weiss A C. High survivorship and few complications with cementless total wrist arthroplasty at a mean followup of 9 years. Clin Orthop Relat Res. 2017;475(12):3082–3087. doi: 10.1007/s11999-017-5445-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reigstad O, Holm-Glad T, Bolstad B, Grimsgaard C, Thorkildsen R, Røkkum M. Five- to 10-year prospective follow-up of wrist arthroplasty in 56 nonrheumatoid patients. J Hand Surg Am. 2017;42(10):788–796. doi: 10.1016/j.jhsa.2017.06.097. [DOI] [PubMed] [Google Scholar]
- 52.Herzberg G, Boeckstyns M, Sorensen A I et al. “Remotion” total wrist arthroplasty: preliminary results of a prospective international multicenter study of 215 cases. J Wrist Surg. 2012;1(01):17–22. doi: 10.1055/s-0032-1323642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hudak P L, Amadio P C, Bombardier C; The Upper Extremity Collaborative Group (UECG).Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected] Am J Ind Med 19962906602–608. [DOI] [PubMed] [Google Scholar]
- 54.Palmer A K, Werner F W, Murphy D, Glisson R. Functional wrist motion: a biomechanical study. J Hand Surg Am. 1985;10(01):39–46. doi: 10.1016/s0363-5023(85)80246-x. [DOI] [PubMed] [Google Scholar]
- 55.National Joint Replacement Registry.Demographics and Outcomes of Elbow and Wrist Arthroplasty: Supplementary Report 2016Available at:https://aoanjrr.sahmri.com/documents/10180/275105/Demographics%20and%20Outcomes%20of%20Elbow%20and%20Wrist%20Arthroplasty. Accessed January 22, 2018
- 56.Grosland N M, Rogge R D, Adams B D. Influence of articular geometry on prosthetic wrist stability. Clin Orthop Relat Res. 2004;(421):134–142. doi: 10.1097/01.blo.0000126304.79828.2c. [DOI] [PubMed] [Google Scholar]
- 57.Cobb T K, Beckenbaugh R D. Biaxial total-wrist arthroplasty. J Hand Surg Am. 1996;21(06):1011–1021. doi: 10.1016/S0363-5023(96)80309-1. [DOI] [PubMed] [Google Scholar]


