Abstract
Background Magnetic resonance (MR) is the most important imaging technique to assess intra-articular pathology of the wrist. Among various MR imaging protocols, the diagnostic performance of indirect MR arthrography needs further investigation.
Purpose The purpose of this study was to assess the diagnostic performance of pre- and postcontrast, 3 T indirect MR arthrography in the diagnosis of scapholunate intrinsic ligament (SLIL) and triangular fibrocartilage complex (TFCC) injuries, using wrist arthroscopy as reference standard.
Patients and Methods We retrospectively evaluated consecutive patients with suspected SLIL or TFCC injury, who had indirect MR arthrography done before arthroscopy. Images were assessed independently by two senior radiologists.
Results Arthroscopy of the 53 wrists demonstrated 16 Geissler stages II and III partial tears and 6 stage IV total SLIL ruptures. Central perforation of the TFCC was found in 24 wrists, and 12 wrists had an ulnar class 1B lesion. To detect any SLIL tear, accuracy was higher for the two observers using postcontrast indirect MR arthrography (0.77 and 0.72) than for precontrast MR imaging (0.60 and 0.60). No difference was found for total SLIL ruptures “0.85 and 0.89” versus “0.85 and 0.89.” To diagnose class 1B TFCC injuries, accuracy was higher using postcontrast indirect MR arthrography (0.85 and 0.75) than for precontrast MR imaging (0.70 and 0.72). No difference in accuracy was demonstrated for TFCC central tears “0.75 and 0.75” versus “0.70 and 0.77.”
Conclusion Postcontrast images at 3 T indirect MR arthrography, compared with precontrast images, have an improved diagnostic performance for the overall detection of SLIL injuries and as well as class 1B TFCC tears.
Level of Evidence This is a Level II, diagnostic study.
Keywords: arthroscopy, diagnostic performance, indirect MR arthrography, MR imaging, scapholunate ligament, triangular fibrocartilage complex, wrist
Commonly injured ligaments in the wrist encompass the triangular fibrocartilage complex (TFCC) and the scapholunate intrinsic ligament (SLIL). While TFCC is an essential stabilizer of the distal radioulnar joint and ulnocarpal joint, the SLIL is important to preserve normal wrist kinematics and to avoid carpal malalignment. 1 Prolonged ligament dysfunction will lead to instability, pain, and articular degeneration. Early recognition and treatment of these injuries are important as it allows better treatment results rather than later reconstruction or salvage procedures.
Magnetic resonance (MR) imaging is an important tool in the diagnosis of SLIL and TFCC injuries. However, the technique is challenged by the small and intricate nature of these structures. Adequate visualization requires 2 to 3 mm thin, contiguous slices, with a high signal-to-noise ratio. 2 Technical innovations within high-field strength magnets and dedicated wrist coils have enabled better imaging with higher spatial and contrast resolution. In accordance, recent publications have demonstrated improved accuracy in detecting wrist ligament injuries using 3 T field strength compared with low-field, 1.5 T imaging. 3 4
Meta-analysis on the diagnostic accuracy of unenhanced MR imaging versus MR arthrography suggests superiority of the later to detect SLIL and TFCC injuries. 4 5 It applies for both direct MR arthrography, where a contrast medium is injected directly into the joint, or indirect MR arthrography using delayed imaging after intravenously contrast administration. 5 6 7 However, there seems to be no essential differences in the diagnostic ability between the two methods. 8
From a clinical perspective, arthroscopy is the reference standard for diagnosis and evaluation of wrist ligament injuries, which further allows direct operative treatment of found pathology. 9 Nonetheless, an accurate MR imaging protocol is valuable for preoperative planning and to avoid an operative procedure if not needed.
The aim of this study was to assess the diagnostic performance of pre- and postcontrast, 3 T indirect MR arthrography, in the diagnosis of SLIL and TFCC injuries using wrist arthroscopy as reference standard.
Patients and Methods
We retrospectively evaluated consecutive patients with suspected SLIL or TFCC injury, whom in the period from April 2009 to September 2013, had pre- and postcontrast, 3 T indirect MR arthrography done before arthroscopy. Fifty-one patients (53 wrists, 30 left, and 23 right hands) were identified. One male and one female were included with bilateral injury. Thereby, the study population contained 27 male and 24 female patients with a median age of 38.3 years (range, 14–68 years). Exclusion criteria were age younger than 14 and older than 75 years, prior fracture or ligament injury in the wrist at question, cognitive disorder, or language problems. The Regional Ethical Review Board at Lund University approved the study and all patients gave informed consent to participate.
MR Imaging
All MR examinations were performed with a 3-T scanner (TIM-Trio, Siemens Healthcare, Erlangen, Germany). Patients were placed in a prone position, with the arm over the head and imaged with a circularly polarized transmit–receive wrist coil. Immediately after the unenhanced MR examination, patients had an intravenous injection of gadopentetate dimeglumine 279.3 mg/mL (Dotarem, Guerbet, France), 0.2 mL/kg body weight, and maximum volume of 20 mL. Patients were allowed to leave the scanner room with instructions to move their hand normally. Half an hour after the contrast injection, the second examination was started. Imaging sequences before contrast injection included short tau inversion recovery (STIR) images and T1-weighted images in the coronal, axial, and sagittal planes. After contrast injection, T1-weighted, fat saturated (FS) images were acquired in the axial and coronal planes. Details of the sequence parameters for the pre- and postcontrast imaging in the indirect MR arthrography protocol are given in Table 1 .
Table 1. Imaging parameters for MR sequences before and after contrast agent administration.
| Precontrast | Postcontrast | |||||
|---|---|---|---|---|---|---|
| Sequences | STIR | T1-w | T1-w | T1-w | FS T1-w | FS T1-w |
| Orientation | Coronal | coronal | axial | sagittal | Coronal | Axial |
| Repetition time (ms) | 4,570 | 650 | 644 | 583 | 500 | 636 |
| Echo time (ms) | 30 | 16 | 16 | 16 | 16 | 16 |
| Inversion time (ms) | 220 | – | – | – | – | – |
| Echo train length | 10 | 3 | 3 | 3 | 3 | 3 |
| Number of slices | 15 | 20 | 30 | 30 | 18 | 30 |
| Slice thickness (mm) | 3 | 2 | 2 | 2 | 2 | 2 |
| Slice gap (mm) | 0.3 | 0.3 | 0.3 | 0.2 | 0.3 | 0.3 |
| Phase encoding | HF | HF | AP | AP | HF | AP |
| Bandwidth (Hz/pixel) | 250 | 203 | 203 | 203 | 203 | 203 |
| Matrix (read × phase) | 256 × 256 | 448 × 443 | 448 × 238 | 448 × 236 | 448 × 332 | 448 × 238 |
| Field of view (mm 2 ) | 100 × 100 | 100 × 100 | 100 × 71 | 100 × 70 | 100 × 100 | 100 × 60 |
| Averages | 1 | 1 | 2 | 2 | 1 | 2 |
| Scan time (min:s) | 4:04 | 4:51 | 5:13 | 4:36 | 5:38 | 6:54 |
Abbreviations: AP, anterior–posterior; FS, fat saturated; HF, head–foot; STIR, short tau inversion recovery.
Image Analysis
Images were assessed independently, by two senior radiologists with more than 10 years of experience within musculoskeletal MR imaging. The observers were blinded to clinical information and arthroscopic findings. The SLIL was categorized as: normal, with a partial tear (edema and deviant ligament signal), or as a full-thickness tear (discontinuity of the dorsal and proximal segments). The palmar segment was not evaluated. Based on Palmer's classification, 10 TFCC lesions were classified as “central” within the avascular part of the horizontal disc, not distinguishing between traumatic (class 1A) and degenerative etiology (class 2). An ulnar avulsion of the TFCC (class 1B) represents a detachment from the ulnar styloid and onward to the foveal attachment on the ulnar head. This lesion can be associated with an ulnar styloid fracture. Also, we registered if there were any sign of TFCC tear, which encompass classes 1A through 1D tears, capsular detachments, as well as injuries to the meniscus homologue.
Arthroscopic Assessment
Surgery was performed by 11 hand surgery specialists. Time from MR examination to arthroscopy was median 140 days (range, 11–561 days). The surgeons were aware of the results from the preoperative MR report. The wrist arthroscopy was performed under axillar nerve block or general anesthesia. We used a 2.7-mm arthroscope (Stryker-Howmedica, (Kalamazoo, MI) to examine the wrist through standard radiocarpal and mid-carpal portals. A probe was used to assess tension and attachment of the TFCC as well as integrity of the SLIL.
TFCC injuries were classified according to Palmer. 10 Impaired resilience (lack of trampoline effect) together with a positive hook sign indicates a class 1B injury with detachment of the TFCC from the fovea.
SLIL tears were graded according to Geissler et al 11 as: Stage 1: Attenuation or hemorrhage of the SLIL but no step-off or malalignment. Stage 2: As in stage 1, but a probe enters the SL joint space but cannot turn. Stage 3: Step-off or malalignment, and probe turns easily in the SL joint space. Stage 4: Complete rupture where a 2.7-mm scope can pass through the SL joint space. For calculation purposes, stages 2 and 3 were merged as partial ligament tears.
Statistics
Sensitivity (proportion of patients with ligament injury at arthroscopy, also classified as having an injury on MR imaging [true positives]), specificity (proportion of patients with no ligament injury at arthroscopy, also classified as having no injury on MR imaging [true negatives]), accuracy (proportion of patients who were correctly classified from MR imaging), positive predictive value (probability that a patient with a positive MR finding has a ligament injury), and negative predictive value (probability that a patient with negative MR finding does not have a ligament injury) was calculated by means of standard formulas.
Cohen's kappa (κ) was used to evaluate chance-corrected interobserver agreement. The κ values were interpreted as: values ≤ 0 indicating no agreement and 0.01 to 0.20 as none to slight, 0.21 to 0.40 as fair, 0.41 to 0.60 as moderate, 0.61 to 0.80 as substantial, and 0.81 to 1.00 as almost perfect agreement. 12
Statistical analysis was done using free R software, version 3.0.1 ( http://www.r-project.org/ ) and SPSS Statistics 18 for Windows (IBM Corporation, Somers, NY).
Results
Arthroscopy of the 53 wrists demonstrated 16 Geissler stages II and III partial tears and 6 stage IV total SLIL ruptures. Central perforation of the TFCC was found in 24 wrists and 12 wrists had an ulnar, class 1B lesion.
The diagnostic performance, for pre- and postcontrast, indirect MR arthrography, in the detection of any SLIL rupture, partial, as well as total, and to specifically detect a total SLIL rupture, are given in Table 2 . To detect any SLIL tear, both observers had higher values for specificity (0.65 and 0.81 vs. 0.42 and 0.58), accuracy (0.77 and 0.72 vs. 0.60 and 0.60) and positive predictive value (0.61 and 0.68 vs. 0.51 and 0.52) using postcontrast indirect MR arthrography, compared with precontrast imaging ( Fig. 1 ). There was no difference between the pre- and postcontrast techniques to detect a total SLIL rupture. Overall, negative predictive values were higher than positive predictive values. Interobserver agreement was moderate (κ = 0.49) using precontrast imaging, while it was good (κ = 0.80) for postcontrast MR arthrography.
Table 2. Diagnostic performance of pre- and postcontrast, 3 T indirect MR arthrography to diagnose any SLIL injury or a total SLIL rupture using arthroscopy as reference standard.
| Observer 1 | Observer 2 | |||
|---|---|---|---|---|
| Precontrast | Postcontrast | Precontrast | Postcontrast | |
| SLIL, any tear | ||||
| Sensitivity | 0.86 | 0.77 | 0.64 | 0.59 |
| Specificity | 0.42 | 0.65 | 0.58 | 0.81 |
| Accuracy | 0.60 | 0.77 | 0.60 | 0.72 |
| Positive predictive value | 0.51 | 0.61 | 0.52 | 0.68 |
| Negative predictive value | 0.81 | 0.88 | 0.69 | 0.74 |
| SLIL, total rupture | ||||
| Sensitivity | 0.40 | 0.40 | 0.50 | 0.50 |
| Specificity | 0.95 | 0.95 | 0.98 | 0.98 |
| Accuracy | 0.85 | 0.85 | 0.89 | 0.89 |
| Positive predictive value | 0.45 | 0.45 | 0.50 | 0.50 |
| Negative predictive value | 0.95 | 0.95 | 0.98 | 0.98 |
Abbreviations: MR, magnetic resonance; SLIL, scapholunate intrinsic ligament.
Fig. 1.
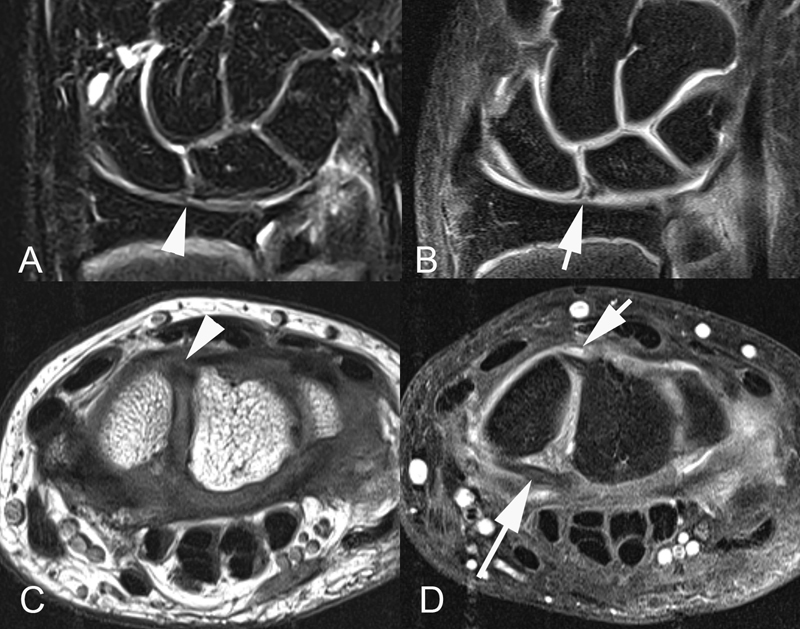
The precontrast STIR coronal image shows a tear in the proximal part of the scapholunate interosseous ligament (arrow head) ( A ), which becomes evident on the T1-weighted, fat saturated, postcontrast indirect MR arthrography (arrow) ( B ). The axial T1-weighted, precontrast image for the same patient shows the dorsal part of scapholunate interosseous ligament (arrow head) ( C ), while the dorsal part (short arrow) as well as the volar part (long arrow) of the scapholunate interosseous ligament appears distinctly on the T1-weighted, fat saturated, postcontrast indirect MR arthrography ( D ). MR, magnetic resonance; STIR, short tau inversion recovery.
The diagnostic performance for pre- and postcontrast, indirect MR arthrography for detection of any TFCC tear, or to specifically diagnose a central tear or a class 1B rupture, is given in Table 3 . To detect a TFCC class 1B tear, values for sensitivity (0.50 and 0.47 vs. 0.40 and 0.33), accuracy (0.85 and 0.75 vs. 0.70 and 0.72), and positive predictive value (0.50 and 0.44 vs. 0.40 and 0.33) were higher for both observers using postcontrast indirect MR arthrography compared with precontrast imaging ( Fig. 2 ). Although positive predictive values were higher than negative predictive values to diagnose TFCC central tears, it was the opposite for detecting of TFCC class 1B tears. Interobserver agreement was fair using either precontrast imaging (κ = 0.26) or postcontrast MR arthrography.
Table 3. Diagnostic performance of pre- and postcontrast, 3 T indirect MR arthrography to diagnose any TFCC injury, a central tear or a class 1B injuries using arthroscopy as reference standard.
| Observer 1 | Observer 2 | |||
|---|---|---|---|---|
| Precontrast | Postcontrast | Precontrast | Postcontrast | |
| TFCC any tear | ||||
| Sensitivity | 0.70 | 0.60 | 0.78 | 0.76 |
| Specificity | 0.75 | 0.81 | 0.81 | 0.81 |
| Accuracy | 0.72 | 0.66 | 0.79 | 0.77 |
| Positive predictive value | 0.87 | 0.88 | 0.91 | 0.90 |
| Negative predictive value | 0.52 | 0.46 | 0.62 | 0.59 |
| TFCC central tear | ||||
| Sensitivity | 0.90 | 1.00 | 0.76 | 0.87 |
| Specificity | 0.65 | 0.69 | 0.78 | 0.71 |
| Accuracy | 0.70 | 0.75 | 0.77 | 0.75 |
| Positive predictive value | 0.90 | 1.00 | 0.76 | 0.87 |
| Negative predictive value | 0.65 | 0.69 | 0.78 | 0.71 |
| TFCC class 1B | ||||
| Sensitivity | 0.40 | 0.50 | 0.33 | 0.47 |
| Specificity | 0.88 | 0.88 | 0.80 | 0.86 |
| Accuracy | 0.70 | 0.85 | 0.72 | 0.75 |
| Positive predictive value | 0.40 | 0.50 | 0.33 | 0.44 |
| Negative predictive value | 0.88 | 0.88 | 0.81 | 0.86 |
Abbreviations: MR, magnetic resonance; TFCC, triangular fibrocartilage complex.
Fig. 2.
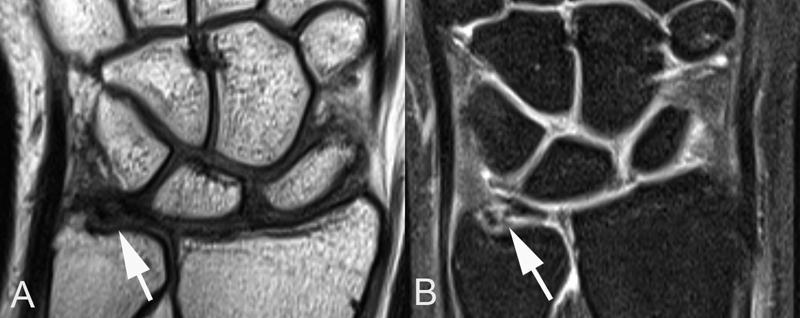
The precontrast, coronal T1-weighted image suggests ulnar peripheral TFCC pathology (arrow) ( A ). The presence of a class 1B TFCC tear (arrow) is more clearly demonstrated on the postcontrast, T1-weighted, fat saturated, indirect MR arthrography ( B ). MR, magnetic resonance; TFCC, triangular fibrocartilage complex.
Discussion
There is a limited number of clinical studies which have evaluated the diagnostic performance of indirect MR arthrography in patients with suspected SLIL or TFCC injuries. 6 13 14 15 Overall, results from these studies are inconclusive and may not necessarily apply today due to technical development of MR imaging as well as improved understanding of detailed anatomy of these injuries. 16
In this study, MR imaging was performed according to the department's routine wrist protocol for indirect MR arthrography. A strict comparison of the pre- and postcontrast imaging would not be justified, as the former includes just one fluid-sensitive STIR sequence in the coronal plane together with T1-weighted sequences in the coronal, axial, and sagittal planes, while the later involves FS T1-weighted sequences in the coronal and the axial planes. Therefore, it could be argued that the precontrast imaging should have included more fluid-sensitive sequences such as proton density and STIR imaging. Nonetheless, this study allows us to evaluate the diagnostic performance of our pre- and postcontrast protocol for 3 T indirect MR arthrography.
A limitation of our study is our reference standard; the arthroscopy was performed by several surgeons. Although it reflects everyday life at our department, and all surgeons were hand specialists, it increases variability in interpretation of the agreed-upon diagnostics for wrist ligament injuries. In addition, the surgeons were not blinded to the preoperative MR report. Other peripheral TFCC pathology than central tears and class 1B lesions were not differentiated because numbers were limited and lesions not clearly definable. It hampers our ability to evaluate TFCC lesion in general and may explain the divergent result for any TFCC tear versus central and class 1B lesions. A further short coming is the limited sample size and retrospective nature of the investigation. Finally, in some cases, the timespan from MR imaging to arthroscopy could have had an impact on comparability due to deterioration or healing of the present injury, or the addition of a new trauma. The strength of our study is the comparative design and that it includes all consecutive patients who underwent our indirect MR arthrography protocol using 3 T imaging technique.
Our results indicate that the diagnostic performance of postcontrast MR arthrography is better for the overall ability to detect any SLIL tear, while precontrast MR imaging appears just as accurate to detect total SLIL ruptures. The advantage of postcontrast MR arthrography in diagnosing SLIL tears is supported by a higher interobserver agreement. For TFCC lesions, postcontrast MR arthrography is better than precontrast MR imaging to diagnose class 1B tears.
Notably, higher negative than positive predictive values for both pre- and postcontrast MR imaging techniques in our study suggest that they are more reliable to rule out than to confirm total SLIL ruptures as well as TFCC class 1B lesions. The opposite was found for the more prevalent TFCC central tears. It is important to be aware that predictive values highly depend on the prevalence of the abnormality that is tested. Therefore, it is more certain that a negative result indicates no abnormality if the lesion is rarer, and it will be less certain that a positive result represents an abnormality.
Evaluation of chronic wrist pain is a challenge. A detailed anamnesis and thorough clinical examination together with radiographs including relevant stress views are mandatory. However, clinical provocative tests may not suffice to rule out the presence of relevant pathology, and total ligament ruptures cannot always be visualized on radiographs due to intact secondary stabilizers. 17 18
MR has become the most important imaging technique to assess intra-articular pathology. At indirect MR arthrography, contrast diffuses from synovia into the joint space where it creates an arthrographic effect which enhances distinction between structures. With direct MR arthrography, there is a distention of the joint which cause separation and stretching of structures for better visualization. Furthermore, the increased intra-articular pressure will force contrast through lesions in ligaments and their attachment. 19 Theoretically, direct MR arthrography should have an advantage in small joints such as the wrist with less volume to distend. However, a clear diagnostic advantage of direct MR arthrography compared with indirect MR arthrography, for detection of intrinsic ligament or TFCC injuries has not been demonstrated. 8 The drawbacks of direct MR arthrography lie in the invasiveness of the method, the technical complexity with injections into one or more joint compartments, and the time consumption.
In the vast majority of cases, a partial SLIL tear can be treated with arthroscopic technique, while a total rupture may require an open procedure and ligament reconstruction. 20 Therefore, the distinction between a partial tear and a total SLIL tear is important. As in this study, the value of MR imaging to diagnose complete SLIL ligament tears has previously been demonstrated. 21 22 TFCC class 1 tears are in principal unrepairable due to the avascularity of articular disk. In contrast, TFCC class 1B tears encompass a range of reparable injuries where the proximal insertion on to the fovea represents the main stabilizer of the distal radioulnar joint. 23 Earlier, a poor ability to detect class 1B TFCC lesions has been reported for indirect as well as direct MR arthrography. 14 21 We believe that our indirect MR arthrography protocol using slice thickness of 2 to 3 mm and very narrow slice gaps (0.2–0.3 mm) adds to its diagnostic performance. 2
Arthroscopy is the reference standard to detect wrist ligament injuries as it allows direct visualization and functional testing of the involved structures. 9 However, MR imaging as a noninvasive procedure plays an important role in diagnostics and preoperative planning in cases where the clinical evaluation is uncertain or when additional pathologies such as: synovitis, tendinosis, bone marrow abnormality, occult fractures, or cartilage lesions 2 are suspected. Based on results from this study, we find postcontrast indirect MR arthrography to have an advantage in the search for SLIL tears, but it may be of particular diagnostic value in the examination of patients with ulnar-sided wrist pain and suspected TFCC injury.
Ethical Approval
The Regional Ethics Committee at Lund University approved the study (LU 459–03).
Funding Statement
Funding Financial support has been received from the Regional Research Fund of Skåne University Hospital, Lund University, Sweden.
Footnotes
Conflict of Interest None.
References
- 1.Berger R A. The ligaments of the wrist. A current overview of anatomy with considerations of their potential functions. Hand Clin. 1997;13(01):63–82. [PubMed] [Google Scholar]
- 2.Zanetti M, Saupe N, Nagy L. Role of MR imaging in chronic wrist pain. Eur Radiol. 2007;17(04):927–938. doi: 10.1007/s00330-006-0365-4. [DOI] [PubMed] [Google Scholar]
- 3.Anderson M L, Skinner J A, Felmlee J P, Berger R A, Amrami K K. Diagnostic comparison of 1.5 Tesla and 3.0 Tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg Am. 2008;33(07):1153–1159. doi: 10.1016/j.jhsa.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 4.Hafezi-Nejad N, Carrino J A, Eng J et al. Scapholunate interosseous ligament tears: diagnostic performance of 1.5 T, 3 T MRI, and MR arthrography-a systematic review and meta-analysis. Acad Radiol. 2016;23(09):1091–1103. doi: 10.1016/j.acra.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Smith T O, Drew B, Toms A P, Jerosch-Herold C, Chojnowski A J. Diagnostic accuracy of magnetic resonance imaging and magnetic resonance arthrography for triangular fibrocartilaginous complex injury: a systematic review and meta-analysis. J Bone Joint Surg Am. 2012;94(09):824–832. doi: 10.2106/JBJS.J.01775. [DOI] [PubMed] [Google Scholar]
- 6.Herold T, Lenhart M, Held P et al. [Indirect MR arthrography of the wrist in the diagnosis of TFCC-lesions] RoFo Fortschr Geb Rontgenstr Nuklearmed. 2001;173(11):1006–1011. doi: 10.1055/s-2001-18318. [DOI] [PubMed] [Google Scholar]
- 7.Magee T. Comparison of 3-T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. Am J Roentgenol. 2009;192(01):80–85. doi: 10.2214/AJR.08.1089. [DOI] [PubMed] [Google Scholar]
- 8.Ross C, Hoffstetter P, Fellner C, Herold T, Nerlich M, Huber M K. [Detection of intrinsic ligament and TFCC lesions of the wrist. Direct versus indirect MRI arthrography] Unfallchirurg. 2015;118(03):251–255. doi: 10.1007/s00113-014-2662-8. [DOI] [PubMed] [Google Scholar]
- 9.Iordache S D, Rowan R, Garvin G J, Osman S, Grewal R, Faber K J. Prevalence of triangular fibrocartilage complex abnormalities on MRI scans of asymptomatic wrists. J Hand Surg Am. 2012;37(01):98–103. doi: 10.1016/j.jhsa.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(04):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 11.Geissler W B, Freeland A E, Savoie F H, McIntyre L W, Whipple T L. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(03):357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Landis J R, Koch G G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(01):159–174. [PubMed] [Google Scholar]
- 13.Haims A H, Schweitzer M E, Morrison W B et al. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology. 2003;227(03):701–707. doi: 10.1148/radiol.2273020398. [DOI] [PubMed] [Google Scholar]
- 14.Haims A H, Schweitzer M E, Morrison W B et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol. 2002;178(02):419–422. doi: 10.2214/ajr.178.2.1780419. [DOI] [PubMed] [Google Scholar]
- 15.Schädel-Höpfner M, Iwinska-Zelder J, Braus T, Böhringer G, Klose K J, Gotzen L. MRI versus arthroscopy in the diagnosis of scapholunate ligament injury. J Hand Surg [Br] 2001;26(01):17–21. doi: 10.1054/jhsb.2000.0450. [DOI] [PubMed] [Google Scholar]
- 16.Burns J E, Tanaka T, Ueno T, Nakamura T, Yoshioka H. Pitfalls that may mimic injuries of the triangular fibrocartilage and proximal intrinsic wrist ligaments at MR imaging. Radiographics. 2011;31(01):63–78. doi: 10.1148/rg.311105114. [DOI] [PubMed] [Google Scholar]
- 17.Prosser R, Harvey L, Lastayo P, Hargreaves I, Scougall P, Herbert R D. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother. 2011;57(04):247–253. doi: 10.1016/S1836-9553(11)70055-8. [DOI] [PubMed] [Google Scholar]
- 18.Cerezal L, de Dios Berná-Mestre J, Canga A et al. MR and CT arthrography of the wrist. Semin Musculoskelet Radiol. 2012;16(01):27–41. doi: 10.1055/s-0032-1304299. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka T, Ogino S, Yoshioka H. Ligamentous injuries of the wrist. Semin Musculoskelet Radiol. 2008;12(04):359–377. doi: 10.1055/s-0028-1100642. [DOI] [PubMed] [Google Scholar]
- 20.Corella F, Del Cerro M, Ocampos M, Larrainzar-Garijo R. Arthroscopic ligamentoplasty of the dorsal and volar portions of the scapholunate ligament. J Hand Surg Am. 2013;38(12):2466–2477. doi: 10.1016/j.jhsa.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 21.Braun H, Kenn W, Schneider S, Graf M, Sandstede J, Hahn D. [Direct MR arthrography of the wrist- value in detecting complete and partial defects of intrinsic ligaments and the TFCC in comparison with arthroscopy] RoFo Fortschr Geb Rontgenstr Nuklearmed. 2003;175(11):1515–1524. doi: 10.1055/s-2003-43404. [DOI] [PubMed] [Google Scholar]
- 22.Moser T, Dosch J C, Moussaoui A, Dietemann J L. Wrist ligament tears: evaluation of MRI and combined MDCT and MR arthrography. AJR Am J Roentgenol. 2007;188(05):1278–1286. doi: 10.2214/AJR.06.0288. [DOI] [PubMed] [Google Scholar]
- 23.Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011;27(03):263–272. doi: 10.1016/j.hcl.2011.05.014. [DOI] [PubMed] [Google Scholar]


