Abstract
Bronchial rupture by blunt chest trauma is rare. We present a case of bronchial injury after blunt chest trauma that was repaired surgically by primary reconstruction. We performed a review of literature to verify if primary reconstruction is suitable for the treatment of adult patients with blunt bronchial injury. A systematic search was conducted to identify cohort studies of bronchial rupture after blunt chest trauma in adult patients between 1985 and 2016 (n=215 articles). Studies were included concerning four or more patients and in case patient data could be extracted. This resulted in 19 articles for final review, consisting of 155 patients. Mean age of 155 patients was 28 (range, 18–60) years. The main bronchus was mostly injured (81%), in 5% including an injury of the trachea and in 14% lobar bronchi injury. Surgical repair was performed in 95% of patients: primary anastomosis in 72%, pneumonectomy in 15%, lobectomy or sleeve resection in 12% and other in 1%. Perioperative mortality rate was 10%. Other complications occurred in 17% (empyema, rebleeding, stenosis and fistula, among others). Data concerning the occurrence of long-term complications or long-term follow-up was not found. Statistical evaluation could not be performed due to lack of consistent patient data. No strong recommendations regarding type and timing of surgery can be made based on the available literature. Based on our multidisciplinary opinion we would advocate primary anastomosis in case of stable vital signs with the goal to preserve healthy lung parenchyma. Moreover, it may be considered transferring these rare cases to an experienced thoracic and trauma surgery center.
Keywords: Bronchus, trauma, rupture, surgery, review
Introduction
Case report
A 19-year-old male patient suffered a blunt trauma after a bicycle versus car collision late in the evening. The patient was dyspneic and had clinical signs of a left sided pneumothorax for which a chest tube was inserted by a specialized mobile medical trauma team. Further assessment showed a normal pulse and blood pressure and a maximal Glasgow coma score.
The patient was transferred to our hospital by helicopter. On presentation at our Accident and Emergency department, the patient was progressively dyspneic with clinical signs of a tension pneumothorax on the right side. A chest tube was inserted after which respiratory function improved. Because of a sudden drop in consciousness level, an orotracheal intubation with a single lumen tube was performed and mechanical ventilation was started.
Whole-body computerized tomography (CT) scan showed subdural and subarachnoid hematomas, subcutaneous emphysema, bilateral pneumothorax with pneumomediastinum, multiple spine fractures, an elbow luxation and a right-sided proximal first metacarpal fracture (Figure 1). The patient was taken to the operating theatre, where flexible bronchoscopy was performed and revealed a complete rupture of the left main bronchus, 3 cm distal of the carina (see Figure 2). Furthermore, the elbow joint was reduced, the open wounds on the left hand were debrided and an intracranial pressure sensor was inserted. Patient’s vital signs remained normal and stable during surgery. After multidisciplinary consultation, it was decided to wait several hours and the patient was planned for surgery next day when a fit surgical team was available. The patient was admitted to the intensive care unit (ICU) pre-surgery.
Figure 1.

Computed tomography scan during initial assessment of the patient at the emergency department, in this coronal plane revealing subcutaneous emphysema, left sided pneumothorax and pneumomediastinum. Furthermore, a suggestion of a rupture of the left main bronchus can be seen.
Figure 2.
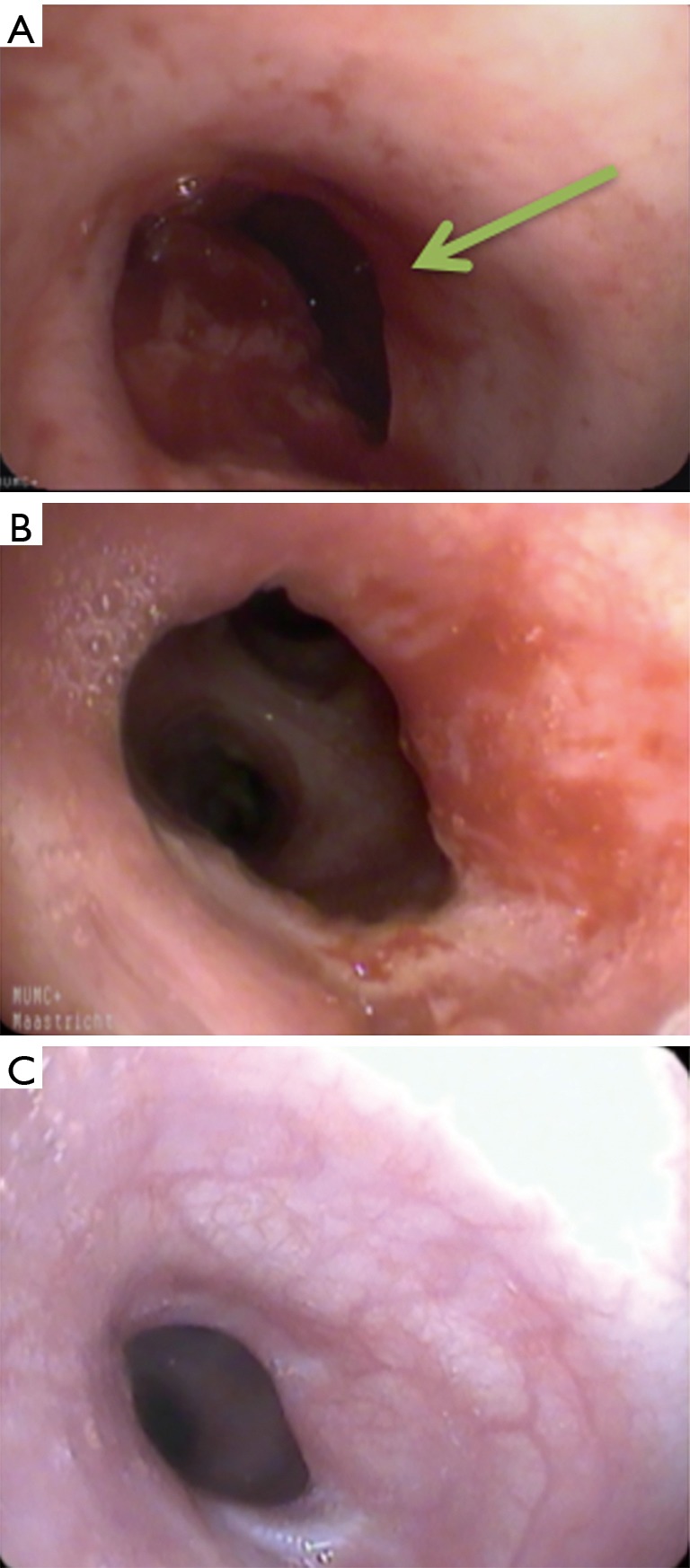
Bronchoscopy at diagnosis and during follow-up. (A) Bronchoscopy showing a complete rupture of the left main bronchus, 3 cm distal of the carina (arrow); (B) bronchoscopy 3 months after surgery. The left upper lobe and lower lobe were scaled as normal. The lumen of the distal left main bronchus was circular slightly narrowed (20% narrowing of lumen). Bronchial mucosa was still irritated and vulnerable; (C) bronchoscopy 9 months after surgery. A circular narrowing of 20% at the distal side of the left main bronchus was present. Bronchial mucosa was recovered with no mucosal defects or granulation tissue.
The operation was performed under general anesthesia. The single lumen tube was uneventfully replaced by a double-lumen tube and a left-sided posterolateral thoracotomy was performed. After mediastinal dissection of pulmonary veins, main pulmonary artery and aortic arch, the completely transected left main bronchus was visualized. As seen on preoperative imaging, the bronchial rupture was localized approximately 3 cm distal to the carina. A tension-free primary end-to-end repair was performed with interrupted 3-0 polydioxanone sutures (PDS) (Figure 3). The anastomosis was covered with an intercostal muscle flap. Underwater testing showed no air leakage. A chest tube was placed and the thoracotomy was closed in layers. Operating time was 3 hours with a blood loss volume of 100 mL. After tube exchange to a single lumen tube, the patient was readmitted to the ICU.
Figure 3.

The completely transected left main bronchus is visualized after mediastinal dissection of pulmonary veins, aortic arch and main pulmonary artery (1). A primary end-to-end repair with interrupted 3-0 polydioxanone sutures (PDS) was performed and visualized in this video. Available online: http://www.asvide.com/article/view/27401
Directly postoperative, an atelectasis of the left lung with respiratory deterioration occurred. After bronchoscopy and mechanical ventilation in prone position, respiratory condition improved. Right and left chest tubes were removed, respectively, on postoperative day 1 and 3. Patient was extubated on day 7 and discharged to the surgical ward on day 10. No complications occurred and the patient was discharged from hospital in favorable condition on day 19.
Bronchoscopy at 3 months follow-up showed the anastomosis with granulation tissue and non-significant stricture (Figure 2B). At 9 months follow-up, there were no residual complaints and pulmonary function was normal (Figure 4, Table 1). Bronchoscopy confirmed a patent anastomosis (Figure 2C). Patient had returned to his pre-injury functional status including physical activities and competitions as semi-professional cyclist.
Figure 4.
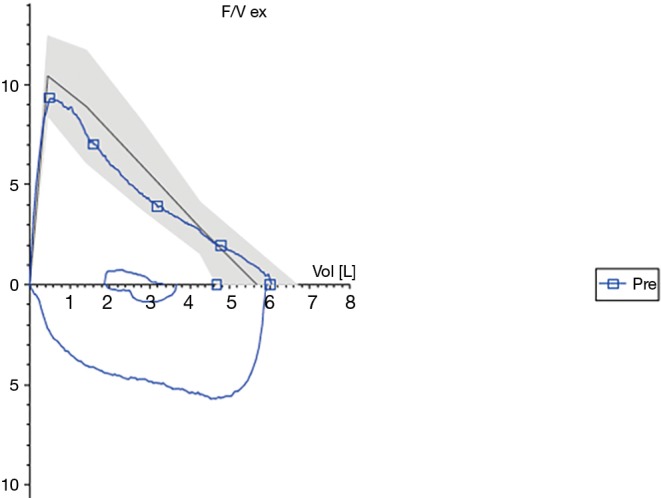
Flow-volume curve at 9 months of follow-up. Black line: normal curve; blue line: curve of patient’s flow volume; X-axis: volume (L), Y-axis: flow (L/s).
Table 1. Pulmonary function (flow-volume) tests at 9 months of follow-up.
| Variable | Value | %pred |
|---|---|---|
| FEV1 | 4.67 (L) | 98 |
| FVC | 5.89 (L) | 99 |
| FEV1/FVC | 73% | |
| PEF | 6.01 (L/s) | 106 |
FEV1, forced expired volume in one second; FVC, forced vital capacity; FEV1/FVC, ratio; PEF, peak expiratory flow.
Objective of the review
Bronchial injury after blunt trauma is rare (1–3%) but potentially life threatening and associated with a high mortality rate (2). Over 70–80% of the patients who sustain tracheal or bronchial injury die before arriving at the hospital, and therefore will stay unreported (3,4). In contrast, the majority of patients who survive until presentation at the hospital are managed non-operatively by supportive measures and chest tube thoracostomy. Only a minority of these patients will need urgent thoracotomy (5).
Bronchial injury has various clinical presentations ranging from lethal situations such as tension pneumothorax, persistent extensive subcutaneous emphysema, or conditions with fewer signs resulting in delay of diagnosis (6). Although bronchial injuries are rare, improved prehospital care has increased the number of patients presenting at the hospital. Familiarity in recognizing the condition and primary and final (surgical) management is therefore increasingly important.
In patients with blunt thoracic trauma, thoracotomy with pulmonary resection might be necessary in patients who are in respiratory extremis, according to a damage control strategy. Damage control surgery is aimed at life-preserving procedures without extensive reconstruction. When vital signs are within limits, an alternative approach might include reconstruction of the bronchus in selected cases, with the aim to preserve lung parenchyma.
This review aims to assess the methods and results of surgical repair and short- and long-term follow-up in adult patients with bronchial injury after blunt chest trauma. We intent to provide important key points in the surgical management of bronchial rupture, a rare and potential life threatening injury.
Methods
This systematic review was performed according to PRISMA guidelines (7). A thorough review of literature was conducted to identify consecutive cohort studies reporting on blunt bronchial injuries in adult patients, published between 1985 and 2016. Medline, Cochrane Library and Embase were searched using the following keywords: bronchus; bronchial; blunt; trauma; and injury. The reference lists of included articles were also searched.
We limited the study to cohort studies reporting on patients with blunt bronchial traumatic injury aged 18 years or older. Studies reporting on penetrating trauma, iatrogenic injuries, children or solitary tracheal injuries were excluded.
Two authors independently performed the search and selection of articles (LvR; MvG). At first, articles were evaluated for eligibility based on title and abstract. Final evaluation and selection of articles was performed after article reading. In case of inconsistency in selection, we discussed these cases together with a third author (EdL) to make a final selection.
We collected information on mechanism of injury, time to diagnosis, anatomic location of injury, type of (surgical) repair, mortality and complications where available. Descriptive categorical data are presented as proportions and absolute numbers. Continuous variables are presented as means with standard deviations (SD). We performed a descriptive analysis, as it was not possible to undertake a meta-analysis due to the high level of heterogeneity of the interventions.
We assessed the risk of bias using the assessment tool of Cochrane Handbook for systematic reviews of interventions. Quality of the study methodology was assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Results
The search resulted in 215 articles published between 1985 and 2016. A total of 180 articles were excluded based on title and abstract. Full text of the remaining 35 (5,8-23) articles (24-41) were evaluated and resulted in exclusion of another 16 articles, because it concerned review or survey articles, case reports, children, or only tracheal or penetrating injuries (5,8-12,17-20,22,26-28,32-34,36,38). Screening of the reference lists did not provide additional articles. So, final selection resulted in 19 articles that met the predefined inclusion criteria, as shown in Figure 5.
Figure 5.
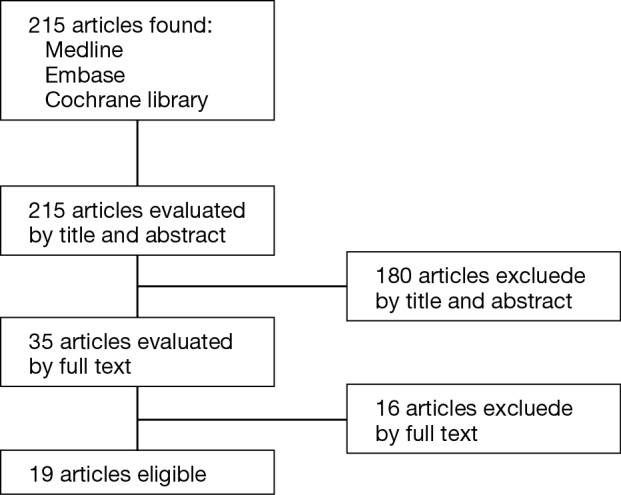
Flowchart of the selection of eligible articles.
All studies were retrospective cohort studies. The 19 articles consisted of a total of 155 patients with blunt bronchial injury. Demographics and clinical characteristics of the patients are reported in Table 2. Their age ranged from 18 to 60 years, with a median of 28 years. Most injuries involved patients aged younger than 30 years (63%). The mechanism of injury involved a car accident in the majority of patients (60%), followed by motorcycle accidents in 16%. Other trauma included crush injury, fall from height, bicycle or pedestrian accidents.
Table 2. Patient demographics and clinical characteristics.
| Total | n | % |
|---|---|---|
| Age in years | ||
| 18–29 | 38 | 63 |
| 30–39 | 13 | 22 |
| 40+ | 9 | 15 |
| Missing | 95 | |
| Cause of injury | ||
| Car accident | 53 | 60 |
| Motorcycle accident | 14 | 16 |
| Fall from height | 9 | 10 |
| Crush injury | 6 | 7 |
| Pedestrian accident | 5 | 6 |
| Bicycle accident | 1 | 1 |
| Missing | 67 | |
| Site of injury | ||
| Left main bronchus | 36 | 23 |
| Right main bronchus | 49 | 32 |
| Main bronchus side unknown | 35 | 23 |
| Bilateral main bronchi | 5 | 3 |
| Trachea and main bronchus | 8 | 5 |
| Main and lobar bronchus | 3 | 2 |
| Lobar bronchus | 19 | 12 |
The main bronchus was most frequently injured (n=125; 81%). The side of injury was documented in 90 of these patients, and showed that the right main bronchus was mostly affected, in 49 patients (32%). Injury of left main bronchus occurred in 36 patients (23%), and bilateral injury to both main bronchi occurred in 5 patients (3%). In 8 patients (5%), the main bronchus as well as the trachea was damaged. The remaining injuries concerned the lobar bronchi with or without damage to the main bronchus, in 22 patients (14%).
The time between trauma and surgical treatment was described in 54% of the cases (n=84). With available data, median time to surgical treatment was 7 days, with a range between zero days and 8 years (only one patient had this delay, unknown cause). Delayed treatment was caused by delayed presentation or diagnosis, transportation to other hospitals, or after failure of conservative treatment.
Surgical repair was performed in 95% of patients. The surgical approach was thoracotomy in all cases. In 72% of the cases, a sutured end-to-end anastomosis was performed, pneumonectomy in 15% and lobectomy in 9%. Other techniques included a sleeve resection, or repair by using an intercostal flap technique (Table 3). Conservative treatment consisted of long term chest tube thoracostomy. One patient died prior to surgery due to failure to establish patent airway.
Table 3. Type of surgical treatment.
| Surgical treatment | n | % |
|---|---|---|
| Surgery | ||
| Thoracotomy | 148 | 95 |
| Tracheostomy | 1 | 1 |
| No surgery | 6 | 4 |
| Type of repair in thoracotomy | ||
| End-to-end anastomosis (sutured) | 107 | 72 |
| Lobectomy | 14 | 9 |
| Sleeve resection | 4 | 3 |
| Pneumonectomy | 22 | 15 |
| Intercostal flap repair | 1 | 1 |
In the study population, the duration of follow-up is unknown and there is also no information on the use of any specific evaluation methods like pulmonary function or bronchoscopy. Data on the occurrence of perioperative complications was provided in only 107 of 155 patients. The mortality rate was 10% and other complications occurred in 17% (e.g., stenosis, empyema, rebleeding, bronchopleural fistula) (Table 4).
Table 4. Perioperative complications.
| Complications | n | % |
|---|---|---|
| Mortality rate | 16 | 10 |
| Unknown cause | 10 | |
| Multiple organ failure | 2 | |
| Other traumatic injury | 2 | |
| Cardiac arrest | 1 | |
| No patent airway | 1 | |
| Complications | 26 | 17 |
| Stenosis | 9 | |
| Empyema | 5 | |
| Pulmonary hypertension | 3 | |
| Persistent air leakage | 2 | |
| Nerve injury | 2 | |
| Dyspnoea during mild exercise | 2 | |
| Wound infection | 1 | |
| Bronchopleural fistula | 1 | |
| Rebleeding | 1 |
Discussion
We presented a case of bronchial injury after blunt chest trauma that was repaired surgically by primary reconstruction and subsequently performed a thorough follow-up. Since these injuries are rare, we performed a review of literature to verify if primary reconstruction is suitable for the treatment of adult patients with blunt bronchial injury.
Blunt bronchial injury comes with a variation in presentation and severity (11,42,43). The main bronchus seems to be affected most frequently, and was in many cases accompanied by severe damage to lung tissue (43). These anatomical differences lead to diverse presentations, which might explain the delay in diagnosis and surgical treatment as discussed in this paper. In the majority of reported cases, there was no reason for an acute procedure. Median time to surgery after injury was 7 days, and still a substantial number of patients underwent surgery even at a later moment. Appropriate timing until surgery is debatable and can be managed best based on patients’ health status, injury characteristics, and expertise of hospital and surgical team. Our case presented in the evening and had stable vital signs, so the multidisciplinary team of trauma surgeon, thoracic surgeons, pulmonologist and intensivist, decided there was no need for damage control surgery and postponed surgery until the next morning. The favorable outcome of our patient supports the decision to postpone surgery. Even in patients with complete transection, adequate lung ventilation is possible in the majority of cases because usually only a small gap exists between the two ends of the ruptured bronchus, with coverage of surrounding tissues (24).
The type of surgical treatment in blunt bronchial injury depends among others on the site and extent of the damage. In this review, bronchial rupture occurred more often in the right compared to the left main bronchus (32% vs. 23%). A study of Altinok et al. commented that this is probably caused by the right main bronchus being shorter and less protected by large surrounding fixed vascular structures, and by a larger volume of the right lung (44).
In 72% of the patients, an end-to-end anastomosis was created, which seems feasible and should be considered in most cases to preserve (healthy) lung parenchyma, in this generally young patient population. Even in older patients this should be considered, since they are more often confronted with pulmonary diseases such as chronic obstructive pulmonary disease (COPD). In contrast to complete bronchial rupture, it is arguable whether smaller defects, that comprise less than the circumferential one third of the main bronchus, can be treated conservatively (43). A paper of Kiser et al. showed that the mortality risk is higher for patients who were conservatively treated (25% vs. 3%), but might be biased by other patient- and injury related characteristics (23). Failure of conservative treatment during follow-up can present by bronchial stenosis or fistulas, although no exact numbers are available on this issue. Surgical treatment can of course lead to complications like bronchial stenosis that was present in 6% of the reviewed population.
Several limitations of this analysis should be discussed. The objectives of our study were, among others, to estimate the morbidity and mortality risk in surgical treatment of blunt bronchial rupture. These outcome measures were however, insufficiently described in the studies included this review. Follow-up data was even completely missing in 31% of the patients and information on follow-up duration per patient was unknown. Reconstructions of bronchial ruptures with primary repair are mainly at risk for anastomotic complications, like stenosis. The case described in this review had favorable follow-up results with no signs of clinical significant stenosis during bronchoscopy even after nine months of follow-up. This could be related to preservation of local circulation.
Furthermore, morbidity and mortality rates are biased in the studies available, partly due to over- as well as under-reporting. Registration of morbidity and mortality is challenging since many patients will be referred patients from other hospitals in a different region, and those are not likely to attend to any follow-up appointments. Furthermore, the complication rate is also biased by concomitant injuries and comorbidity. Unfortunately, we could not report on this topic due to missing data in the included studies on concomitant injuries or injury severity score.
Another limitation could be that we decided to exclude case reports and thus valuable information about this rare condition could have been lost. However, small studies with unfavorable results are unlikely to be published and therefore we believe that excluding those reports is a more correct approach to the analyses.
Conclusions
Blunt bronchial rupture mostly occurs in younger trauma patients and is associated with high morbidity and mortality rates. No strong recommendations regarding type and timing of surgery can be made based on the available literature. Based on our multidisciplinary opinion we would advocate primary anastomosis in case of stable vital signs with the goal to preserve healthy lung parenchyma. Moreover, it may be considered transferring these rare cases of bronchial rupture to an experienced thoracic and trauma surgery center.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.van Roozendaal LM, van Gool MH, Sprooten RT, et al. The completely transected left main bronchus is visualized after mediastinal dissection of pulmonary veins, aortic arch and main pulmonary artery. Asvide 2018;5:783. Available online: http://www.asvide.com/article/view/27401
- 2.Devitt JH, Boulanger BR. Lower airway injuries and anaesthesia. Can J Anaesth 1996;43:148-59. 10.1007/BF03011256 [DOI] [PubMed] [Google Scholar]
- 3.Kummer C, Netto FS, Rizoli S, et al. A review of traumatic airway injuries: potential implications for airway assessment and management. Injury 2007;38:27-33. 10.1016/j.injury.2006.09.002 [DOI] [PubMed] [Google Scholar]
- 4.Nishiumi N, Inokuchi S, Oiwa K, et al. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg 2010;89:232-8. 10.1016/j.athoracsur.2009.09.041 [DOI] [PubMed] [Google Scholar]
- 5.Koletsis E, Prokakis C, Baltayiannis N, et al. Surgical decision making in tracheobronchial injuries on the basis of clinical evidences and the injury's anatomical setting: a retrospective analysis. Injury 2012;43:1437-41. 10.1016/j.injury.2010.08.038 [DOI] [PubMed] [Google Scholar]
- 6.Bertelsen S, Howitz P. Injuries of the trachea and bronchi. Thorax 1972;27:188-94. 10.1136/thx.27.2.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiarelli M, Gerosa M, Guttadauro A, et al. Urgent pulmonary lobectomy for blunt chest trauma: report of three cases without mortality. J Thorac Dis 2016;8:1825-9. 10.21037/jtd.2016.06.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bagheri R, Afghani R, Haghi SZ, et al. Outcome of repair of bronchial injury in 10 patients with blunt chest trauma. Asian Cardiovasc Thorac Ann 2015;23:180-4. 10.1177/0218492314545621 [DOI] [PubMed] [Google Scholar]
- 10.Bolca C, Danaila O, Paleru C, et al. Main bronchial stenosis--sequel of delayed diagnosis after posttraumatic bronchial injury. Pneumologia 2013;62:146-7. [PubMed] [Google Scholar]
- 11.Farzanegan R, Alijanipour P, Akbarshahi H, et al. Major airways trauma, management and long term results. Ann Thorac Cardiovasc Surg 2011;17:544-51. 10.5761/atcs.oa.11.01679 [DOI] [PubMed] [Google Scholar]
- 12.Carretta A, Melloni G, Bandiera A, et al. Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries. World J Surg 2011;35:2568-74. 10.1007/s00268-011-1227-z [DOI] [PubMed] [Google Scholar]
- 13.Fatimi SH, Hanif HM, Ahmed A, et al. Outcomes of surgical management of tracheobronchial injuries---a case series from a developing country. Chin J Traumatol 2011;14:161-4. [PubMed] [Google Scholar]
- 14.Schneider T, Volz K, Dienemann H, et al. Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg 2009;8:571-6. 10.1510/icvts.2008.196790 [DOI] [PubMed] [Google Scholar]
- 15.Jamal-Eddine H, Ayed AK, Peric M, et al. Complex bronchial ruptures successfully treated with primary reconstruction and limited lung resection. Gen Thorac Cardiovasc Surg 2009;57:261-3. 10.1007/s11748-008-0351-7 [DOI] [PubMed] [Google Scholar]
- 16.Glazer ES, Meyerson SL. Delayed presentation and treatment of tracheobronchial injuries due to blunt trauma. J Surg Educ 2008;65:302-8. 10.1016/j.jsurg.2008.06.006 [DOI] [PubMed] [Google Scholar]
- 17.Glinjongol C, Pakdirat B. Management of tracheobronchial injuries: a 10-year experience at Ratchaburi hospital. J Med Assoc Thai 2005;88:32-40. [PubMed] [Google Scholar]
- 18.Richardson JD. Outcome of tracheobronchial injuries: a long-term perspective. J Trauma 2004;56:30-6. 10.1097/01.TA.0000108631.72315.78 [DOI] [PubMed] [Google Scholar]
- 19.Ayed AK, Al-Shawaf E. Diagnosis and treatment of traumatic intrathoracic major bronchial disruption. Injury 2004;35:494-9. 10.1016/j.injury.2003.08.014 [DOI] [PubMed] [Google Scholar]
- 20.Balci AE, Eren N, Eren S, et al. Surgical treatment of post-traumatic tracheobronchial injuries: 14-year experience. Eur J Cardiothorac Surg 2002;22:984-9. 10.1016/S1010-7940(02)00591-2 [DOI] [PubMed] [Google Scholar]
- 21.Dewan RK, Mishra AK, Lewate VK, et al. Delayed presentation and surgical management of a bronchial tear. Indian J Chest Dis Allied Sci 2003;45:205-8. [PubMed] [Google Scholar]
- 22.Chen D, Han L, Hu Y, et al. Diagnosis and treatment of bronchial rupture from blunt thoracic trauma. Chin Med J (Engl) 2001;114:540-1. [PubMed] [Google Scholar]
- 23.Mussi A, Ambrogi MC, Ribechini A, et al. Acute major airway injuries: clinical features and management. Eur J Cardiothorac Surg 2001;20:46-51, discussion -2. [DOI] [PubMed]
- 24.Kiser AC, O'Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001;71:2059-65. 10.1016/S0003-4975(00)02453-X [DOI] [PubMed] [Google Scholar]
- 25.Tcherveniakov A, Tchalakov P, Tcherveniakov P. Traumatic and iatrogenic lesions of the trachea and bronchi. Eur J Cardiothorac Surg 2001;19:19-24. 10.1016/S1010-7940(00)00610-2 [DOI] [PubMed] [Google Scholar]
- 26.Cassada DC, Munyikwa MP, Moniz MP, et al. Acute injuries of the trachea and major bronchi: importance of early diagnosis. Ann Thorac Surg 2000;69:1563-7. 10.1016/S0003-4975(00)01077-8 [DOI] [PubMed] [Google Scholar]
- 27.Matsumoto K, Noguchi T, Ishikawa R, et al. The surgical treatment of lung lacerations and major bronchial disruptions caused by blunt thoracic trauma. Surg Today 1998;28:162-6. 10.1007/s005950050099 [DOI] [PubMed] [Google Scholar]
- 28.Rossbach MM, Johnson SB, Gomez MA, et al. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg 1998;65:182-6. 10.1016/S0003-4975(97)01001-1 [DOI] [PubMed] [Google Scholar]
- 29.Wu MH, Tseng YL, Lin MY, et al. Surgical results of 23 patients with tracheobronchial injuries. Respirology 1997;2:127-30. 10.1111/j.1440-1843.1997.tb00065.x [DOI] [PubMed] [Google Scholar]
- 30.Huh J, Milliken JC, Chen JC. Management of tracheobronchial injuries following blunt and penetrating trauma. Am Surg 1997;63:896-9. [PubMed] [Google Scholar]
- 31.Barmada H, Gibbons JR. Tracheobronchial injury in blunt and penetrating chest trauma. Chest 1994;106:74-8. 10.1378/chest.106.1.74 [DOI] [PubMed] [Google Scholar]
- 32.Lin MY, Wu MH, Chan CS, et al. Bronchial rupture caused by blunt chest injury. Ann Emerg Med 1995;25:412-5. 10.1016/S0196-0644(95)70302-0 [DOI] [PubMed] [Google Scholar]
- 33.Iwasaki M, Kaga K, Ogawa J, et al. Bronchoscopy findings and early treatment of patients with blunt tracheo-bronchial trauma. J Cardiovasc Surg (Torino) 1994;35:269-71. [PubMed] [Google Scholar]
- 34.Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways from blunt trauma: treatment of complex injuries. Ann Thorac Surg 1992;54:177-83. 10.1016/0003-4975(92)91177-B [DOI] [PubMed] [Google Scholar]
- 35.Velly JF, Martigne C, Moreau JM, et al. Post traumatic tracheobronchial lesions. A follow-up study of 47 cases. Eur J Cardiothorac Surg 1991;5:352-5. 10.1016/1010-7940(91)90051-K [DOI] [PubMed] [Google Scholar]
- 36.Baumgartner F, Sheppard B, de Virgilio C, et al. Tracheal and main bronchial disruptions after blunt chest trauma: presentation and management. Ann Thorac Surg 1990;50:569-74. 10.1016/0003-4975(90)90191-8 [DOI] [PubMed] [Google Scholar]
- 37.Taskinen SO, Salo JA, Halttunen PE, et al. Tracheobronchial rupture due to blunt chest trauma: a follow-up study. Ann Thorac Surg 1989;48:846-9. 10.1016/0003-4975(89)90683-8 [DOI] [PubMed] [Google Scholar]
- 38.de la Rocha AG, Kayler D. Traumatic rupture of the tracheobronchial tree. Can J Surg 1985;28:68-71. [PubMed] [Google Scholar]
- 39.Flynn AE, Thomas AN, Schecter WP. Acute tracheobronchial injury. J Trauma 1989;29:1326-30. 10.1097/00005373-198910000-00005 [DOI] [PubMed] [Google Scholar]
- 40.Thompson DA, Rowlands BJ, Walker WE, et al. Urgent thoracotomy for pulmonary or tracheobronchial injury. J Trauma 1988;28:276-80. 10.1097/00005373-198803000-00002 [DOI] [PubMed] [Google Scholar]
- 41.Kelly JP, Webb WR, Moulder PV, et al. Management of airway trauma. II: Combined injuries of the trachea and esophagus. Ann Thorac Surg 1987;43:160-3. 10.1016/S0003-4975(10)60387-6 [DOI] [PubMed] [Google Scholar]
- 42.Cheaito A, Tillou A, Lewis C, et al. Traumatic bronchial injury. Int J Surg Case Rep 2016;27:172-5. 10.1016/j.ijscr.2016.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhao Z, Zhang T, Yin X, et al. Update on the diagnosis and treatment of tracheal and bronchial injury. J Thorac Dis 2017;9:E50-6. 10.21037/jtd.2017.01.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Altinok T, Can A. Management of tracheobronchial injuries. Eurasian J Med 2014;46:209-15. 10.5152/eajm.2014.42 [DOI] [PMC free article] [PubMed] [Google Scholar]


