Abstract
Background
Previous studies have found that the prescription rates of inhaled corticosteroid (ICS) were considerably low although it is recommended as the optimal asthma treatment. The aim of this study was to analyze the current status of ICS prescription for asthma patients in the South Korea.
Methods
We evaluated quality assessment data based on nationwide Health Insurance Review and Service (HIRA) database from July 2013 to June 2014. ICS prescription rates in asthma patients were analyzed by types and specialty of medical institutions. Also, we graded medical institutions by their ICS prescription rate. In addition, ICS prescription rates were calculated by patient gender, age, and insurance type.
Results
This study included 831,613 patients and 16,804 institutions in the analysis. The overall mean ICS prescription rate was 22.58%. Tertiary hospitals had the highest mean prescription rate (84.16%) whereas primary healthcare clinics had the lowest (20.71%). By specialty, internal medicine physicians prescribed ICS more frequently compared to other specialists. Of all, 47.17% of medical institutions prescribed ICS to <10% of asthma patients, while less than 6% of institutions prescribed ICS to >80% of asthma patients. Also, we found that female and patients with age >90 or <20 years exhibited lower ICS prescription rate.
Conclusions
The ICS prescription rate was found to be inadequate, given the importance of ICS as an asthma treatment. The prescription rates were especially low in primary healthcare clinics, and by specialists in fields other than internal medicine.
Keywords: Inhaled corticosteroid (ICS), asthma, Health Insurance Review and Service (HIRA), Korea, nationwide-population-based
Introduction
Asthma is a common chronic disease associated with a substantial social and economic burden. The disease affects 7–10% of all persons worldwide, i.e., more than 300 million people, and its prevalence is increasing (1-3). Asthmatics exhibit low productivity, have a poor quality of life, and must deal with the high financial cost of remedies, especially in sub-optimally controlled patients (4-6). Although high-quality care is helpful, less than half of all asthma is well-controlled (6-9), for various reasons (10,11) including disease-, doctor-, and patient-specific factors. Often, treatment is inappropriate because of physician ignorance and/or patient nonadherence (12). The Global Initiative for Asthma (GINA) 2016 guideline states that inhaled corticosteroid (ICS) should be prescribed to asthma patients at steps 2–5 of disease, and should also be considered for those at step 1 (13). However, previous studies found that ICS use rate was relatively low (14,15). To eliminate such underutilization, it is important to analyze the current status of ICS prescription.
In the South Korea, almost all persons are enrolled in national health insurance (NHI) systems, either the NHI, National Medical Aid (NMA), or the Korea Veterans Health Service (16). All medical institutions claim reimbursements from the Health Insurance Review and Service (HIRA), which monitors and approves such charges. Also, HIRA collects clinical data reported by the claiming doctors. Thus, HIRA has data on almost every asthmatic who has visited a medical institution.
We analyzed the current status of ICS prescriptions in Korea. We studied the ICS prescription rates of various healthcare institutions and medical specialists, and the general characteristics of patients.
Methods
Data source and selection
This was a nationwide population-based study that used the HIRA database on insurance claims made by medical institutions. We extracted patient data from July 2013 to June 2014; these included general demographic data (age, gender, type of insurance); diagnoses based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10); and the type of medical institution or medical specialist visited. The inclusion criteria were: (I) age >15 years; (II) primary or first secondary diagnosis of asthma (ICD-10 codes J45 and J46, respectively); and either (III) prescription of asthma medication more than once in an outpatient clinic or (IV) a history of systemic corticosteroid use plus a visit to an outpatient clinic followed by prescription of asthma medication.
Medical institutions
Medical institutions were categorized as tertiary hospitals, general hospitals, hospitals, convalescent hospitals, primary healthcare clinics, public health centers, branch offices of public health centers, and county hospitals. Definitions of each medical institutions are shown in Table 1. Any other medical institution, such as oriental hospitals, dental clinics, and maternity clinics, were excluded, as were medical institutions that did not receive any visits from asthma patients. Doctors were also categorized by medical specialty (internal medicine, general practice, otorhinolaryngology, pediatrics, family medicine, or other). Internal medicine is defined as doctors who graduated medical college, trained in internship and residency and achieved certification of the specialty in internal medicine. General practitioner is defined as doctors who graduated medical college and did not achieved any specialty. Otorhinolaryngology is defined as doctors who graduated medical college, trained in internship and residency and achieved certification of the specialty in otorhinolaryngology. Pediatrics is defined as doctors who graduated medical college, trained in internship and residency and achieved certification of the specialty in pediatrics. Family medicine is defined as doctors who graduated medical college, trained in internship and residency and achieved certification of the specialty in family medicine. Others is defined as doctors who graduated medical college, trained in internship and residency and achieved certification of the specialty other than previous specialties.
Table 1. Definitions of each type of medical institutions.
| Type of medical institutions | Definition |
|---|---|
| Tertiary hospital | General hospitals which provide specialized medical practice for disease with high severity |
| General hospital | Hospitals with more than 100 beds and more than 7 or 9 medical specialties |
| Hospital | Medical center with more than 30 beds |
| Convalescent hospital | Hospital which mainly provide convalescent services |
| Primary healthcare clinic | Medical center with less than 30 beds, which mainly provide primary medical service |
| Public health center | Medical center established by local government |
| Branches of public health center | Branches of public health center, which covers smaller region in need of medical service |
| County hospital | Public health center that meet the qualifications as hospital |
ICS prescription rate
The ICS prescription rate was the ratio of the number of patients prescribed ICS to all asthmatics. The rates were calculated for the different medical institutions and specialties. Also, we graded medical institutions by their ICS prescription rate. In addition, we analyzed prescription rates by patient gender, age and 3 different health services (NHI: covers every citizen in the Republic of Korea who are resident in the nation. Exclude people who are covered by NMA or Korea Veterans Health Service. NMA: Covers people who are not capable of make a living by themselves that government decided to support their maintenance of livelihood, medical wellness, residence and education. Korea Veterans Health Service; Covers patriots and veterans who dedicated to the nation.)
Ethics
Our study was approved by the ethics committee of Seoul St. Mary’s Hospital (KIRB-0E482-001).
Statistical analysis
The chi-squared test was used to compare categorical variables. The Mantel-Haenszel chi-squared test was employed to assess correlations between such variables. All statistical analyses were conducted using SAS software (ver. 9.2; SAS Institute, Cary, NC, USA).
Results
Subjects
We included 831,613 patients and 16,804 institutions in the analysis (Table 2). Primary healthcare clinics constituted the largest proportion of institutions (14,745) and treated the most patients (686,063). Number of patients per institution were 46.53. In terms of tertiary hospitals, 43 institutions treated 43,471 patients, and number of patients per institution were 1010.95.
Table 2. Number of patients by institution type.
| Type of medical institutions | Subjects for evaluation | Patient number/institution (n) | |
|---|---|---|---|
| Number of institutions (n) (%) | Number of patients (n) (%) | ||
| Overall | 16,804 (100.00) | 831,613 (100.00) | 49.49 |
| Tertiary hospital | 43 (0.26) | 43,471 (5.23) | 1010.95 |
| General hospital | 280 (1.67) | 83,194 (10.00) | 297.12 |
| Hospital | 910 (5.42) | 44,503 (5.35) | 48.90 |
| Convalescent hospital | 379 (2.26) | 2,933 (0.35) | 7.74 |
| Primary healthcare clinic | 14,745 (87.75) | 686,063 (82.50) | 46.53 |
| Public health center | 212 (1.26) | 2,424 (0.29) | 11.43 |
| Branch office of public health center | 222 (1.32) | 532 (0.06) | 2.40 |
| County hospital | 13 (0.08) | 416 (0.05) | 32.00 |
ICS prescription rates
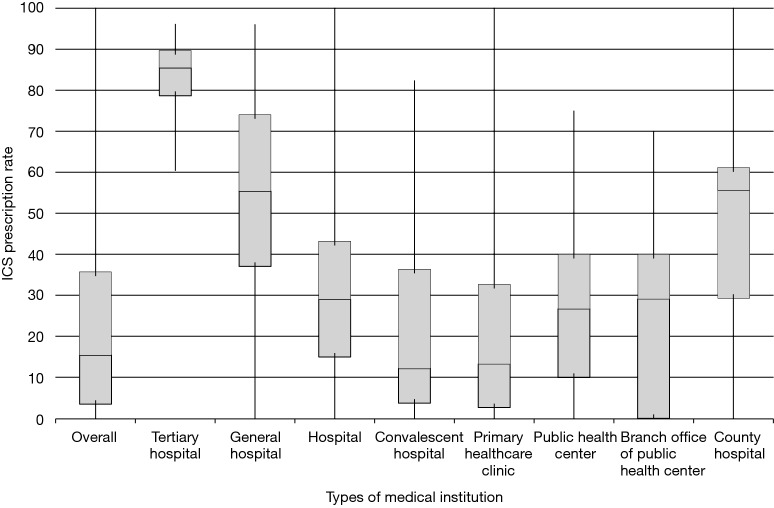
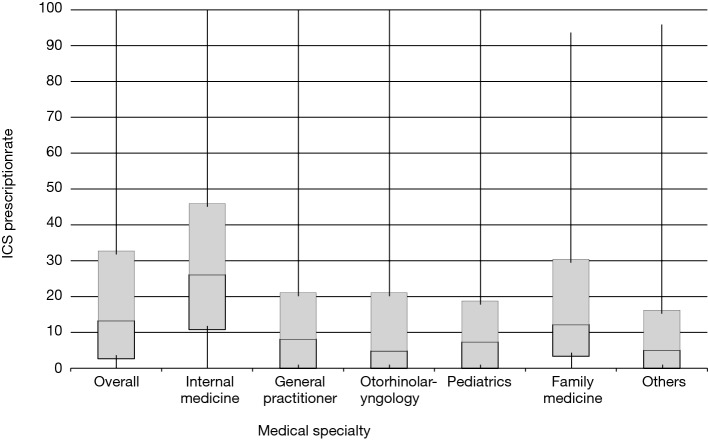
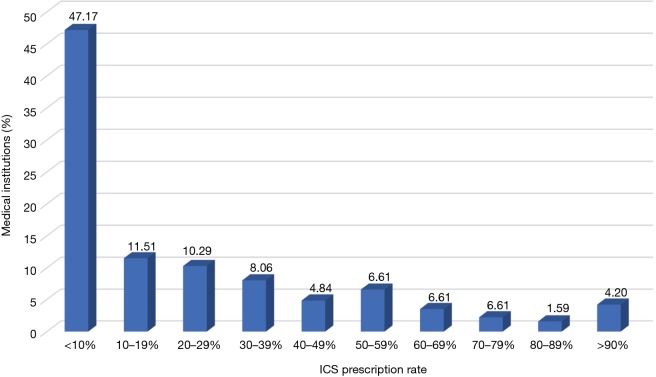
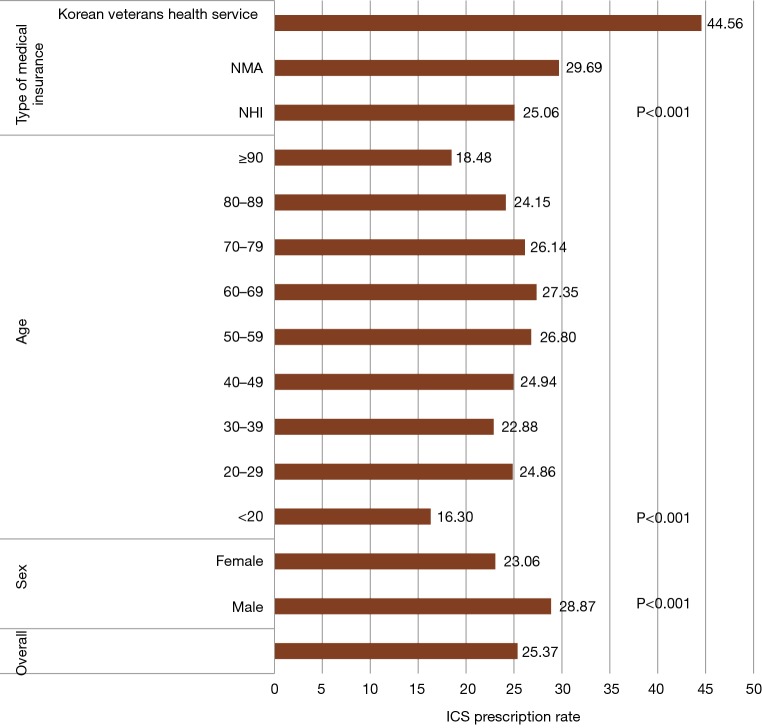
The overall mean ICS prescription rate was 22.58%. The prescription rates by medical institution type are shown in Figure 1. Tertiary hospitals (84.16%) and general hospitals (54.94%) had the highest mean prescription rates and convalescent hospitals (19.57%), and primary healthcare clinics (20.71%) had the lowest. ICS prescription rates by doctors in primary healthcare clinics by medical specialty are shown in Figure 2. Internal medicine physicians (30.43%) had the highest mean prescription rate and all other specialists had mean rates <20%. The ICS prescription rates of the various medical institutions are shown in Figure 3. Overall, 47.17% of all institutions prescribed ICS to <10% of asthma patients, and <6% of institutions prescribed ICS to >80% of asthma patients. We also studied ICS prescription rate by general patient characteristics (Figure 4). Male patients received more ICS prescriptions than females (28.87% vs. 23.06%, P<0.001 by the chi-squared test). Although patients aged 20–90 years exhibited similar prescription rates, the rates for those aged >90 or <20 years were lower (P<0.001 by the chi-squared test). Patients covered by the Korean Veterans Health Service had a higher ICS prescription rate than those covered by the NHI or NMA (44.56% vs. 25.06% vs. 29.69%, P<0.001 by the chi-squared test, P<0.001 by the Mantel-Haenszel chi-squared test).
Figure 1.
ICS prescription rates of different types of medical institution. Data are expressed as median ± interquartile range. ICS, inhaled corticosteroid.
Figure 2.
ICS prescription rates by doctors in primary healthcare clinics by medical specialty. Data are expressed as median ± interquartile range. ICS, inhaled corticosteroid.
Figure 3.
ICS prescription rates of various medical institution (%). X-axis represents range of ICS prescription rate. Y-axis represents percentage of institution according to ICS prescription rate. ICS, inhaled corticosteroid.
Figure 4.
ICS prescription rates according to general patient characteristics. ICS, inhaled corticosteroid; NMA, National Medical Aid; NHI, national health insurance.
Discussion
Asthma treatment focuses on alleviation of impairment and reduction of risks (17). ICS is very useful in these contexts (18,19). Most treatment guidelines suggest that ICS should be used by asthma patients with persistent symptoms (17,20). Furthermore, increasing evidence suggests that ICS should be considered for those with mild asthma (intermittent symptoms) (step 1 disease of the GINA guideline); this was not recommended previously (21,22).
HIRA performed a qualitative assessment of asthma care after reviewing all medical institutions of Korea, and their prescriptions (23), seeking to improve the quality of asthma care by assessing diagnoses and treatments. We used this database to explore the current status of ICS prescriptions in Korea; we evaluated 831,613 patients and 16,804 institutions. The overall ICS prescription rate was 22.58% and almost half of all institutions prescribed ICS to <10% of asthma patients. Only 6% of institutions prescribed ICS to >80% of patients, which may be appropriate. This is disappointing because ICS is the optimal asthma treatment (13).
ICS is under prescribed by primary healthcare clinics: the prescription rate was 84.16% in tertiary hospitals but only 20.71% in primary healthcare clinics. Promotion of guideline-based therapy in such clinics is key to improve asthma care nationwide. This discrepancy may be a result of different patient number per institution between each type of medical institutions. In tertiary hospital, annual patient number per institution count up to 1,010.95 which may help to maintain specialty for asthma treatment. However, in primary healthcare clinic, the number is much lower as 46.53 that specialized asthma treatment may be compromised. Also, there are some possibility that different disease severities have affected this result. Severe asthma patients may have visited higher grade medical institutions and the prescription rate of ICS would be expected to be higher for those patients. Also, specialists other than internal medicine physicians prescribed ICS very infrequently. Although this result also may have been affected by different disease severity between various medical specialty, undereducation and neglection of ICS in asthma treatment may have been most important factor. Therefore, more improvement should be made especially for primary healthcare clinics or general practitioners. Education and monitoring system should be established for doctors in primary healthcare clinics and general practitioners. Also, system should be made which connects primary healthcare clinics or medical institutions in absence of internal medicine specialists to higher grade hospital for treatment of severe, uncontrolled asthma patients.
There are also some specific problems in Korea regarding low rate of ICS use. First, there is cultural preference for oral medication. Many Korean patients are not still familiar with inhaler. Some patients even refuse to use inhaler. Second, the number of doctors is relatively limited and Korean doctors should take care of many patients in limited time. Thus, time for education for inhaler technique is insufficient. Due to this reason, especially in primary care clinic, doctors give up prescribing inhalers. Third, reimbursement of inhaler also can be a reason. For example, reimbursement criteria for combination therapy of ICS and long acting β2-agonist (ICS/LABA) is asthma patients with partly or uncontrolled. However, some doctors, especially general practitioners, are not exactly aware of these criteria and having hard time to prescribe inhaler.
Previous studies reported that ICS prescription rates ranged from 13% to 77% of the asthmatic population (14,24-28). Several studies showed that ICS prescription rate was disappointing as our study. The Asthma Insights and Reality in Asia-Pacific Study (AIRIAP), which enrolled eight centers in the Asia-Pacific region, reported a lowest ICS prescription rate of 13% (14). A study which enrolled 2,509 asthma patients in United States by telephone survey reported ICS prescription rate as 15% (27). European Community Respiratory Health Survey (ECRHS) II, which is a multicenter study participated by 48 centers in Europe, reported better result of 43%, however the number is still low regarding to the guideline (26). As adherence to long-term ICS therapy was known to be poor in >75% of patients, many asthma patients may not have been receiving appropriate treatment (29).
In contrast, studies from several countries have reported relatively higher ICS prescription rate. A cross-sectional survey proceeded in New Zealand and Australia reported ICS prescription rate of 68.8% and 60.9% (28). This result may have been obtained by universal public health system, directed by well-educated general practitioner and specialists. In Canada, primary care models were improved to provide more comprehensive care (25). The ICS prescription rate rose by 5.1% over 4 years (from 72.9% to 76.6%, P<0.001). As the baseline rate was already relatively high, the improvement would be greater in other countries with low pre-improvement baselines.
We found that male and elderly patients (aged 50 to 80) received ICS more often than female and younger patients. Possible reason for the age difference is that elderly patients tend to have more severe disease and require higher ICS dose compared to younger patients (30). Doctors may have been more cautious when treating asthma patients with severe disease status. However, as previous studies showed that disease severity is higher in female patients, other factors may have influenced the gender difference (31,32). Further studies are needed, especially for the gender difference of disease severity in the South Korea.
Previous studies reported conflicting results for age and gender difference of ICS prescription rate. Steppuhn et al. found that the ICS prescription rate was higher in males (39.9% vs. 37.5%) and the elderly (84% vs. 67%) than in female and younger patients, in agreement with our findings (24). However, Schatz et al. reported that females received ICS more often than males (33), perhaps because disease severity was greater in females, as reflected in a higher hospitalization rate (OR: 1.70).
Difference of ICS prescription rate between different health service may be explained by different medical cost burdened to patients. Korean Veterans Health Service and NHA covers profound amount of medical costs compared to NHI, which may improve accessibility to better medical care.
A strength of our study was that we used a very large nationwide database (with information on >50,000,000 persons) and evaluated a large number of institutions. As HIRA covers almost all medical expenses incurred in Korea, the database reliably reflects real-world asthma care (15). Also, to the best of our knowledge, this is the first study to show that ICS prescription rate differs by physician specialty. This study provides valuable reference data on asthma care, which will guide healthcare policy seeking to improve the quality of asthma management.
However, our work had certain limitations. First, the study was observational and retrospective in nature; several forms of bias, such as selection bias or observer bias, may have been present. However, the HIRA database has minimal missing data, such that bias may be well controlled. Second, we evaluated only 1-year data; longer follow-up is needed. Also, we included only asthma patients who visited healthcare centers at least twice. Some patients may visit less than once a year, so we may have underestimated the asthma population on that basis (34,35). Since we collected nationwide claim data during one-year period from not only referral hospital but also primary care clinics, we believe the number of asthma patients who did not use any asthma medication for a year were very small. Third, we defined asthma patients only by ICD-10 code and prescription of asthma medication. However, our working definition of asthma has been used consistently in our previous studies (15,36,37).
Conclusions
We analyzed the nationwide 2013 HIRA database to assess national ICS prescription rates in asthmatics; the rate was found to be inadequate, given the importance of ICS as an asthma treatment. The prescription rates were especially low in primary healthcare clinics, and by specialists in fields other than internal medicine.
Acknowledgements
This study was supported by HIRA (Join Project on Quality Assessment Research).
Ethical Statement: Our study was approved by the ethics committee of Seoul St. Mary’s Hospital (KIRB-0E482-001).
Footnotes
Conflicts of Interest: CK Rhee received consulting/lecture fees from MSD, AstraZeneca, Novartis, GSK, Takeda, Mundipharma, Sandoz, Boehringer-Ingelheim, and Teva-Handok. The other authors have no conflicts of interest to declare.
References
- 1.Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469-78. 10.1111/j.1398-9995.2004.00526.x [DOI] [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Bailey C, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief 2012:1-8. [PubMed] [Google Scholar]
- 3.Anandan C, Nurmatov U, van Schayck OC, et al. Is the prevalence of asthma declining? Systematic review of epidemiological studies. Allergy 2010;65:152-67. 10.1111/j.1398-9995.2009.02244.x [DOI] [PubMed] [Google Scholar]
- 4.Sullivan PW, Slejko JF, Ghushchyan VH, et al. The relationship between asthma, asthma control and economic outcomes in the United States. J Asthma 2014;51:769-78. 10.3109/02770903.2014.906607 [DOI] [PubMed] [Google Scholar]
- 5.Dominguez-Ortega J, Phillips-Angles E, Barranco P, et al. Cost-effectiveness of asthma therapy: a comprehensive review. J Asthma 2015;52:529-37. 10.3109/02770903.2014.999283 [DOI] [PubMed] [Google Scholar]
- 6.Williams SA, Wagner S, Kannan H, et al. The association between asthma control and health care utilization, work productivity loss and health-related quality of life. J Occup Environ Med 2009;51:780-5. 10.1097/JOM.0b013e3181abb019 [DOI] [PubMed] [Google Scholar]
- 7.Demoly P, Annunziata K, Gubba E, et al. Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev 2012;21:66-74. 10.1183/09059180.00008111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braido F, Brusselle G, Guastalla D, et al. Determinants and impact of suboptimal asthma control in Europe: The INTERNATIONAL CROSS-SECTIONAL AND LONGITUDINAL ASSESSMENT ON ASTHMA CONTROL (LIAISON) study. Respir Res 2016;17:51. 10.1186/s12931-016-0374-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bosnic-Anticevich S, Kritikos V, Carter V, et al. Lack of asthma and rhinitis control in general practitioner-managed patients prescribed fixed-dose combination therapy in Australia. J Asthma 2018;55:684-94. [DOI] [PubMed] [Google Scholar]
- 10.Braido F. Failure in asthma control: reasons and consequences. Scientifica (Cairo) 2013;2013:549252. 10.1155/2013/549252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chapman KR, Boulet LP, Rea RM, et al. Suboptimal asthma control: prevalence, detection and consequences in general practice. Eur Respir J 2008;31:320-5. 10.1183/09031936.00039707 [DOI] [PubMed] [Google Scholar]
- 12.Baiardini I, Braido F, Bonini M, et al. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol 2009;9:228-33. 10.1097/ACI.0b013e32832b4651 [DOI] [PubMed] [Google Scholar]
- 13.Guideline GINA, 2016. Available online: http://ginasthma.org
- 14.Lai CK, De Guia TS, Kim YY, et al. Asthma control in the Asia-Pacific region: the Asthma Insights and Reality in Asia-Pacific Study. J Allergy Clin Immunol 2003;111:263-8. 10.1067/mai.2003.30 [DOI] [PubMed] [Google Scholar]
- 15.Choi JY, Yoon HK, Lee JH, et al. Current status of asthma care in South Korea: nationwide the Health Insurance Review and Assessment Service database. J Thorac Dis 2017;9:3208-14. 10.21037/jtd.2017.08.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grace MS, Baxter M, Dubuis E, et al. Transient receptor potential (TRP) channels in the airway: role in airway disease. Br J Pharmacol 2014;171:2593-607. 10.1111/bph.12538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCracken JL, Veeranki SP, Ameredes BT, et al. Diagnosis and Management of Asthma in Adults: A Review. Jama 2017;318:279-90. 10.1001/jama.2017.8372 [DOI] [PubMed] [Google Scholar]
- 18.Adams NP, Bestall JC, Lasserson TJ, et al. Fluticasone versus placebo for chronic asthma in adults and children. Cochrane Database Syst Rev 2008:CD003135. [DOI] [PubMed] [Google Scholar]
- 19.Corrao G, Arfe A, Nicotra F, et al. Persistence with inhaled corticosteroids reduces the risk of exacerbation among adults with asthma: A real-world investigation. Respirology 2016;21:1034-40. 10.1111/resp.12791 [DOI] [PubMed] [Google Scholar]
- 20.Fanta CH. Asthma. N Engl J Med 2009;360:1002-14. 10.1056/NEJMra0804579 [DOI] [PubMed] [Google Scholar]
- 21.Reddel HK, Busse WW, Pedersen S, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post-hoc efficacy analysis of the START study. Lancet 2017;389:157-66. 10.1016/S0140-6736(16)31399-X [DOI] [PubMed] [Google Scholar]
- 22.Boulet LP, Turcotte H, Prince P, et al. Benefits of low-dose inhaled fluticasone on airway response and inflammation in mild asthma. Respir Med 2009;103:1554-63. 10.1016/j.rmed.2009.02.015 [DOI] [PubMed] [Google Scholar]
- 23.Kim SR, Lee YC, Sung MJ, et al. Current Epidemiological Data on Asthma Management in South Korea from Qualitative Assessment of Asthma Management by Health Insurance Review and Assessment Service (HIRA). Tuberc Respir Dis (Seoul) 2017;80:221-5. 10.4046/trd.2017.80.3.221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steppuhn H, Langen U, Mueters S, et al. Asthma management practices in adults--findings from the German Health Update (GEDA) 2010 and the German National Health Interview and Examination Survey (DEGS1) 2008-2011. J Asthma 2016;53:50-61. 10.3109/02770903.2015.1059853 [DOI] [PubMed] [Google Scholar]
- 25.To T, Guan J, Zhu J, et al. Quality of asthma care under different primary care models in Canada: a population-based study. BMC Fam Pract 2015;16:19. 10.1186/s12875-015-0232-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol 2007;120:1360-7. 10.1016/j.jaci.2007.09.019 [DOI] [PubMed] [Google Scholar]
- 27.Adams RJ, Fuhlbrigge A, Guilbert T, et al. Inadequate use of asthma medication in the United States: results of the asthma in America national population survey. J Allergy Clin Immunol 2002;110:58-64. 10.1067/mai.2002.125489 [DOI] [PubMed] [Google Scholar]
- 28.Reddel HK, Beckert L, Moran A, et al. Is higher population-level use of ICS/LABA combination associated with better asthma outcomes? Cross-sectional surveys of nationally representative populations in New Zealand and Australia. Respirology 2017;22:1570-8. 10.1111/resp.13123 [DOI] [PubMed] [Google Scholar]
- 29.Laforest L, Belhassen M, Devouassoux G, et al. Long-Term Inhaled Corticosteroid Adherence in Asthma Patients with Short-Term Adherence. J Allergy Clin Immunol Pract 2016;4:890-9.e2. 10.1016/j.jaip.2016.07.008 [DOI] [PubMed] [Google Scholar]
- 30.Ciprandi G, Schiavetti I, Ricciardolo FLM. The impact of aging on outpatients with asthma in a real-world setting. Respir Med 2018;136:58-64. 10.1016/j.rmed.2018.01.018 [DOI] [PubMed] [Google Scholar]
- 31.Fuseini H, Newcomb DC. Mechanisms Driving Gender Differences in Asthma. Curr Allergy Asthma Rep 2017;17:19. 10.1007/s11882-017-0686-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kynyk JA, Mastronarde JG, McCallister JW. Asthma, the sex difference. Curr Opin Pulm Med 2011;17:6-11. 10.1097/MCP.0b013e3283410038 [DOI] [PubMed] [Google Scholar]
- 33.Schatz M, Camargo CA., Jr The relationship of sex to asthma prevalence, health care utilization, and medications in a large managed care organization. Ann Allergy Asthma Immunol 2003;91:553-8. 10.1016/S1081-1206(10)61533-5 [DOI] [PubMed] [Google Scholar]
- 34.Zeiger RS, Baker JW, Kaplan MS, et al. Variability of symptoms in mild persistent asthma: baseline data from the MIAMI study. Respir Med 2004;98:898-905. 10.1016/j.rmed.2004.02.016 [DOI] [PubMed] [Google Scholar]
- 35.Vermeire PA, Rabe KF, Soriano JB, et al. Asthma control and differences in management practices across seven European countries. Respir Med 2002;96:142-9. 10.1053/rmed.2001.1241 [DOI] [PubMed] [Google Scholar]
- 36.Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. Copd 2014;11:163-70. 10.3109/15412555.2013.831061 [DOI] [PubMed] [Google Scholar]
- 37.Park HJ, Byun MK, Kim HJ, et al. Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma. Allergy Asthma Clin Immunol 2018;14:29. 10.1186/s13223-018-0250-0 [DOI] [PMC free article] [PubMed] [Google Scholar]