Summary
Introduction
Despite concerted efforts by governmental and non-governmental organizations, water and adequate sanitation still remain a challenge worldwide. Therefore, this study assessed the availability and utilization of sanitation facilities in Enderta district of Tigray, Ethiopia.
Methods
A cross-sectional study was conducted in May 2016. An interview and observation were conducted in a total of 450 households. An interviewer administered questionnaire and observation checklist were used to collect the data. Multivariable logistic regression was done to identify the predictors of availability and utilization of latrine, hand washing, and drinking water.
Results
Out of 450 households, only 68.4% had latrine of which only 21.4% had hand washing facility near the toilet. Likewise, only 9.3% washed their hand after toilet. However, all households had access to improved water source. In this study, proper utilization of latrine, hand washing, and water facilities was observed in 53%, 42.4% and 36.2% of the study households, respectively. The family size and getting sanitation information from health care providers, health extension workers, and health development army had a positive effect on availability and utilization.
Conclusions
Though Community-Led total sanitation and hygiene approach has been implemented in the study area, the availability and proper utilization of latrine, and hand washing are still low. Only few households used drinking water properly. The education or information on hygienic practices found to affect the availability and utilization of the sanitation facilities positively. Therefore, strengthening the health extension workers and health development army to provide sustainable education and health information is needed.
Keywords: Availability, Utilization, Sanitation, Water, Ethiopia
Introduction
Adequate drinking water, proper sanitation, and hygiene are essential requirements to ensure human health and better economic development [1]. Currently, the importance of water and adequate sanitation is recognized at both local and global levels. In spite of concerted efforts by governmental and non-governmental organizations, water and adequate sanitation are still remained a challenge. Globally, 2.4 billion people still lack improved sanitation facilities, and more than half billion people lack access to improved drinking water sources [2]. And, sub-Saharan Africa is the region where most of these people live. In Ethiopia, though there is a significant improvement in access to water and sanitation facilities, the sanitation coverage is still minimal [3]. An estimated 47.5% and 72% of the population lack access to improved drinking water source and sanitation facilities, respectively [2, 4]. Moreover, open defecation is still practiced by more than a quarter (29%) of the population [5, 6]. In Tigray region, the area in which the current study conducted, the open field defecation rate is 35.6% which is slightly higher than the national level [5]. Further, in 2011 the latrine coverage was 87%, though the utilization rate was very minimal (34%) in the region [7]. However, a higher latrine utilization rate (57.3%) was reported in one of the districts of the region since 2013 [8].
Diarrheal diseases represent the most significant health impact of unimproved sanitation, and extremely high impact upon children [9]. Globally, inadequate sanitation, poor hygiene, and unsafe drinking water contribute to 88% of diarrheal disease [9-11]. Moreover, diarrheal diseases are the second leading cause of death in children under the age of five, estimated that 1.5 million child deaths annually. Severe diarrhea may be life threatening due to fluid loss, particularly in infants, young children, the malnourished and people with impaired immunity such as those living with Human Immunodeficiency Virus (HIV). Likewise, the impact of poor sanitation, hygiene, and unsafe drinking water is also recognized to have a positive effect on the burden of neglected tropical diseases such as trachoma, dracunculiasis and visceral leishmaniasis [12].
In Ethiopia, 60% of overall diseases are related to poor sanitation and lack of hygiene. Diarrhea is the leading cause of under-five mortality causing 23% of all under-five deaths in the country [13]. By improving water, sanitation, and hygiene about 64,540 children could be saved every year in the country. About 40% of under-five children in Ethiopia are stunted, which can be strongly linked to the childhood incidence of diarrhea [13, 14].
The Community-led Total Sanitation and Hygiene (CLTSH) approach has been proven as one of the cost effective approaches to improve the water, sanitation, and hygiene worldwide especially for those with low-income. Thus, with the goal of ending “open defecation” through self-built toilets, and by encouraging appropriate hand washing and water handling practices; the government of Ethiopia has been implementing CLTSH by integrating it with the health extension program in all the nine regions since 2011 [15]. However, political commitment at all levels had focused on sanitation coverage, with less attention given to improving safe water, sanitation, and hygiene practices such as hand-washing, safe water storage and handling, and latrine maintenance and usage [16]. As a result, with all the efforts, the prevalence of sanitation related diseases is still high in the country [17].
There are few studies conducted in Ethiopia [8, 18-21]. However, these studies were focused on larine utilization and they were conducted at the time when the CLTSH was not implemented or too child in the country. They were only focused on utilization of latrine but all issues regarding sanitation and drinking water were not addressed fully. However, the current study was conducted after five years of CLTSH implementation thus the findings could show us the improvement brought by the program. Therefore, the aim of this study is to assess the availability and utilization of sanitary facilities in CLTSH implemented district of Tigray region, Ethiopia. The finding of the study, therefore, will help to design evidence based strategy to enhance availability and utilization of sanitary facilities on the study area. Hence, the CLTSH implementation will be further strengthened.
Methods
STUDY AREA AND DESIGN
A community-based cross-sectional study was conducted in May 2016 in Enderta district. The district is located at the 795 kms north of Addis Ababa, the capital of Ethiopia, and about 12 kms southeast of the Tigray Regional city, Mekelle. The district comprises 17 kebeles (the smallest administrative unit in Ethiopia) and 60 villages. In 2015, the district had a total of 112,154 and 25,489 population and households, respectively. There are 6 health centers, 11 health posts, and 664 health development armies with the total health staffs of 170, of which 35 are Health Extension Workers (HEWs).
STUDY POPULATION
Randomly selected households of the rural community who owned private latrine were the study population for this study.
SAMPLE SIZE, SAMPLING TECHNIQUE AND PROCEDURE
The sample size was determined using single population formula with 2015 estimates of access to sanitation 28% [2], with a margin of error of 0.05% at the 95% confidence level. Then, multiplying by a design effect of 1.5, the total sample size was calculated to be 450. A multistage sampling technique was employed to select the sample households. Primarily, three kebeles were selected randomly. From each kebele, one village was selected randomly. Then, the sample of 450 households was selected based on proportional to population size (PPS) allocation to each of the selected villages. The households were selected by systematic sampling method from the already prepared sampling frame. Then, in the selected households, the household heads were recruited and observations were done.
DATA COLLECTION TOOLS AND PROCEDURE
Data collection tools such as interviewer administered questionnaire and observation checklist were used to collect data from the households. The data collection tools include socio-demographic and other characteristics that would measure the availability and utilization of sanitation facilities and associated factors after reviewing relevant literatures.
OPERATIONAL DEFINITIONS
Presence of sanitation and hygiene facilities such as a latrine, hand washing, and water source was considered as availability. Households were considered as properly utilizing latrine if the latrine is not shared, pit with slab/cover, the compound is free of observable faeces and has functional latrine during the study, having no observable faeces around the squat hole [22]. Households were considered as properly practice hand washing if there was hand washing material with water and soap/or ash during the data collection period. In this study, a household was considered as properly handling water, if the container is clean, has cover and placed away from any source contamination such as animals during the data collection period [22].
DATA QUALITY CONTROL
Prior to data collection training was given to data collectors and supervisors on the content, objective and methods of data collection and interviewing techniques. The pretest was done in 5% of the sample from villages with the population having similar socio-demographic characteristics that were not included in the study and minor correction was done accordingly. The questionnaire was also translated into local language (Tigrigna) and back-translated to English to ensure the consistency of the thought of the questions. During data collection time, a clear introduction that explained the purpose and objectives of the study were provided to respondents. A close supervision, honest communication and on spot decisions were made during data collection.
Validity and reliability of the questionnaire was determined as follows. Face and content validity of the tool was determined based on viewpoints of the experts on the area. Test-retest reliability of the tool was examined by pre-testing the tool on 5% of the sample size in similar context with 10-12 days interval. Hence, the questionnaire was reviewed and analysed for repeatability and internal consistency aspects. Cronbach’s alpha coefficient was also used to assess internal consistency and said to be internally consistent if score of 0.8 and above. Repeatability was estimated using the intra-class correlation coefficient (ICC). Based on ICC reliability ranges of less than 0.4 (poor), 0.4-0.7 (fair to good), 0.6-0.8 (good) and 0.8-1 (excellent), the reliability of the questionnaire was considered excellent.
DATA MANAGEMENT AND ANALYSIS
Quantitative data were checked for completeness, edited, coded, entered and analyzed using STATA version 13 (Stata Corp. Texas, USA). The descriptive summary was done using frequencies and proportions. Multivariable logistic regression was done to identify the independent predictors of availability and utilization of sanitation facilities and drinking water. The strength of association was measured by odds ratios at their 95% Confidence levels and the statistical significance was set at the p-value of 0.05.
ETHICAL CONSIDERATION
Ethical approval was obtained from the Institutional Review Board of College of Health Sciences, Mekelle University (EBC-06128/2016). Verbal consent was obtained from each study participants after the information about the study like the objective was explained. The participants were informed that it was their right to refuse or withdraw from the study at any point during the course of study. Names and other personal information which could violate the confidentiality of respondents were not recorded and information was kept confidential.
Results
SOCIO-DEMOGRAPHIC CHARACTERISTICS OF HOUSEHOLD HEADS
A total of 450 households were included in the study with 100% response rate. Of the total respondents, 323 (71.8 %) were female headed and 334 (74%) were married. More than half (56%) of households had more than 4 family sizes. About 82% (370) household heads were illiterate (Tab. I).
Tab. I.
Background characteristics of household heads in Enderta Woreda, Ethiopia, 2016 (n = 450).
| Characteristics | Frequency | % |
|---|---|---|
| Family size 1-4 > 4 |
197 253 |
43.8 56.2 |
| Sex (HH head) Male Female |
127 323 |
28.2 71.8 |
| Marital status Single Married Divorced Widowed |
60 334 26 30 |
13.3 74.2 5.8 6.7 |
| Occupational status Farmer Daily laborer Merchant Government employee |
422 12 10 6 |
93.8 2.7 2.2 1.3 |
| Educational status Illiterate Primary Secondary & above |
370 29 51 |
82.2 6.4 11.3 |
HH: household.
AVAILABILITY AND UTILIZATION OF SANITATION FACILITIES
Out of the total observed households (N = 450), 68.4% respondents had the latrine, of which 45.8% were with a cover of the hole. About six in ten (86.7%) households had no faeces on the wall, floor and/or door, and 85.1% households had no faeces on their compound. Sixty-six (21.4%) had hand washing facility near to the toilet. However, fewer than half (42%) of hand washing facilities were with ash/soap. Although all households were using public piped hand pump water and 98.4% of them had a water container with cover, in 61.8% of them the water container was not hygienic. Three hundred ninety-three (87.8%) of the observed Households keep their drinking water away from animals (Tab. II). The overall proper utilization of latrine, hand washing and water were 53.3%, 42.4%, and 36.2%, respectively.
Tab. II.
Availability and utilization of sanitation facilities Enderta Woreda, Ethiopia, 2016.
| Sanitation facilities | Variables | Frequency | % | |
|---|---|---|---|---|
| Availability | Latrine |
Latrine (n = 450) No Yes |
142 308 |
31.6 68.4 |
| Hand washing |
Hand washing facility near the latrine (n = 308) No Yes |
242 66 |
78.6 21.4 |
|
| Water |
Presence of improved drinking water sourcea Yes |
450 | 100 | |
| Utilization | Latrine (n = 308) |
Latrine hole has cover/slab No Yes Absence of faeces on the wall, floor, and door No Yes Absence of faeces on the compound of HHs No Yes Latrine shared Yes No |
103 205 41 267 46 262 41 267 |
33.4 66.6 13.3 86.7 14.9 85.1 13.1 86.9 |
| Hand washing (n = 66) |
Presence of water for hand washing No Yes Presence of soap/ash on the hand washing No Yes |
23 43 38 28 |
34.8 65.2 57.6 42.4 |
|
|
Water (n = 450) |
Is water container covered No Yes Is water container hygienic/dipper not put on floor No Yes Is drinking water away from domestic animals No Yes |
8 442 278 172 55 395 |
1.6 98.4 61.8 38.2 12.2 87.8 |
a: all households had public piped hand pump water.
HAND WASHING PRACTICE
Regarding hand washing practice during critical times, only 9.3% of household wash their hands after toilet. Similarly, lower proportions of households, 27.8%, and 34.2%, washed their hands before feeding their child and after cleaning their child, respectively. Whereas, most of the households, 83.3%, and 90.4%, washed their hands before preparing and eating their food, respectively (Fig. 1).
Fig. 1.
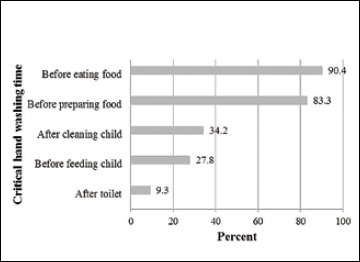
Hand washing practice in the critical times in households of Enderta district, Tigray, Ethiopia, 2016 (n = 450).
FACTORS ASSOCIATED WITH AVAILABILITY OF SANITATION FACILITIES
Family size and getting information or education about sanitation by either health professionals or health extension workers and health development army were positively associated with the availability of latrine. Households who had more than or equals to four family size had 72% (AOR = 1.72; 95% CI (1.13, 2.61)) higher odds of having latrine than those households that had less than four family size. According to trend chi-square test, there was increasing in the trend of having latrine as the number of sources of information about sanitation is increased (P-value < 0.001) (Tab. III). Households that have more than four families had 80% higher [AOR = 1.8; 95% CI (1.00, 3.32)] odds of having hand washing facility than their less than four counterparts.
Tab. III.
Factors associated with availability of sanitation facilities in Enderta district, North Ethiopia.
| Variables | Availability of latrine |
X2-test | AOR (95% CI) | |
|---|---|---|---|---|
| No: n (%) | Yes: n (%) | |||
| Family size | ||||
| 1-4 > 4 |
75 (38.1) 67 (26.5) |
122 (61.9) 186 (73.5) |
1 6.9** |
1 1.72(1.13, 2.61)* |
| Informed by HPs | ||||
| No Yes |
18 (50.0) 124 (29.9) |
18 (50.0) 290 (70.1) |
1 6.2* |
1 2.96 (1.44, 6.09)** |
| Informed by HEWs | ||||
| No Yes |
100 (41.2) 42 (20.3) |
143(58.8) 165(79.7) |
1 22.5*** |
1 2.21 (1.40, 3.47)** |
| Informed by HDAs | ||||
| No Yes |
121 (37.0) | 206 (63.0) | 1 | 1 |
| 21 (17.1) | 102 (82.9) | 16.4*** | 2.32 (1.31, 4.09)** | |
| Source of information about latrine | ||||
| Not heard from any of the (HP, HEW, HDA) Heard from one of (HP, HEW, HDA) Heard from two Heard from three of them |
5 (55.6) 99 (43.4) 26 (21.1) 12 (13.3) |
4 (44.4) 129 (56.6) 97 (78.9) 78 (86.7) |
5.9a*** | - |
| Availability of hand washing facility | X2-test | AOR (95% CI) | ||
| No: n (%) | Yes: n (%) | |||
| Family size | ||||
| 1-4 > 4 |
103 (84.4) 139 (74.7) |
19 (15.6) 47 (25.3) |
4.1* | 1.8 (1.00, 3.32)* |
| Informed by HDAs | ||||
| No Yes |
152 (73.8) 90 (88.2) |
54 (26.2) 12 (11.8) |
8.5** | 0.37(0.19, 0.74)** |
HPs: health professionals; HDAs: health development armies; HEWs: health extension workers; AOR: adjusted odds ratio;
a: trend Chi-square test; significant at p-value:
*< 0.05
**< 0.01
***< 0.001.
FACTORS ASSOCIATED WITH UTILIZATION OF SANITATION FACILITIES
Having hand washing facility, properly use water and informed about sanitation by health development Army (HAD) were positively associated with latrine utilization. Households having hand washing facility had 2.53 times [AOR = 2.53; 95% CI (1.38, 4.59)] higher odds to utilize latrine than households that did not have hand washing facility. Likewise, those who properly use water had 97% higher [AOR = 1.97; 95% CI (1.22, 3.20)] odds to use latrine than households who did not use water properly. Households who got information/education about sanitation had 2.31 times [AOR = 2.31; 95% CI (1.39, 3.86)] higher odds to use latrine properly than their counterparts (Tab. IV).
Tab. IV.
Factors associated with utilization of sanitation facilities in Enderta district, North Ethiopia.
| Variables | Utilization of latrine | X2- test |
AOR (95% CI) | |
|---|---|---|---|---|
| No: n (%) | Yes: n (%) | |||
| Hand washing facility | ||||
| Not available Available |
123 (50.8) 21 (31.8) |
119 (49.2) 45 (68.2) |
7.52** | 1 2.53 (1.38, 4.59)** |
| Proper water utilization | ||||
| No Yes |
98 (53.3) 46 (37.1) |
86 (47.7) 78 (62.9) |
7.77** | 1 1.97 (1.22, 3.20)** |
| Informed by HDAs | ||||
| No Yes |
107 (51.9) 37 (36.3) |
99 (48.1) 65 (63.7) |
6.72** | 1 2.31 (1.39, 3.86)** |
| Utilization of hand washing facility |
X2- test |
AOR (95%CI) |
||
| No: n (%) | Yes: n (%) | |||
| Informed by HEWs | ||||
| No Yes |
28 (70.0) 10 (38.5) |
12 (30.0) 16 (61.5) |
6.41* | 1 3.73 (1.32, 10.56)* |
| Proper utilization/handling of water |
X2- test |
AOR (95% CI) |
||
| No: n (%) | Yes: n (%) | |||
| Informed by HDAs | ||||
| No Yes |
207 (63.3) 80 (65.0) |
327 (36.7) 43 (35.0) |
0.11 | 1 0.57 (0.33, 0.99)* |
| Informed by HEWs | ||||
| No Yes |
178 (73.3) 109 (52.7) |
65 (26.7) 98 (47.3) |
20.5*** | 1 2.05 (1.23, 3.42)** |
| Latrine utilization | ||||
| No Yes |
98 (68.1) 86 (52.4) |
46 (31.9) 78 (47.6) |
7.77** | 1 2.07 (1.27, 3.38)** |
| Visited by sanitation committee | ||||
| No Yes |
94 (75.8) 193 (59.2) |
30 (24.2) 133 (40.8) |
1 10.72** |
1 2.23 (1.27, 3.89)** |
HDAs: health development armies; HEWs: health extension workers; AOR: adjusted odds ratio; significant at p-value:
*< 0.05
** < 0.01
***< 0.001.
Getting information about sanitation from HEWs was positively associated with utilization of hand washing facility. Moreover, getting information about sanitation from HEWs, using the latrine and visited by the community sanitation committee were positively associated with proper utilization of water. Households who used latrine properly had 2.07 times [AOR = 2.07; 95% CI (1.27, 3.38)] higher odds of using water properly than those who did not use latrine (Tab. IV).
Discussion
The current study found that 68.4% of the household had latrine though only 21.4% of these households had hand washing facility near the latrine. Our finding is comparable with the 2015 national sanitation review report that reported 68% and 61% of latrine coverage nationally and in Tigray region, respectively [5]. The present study also showed that all the households in the study area had access to improved water source (public stand hand pump) [2]. However, the proper utilization was low in which 53%, 42.4% and 36.2% of households utilize latrine, hand washing, and drinking water properly, respectively. The current finding is consistent with the previous finding reported in 2013 as 57.3%, and 61.2% of latrine utilization rate [8, 20]. Besides, the present finding clearly indicates the availability of the latrine could not be a guarantee for proper utilization.
Though more than two-third of households had a latrine, only a few (9.3%) households wash hands after visiting toilet that is much lower than the nationally reported 45% [5]. Further, low proportions of households washed their hands before feeding the child (27.8%) and after cleaning their child (34.2%). However, the present study revealed higher proportions of households wash their hands before preparing (83.3%) and eating (90.4%) food which is consistent with national survey report of 2016 in which 96% of households wash their hands before eating food.
The current study also found that family size and getting information or education about water, sanitation, and hygiene from either health professionals or health extension workers or HDA were positively affected the availability of latrine in the households. That is, the households who had more than four family members had higher odds of having latrine than their counterparts. This is consistent with the finding from Ethiopia in which households who had been visited by health professionals are more likely to construct latrine and good sanitation practice [18]. Also, it was found that the size of the family was positively related with the availability of hand washing facility. The households that have more than four family members had 80% higher odds of having hand washing facility near the toilet than those who have less than four family members.
Regarding utilization, households who had hand washing facility near their toilet were 2.5 times likely to use latrine properly. Likewise, those who use water properly had 97% higher odds to utilize latrine properly than their counterparts. Providing health information about sanitation through HDA, HEWs, and health professionals had a positive effect on proper utilization of latrine, hand washing, and water. In line with the present finding, it is evidenced that having materials to build the latrine and to improve latrine utilization have a positive effect on the utilization of latrine [8]. Further, it has been evidenced that households educated or get informed in hygienic practices are more likely to practice latrine, water, and hygiene properly [23].
Being a model in healthy practice is evidenced to enhance the community to practice healthy behaviors [24, 25]. Likewise, in the present study, the households that used latrine properly had 2 times higher odds of utilizing water properly than those who had improper latrine use. Visit by community sanitation committee was found to have a positive effect on proper utilization of water. In line with this, a study conducted in 2015, in Ethiopia shows the households need sustainable information and education in order to utilize latrine, water and hygiene practice properly [26].
As the present study attempted to collect appropriate primary data through observation and interview, the findings are highly valid and reliable for the study area and can be applied in other similar settings.
Conclusions
This study found that significant proportions of households have no latrine and hand washing facility though they have access to improved water source. It was also found that only a few utilize latrine, hand washing, and drinking water properly. Further, though more than three-fourth (68.4%) of households had a latrine, the present study found that only 9.3% of them wash their hands after toilet. In general, our findings showed the availability and proper utilization of latrine, hand washing, and water depends mainly on the follow-up of households to encourage and educate on hygienic practices by either health extension workers, HDAs or the sanitation committee. To have important sustainable outcomes from CLTSH program, it was evidenced to provide training to local actors including HEWs and HDA [27]. Therefore, strengthening the HEWs and the HDAs to provide sustainable education and health information is needed.
Acknowledgements
The authors are thankful for the data collectors and the study participants who involved in the study. We would like to extend our gratitude for College of Health Sciences, Mekelle University that supported on the overall research process.
Abbreviations/acronyms
- AOR
Adjusted Odds Ratio
- CI
Confidence Interval
- CLTSH
Community-led Total Sanitation and Hygiene
- HDA
Health Development Army
- HEWs
Health Extension Workers
- HHs
Households
- ICC
Intra-class Correlation Coefficient
- PPS
Proportional to Population Size
- HPs
Health Professionals.
Footnotes
Conflict of interest statement
None declared.
Authors' contributions
All authors involved in conception, design, coordination and supervision of the research project. AB, ZA and MB have made analysis of the data and interpretation of the results. AB and MB wrote the manuscript. All authors revised the manuscript and gave their contribution to improve the paper. All authors read and approved the final manuscript.
References
- [1].Eid U. The importance of water, sanitation, and hygiene as keys to national development. Johns Hopkins water magazine 2015; Available at: http://water.jhu.edu/index.php/magazine/climate-change-and-health-why-the-link-to-water-is-critical. Accessed on 02/02/2016.
- [2].WHO and UNICEF. Progress on sanitation and drinking water - 2015 update and MDG assessment. Geneva; 2015. [Google Scholar]
- [3].WHO. Sanitation, drinking-water and hygiene status overview. 2015. [Google Scholar]
- [4].Central Statistical Agency (Ethiopia). Ethiopia mini demographic and health survey. Ethiopia: Addis Ababa; 2014. [Google Scholar]
- [5].UNICEF. Progress on CLTSH - findings from a national review of rural sanitation in Ethiopia: WASH learning note. 2016. [Google Scholar]
- [6].Beyene A, Hailu T, Faris K, Kloos H. Current state and trends of access to sanitation in Ethiopia and the need to revise indicators to monitor progress in the post-2015 era. BMC Public Health 2015;15(451):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Admasu A, Kiros M, Memhur A. Baseline survey report of Tigray region on WASH. 2011. [Google Scholar]
- [8].Debesay N, Ingale L, Gebresilassie A, Assefa H, Yemane D. Latrine utilization and associated factors in the rural communities of Gulomekada District, Tigray Region, North Ethiopia, 2013: a community based cross-sectional study. J Community Med Heal Educ 2015;5(2):5-10. [Google Scholar]
- [9].Bartram J, Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med 2010;7(11):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bos R, Gore F, Bartram J. Safer water, better health: costs, benefts and sustainability of interventions to protect and promote health. WHO; 2008. [Google Scholar]
- [11].WHO. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva; 2009. [Google Scholar]
- [12].WHO. Water, sanitation & hygiene for accelerating and sustaining progress on neglected tropical diseases: a global strategy 2015-2020. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].UNICEF. Sanitation priorty country factsheet, Ethiopia. 2014. Available at: http://www.unicef.org/ethiopia/Ethiopia_Fact_Sheet_Jan_2014._final.pdf.
- [14].Anteneh A, Kumie A. Assessment of the impact of latrine utilization on diarrhoeal diseases in the rural community of Hulet Ejju Enessie. Ethiop J Heal Dev 2010;24(2):110-8. [Google Scholar]
- [15].Crocker J, Ryan Rowe. Community-led total sanitation in Ethiopia findings from a situational assessment. The water institute at UNC, Plan International Ethiopia. 2015. [Google Scholar]
- [16].Federal Democratic Republic of Ethiopia. Part II: National hygiene & sanitation strategic action plan for rural, per-urban & informal settlements in Ethiopia. Ethiopia: Addis Ababa; 2011. [Google Scholar]
- [17].Federal Democratic Republic of Ethiopia Ministry of Health. Health and health related indicator, EFY 2007. Ethiopia: Addis Ababa; 2015. [Google Scholar]
- [18].Awoke W, Muche S. A cross sectional study : latrine coverage and associated factors among rural communities in the District of Bahir Dar Zuria, Ethiopia. BMC Public Health: 2013;13(99):2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ashebir Y, Sharma HR, Alemu K, Kebede G. Latrine use among rural households in northern Ethiopia: a case study in Hawzien district, Tigray. Int J Environ Stud 2013;70(4):629-36. Available at: 10.1080/00207233.2013.835533. [DOI] [Google Scholar]
- [20].Yimam YT, Gelaye KA, Chercos DH. Latrine utilization and associated factors among people living in rural areas of Denbia district, Northwest Ethiopia,. 2013, a cross-sectional study. Pan Afr Med J 2014;18(334):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Oljira D, Berkessa T. Latrine use and determinant factors in Southwest Ethiopia. J Epidemiol Public Heal Rev 2016;1(6):1-5. [Google Scholar]
- [22].WHO and UNICEF. Core questions on drinking-water and sanitation for household surveys. Geneva; 2006. [Google Scholar]
- [23].Yallew WW, Terefe MW, Herchline TE, Sharma HR, Bitew BD, Kifle MW, Tetemke DM, Tefera MA, Adane MM. Assessment of water, sanitation, and hygiene practice and associated factors among people living with HIV/AIDS home based care services in Gondar city, Ethiopia. BMC Public Health 2012;12(1):1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chawicha K, Asnake M, Kassie G, Nigatu T, Belachew M, Zerihun H. The status of hygiene and sanitation practice among rural model families of the Health Extension Program (HEP) in Wolayta and Kembata Tembaro Zones of Southern Nations, Nationalities and peoples’ Region of Ethiopia. Ethiop J Heal Dev 2012;26(2):93-100. [Google Scholar]
- [25].Tulu L, Kumie A, Hawas SB, Demissie HF, Segni MT. Latrine utilization and associated factors among kebeles implementing and non implementing urban community led total sanitation and hygiene in Hawassa town, Ethiopia. African J Environ Sci Technol 2017;11(3):151-62. [Google Scholar]
- [26].Gedefaw M, Amsalu Y, Tarekegn M, Awoke W. Opportunities, and challenges of latrine utilization among rural communities of Awabel district, Northwest Ethiopia, 2014. Open J Epidemiol 2015;5:98-106. [Google Scholar]
- [27].Crocker J, Saywell D, Bartram J. Sustainability of community-led total sanitation outcomes: evidence from Ethiopia and Ghana. Int J Hyg Environ Health 2017;220(3):551-7. Available at: 10.1016/j.ijheh.2017.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


