Summary
Background
We assessed knowledge, attitudes and practices regarding pesticide handling and related health problems among pesticide applicators (PAs) from the Autonomous Province of Trento, Italy.
Methods
A cross-sectional questionnaire-based study was performed in spring 2016, involving 260 PAs. Logistic regression analyses were used to identify factors associated with a safer use of pesticides.
Results
The mean age of participants was 48.8 ± 13.2 years. 89.2% were males. Use of personal protective equipment (PPE) was diffuse, particularly gloves (92.7%), face mask (91.2%), and post-spraying personal hygiene practices were extensively applied. Overall, 43.5% had experienced pesticide-related symptoms especially in subjects misusing PPE, but also for avoiding hygienic procedures. Knowledge about pesticides was a significant predictor for frequency of symptoms.
Conclusions
As a better knowledge of pesticide-related risks was a significant predictor to reduce symptoms, our results stress that improving awareness and promoting safe use of pesticide may improve the health of PAs.
Keywords: Pesticides, Agricultural worker, Knowledge attitudes and practices (KAP), Personal hygiene and sanitation, Personal protective equipment (PPE)
Introduction
Pesticides are known human and environmental toxicants, and are widely used throughout the world in order to assure crop protection against pests and guarantee high crop yields [1-4]. Even though several products have been banned due to their acute and chronic effects [5], pesticide applicators (PAs) are often not aware that also modern pesticides retain a significant toxicological profile, with a consequent global health burden [6-9]. Even though two-thirds of the 350,000 annual pesticide-related deaths occur in developing countries, figures remain of significant relevance also for high income countries [10, 11]. In Italy, for example, a total of around 2,500 occupational cases of acute pesticide intoxications were identified between 2005 and 2011, representing 5% of all poisonings [12].
Unsafe occupational exposure to these “poisons by design” has been associated with the lack of product knowledge and safety awareness among handlers [3, 13-16]. More specifically, available studies suggest that inappropriate practices and attitudes (i.e. use of banned substances, overspraying, lack of self-protection, incorrect storage, mishandling of pesticide containers, reuse of washed pesticide tanks as containers for food and drinking water) [2, 17-22], would be associated with significant knowledge and information gaps [1, 11, 13, 16, 23].
Even though educative interventions have been acknowledged as an appropriate approach for reducing occupational exposures in farmers [2-4, 24], a growing evidence suggests that applicants’ behaviour may be quite more complex. First at all, subjects who are aware of the risks may still misuse pesticides to avoid a lower crop production [25], or may find the use of protective devices very uncomfortable (especially respirators, facemasks and overalls) because of the climate factors, such as high humidity and temperature [26]. Moreover, education may be not enough to bring about behaviour changes, being overwhelmed by personal experiences on pesticide side effects, social and shared interactions, in particular with retailers and resellers [11]. Finally, contextual and structural factors such as availability of appropriate materials and facilities (e.g. soap, water, gloves, showering facilities etc.), employers’ and workers’ commitment to occupational health and safety, likely influence the application of recommended protective behaviours [2-4, 11, 24, 25, 27].
Unfortunately, the majority of available researches regarding knowledge (i.e. the awareness of official recommendations regarding pesticide handling), attitudes (i.e. propensity towards preventive measures) and practices (i.e. actual prevalence of appropriate handling practices), or KAP, of pesticide applicators (PAs) has been performed in workers from highly or relatively deprived socioeconomic environments [1, 4, 11, 13, 20, 23, 28-30]. In order to assess how inappropriate KAP do affect modern PAs from highly developed, and profitable farm settings, the present study was therefore carried out having the following objectives:
assessment of the knowledge of farmers regarding the use of pesticides, their effects, their route of entry into the body;
investigation of the determinants and predictors of poor/good knowledge;
evaluation of the practices for the storage, preparation and disposal of pesticides;
evaluation of field practices with pesticides in relation to the farmers’ knowledge including use of personal protective equipment (PPE);
determination of the prevalence of self-reported health symptoms associated with pesticide exposure and their relation to work practices.
Materials and methods
SUBJECTS AND SETTINGS
The present questionnaire-based cross sectional study included PAs from the Autonomous Province of Trento (APT). APT (537,416 inhabitants at 2015 census) is located in Italy’s North East, covering a total area of 6,214 km2. Its territory is overwhelmingly mountainous (70% over 1,000 m above sea level), and agricultural area only accounts for 22% of the total surface, but highly profitable cultivations (i.e. apples, vineyard) have significantly sustained the regional economic development. According to labour force statistics, the agricultural sector in APT directly accounts for around 20,000 employees (dependent and self-employed) in 11,958 agricultural enterprises, usually of small extent (89% are smaller than 5 hectares and 56% smaller than 1 hectare). These figures however do not include part-time employees, whose number may largely exceed full-time employees [31].
Despite local policies have extensively promoted the biological control of pests, between 2001 and 2012, a mean of 9.1 ± 0.6 kg/ha of pesticides has been used in the APT, significantly greater than in the rest of the country (6.1 ± 0.7 kg/ha). Among the pesticides more extensively used are in particular fungicides (1,893 T; 37.1 kg/ha), followed by insecticides (338 T; 10.6 kg/ha) and herbicides (111 T; 1.8 kg/ha) [32].
STUDY PARTICIPANTS
Sampling was performed by convenience. In APT, PAs must obtain professional certification in order to buy, sell, manage pesticides, irrespective of the volumes of the chemicals effectively used, or the frequency of their handling. Individuals participating to certification courses held between March and December 2016 were invited to participate (n = 366). Participants giving their preliminary consents shortly before the beginning of the courses received by hand a structured questionnaire that inquired their KAP regarding the use of pesticides. In order to avoid that the content of courses may influence participants regarding their answers, delivery and gathering of questionnaires was performed before the beginning of the courses.
INSTRUMENTS
A questionnaire based on the WHO field survey of Exposure to Pesticides Standard Protocol and similar studies [4, 28, 29, 33] was prepared and preliminary tested in 30 farm workers, who did not participate in the final study and completed the questionnaire at two different points in time in order to test-retest reliability of questionnaire items. A correlation coefficient was calculated to compare the two sets of responses: items having a coefficient > 0.80 were interpreted as consistent and, therefore, were included in the questionnaire used in this survey. All questions were self-reported and not externally validated and included the following items:
Basic information about the interviewee, such as gender, age, educational level, and farming practices (crop types and yields, agrochemical products used etc.).
The practice of pesticide application, including attitudes regarding the use of pesticides and PPE or clothes during preparation and application of pesticides; practice questions included: the wearing of PPE; following label instructions; smoking, eating, drinking water or chewing gum during application of pesticides; whether to have a water bath or not after application; and whether they complied with the safety period and concentration recommended.
The level of awareness of the dangers of the pesticides, including knowledge of the acute and chronic toxicity of pesticides, effects of pesticides on human health, the route of pesticide entry into the human body. The responses were documented as “yes”, “no” or “don’t know”. A cumulative knowledge score (KS) was calculated by awarding a score of “+ 1” for each “correct” response, whereas for “wrong” answer and for “don’t’ know” a score of “0” was given.
Health impact of exposure to pesticides as self-reported symptoms associated with pesticide use; participants were asked to rate through a 5-point Likert scale (i.e. never, almost never, occasionally/sometimes, almost every time, every time) the frequency of 11 symptoms usually associated with pesticide use (i.e. headache; eyes itching; vision disturbances; shortness of breath; dizziness; nausea, vomiting, diarrhoea; salivation; skin rash/redness of skin; abdominal pain; disturbances of memory; tremor at rest); a cumulative symptom score (SyS) was then calculated by awarding a score of “+ 1” for a symptom frequency rated as “never”, “+ 2” for “almost never”, and so on.
ETHICS
Before they received the questionnaires, inquired subjects were informed that participation to the present survey was voluntary, and that the questionnaires would be gathered only in subjects expressing preliminary consent for study participation. Participants were guaranteed that they may withdraw from the survey in any time, by simply not delivering the questionnaire at the end of the course session, and that all collected information would be handled anonymously and confidentially. As the questionnaire was strictly anonymous, it is implausible that individual participants could be identified based on the presented material, and ultimately this study caused no plausible harm or stigma to participating individuals. Moreover, as the final examiners of professional courses were totally blind regarding the status of inquired subjects (i.e. whether they had participated or not to the survey), it is also improbable that individual participants have felt forced to give their consent. As the study design assured an adequate protection of study participants, and neither include clinical data about patients nor configure itself as a clinical trial, competent Ethical Committee of the Provincial Agency for Health Services reputed a preliminary evaluation as not required.
DATA ANALYSIS
Two independent researchers, one of whom read the responses from each questionnaire while the other researcher reviewed the entered data, ensured the accuracy of data entry. The primary investigator examined unclear responses to determine the correct answer. Questionnaire lacking basic information about the interviewee were excluded from the study. Continuous variables were tested for normal distribution (D’Agostino & Pearson omnibus normality test): where the corresponding p value was < 0.10, normality distribution was assumed as rejected and variables were compared through Mann-Whitney or Kruskal-Wallis test for multiple independent samples. On the other hand, variables passing the normality check (D’Agostino & Pearson p value ≥ 0.10) were compared using the Student’s t test or ANOVA, where appropriate.
Association of discrete variables with the presence of symptoms was initially assessed through chi-squared test. All variables whose association with self-symptoms was significant at univariate analysis, were then assessed by stepwise binary logistic regression analysis as adjusted OR with the respective 95% CI.
A linear regression analysis was also modelled in order to assess the relative influence of the KS, on the dependent variable SyS. The model included personal attitudes (i.e. information sources, reading of pesticide labels/instructions), and assessed practices (i.e. appropriate storage and disposal, appropriate use of PPE and personal hygiene practice) as covariates.
All regression analyses were controlled for age, sex and ethnicity (i.e. Italian born vs non-Italian born people) and performed on SPSS 24 (IBM Corp. Armonk, NY). Significance level was p < 0.05 for all calculations.
Results
SOCIO-DEMOGRAPHICS CHARACTERISTICS OF THE FARMERS PARTICIPATING TO THE STUDY (TAB. I)
Tab. I.
Demographics of 260 pesticide applicators from the Autonomous Province of Trento participating to the study (2016).
| Category | Variables | N | % |
|---|---|---|---|
| Gender | Male Female |
232 28 |
89.2 10.8 |
| Origin | Italian born people Foreign born people |
243 17 |
93.5 6.5 |
| Smoking status | Current smoker No smoker |
71 189 |
27.3 72.7 |
| Age | ≤ 30 30-39 40-49 ≥ 50 |
28 33 63 136 |
10.8 12.7 24.2 52.3 |
| Occupational status | Farmer (owner) Hobby farmer Farmer (employee) |
137 93 30 |
52.7 35.8 11.5 |
| Education level | University or more High school or greater Primary/Secondary school |
31 147 82 |
11.9 56.5 31.5 |
| Type of crop grown | Fruits or Vegetables Flowers Mixed |
202 25 33 |
77.7 9.6 12.7 |
| Type of agricultural fields | Open fields Closed fields Both open and closed fields |
224 11 25 |
86.2 4.2 9.6 |
A total of 260 questionnaires were ultimately retrieved (Fig. 1), with a response rate of 71.0%, including 243 Italians (93.5%) and 17 subjects from a migration background (6.5%). The mean age of the participants was 48.8 ± 13.2 years, with PAs older than 50 years representing the 52.3% of the sample, that included 232 males (mean age 49.2 years ± 13.3) and 28 females (mean age 45.8 years ± 12.5, p = 0.195). Overall, 71 subjects (27.3%) were either current or past smokers. All the participants had completed at least the primary education (5 + 3 years), and 68.4% of them had achieved secondary education level (13 years) or higher. Majority of respondents performed pesticide handling as professional farmers (64.2%), either self-employed (52.7%) or salaried farm workers (11.5%), whereas 35.8% of participants self-styled as “hobby farmers”. Main crops were fruits or vegetables (75.0%), followed by flowers (25 subjects, 9.6%), and mixed cultures (12.7%).
Fig. 1.
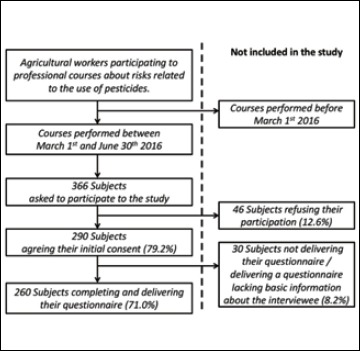
Flow-chart explaining the selection of the study sample.
ATTITUDES, PRACTICES AND BEHAVIOURS (TAB. II)
Tab. II.
Attitudes, practices and personal behaviours related to the use of pesticides in 260 pesticide applicators from the Autonomous Province of Trento (2016).
| Variables | N | % | |
|---|---|---|---|
| Professional courses attended about the safe use of pesticides | None in the last 5 years At least one in last 5 years |
213 47 |
81.9 18.1 |
| Days, per month, working with pesticides | 1-2 days 3-10 days 11 days or more |
92 132 36 |
35.4 50.8 13.8 |
| Years of pesticide use | 1-5 years 6-10 years 11-20 years > 20 years |
66 47 49 98 |
25.4 18.1 18.8 37.7 |
| Main information sources about pesticides | Resellers Personal experience Professional courses Conventional media New media Friends/Relatives Health professional |
88 60 46 22 19 16 9 |
33.8 23.1 17.6 8.5 7.3 6.2 3.5 |
| Pesticide label or instructions | Reading, regularly Not reading |
241 19 |
92.7 7.3 |
| Storage1 | Home Specific store nearby home Animal house Farm site |
26 112 7 124 |
10.0 43.1 2.7 47.7 |
| Disposal of leftover pesticides1 | Specific disposal Storing for reuse Burying Pour in the field |
213 49 - 24 |
81.9 18.8 - 9.2 |
| Disposal of empty containers1 | Specific disposal Washing and reusing Burying Leave in the field I prefer not explain it |
243 13 - 3 1 |
93.5 5.0 - 1.2 0.4 |
| Self-referred use of Personal Protective Equipments, and personal practices performed during spray1 | Face mask Gloves Eye mask Specific shoes Specific clothes Impermeable clothes Long sleeve clothes Hat / Hood Consume food and/or water Drink alcohol Smoking Chewing gum |
237 241 180 195 198 169 219 210 18 10 20 10 |
91.2 92.7 69.2 75.0 76.2 65.0 84.2 80.8 6.9 3.8 7.7 3.8 |
| Self-referred personal practices of the participants after spray1 | Replace/clean face mask and/or filters Replace/clean gloves Wait at least 24 h to re-enter Change clothes Clean/wash clothes Wash hands Take a shower/bath Consume food and/or water Drink alcohol Smoking Chewing gum |
204 199 258 219 210 246 224 199 243 212 232 |
78.5 76.5 99.2 84.2 80.8 94.6 86.2 76.5 93.5 81.5 89.2 |
1: as multiple answers were allowed, total sum may exceed 100%.
Professional handling of pesticides for at least 5 years was reported by 74.6% of participants, with around a third (n = 98, 37.7%) for over 20 years, and the majority of the respondents reported to handle pesticides at least 3 times per month during the crop season (63.5%). Pesticide labels and instructions were regularly read by 92.7% of participants, whereas 5.0% of them omitted their assessment because the information was “too complicated”. More specifically, the most frequently referred information source was represented by pesticide resellers (33.8%), followed by personal experience (23.1%) and professional courses (17.7%), while the least reported was represented by health professionals such as occupational physician (3.5%). In addition, 47 PAs (18.1%) claimed that they had participated in at least one professional course (not including the present one) in the previous 5 years.
The majority of participants (90.8%) claimed that there was a special site for pesticide storage, either nearby home or in the farm, and only 26 individuals (10.0%) reported storing these products inside their house. The empty pesticide containers were returned to the specific disposal program by 93.5% of respondents, whereas 13 (5.0%) washed and reused the containers. Similarly, majority of participants disposed leftover pesticides through specific programs (81.9%), 18.8% stored them for reuse and 9.2% simply poured them on the fields. No one reported to have buried or burned the containers or leftover pesticides, but 1 participant (0.4%) declared that he preferred to not share information about the management of containers.
Focusing on the use of PPE during the disposal of pesticides, the majority of participants regularly wore specific gloves (92.7%), a face mask (91.2%), long sleeve clothes (84.3%), and a hat or a hood (80.8%). Similarly, a high share of respondents mentioned not drinking and/or eating (96.9%), not smoking (92.3%), and not chewing gum (96.2%). After pesticide handling, the majority of respondents reported to regularly wash the hands (94.6%), taking a shower or a water bath (86.2%), managing the face mask or the filters (88.5%), changing (84.2%) or cleaning/washing the clothes (80.8%), and replacing/cleaning the gloves (76.5%). Eventually, 76.5% of PAs reported that they did not consume food and/or drink water after the pesticide dispersal, whereas 18.5% referred to regularly smoke and 10.8% chewed gum.
KNOWLEDGE OF FARMERS ABOUT HEALTH EFFECTS OF PESTICIDES
The potential range of KS was 0-33, and we assessed a mean of 23.4 ± 5.7 (actual range: 11 to 33). Focusing on the single statements (Tab. III), the majority of the participants were aware that pesticide may have health effects for applicators (85.0%) and nearby residents (76.5%), that their use may cause potentially lethal intoxications (90.0%) and long term effects (71.2%), and that pesticides may similarly affect surface waters (99.2%), pollinating insects (96.9%) and livestock (96.2%), ultimately involving the soil fertility (78.1%). Moreover, farmers had considerable high knowledge that pesticides may accumulate in groundwater and surface waters (96.5%), in the soil (92.3%), and eventually in fruits/vegetables (91.9%). All participants acknowledged the skin as a main route of entry of pesticides in the human body, whereas 99.6% and 93.8% claimed nose and mouth as a possible route of entry, respectively. Actually, majority of the farmers were aware that pesticides should be handled by using PPE only (93.8%), but almost a third of the sample (27.3%) believed that the human body may ultimately develop some form of resistance against the used pesticides.
Tab. III.
Knowledge of 260 pesticide applicators from the Autonomous Province of Trento about health effects of pesticides, including symptoms potentially related to pesticide use.
| Correct | Incorrect | Don’t know | |
|---|---|---|---|
| Knowledge regarding pesticide use | |||
| Pesticides are deprived of health effects for applicators | 221 (85.0%) | 24 (9.2%) | 15 (5.8%) |
| Pesticides enter into the body through the skin | 260 (100.0%) | - | - |
| Pesticides enter into the body through the mouth | 244 (93.8%) | 9 (3.5%) | 7 (2.7%) |
| Pesticides enter into the body through the nose | 259 (99.6%) | 1 (0.4%) | - |
| Pesticides affect livestock | 250 (96.2%) | 1 (0.4%) | 9 (3.5%) |
| Pesticides affect pollinating insects (e.g. bees) | 252 (96.9%) | 5 (1.9%) | 3 (1.2%) |
| Pesticides affect surface water | 258 (99.2%) | - | 2 (0.8%) |
| Pesticides affect soil fertility | 203 (78.1%) | 36 (13.8%) | 21 (8.1%) |
| Pesticides induce only short-term effects | 185 (71.2%) | 68 (26.2%) | 7 (2.7%) |
| Pesticides accumulate in the soil | 240 (92.3%) | 11 (4.2%) | 9 (3.5%) |
| Pesticides affect only applicators, not nearby residents | 199 (76.5%) | 55 (21.2%) | 6 (2.3%) |
| Pesticides accumulate in groundwater and surface waters | 251 (96.5%) | 9 (3.5%) | - |
| Pesticides accumulate in fruits and vegetables | 239 (91.9%) | 14 (5.4%) | 7 (2.7%) |
| Some pesticides have been banned | 226 (86.9%) | 18 (6.9%) | 16 (6.2%) |
| Some pesticides may cause potentially lethal intoxications | 234 (90.0%) | 12 (4.6%) | 14 (5.4%) |
| Human body develop resistance against pesticides | 126 (48.5%) | 71 (27.3%) | 63 (24.2%) |
| Pesticides should be handled only using PPE | 244 (93.8%) | 13 (5.0%) | 3 (1.2%) |
| Pesticides affects only children and elders | 247 (95.0%) | 6 (2.3%) | 7 (2.7%) |
| Health effects associated with pesticide use | |||
| Headache | 167 (64.2%) | 54 (20.8%) | 39 (15.0%) |
| Eyes itching | 209 (80.4%) | 32 (12.3%) | 19 (7.3%) |
| Vision disturbance | 191 (73.5%) | 40 (15.4%) | 29 (11.2%) |
| Shortness of breath | 185 (71.2%) | 45 (17.3%) | 30 (11.5%) |
| Dizziness | 107 (41.2%) | 73 (28.1%) | 80 (30.8%) |
| Nausea, vomiting, diarrhoea | 176 (67.7%) | 53 (20.4%) | 31 (11.9%) |
| Salivation | 105 (40.4%) | 64 (24.6%) | 91 (35.0%) |
| Skin rash/redness of skin | 192 (73.8%) | 43 (16.5%) | 25 (9.6%) |
| Abdominal pain | 83 (31.9%) | 82 (31.5%) | 95 (36.5%) |
| Forgetfulness | 41 (15.8%) | 115 (44.2%) | 104 (40.0%) |
| Congenital malformations | 72 (27.7%) | 85 (32.7%) | 103 (39.6%) |
| Fever/shivering | 80 (30.8%) | 77 (29.6%) | 103 (39.6%) |
| Neoplasia | 152 (58.5%) | 50 (19.2%) | 58 (22.3%) |
| Stillbirth/abortion | 77 (29.6%) | 65 (25.0%) | 118 (45.4%) |
| Neurological disorders (e.g. Parkinson’s, Alzheimer’s disease) | 98 (37.7%) | 61 (23.5%) | 101 (38.8%) |
The best known consequences of pesticide exposure were itching eyes (80.4%), followed by skin rash or redness of the skin (73.8%), visual disturbances (73.5%), shortness of the breath (71.2%), nauseas, vomiting, and diarrhoea (67.7%). Around 60% of the participants identified neoplasia as a pesticide-related health effect (58.5%), and nearly 40% of the farmers identified the risk for neurological disorders such as Parkinson’s or Alzheimer’s disease (37.7%). Finally, the least known health effects were stillbirth / abortion (29.6%), congenital malformations (27.7%) and forgetfulness (15.8%).
KS significantly increased with education level (p < 0.001), and graduated PAs had mean scores (26.3 ± 4.6) significantly higher than subjects referring high school (24.1 ± 5.5) and primary/secondary school (21.1 ± 5.7) degree. KS conversely decreased with the years of pesticide use, being higher in subject referring 1 to 5 years of experience (25.9 ± 4.6), and lower in participants handling pesticides for 20 or more years (22.3 ± 5.9, p = 0.001) (Tab. IV).
Tab. IV.
Knowledge score by demographic factors and main attitude towards the use of pesticides in 260 pesticide applicators from the Autonomous Province of Trento.
| Category | Variables | Knowledge score | P value |
|---|---|---|---|
| Gender | Male Female |
23.4 ± 5.7 23.5 ± 5.8 |
0.911 |
| Origin | Italian born people Foreign born people |
23.5 ± 5.7 22.4 ± 6.3 |
0.466 |
| Smoking status | Current smoker No smoker |
22.7 ± 4.6 23.6 ± 6.1 |
0.189 |
| Age | ≤ 30 30-39 40-49 ≥ 50 |
24.1 ± 5.1 24.6 ± 6.0 23.0 ± 5.9 23.2 ± 5.7 |
0.512 |
| Occupational status | Farmer (owner) Hobby farmer Farmer (employee) |
23.8 ± 6.0 22.8 ± 5.3 23.8 ± 5.6 |
0.424 |
| Education level | University or more High school or greater Primary/Secondary school |
26.3 ± 4.6 24.1 ± 5.5 21.1 ± 5.7 |
< 0.001 |
| Type of crop grown | Fruits or Vegetables Flowers Mixed |
23.6 ± 6.0 26.5 ± 4.0 22.7 ± 5.7 |
0.001 |
| Type of agricultural fields | Open fields Closed fields Both open e closed fields |
23.4 ± 5.7 21.4 ± 4.7 24.2 ± 6.0 |
0.391 |
| Professional courses | None in the last 5 years At least one in last 5 years |
21.7 ± 5.6 23.7 ± 5.7 |
0.030 |
| Days, per month, working with pesticides | 1-2 days 3-10 days 11 days or more |
21.1 ± 6.4 23.6 ± 5.2 23.3 ± 5.9 |
0.823 |
| Years of pesticide use | 1-5 years 6-10 years 11-20 years > 20 years |
25.9 ± 4.6 24.1 ± 5.7 22.3 ± 5.9 22.1 ± 5.7 |
0.001 |
| Main information sources about pesticides | Resellers Personal experience Professional courses Conventional media New media Friends/Relatives Health professional |
22.4 ± 5.5 23.7 ± 5.8 25.6 ± 4.4 23.5 ± 5.4 22.5 ± 8.1 20.1 ± 4.7 26.9 ± 1.6 |
0.004 |
A better KS was then identified in subjects who had attended at least one professional course in the previous 5 years (23.7 ± 5.7 vs 21.7 ± 5.6, p = 0.030) and growing flowers (23.6 ± 6.0) rather than fruits or vegetables (23.6 ± 6.0) or even mixed cultures (22.7 ± 5.7, p = 0.001). Focusing on information sources, a better score was identified in subjects relying on health professionals (26.9 ± 1.6) and professional courses (25.6 ± 4.4), whereas PAs referring new media (22.5 ± 8.1), resellers (22.5 ± 5.5), and in particular friends/relatives (20.1 ± 4.7) had the lowest ones.
SELF-REPORTED TOXICITY SYMPTOMS AND THEIR ASSOCIATION WITH PERSONAL CHARACTERISTICS/BEHAVIOUR
A total of 113 participants (43.5%) self-reported every time or almost every time they handled pesticides at least one of the listed symptoms, with a mean SyS of 15.0 ± 6.3 (potential range of 11 to 55; actual range 11 to 52). As shown in Figure 2, itching of the eyes (72, 27.7%), vision disturbances (63, 24.2%), headache (53, 20.4%) were the most common ones, and forgetfulness (12, 4.6%), abdominal pain, resting tremor (both symptoms: 11, 4.2%) and dizziness (10, 3.8%) the least common.
Fig. 2.

Self-reported symptoms complained “every time” or “almost every time” by 260 pesticide applicators from the Autonomous Province of Trento after pesticide handling.
Prevalence of toxicity symptoms was not significantly affected by main demographic variables, including sex, age, education level and occupational status (Tab. V). Focusing on work-related practices, only workers having a pesticide use history of 20 years or more referred a significantly increased prevalence of symptoms, whereas frequency of pesticide application was unrelated with the prevalence of symptoms.
Tab. V.
Prevalence of the self-reporting of one or more symptoms related with pesticide exposure among 260 farmers, broken down by demographics and attitude and pesticide-related behaviors. Odds ratios (OR) with their respective 95% confidence intervals were obtained through bivariate analysis.
| Variables | Self-referred symptoms (any) | P value | OR (95%CI) | |
|---|---|---|---|---|
| Gender | Male Female |
99 (42.7%) 14 (50.0%) |
0.591 | - |
| Origin | Italians Migration background |
106 (43.6%) 7 (41.2%) |
0.844 | - |
| Smoking status | Previous/Current smoker Never smoker |
32 (45.1%) 81 (42.9%) |
0.784 | - |
| Age (years) | ≤ 30 30-39 40-49 ≥ 50 |
9 (32.1%) 10 (30.3%) 33 (52.4%) 61 (44.9%) |
0.115 | - |
| Occupational status | Farmer (owner) Hobby farmer Farmer (employee) |
64 (46.7%) 36 (38.7%) 13 (43.3%) |
0.486 | - |
| Education level | University or higher High school or higher Primary/Secondary school |
12 (38.7%) 70 (47.6%) 31 (37.8%) |
0.303 | - |
| Type of crop grown | Fruits or Vegetables Flowers Mixed |
80 (39.6%) 13 (52.0%) 20 (60.6%) |
0.052 | - |
| Professional courses | None in the last 5 years At least one in last 5 years |
98 (46.0%) 15 (31.9%) |
0.077 | - |
| Days, per month, working with pesticides | 1-2 3-10 11 or more |
37 (40.2%) 66 (50.0%) 10 (30.3%) |
0.083 | - |
| Years of pesticide use | 1-5 6-10 11-20 > 20 |
18 (27.3%) 19 (40.4%) 20 (40.8%) 56 (57.1%) |
0.002 | REF 1.810 (0.817-4.009) 1.839 (0.838-4.037) 3.556 (1.813-6.972) |
| Main information sources about pesticides | Resellers Personal experience Professional courses Conventional media New media Friends/Relatives Health professional |
40 (45.5%) 34 (56.7%) 18 (39.1%) 4 (18.2%) 7 (36.8%) 5 (31.3%) 5 (55.6%) |
0.055 | - |
| Pesticide label or instructions | Reading, regularly Not reading |
104 (43.2%) 9 (47.4%) |
0.721 | - |
| Storage site of pesticides | Home Specific store nearby home Animal house Farm site |
13 (50.0%) 46 (51.1%) 4 (57.1%) 56 (45.2%) |
0.724 | - |
| Disposal of leftover pesticides | Specific disposal Storing for reuse Pour in the field |
91 (42.7%) 22 (44.9%) 15 (62.5%) |
0.182 | - |
| Disposal of empty containers | Specific disposal Washing and reusing Leave in the field |
106 (43.6%) 6 (46.2%) 3 (100.0%) |
0.147 | - |
A greater prevalence of toxicity symptoms was referred by subjects not wearing a face mask, specific clothes, gloves, impermeable shoes, and eye mask during pesticide dispersal. Similarly, farmers not washing their hands, not replacing working clothes and gloves, as well as drinking alcohol, chewing gum, and smoking after the spray had a significant association with self-referral of symptoms (Tab. VI).
Tab. VI.
Selected practices during and after spraying of 260 pesticide applicators from the Autonomous Province of Trento (2016), and their correlation with the presence/absence of symptoms. Adjusted Odds Ratio (OR) were calculated through regression analysis.
| Practices | Use | Symptoms | P value | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Yes (113, 43.5%) |
No (147, 56.5%) |
(LL-UL) | ||||
| At spraying | ||||||
| Wear: face mask | No Yes |
18, 15.9% 95, 84.1% |
5, 3.4% 142, 96.6% |
0.026 | 7.849 | 2.610-23.6 |
| Wear: gloves | No Yes |
13, 11.5% 100, 88.5% |
6, 4.1% 141, 95.9% |
0.017 | 5.972 | 1.979-18.0 |
| Wear: eye mask | No Yes |
45, 39.8% 68, 60.2% |
35, 23.8% 112, 76.2% |
0.033 | 2.965 | 1.616-5.443 |
| Wear: specific shoes | No Yes |
42, 37.2% 71, 62.8% |
23, 15.6% 124, 84.4% |
0.010 | 3.822 | 1.988-7.349 |
| Wear: specific clothes | No Yes |
26, 23.0% 87, 77.0% |
36, 24.5% 111, 75.5% |
0.541 | - | - |
| Wear: impermeable clothes | No Yes |
51, 45.1% 62, 54.9% |
40, 27.2% 107, 72.8% |
0.005 | 2.284 | 1.285-4.060 |
| Wear: long sleeve clothes | No Yes |
20, 17.7% 93, 82.3% |
21, 14.3% 126, 85.7% |
0.170 | - | - |
| Wear: hat/hood | No Yes |
19, 16.8% 94, 83.2% |
31, 21.1% 116, 78.9% |
0.738 | - | - |
| Consume food and/or water | Yes No |
8, 7.1% 105, 92.9% |
10, 6.8% 137, 93.2% |
0.354 | - | - |
| Drink alcohol | Yes No |
5, 4.4% 108, 95.6% |
5, 3.4% 142, 96.6% |
0.002 | - | - |
| Smoking | Yes No |
10, 8.8% 103, 91.2% |
10, 6.8% 137, 93.2% |
0.250 | - | - |
| Chewing gum | Yes No |
5, 4.4% 108, 95.6% |
5, 3.4% 142, 96.6% |
0.006 | - | - |
| After spraying | ||||||
| Replace/clean face mask and/or filters | No Yes |
36, 31.9% 77, 68.1% |
20, 13.6% 127, 86.4% |
0.040 | 3.504 | 1.781-6.893 |
| Replace/clean gloves | No Yes |
34, 30.1% 79, 69.9% |
27, 18.4% 120, 81.6% |
0.006 | 2.057 | 1.100-3.845 |
| Wait at least 24 h to re-enter | No Yes |
2, 1.8% 111, 98.2% |
0 147, 100% |
0.042 | - | - |
| Change clothes | No Yes |
28, 24.8% 85, 75.2% |
13, 8.8% 134, 91.2% |
0.003 | 4.629 | 2.022-10.6 |
| Clean/wash clothes | No Yes |
24, 21.2% 89, 78.8% |
26, 17.7% 121, 82.3% |
0.008 | - | - |
| Wash hands | No Yes |
13, 11.5% 100, 88.5% |
1, 0.7% 146, 99.3% |
0.001 | 36.343 | 4.206-313.0 |
| Take a shower/bath | No Yes |
17, 15.0% 96, 85.0% |
19, 12.9% 128, 87.1% |
0.030 | - | - |
| Consume food and/or water | Yes No |
27, 23.9% 86, 76.1% |
34, 23.1% 113, 76.9% |
0.135 | - | - |
| Drink alcohol | Yes No |
15, 13.3% 98, 86.7% |
2, 1.4% 145, 98.6% |
0.001 | 20.718 | 4.154-103.4 |
| Smoking | Yes No |
27, 23.9% 86, 76.1% |
21, 14.3% 126, 85.7% |
< 0.001 | 2.358 | 1.186-4.688 |
| Chewing gum | Yes No |
21, 18.6% 92, 81.4% |
7, 4.8% 140, 95.2% |
0.005 | 7.054 | 2.635-18.9 |
REGRESSION ANALYSIS
In multivariate analysis, after adjustments for sex, age, cultivation type, years of experiences, previous frequency to formation courses, all aforementioned practices and behaviours were confirmed as significantly associated with a positive status for toxicity symptoms. In particular, not washing hands (OR 36.343 95% CI 4.206-313.0), drinking alcohol (OR 20.718 95% CI 4.154-103.4), and chewing gum (OR 7.054 95% CI 2.635-18.884) after spraying, and the inappropriate use of PPE such as face mask (OR 7.849 95% CI 2.610-23.604), gloves (OR 5.972 95% CI 1.979-18.023) and shoes (OR 3.822 95% CI 1.988-7.349) were associated with higher prevalence of self-reported symptoms (Tab VI).
In linear regression analysis, SyS found a statistically significant predictor in KS (B coefficient = – 0.204, 95% CI – 0.325 to – 0.082, p < 0.001), i.e. farmers having a better awareness of the risk related to pesticide handling had a lower frequency of pesticide related symptoms.
Discussion
Agricultural workers and PAs are usually described as affected by an extensive lack of knowledge about the risks associated with pesticide handling [1, 6, 20, 34]. As the majority of the available surveys were performed in developing countries, or included workers from relatively or even highly deprived socioeconomic environments, the consistency of these reports with high-income countries, with a higher ratio of highly profitable cultivations, and where the use of pesticides is strictly regulated, might therefore be disputed [1, 4, 11, 13, 20, 23, 28-30].
Our results suggest that PAs from a high-developed agricultural system may exhibit satisfying knowledge of health and environmental effects of pesticides, and are presumptively related with some specificities of the studied population.
First at all, mean age of participants was relatively higher than that in previous studies, with 52.3% of them aged more than 50 years, but such figures were not unexpected as epidemiological studies clearly indicate that in developed countries agricultural workers (AWs) are significantly older than most other occupational groups [35-37].
Second, a high share of PAs reported a formal education > 13 years [29, 34, 38, 39]: in this regard, it should be stressed that in APT a significant number of farmers perform agricultural activities as a collateral and/or part-time job, eventually reverting to agricultural activities after their retirement [31]. Even though older farmers usually show significant knowledge gaps, and also in our study KS was significantly decreased in higher age groups, education level has been repetitively described as a main determinant for the misuse of pesticides [1, 6]. More specifically, subjects of lower education level apparently perceive lower risks and higher benefits from using pesticides, potentially leading them to incorrect behaviour [1, 6]. In particular, lower education is associated with inappropriate reading of pesticides labels, hazard warnings and provided instructions [20, 34], as they are perceived too technical and not understandable [25].
Third, as a consequence of the convenience sampling we performed, not only all the participants actually handled pesticides, but around 75% of them had managed pesticides for at least 5 years.
Not coincidentally, around 92.5% of the sample referred the regular reading of pesticide labels and instructions, and nearly 80% recalled adequate and reliable sources of information, such as resellers, professional courses, and also health professionals [4]. In effect, even though only 18.1% of the study participants referred to have attended at least a professional course about the safe use of pesticides in the previous 5 years, participants referring health professionals and specific professional courses as main information sources had the better KS of this survey. In this regard, oral communication with retailers was associated with more ambiguous results. On the one hand, it played a dominant role in learning about pesticides and their functions, but the resulting level of knowledge was apparently unsatisfying, ultimately emphasizing the need for specific education and supervision programmes for pesticide resellers [7].
Focusing on the referred practices, proper methods of storing pesticide was diffuse [8, 34, 40, 41], with most of participants referring a specific storage site either nearby home or in the farm site. Moreover, the majority of the participant referred a specific disposal of leftover pesticides and empty containers, as the latter were washed and reused only by 5.0% of the participants. This is of particular interest not only for occupational health and safety, but also in broader terms, as storing pesticides at home or in inappropriate working environment can easily contaminate drinking water and food, ultimately threatening the health of other non-professionally exposed family members, whereas the disposal of the empty containers in the field or by throwing them near or into local waste containers has been reported as a major public health problem in a number of studies [1, 25, 29, 34, 38, 42]. Unsurprisingly, not only storing pesticides at home was associated with a lower KS, but also an appropriate storage and disposal were consistently associated with better scores.
Analysis of personal practices identified a more ambiguous pattern. On the one hand, available evidence suggests a general acknowledgement that the use of appropriate PPE (i.e. long-sleeved shirts, impermeable working clothes, work boots, gloves and a hat/hood) at spraying significantly decreases the probability of poisoning in pesticide handlers [8, 43]. On the other hand, personal hygiene measures such as washing hands, changing clothes, showering, and washing work clothes from household laundry immediately after work have been also described as efficient in order to avoid poisoning after pesticide application [44], but are more inconsistently applied, and frequently neglected [40]. In facts, several studies have found detectable levels of pesticide residues on farm workers’ work boots, clothes etc., suggesting a significant household contamination from inappropriate practices of personal hygiene measures [8, 41]. Not coincidentally, in our survey subjects correctly applying personal hygiene measure, in particular post-spraying, were associated with better KS, whereas it was unrelated with practices involving PPE.
These results may found several explanations [4, 29, 45]. First at all, the correlation between knowledge and practices may be not so straight as previously supposed. Available studies suggests that farmers may actually ignore appropriate preventive measure notwithstanding an appropriate awareness of related risks, not only in developing countries, because of factors other than knowledge of pesticide health effects [4, 25, 28, 38, 46]. For example, unavailability and/or inappropriate handling of PPE may be easily recognized and fined by work inspectors, and therefore the use of some PPE may be perceived by the worker more as a regulatory requirement rather than as a safety measure, ultimately operating the equipment without any understanding of its rationale [23]. Again, as climate scenarios project an increase in global mean temperature and in the frequency and intensity of heat waves over most areas around the world in the near future [47], rigorous usage of PPE becomes ever more difficult, especially in an increasingly older group of workers. Finally, we cannot rule out that the use of PPE may have been perceived by participants as the “socially appropriated” behaviour (i.e. social desirability bias), with our results ultimately overstating their actual use [48].
The prevalence of symptoms potentially related to pesticide intoxication may be interpreted as an outcome of knowledge, attitudes and practices of farmers regarding pesticide handling and personal protective measures, including both the use of PPE and personal hygiene practices [2-4, 11, 13, 20, 21, 23, 25, 28, 29, 45, 49, 50]. In our sample, prevalence of symptoms was relatively high (43.5%), and linear regression analysis identified KS as a significant predictor for their frequency. Consistently with previous reports, higher rates toxicity-related symptoms were also identified in subjects having a lower education level, and referring higher prevalence of inappropriate attitudes and practices. In particular, participants denying the use of face mask (adjOR 7.849, 95% CI 2.610-23.6), gloves (adjOR 5.972, 95% CI 1.979-18.0), eye mask (adjOR 2.965, 95% CI 1.616-5.433), specific shoes and impermeable clothes (adjOR 3.822, 95% CI 1.988-7.349 and 2.284, 95% CI 1.285-4.060, respectively) at spraying, and not replacing or cleaning respiratory tract PPE (adjOR 3.504, 95% CI 1.781-6.893), gloves (adjOR 2.057, 95% CI 1.100-3.845), clothes (adjOR 4.629, 95% CI 2.022-10.6), or simply not washing their hands (adjOR 36.343 95% CI 4.206-313.0) after spraying referred a significantly higher prevalence of complaints. Also the avoiding of simple post-spraying personal hygiene practices such as not smoking (adjOR 2.358, 95% CI 1.186-4.688) and not chewing gum (adjOR 7.054, 95% CI 2.635-18.9) was significantly associated with increased risk for pesticide related symptoms. Despite relatively few participants reported to drink alcohol immediately after spraying, the ratio of complaints was relatively high (15/17 vs 98/145; adjOR 20.718, 95% CI 4.154-103.4), and may be explained as a function of the high consumption of fungicides such as dithiocarbamate in the APT [31, 32].
Dithiocarbamate induced alcohol intolerance is actually well known, and the inhibitory effects on enzymes is only slowly reversible, ultimately increasing the risk for subjects performing repetitive treatments [1-8].
On the contrary, PAs relying on conventional media as main information source referred a significantly lower prevalence of intoxication symptoms, and we may tentatively explain these result as the assessing of an attitude towards the search for updated information rather as the effect of the information by itself, ultimately identifying subjects more proactive regarding the use of appropriate personal protective practices.
Collectively, these outcomes are somehow coherent with more recent studies suggesting a complex correlation between knowledge and practices in pesticide applicators. PAs may be aware that pesticides are harmful, still not applying appropriate measures to avoid and/or reduce exposure [25], not only because of misbeliefs or even false beliefs regarding pathways of exposure and specific health effects, but because of personal interest [2-4, 11, 13, 20, 21, 23, 25, 28, 29, 45, 49, 50].
However, it should be stressed that studies inquiring symptoms in farmers and PAs handling pesticides are limited in number, and their reliability is usually limited by the usual self-assessment of symptoms, frequently identified as a weak indicator for pesticide poisoning for several reasons, and also our study shares these limitations [2-4, 11, 13, 20, 21, 23, 25, 28, 29, 45, 49, 50]. On the one hand, as pesticides are frequently recognised “poisons by design”, participants may potentially overstate their complaints during and after spraying, reporting them in terms of “common-sense” rather than as a consequence of their previous occupational experience [15, 44, 50].
On the other hand, most of pesticide-related symptoms are very common disorders. Headache, eye discomfort, visual disturbances, together with nausea/vomiting, and skin disorders have been frequently reported after pesticide use, and these conditions are not only very common in the general population, but are also potentially correlated with other occupational exposures such as pollens, dusts and UV rays. Our results may therefore overstate their actual prevalence, depending on causes other than pesticide exposure [28, 34, 40, 51].
Several major limitations of the study should be addressed. For instance, we assessed a sample of relatively small size, gathered through convenience sampling and a regional basis. The latter, may represent a main issue, as Italy has been repetitively acknowledged as highly heterogeneous in terms of socioeconomically development, education level, and also agricultural practices are deeply regionalized [52]. APT in particular is associated with developed, high profitable farming, characterized by an extensive use of pesticides in small enterprises, usually managed by the owner himself. Again, it should be remarked that the study population included only subjects having a relatively high qualification, both in term of personal education and in empirical experience with pesticide handling. Moreover, most of them are either “hobby farmers”, or part-time farmers: in other words, the sample we presented may not be representative of the national level [52].
Generalization of our results may be furtherly compromised by the very same retrospective conception of the survey, potentially lacking the sensibility to correctly recall cases related to pesticide toxicity both in terms of frequency and severity [7, 44, 50]. Moreover, we did not assess other professional exposures potentially related with reported symptoms, such as high environmental temperatures, solar radiation, and also chemicals other than pesticides.
In conclusion, PAs from APT exhibited a relatively high awareness about possible adverse effects of pesticides, high levels of adoption of appropriate measures including the use of PPE and personal hygiene practices. Younger age groups and higher education were correlated with lower prevalence and frequency of symptoms, and also participants interacting with health professionals and who took part to professional courses similarly had a better awareness of the risks. The role for pesticide resellers and some information sources, including both conventional and new media, was more controversial. Professional courses, possibly involving health professionals such as occupational physicians, may therefore represent the more appropriate items to raise the awareness of farm workers towards the appropriate use of well-maintained PPE and personal hygiene practices, during and after the handling of pesticides.
Acknowledgements
The authors express their gratitude to all participants.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
None declared.
Authors' contributions
MR, GG and LV equally contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript. However, as primary investigator, MR was asked to assess unclear responses of the questionnaires to determine the correct answers, whereas GG and LV performed the majority of data entry.
References
- [1].Hashemi SM, Hosseini SM, Hashemi MK. Farmers’ perceptions of safe use of pesticides: determinants and training needs. Int Arch Occup Environ Health 2012;85(Suppl. 1):57-66. doi: 10.1007/s00420-011-0641-8. [DOI] [PubMed] [Google Scholar]
- [2].Damalas CA, Eleftherohorinos IG. Pesticide exposure, safety issues, and risk assessment indicators. Int J Environ Res Public Health 2011;8(5):1402-19. doi: 10.3390/ijerph8051402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Damalas CA, Hashemi SM. Pesticide risk perception and use of personal protective equipment among young and old cotton growers in northern Greece. Agrociencia 2010;44(3):363-71. Available at: http://www.scielo.org.mx/pdf/agro/v44n3/v44n3a10.pdf. Accessed on 2017. [Google Scholar]
- [4].Salameh PR, Baldi I, Brochard P, Saleh BA. Pesticides in Lebanon: a knowledge, attitude, and practice study. Environ Res 2004;94(1):1-6. doi: 10.1016/S0013-9351(03)00092-6. [DOI] [PubMed] [Google Scholar]
- [5].Verger PJP, Boobis AR. Global food supply. Reevaluate pesticides for food security and safety. Science 2013;341(6147):717-8. doi: 10.1126/science.1241572. [DOI] [PubMed] [Google Scholar]
- [6].Fan L, Niu H, Yang X, Qin W, Bento CP, Ritsema CJ, Geissen V. Factors affecting farmers’ behaviour in pesticide use: Insights from a field study in northern China. Sci Total Environ 2015;537:3608 doi: 10.1016/j.scitotenv.2015.07.150. [DOI] [PubMed] [Google Scholar]
- [7].Yang X, Wang F, Meng L, Zhang W, Fan L, Geissen V, Ritsema CJ. Farmer and retailer knowledge and awareness of the risks from pesticide use: a case study in the Wei River catchment, China. Sci Tot Environ 2014;497-8:172-9. doi: 10.1016/j.scitotenv.2014.07.118. [DOI] [PubMed] [Google Scholar]
- [8].Strong LL, Thompson B, Koepsell TD, Meischke H. Factors associated with pesticide safety practices in farmworkers. Am J Ind Med 2007;51(1):69-81. doi: 10.1002/ajim.20519. [DOI] [PubMed] [Google Scholar]
- [9].Jeyaratnam J. Acute pesticide poisoning: a major global health problem. World Health Stat Q 1990;43(3):139-44. Available at: http://apps.who.int/iris/bitstream/10665/51746/1/WHSQ_1990_43_n3_p139-144_eng.pdf. Accessed on 16, August 2017. [PubMed] [Google Scholar]
- [10].World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, World Health Organization, 2008. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ Accessed August 16, 2017. [Google Scholar]
- [11].Ríos-González A, Jansen K, Sánchez-Pérez HJ. Pesticide risk perceptions and the differences between farmers and extensionists: towards a knowledge-in-context model. Environ Res 2013;124:43-53. doi: 10.1016/j.envres.2013.03.006. [DOI] [PubMed] [Google Scholar]
- [12].Settimi L, Davanzo F, Urbani E, Giordano F, Cossa L. National informative system for surveillance of toxic exposures and poisonings: cases identified in 2010. 5th annual report. Report No. 14/13. Rome: Italian National Health Institute; 2014. Availableat: http://www.iss.it/binary/publ/cont/14_13_web.pdf Accessed on August 16, 2017. [Google Scholar]
- [13].Hashemi SM, Damalas CA. Farmers’ perceptions of pesticide efficacy: reflections on the importance of pest management practices adoption. J Sust Agricul 2010;35(Suppl. 1):69-85. doi: 10.1080/10440046.2011.530511. [Google Scholar]
- [14].Lekei EE, Ngowi AV, London L. Farmers’ knowledge, practices and injuries associated with pesticide exposure in rural farming villages in Tanzania. BMC Public Health 2014;14:389 doi: 10.1186/1471-2458-14-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lekei EE, Ngowi AV, London L. Pesticide retailers’ knowledge and handling practices in selected towns of Tanzania. Environmental Health 2014;13:79 doi: 10.1186/1476-069X-13-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Khan M, Damalas CA. Farmers’ willingness to pay for less health risks by pesticide use: a case study from the cotton belt of Punjab, Pakistan. Sci Total Environ 2015;530-1:297-303. doi: 10.1016/j.scitotenv.2015.05.110. [DOI] [PubMed] [Google Scholar]
- [17].Van Hoi P, Mol APJ, Oosterveer PJM. Market governance for safe food in developing countries: the case of low-pesticide vegetables in Vietnam. J Environ Manage 2009;91(1):380-8. doi: 10.1016/j.jenvman.2009.09.008. [DOI] [PubMed] [Google Scholar]
- [18].Grovermann C, Schreinemachers P, Berger T. Quantifying pesticide overuse from farmer and societal points of view: An application to Thailand. Crop Prot 2013;53:161-8. doi: 10.1016/j.cropro.2013.07.013. [Google Scholar]
- [19].Stadlinger N, Mmochi AJ, Kumblad L. Weak governmental institutions impair the management of pesticide import and sales in Zanzibar. Ambio 2012;42(1):72-82. doi: 10.1007/s13280-012-0338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ibitayo OO. Egyptian farmers’ attitudes and behaviors regarding agricultural pesticides: implications for pesticide risk communication. Risk Anal 2006;26(4):989-95. doi: 10.1111/j.1539-6924.2006.00794.x. [DOI] [PubMed] [Google Scholar]
- [21].Karunamoorthi K, Mohammed M, Wassie F. Knowledge and practices of farmers with reference to pesticide management: implications on human health. Arch Environ Occup Health 2012;67(2):109-16. doi: 10.1080/19338244.2011.598891. [DOI] [PubMed] [Google Scholar]
- [22].Tijani AA. Pesticide use practices and safety issues: the case of cocoa farmers in Ondo State, Nigeria. J Hum Ecol 2006;19(3):183-90. [Google Scholar]
- [23].Sam KG, Andrade HH, Pradhan L, Pradhan A, Sones SJ, Rao PG, Sudhakar C. Effectiveness of an educational program to promote pesticide safety among pesticide handlers of South India. Int Arch Occup Environ Health 2008;81(6):787-95. doi: 10.1007/s00420-007-0263-3. [DOI] [PubMed] [Google Scholar]
- [24].Chen S, He F, Zhang Z, Gao Y, Zhou A, Xie C, Xiong L, Chen D, Wang S, Jia J. Evaluation of a safety educational programme for the prevention of pesticide poisoning. Med Lav 1998;89(Suppl 2):S91-8. [PubMed] [Google Scholar]
- [25].Damalas CA, Georgiou EB, Theodorou MG. Pesticide use and safety practices among Greek tobacco farmers: a survey. Int J Enrivon Health Res 2006;16(5):339-48. doi: 10.1080/09603120600869190. [DOI] [PubMed] [Google Scholar]
- [26].Gatto MP, Cabella R, Gherardi M. Climate change: the potential impact on occupational exposure to pesticides. Ann Ist Super Sanità 2016;52(3):374-85. doi: 10.4415/ANN_16_03_09. [DOI] [PubMed] [Google Scholar]
- [27].Salvatore AL, Bradman A, Castorina R, Camacho J, López J, Barr DB, Snyder J, Jewell NP, Eskenazi B. Occupational behaviors and farmworkers’ pesticide exposure: findings from a study in Monterey county, California. Am J Ind Med 2008;51(10):782-94. doi: 10.1002/ajim.20622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yassin MM, Abu Mourad TA, Safi JM. Knowledge, attitude, practice, and toxicity symptoms associated with pesticide use among farm workers in the Gaza Strip. Occup Environ Med 2002;59(6):387-94. doi: 10.1136/oem.59.6.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zyoud SH, Sawalha AF, Sweileh WM, Awang R, Al-Khalil SI, Al-Jabi SW, Bsharat NM. Knowledge and practices of pesticide use among farm workers in the West Bank, Palestine: safety implications. Environ Health Prev Med 2010;15(4):252-61. doi: 10.1007/s12199-010-0136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 2002;360(9347):1728-36. doi: 10.1016/S0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- [31].Agnolin C, Ioriatti C, Pontalti M, Venturelli MB. IFP experiences in Trentino, Italy. Acta Hort 2000;525:45-50. doi: 10.17660/ActaHortic.2000.525.3. [Google Scholar]
- [32].Istituto Superiore per la Protezione e la Ricerca Ambientale (ISPRA). National Report on water-borne pesticides, 2013-2014. 2016. Available at: http://www.isprambiente.gov.it/files/pubblicazioni/rapporti/rapporto-244/Rapporto_244_2016.pdf. Accessed on August 16, 2017.
- [33].Mohanty MK, Behera BK, Jena SK, Srikanth S, Mogane C, Samal S, Behera AA. Knowledge attitude and practice of pesticide use among agricultural workers in Puducherry, South India. J Forensic Leg Med 2013;20(8):1028-31. doi: 10.1016/j.jflm.2013.09.030. [DOI] [PubMed] [Google Scholar]
- [34].Recena MCP, Caldas ED, Pires DX, Pontes ERJC. Pesticides exposure in Culturama, Brazil-Knowledge, attitudes, and practices. Environ Res 2006;102(2):230-6. doi: 10.1016/j.envres.2006.01.007- [DOI] [PubMed] [Google Scholar]
- [35].Betsch C, Wicker S. Personal attitudes and misconceptions, not official recommendations guide occupational physicians’ vaccination decisions. Vaccine 2014;32(35):4478-84. doi: 10.1016/j.vaccine.2014.06.046. [DOI] [PubMed] [Google Scholar]
- [36].Riccò M, Cattani S, Veronesi L, Colucci E. Knowledge, attitudes, beliefs and practices of construction workers towards tetanus vaccine in Northern Italy. Ind Health 2016;54(6):554-64. doi: 10.2486/indhealth.2015-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Zingg A, Siegrist M. Measuring people’s knowledge about vaccination: Developing a one-dimensional scale. Vaccine 2012;30(25):3771-7. doi: 10.1016/j.vaccine.2012.03.014. [DOI] [PubMed] [Google Scholar]
- [38].Mekonnen Y, Agonafir T. Pesticide sprayers’ knowledge, attitude and practice of pesticide use on agricultural farms of Ethiopia. Occup Med 2002;52:311-5. doi: 10.1093/occmed/52.6.311. [DOI] [PubMed] [Google Scholar]
- [39].Oliveira Pasiani J, Torres P, Roniery Silva J, Diniz BZ, Dutra Caldas E. Knowledge, attitudes, practices and biomonitoring of farmers and residents exposed to pesticides in Brazil. Int J Environ Res Public Health 2012;9(9):3051-68. doi: 10.3390/ijerph9093051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ngowi AV, Mbise TJ, Ijani ASM, London L, Ajayi OC. Pesticides use by smallholder farmers in vegetable production in Northern Tanzania. Crop Prot 2007;26(11):1617-24. doi: 10.1016/j.cropro.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Rao P, Gentry AL, Quandt SA, Davis SW, Snively BM, Arcury TA. Pesticide safety behaviors in Latino farmworker family households. Am J Ind Med 2006;49(4):271-80. doi: 10.1002/ajim.20277. [DOI] [PubMed] [Google Scholar]
- [42].Avory G, Coggon D. Determinants of safe behaviour in farmers when working with pesticides. Occup Med 1995;44(5):236-8. doi: 10.1093/occmed/44.5.236. [DOI] [PubMed] [Google Scholar]
- [43].Quandt SA, Hernández-Valero MA, Grzywacz JG, Hovey JD, Gonzales M, Arcury TA. Workplace, Household, and Personal Predictors of Pesticide Exposure for Farmworkers. Environ Health Perspect 2006;114(6):943-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Dasgupta S, Meisner C, Wheeler D, Xuyen K, Lam NT. Pesticide poisoning of farm workers-implications of blood test results from Vietnam. Int J Hyg Environ Health 2007;210(2):121-32. doi: 10.1016/j.ijheh.2006.08.006. [DOI] [PubMed] [Google Scholar]
- [45].Zadjali Al S, Morse S, Chenoweth J, Deadman M. Personal safety issues related to the use of pesticides in agricultural production in the Al-Batinah region of Northern Oman. Sci Total Environ 2015;502:457-61. doi: 10.1016/j.scitotenv.2014.09.044. [DOI] [PubMed] [Google Scholar]
- [46].Schenker MB, Orenstein MR, Samuels SJ. Use of protective equipment among California farmers. Am J Ind Med 2002;42(5):455-64. doi: 10.1002/ajim.10134. [DOI] [PubMed] [Google Scholar]
- [47].Ricco M. Air temperature exposure and agricultural occupational injuries in the Autonomous Province of Trento (2000-2013, North-Eastern Italy). Int J Occup Med Environ Health 2018;31(3):317-33. doi: 10.13075/ijomeh.1896.01114. [DOI] [PubMed] [Google Scholar]
- [48].King MF, Bruner GC. Social desirability bias: a neglected aspect of validity testing. Psychol Mark 2000;17(2):79-103. doi: 10.1002/(SICI)1520-6793(200002)17:2<79::AID-MAR2>3.0.CO;2-0. [Google Scholar]
- [49].Hashemi SM, Rostami R, Hashemi MK, Damalas CA. Pesticide use and risk perceptions among farmers in Southwest Iran. Hum Ecol Risk Ass 2012;18(2):456-70. doi: 10.1080/10807039.2012.652472. [Google Scholar]
- [50].Oesterlund AH, Thomsen JF, Sekimpi DK, Maziina J, Racheal A, Jørs E. Pesticide knowledge, practice and attitude and how it affects the health of small-scale farmers in Uganda: a cross-sectional study. Afr Health Sci 2014;14(2):420-14. doi: 10.4314/ahs.v14i2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Ngowi AV, Maeda DN, Partanen TJ. Knowledge, attitudes and practices (KAP) among agricultural extension workers concerning the reduction of the adverse impact of pesticides in agricultural areas in Tanzania. Med Lav 2002;93(4):338-46. [PubMed] [Google Scholar]
- [52].Macri MC, Petriccione G, Povellato A, Pupo d’Andrea MR, Sardone R. Italian Agriculture 2010. Rome: Italian National Institute for Agricultural Economy; 2012. Available at: http://dspace.crea.gov.it/bitstream/inea/367/1/SE5-2013-4.pdf. Accessed on August 16, 2017. [Google Scholar]


