Abstract
Background:
Tibial tuberosity osteotomy (TTO) is a versatile procedure commonly used to treat patellar instability as well as to unload cartilage lesions. TTO with concomitant distalization (TTO-d) may be performed in patients with patella alta to stabilize the patella by helping it to engage in the trochlea earlier during flexion.
Purpose:
To identify and compare perioperative complications in patients who underwent TTO and those who underwent TTO-d and to analyze risk factors associated with these complications.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We retrospectively identified perioperative complications and associated factors from medical records for 240 patients who underwent TTO with or without distalization performed by 2 surgeons at 2 institutions between 2009 and 2015. A musculoskeletal radiologist at each institution determined osteotomy union using a published grading system. Significance was set at P < .01.
Results:
Of the 240 patients, 153 (122 TTO, 31 TTO-d) had clinical and radiographic follow-up of at least 90 days or evidence of osseous union. Eighty-eight complications were identified in 71 of 153 (46%) patients: delayed union (n = 35); painful hardware (n = 32); deep vein thrombosis (n = 4); clinical nonunion, delayed range of motion, sensory deficit, and wound breakdown (n = 3 each); and broken screw, fascial hernia, hematoma, quadriceps dysfunction, and tibial fracture (n = 1 each). Thirteen of 35 delayed unions occurred in the TTO-d group (P = .005). Painful hardware was more frequent in patients who received 4.5-mm screws (31/115) than in those who received 3.5-mm screws (1/38) (P = .001). A reoperation was required in 38 of 153 patients (37 patients using 4.5-mm screws vs 1 patient using 3.5-mm screws; P < .001), primarily for screw removal (32/38).
Conclusion:
Minor complications, including delayed union and painful hardware, were common, but major complications such as tibial fracture, deep vein thrombosis, and clinical nonunion were rare. Delayed union was more frequent in the TTO-d group. The 3.5-mm screws were less painful and less likely to need removal than the 4.5-mm screws.
Keywords: anteromedialization, complications, dislocation, distalization, instability, osteotomy, patella, patellofemoral, tibia, tuberosity
Various surgical options are available for treating patellar instability and/or patellofemoral pain and osteoarthritis, including soft tissue procedures such as medial patellofemoral ligament reconstruction or repair as well as numerous femoral and tibial osteotomies. These techniques are effective in most patients; however, complications can occur in 4% to 8% of cases.13,16
For tibial tuberosity osteotomy (TTO), fractures of the proximal tibia, loss of tibial tuberosity fixation, nonunion of the tuberosity, and deep vein thrombosis19 have been reported.1,5,10–15,22 The risk factors associated with these complications are incompletely understood; however, evidence suggests an increased risk of osseous complications with early weightbearing and with procedures involving complete detachment of the distal tuberosity, as required during distalization (Figures 1 and 2).7,13,18
Figure 1.
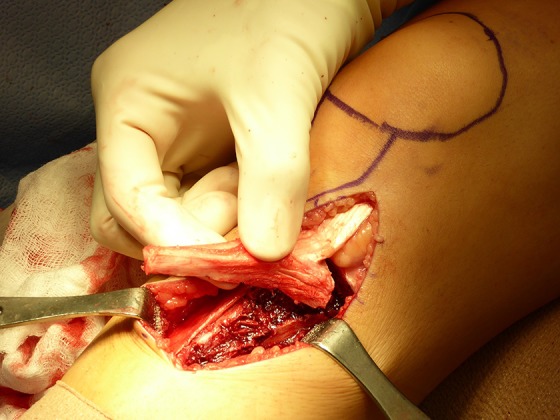
During distalization, the tibial tuberosity is completely detached from the tibia.
Figure 2.

The segment of bone that was removed from the distal tuberosity is then placed proximally in the gap created from distal translation of the tuberosity.
Our goals were to identify complications in patients who underwent TTO and to analyze patients who underwent concomitant distalization (TTO-d). We additionally analyzed surgical variables associated with complications, including the diameter and number of screws used for fixation. We hypothesized that osseous complications would be more prevalent in the TTO-d group, in which the tuberosity was completely detached, compared with the TTO group, in which the distal portion of the osteotomy site was greensticked.
Methods
Between 2009 and 2015, a total of 240 TTO procedures were performed by 2 experienced, fellowship-trained sports medicine orthopaedic surgeons (B.E.S.S., A.J.C.) at 2 institutions. Surgical indications were patellar instability or patellofemoral arthritis. Medialization was indicated for a tibial tuberosity–trochlear groove distance of greater than 15 to 20 mm. Anteromedialization was indicated for high-grade chondral lesions involving the inferior pole or lateral patellofemoral joint and when substantial retropatellar pain was present. Distalization was performed when the Caton-Deschamps index was greater than 1.3 to 1.4. Concomitant medial patellofemoral ligament reconstruction was performed in cases in which the medial restraints were incompetent, as determined by examination under anesthesia, or when the patella remained unstable after the tuberosity was moved. Concomitant lateral retinacular release was performed in cases in which the lateral retinaculum was excessively tight, as determined by the patellar tilt on examination under anesthesia. Osteotomies were fixed with either three 3.5 mm–diameter screws or two 4.5 mm–diameter screws.
After obtaining approval from the institutional review boards at both institutions, we reviewed the medical records of all patients who underwent TTO between 2009 and 2015. Preoperative history and physical examination information, as well as surgical details, were obtained. Postoperative symptoms and complications were determined from clinical notes. We excluded patients who had fewer than 90 days of clinical or radiographic follow-up unless they had evidence of a healed osteotomy site at final radiographic follow-up. A board-certified musculoskeletal radiologist at each institution (D.N.M., S.D.) reviewed each radiograph from his or her institution and determined osteotomy union using a mutually agreed-upon published grading system adapted for the proximal tibia.2 Delayed union was defined as incomplete healing according to these criteria at 90 days.
Data were collected independently at each institution and then uploaded and managed using REDCap electronic data capture tools hosted by Cornell University.6 Demographic characteristics and surgical variables, including distalization, screw diameter, and number of screws used, were recorded from the operative notes. Levels of association between these variables and complications were analyzed using the Pearson chi-square test or Fisher exact test for categorical data and the 2-sample Student t test for continuous data. We used Stata version 12 software (StataCorp). Findings of P < .01 were considered significant. A detailed description of the TTO surgical technique is included in the Appendix.
Results
Patient Characteristics
Of the 240 patients, 153 (64%) met our inclusion criteria (122 TTO, 31 TTO-d). The surgical indication was patellar instability in 134 (88%) patients and patellofemoral osteoarthritis in 19 (12%) patients. These 19 patients with patellofemoral osteoarthritis were all in the TTO group. All patients in the TTO-d group had patellar instability. The mean (±SD) follow-up time was 15.0 ± 0.3 months, with a range of 3.2 to 57.5 months. Compared with patients in the TTO group, patients in the TTO-d group were younger (mean age, 22 ± 0.9 vs 29 ± 1.1 years, respectively; P = .002) and had a lower mean body mass index (21 ± 0.9 vs 24 ± 0.4 kg/m2; P = .005) (Table 1).
TABLE 1.
Patient Characteristicsa
| Characteristic | TTO (n = 122) | TTO-d (n = 31) | P |
|---|---|---|---|
| Sex, n (%) | .726 | ||
| Male | 23 (19) | 5 (16) | |
| Female | 99 (81) | 26 (84) | |
| Age, y | 29 ± 1.1 (27-32) | 22 ± 0.9 (21-24) | .002 |
| Body mass index, kg/m2 | 24 ± 0.4 (23-24) | 21 ± 0.9 (19-23) | .005 |
| Current smoker, n (%) | 5 (4) | 1 (3) | >.999 |
| Previous surgery on operative knee, n (%) | 50 (41) | 8 (26) | .120 |
| Oral contraceptive use, n (%) | 30 (25) | 5 (16) | .470 |
| Follow-up, d | 428 ± 28 (373-482) | 541 ± 58 (422-660) | .069 |
aData are shown as mean ± SD (range) unless otherwise indicated. TTO, tibial tuberosity osteotomy; TTO-d, tibial tuberosity osteotomy with distalization.
Overall Complications
Seventy-one patients (46%) experienced at least 1 complication. There were 88 complications in 153 patients, including the following: delayed union (n = 35 [23%]); painful hardware (n = 32 [21%]); deep vein thrombosis (n = 4 [3%]); clinical nonunion, delayed range of motion, sensory deficit, and wound breakdown (n = 3 [2%] each); and broken screw, fascial hernia, hematoma, quadriceps dysfunction, and tibial fracture (n = 1 [1%] each). There were no cases of compartment syndrome, infection, or pulmonary embolism. Thirty-eight patients (25%) required a reoperation, most commonly for screw removal (32/38).
Complications by Osteotomy Type
The rate of delayed union, defined as incomplete healing by radiographic criteria at 90 days, was higher in the TTO-d group (42%) versus the TTO group (18%) (P = .005) (Table 2). Two patients in the TTO-d group (6.5%) and 1 patient in the TTO group (1%) were not healed at the time of the most recent visit, although this difference was not statistically significant. There were no other significant differences in the rates of clinical complications or reoperation between the 2 groups.
TABLE 2.
Complications by Osteotomy Typea
| Complication | TTO (n = 122) | TTO-d (n = 31) | P |
|---|---|---|---|
| ≥1 complication | 53 (43) | 18 (58) | .145 |
| Reoperation | 31 (25) | 7 (23) | .745 |
| Painful hardware | 27 (22) | 5 (16) | .463 |
| Delayed union | 22 (18) | 13 (42) | .005 |
| Deep vein thrombosis | 4 (3.3) | 0 (0.0) | .583 |
| Wound breakdown | 3 (2.5) | 0 (0.0) | >.999 |
| Delayed range of motion | 2 (1.6) | 1 (3.2) | .496 |
| Sensory deficit | 2 (1.6) | 1 (3.2) | .496 |
| Clinical nonunion | 1 (0.8) | 2 (6.5) | .105 |
| Fascial hernia | 1 (0.8) | 0 (0.0) | >.999 |
| Hematoma | 1 (0.8) | 0 (0.0) | >.999 |
| Quadriceps dysfunction | 1 (0.8) | 0 (0.0) | >.999 |
| Tibial fracture | 1 (0.8) | 0 (0.0) | >.999 |
| Broken screw | 0 (0.0) | 1 (3.2) | .203 |
aData are shown as n (%). TTO, tibial tuberosity osteotomy; TTO-d, tibial tuberosity osteotomy with distalization.
Complications by Screw Diameter
All osteotomies using two 4.5-mm screws were performed at one of the institutions, and those using three 3.5-mm screws were performed at the other institution. Patients were 10 times as likely to have symptomatic (painful or prominent) screws if their osteotomy was fixed with 4.5-mm screws (27%) compared with 3.5-mm screws (2.6%) (P = .001). Reoperations, most commonly for screw removal (32/38), were more frequent in osteotomies fixed with 4.5-mm screws (37 reoperations [32%]) versus 3.5-mm screws (1 reoperation [2.6%]) (P < .001). There were no other significant differences in the rates of clinical or radiographic complications by screw diameter (Table 3).
TABLE 3.
Complications by Screw Diametera
| Complication | 4.5-mm Screws (n = 115) | 3.5-mm Screws (n = 38) | P Value |
|---|---|---|---|
| ≥1 complication | 61 (53) | 10 (26) | .004 |
| Reoperation | 37 (32) | 1 (2.6) | <.001 |
| Delayed union | 31 (27) | 4 (11) | .045 |
| Painful hardware | 31 (27) | 1 (2.6) | .001 |
| Deep vein thrombosis | 4 (3.5) | 0 (0.0) | .573 |
| Clinical nonunion | 3 (2.6) | 0 (0.0) | .574 |
| Delayed range of motion | 2 (1.7) | 1 (2.6) | >.999 |
| Sensory deficit | 1 (0.9) | 2 (5.3) | .153 |
| Wound breakdown | 1 (0.9) | 2 (5.3) | .153 |
| Broken screw | 1 (0.9) | 0 (0.0) | >.999 |
| Fascial hernia | 1 (0.9) | 0 (0.0) | >.999 |
| Hematoma | 1 (0.9) | 0 (0.0) | >.999 |
| Quadriceps dysfunction | 1 (0.9) | 0 (0.0) | >.999 |
| Tibial fracture | 1 (0.9) | 0 (0.0) | >.999 |
aData are shown as n (%).
Discussion
In this series of 153 patients who underwent TTO, primarily for recurrent instability, major perioperative complications occurred in ≤3% of cases. The 3% rate of deep vein thrombosis was consistent with the 3.8% rate reported by Tanaka et al.19 Although the overall rate of delayed union (23%) was high, only 3 patients with clinical nonunion were identified. Of these 3 patients, 1 underwent revision TTO with the use of bone morphogenetic protein, and the other 2 eventually achieved union. This suggests that the accepted radiographic criteria for osteotomy healing may not be clinically important at 90 days and that it may be inappropriate to consider delayed union as a true complication. If delayed union is not considered to be a complication, the total number of complications drops to 53, with 31% of patients (47/153) experiencing at least 1 complication other than delayed union. Delayed union occurred more frequently in the TTO-d group compared with the TTO group. There were no significant differences between the 2 groups in complication rates.
Screw removal was required in 21% of patients, nearly all of whom underwent osteotomy using two 4.5-mm screws. This instrumentation has been used widely for tibial tuberosity anteromedialization osteotomy procedures since it was first described by Fulkerson4; however, no study has reported the rate of complications associated with different screw sizes and numbers. Theoretically, 3.5-mm screws could produce less irritation of the anterior soft tissues because they have a smaller and lower-profile screw head compared with 4.5-mm screws. Prior studies reporting screw sizes and the percentage of cases requiring removal support this idea.8 These studies suggest that 3.5-mm screws are removed in 16% of cases,17 4.0-mm screws are removed in 30% of cases,12 and 4.5-mm screws are removed in 52% of cases.9,14,21 The removal of screws of 6.5-mm diameter is typically planned per the protocol.3,9,20 This might explain the lower reoperation rate seen in procedures using 3.5-mm screws versus 4.5-mm screws in our study.
There was 1 tibial fracture in a 60-year-old woman who underwent TTO for patellofemoral osteoarthritis and who fell 8 weeks after surgery. The fracture occurred at the most distal 4.5-mm screw (Figure 3). The patient was treated nonoperatively with a brace, and the fracture healed without further complications.
Figure 3.

Lateral radiograph of the proximal tibia showing a transverse fracture exiting at the level of the far tip of the distal 4.5-mm screw.
Limitations
We recognize several major limitations in this study. First, we pooled data from patients who underwent procedures by 2 surgeons at 2 institutions with slightly different surgical techniques. Although operative techniques and surgeon experience were similar, differences in the technique may have influenced the results. Most importantly, all procedures using three 3.5-mm screws were performed by 1 surgeon at 1 institution, and all procedures using two 4.5-mm screws were performed by a second surgeon at the other institution. Therefore, it is possible that the differences that we observed in pain from screws and the need for surgical removal between cases performed with 3.5-mm versus 4.5-mm screws are a result of the surgeon’s technique, surgeon’s decision making, or institutional differences. For example, the practice of countersinking screws (a difference in technique between the 2 surgeons) could make screws less prominent and lessen the need for removal (a confounding variable with screw size). Other than the rates of painful hardware and reoperations for screw removal, no significant differences were found between complications at the 2 institutions.
Second, we included patients undergoing TTO for instability as well as for patellofemoral arthritis. We felt it appropriate to include multiple indications in our analysis of early perioperative complications because the surgical procedure did not differ by indication. Alternatively, if our goal had been to investigate long-term outcomes, recurrent instability, or conversion to arthroplasty rates, we would not have pooled surgeries performed for instability with those performed for arthritis.
Similarly, our follow-up time was less than 2 years; however, because the focus of the study was perioperative complications rather than long-term outcomes, we consider this to be sufficient to capture all complications during the period of interest. Additionally, the inclusion rate of 64% for this study (for lack of either clinical or radiological follow-up data) is not ideal; however, in this relatively young and healthy population of patients who overall do well after surgery, it is understandable that many patients may not return for final follow-up visits and radiographs.
Another limitation was that we were unable to determine the true frequency of incidental tuberosity detachment during TTO without distalization. Distalization, by nature, requires complete detachment of the shingle; therefore, distalization procedures serve as a surrogate for distal shingle detachment in our study. However, it is possible that the distal shingle was detached in some TTO procedures, and these were not specifically addressed.
Finally, it is possible that a difference in the overall complication rate between the TTO and TTO-d groups was not identified because there were not enough patients in each group to show such a difference. Using the effect size data from Payne et al,13 in which complication rates were reported as 10.70% in patients for whom the osteotomy shingle was completely detached (TTO-d in our study) versus 3.30% in patients for whom the distal shingle attachment was preserved (TTO in our study), a power of 0.80, and an alpha of 0.05, a minimum of 212 patients in each group would have been needed.
Conclusion
In the current study, 46% of patients experienced at least 1 complication. The risk of major complications was ≤3%. In this limited series, the risk of complications (other than delayed union) was not significantly higher in the patients who underwent distalization. The most common complication, painful hardware requiring removal, may potentially be avoided by using three 3.5-mm screws rather than two 4.5-mm screws.
APPENDIX
Surgical Technique
Patients who were indicated for TTO underwent examination under anesthesia to assess patellar translation and lateral retinacular tightness. Diagnostic knee arthroscopic surgery was then performed to evaluate the patellofemoral articular surfaces. Loose cartilage flaps were routinely debrided. At one institution, grade 4 cartilage lesions were typically addressed with juvenile particulate cartilage (DeNovo; Zimmer). Arthroscopic lateral retinacular release was performed when indicated according to radiographic criteria and a physical examination.
A tourniquet was inflated around the thigh, and the tibial crest and medial and lateral borders of the patellar tendon were exposed. The anterolateral compartment musculature was sharply released off the proximal anterolateral tibia as a single subperiosteal unit. The periosteum along the medial border of the patellar tendon was incised. At one institution, TTO was performed using a sagittal saw. Two 0.045-cm Kirschner wires were placed medial to lateral to serve as guides for the cut. The cut angle was determined by the desired degree of anteriorization. A 40-mm sagittal saw blade was then used to cut the tibia. The transverse cut was completed with a 10-mm straight osteotome and a 6-mm osteotome. The periosteum remained intact at the distal hinge. When concomitant distalization was indicated, the distal portion of the tibial tuberosity was completely detached from the tibia. The desired distalization (typically 8-12 mm) was achieved by removing the distal portion of the shingle and translating it distally. Fixation was achieved under fluoroscopic guidance using 2 fully threaded 4.5-mm cortical screws (Synthes). Screws were placed in a lagging fashion. Prophylactic anterior compartment release was also performed.
At the other institution, osteotomy was performed using a series of 2.5-mm drill bits placed 1 cm apart, beginning at the level of the tibial tuberosity and extending distally 6 to 7 cm. The medial side of the osteotomy site was completed by fracturing the bone between the drill holes with a 6-mm straight osteotome, and the lateral side was completed with a 6-mm curved osteotome. The transverse portion of the osteotomy site was completed with 6- and 12-mm straight osteotomes. The shingle was then translated anteromedially to the desired distance and slope according to preoperative calculations. The distal portion of the shingle remained attached to the tibia in almost all cases. When distalization was indicated, the shingle was released completely from the proximal tibial osteotomy bed (see Figure 1). The bone fragment from the distal portion of the shingle was used to fill the proximal gap and to provide a buttress to medial displacement (see Figure 2). Three fully threaded 3.5-mm cortical screws (Synthes) were used. The screw holes were countersunk. A local bone graft was harvested from the lateral side of the shingle and packed under the medial overhang. The anterior compartment muscles were repaired to the lateral side of the transferred shingle. No compartment release was performed.
After surgery, each patient underwent a standardized rehabilitation protocol that allowed progression to full weightbearing at 6 weeks.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: D.N.M. is a paid section editor for Rheumatology. B.E.S.S. is a consultant for Arthrex, is a paid speaker/presenter for Arthrex, and has received hospitality payments from DePuy. A.J.C. has received research support from the Arthroscopy Association of North America, has been paid to provide expert testimony, and receives royalties from Elsevier. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Johns Hopkins University’s Office of Human Subjects Research.
References
- 1. Bellemans J, Cauwenberghs F, Brys P, Victor J, Fabry G. Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer: a report of four cases. Am J Sports Med. 1998;26(2):300–302. [DOI] [PubMed] [Google Scholar]
- 2. Bhandari M, Chiavaras M, Ayeni O, et al. Assessment of radiographic fracture healing in patients with operatively treated femoral neck fractures. J Orthop Trauma. 2013;27(9):e213–e219. [DOI] [PubMed] [Google Scholar]
- 3. Endres S, Wilke A. A 10 year follow-up study after Roux-Elmslie-Trillat treatment for cases of patellar instability. BMC Musculoskelet Disord. 2011;12:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177:176–181. [PubMed] [Google Scholar]
- 5. Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18(5):490–496. [DOI] [PubMed] [Google Scholar]
- 6. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harrison RK, Magnussen RA, Flanigan DC. Avoiding complications in patellofemoral surgery. Sports Med Arthrosc Rev. 2013;21(2):121–128. [DOI] [PubMed] [Google Scholar]
- 8. Johnson AA, Cosgarea AJ. Complications of tibial tuberosity osteotomy. Sports Med Arthrosc. 2017;25(2):85–91. [DOI] [PubMed] [Google Scholar]
- 9. Karataglis D, Green MA, Learmonth DJ. Functional outcome following modified Elmslie-Trillat procedure. Knee. 2006;13(6):464–468. [DOI] [PubMed] [Google Scholar]
- 10. Luhmann SJ, Fuhrhop S, O’Donnell JC, Gordon JE. Tibial fractures after tibial tubercle osteotomies for patellar instability: a comparison of three osteotomy configurations. J Child Orthop. 2011;5(1):19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2545–2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Naveed MA, Ackroyd CE, Porteous AJ. Long-term (ten- to 15-year) outcome of arthroscopically assisted Elmslie-Trillat tibial tubercle osteotomy. Bone Joint J. 2013;95(4):478–485. [DOI] [PubMed] [Google Scholar]
- 13. Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The incidence of complications of tibial tubercle osteotomy: a systematic review. Arthroscopy. 2015;31(9):1819–1825. [DOI] [PubMed] [Google Scholar]
- 14. Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25(4):533–537. [DOI] [PubMed] [Google Scholar]
- 15. Pritsch T, Haim A, Arbel R, Snir N, Shasha N, Dekel S. Tailored tibial tubercle transfer for patellofemoral malalignment: analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):994–1002. [DOI] [PubMed] [Google Scholar]
- 16. Saltzman BM, Rao A, Erickson BJ, et al. A systematic review of 21 tibial tubercle osteotomy studies and more than 1000 knees: indications, clinical outcomes, complications, and reoperations. Am J Orthop. 2017;46(6):e396–e407. [PubMed] [Google Scholar]
- 17. Shelbourne KD, Porter DA, Rozzi W. Use of a modified Elmslie-Trillat procedure to improve abnormal patellar congruence angle. Am J Sports Med. 1994;22(3):318–323. [DOI] [PubMed] [Google Scholar]
- 18. Stetson WB, Friedman MJ, Fulkerson JP, Cheng M, Buuck D. Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med. 1997;25(4):570–574. [DOI] [PubMed] [Google Scholar]
- 19. Tanaka MJ, Munch JL, Slater AJ, Nguyen JT, Shubin Stein BE. Incidence of deep venous thrombosis after tibial tubercle osteotomy: a single case series study. Orthop J Sports Med. 2014;2(8):2325967114544457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tecklenburg K, Feller JA, Whitehead TS, Webster KE, Elzarka A. Outcome of surgery for recurrent patellar dislocation based on the distance of the tibial tuberosity to the trochlear groove. J Bone Joint Surg Br. 2010;92(10):1376–1380. [DOI] [PubMed] [Google Scholar]
- 21. Tjoumakaris FP, Forsythe B, Bradley JP. Patellofemoral instability in athletes: treatment via modified Fulkerson osteotomy and lateral release. Am J Sports Med. 2010;38(5):992–999. [DOI] [PubMed] [Google Scholar]
- 22. Valenzuela L, Nemtala F, Orrego M, et al. Treatment of patellofemoral chondropathy with the Bandi tibial tubercle osteotomy: more than 10 years follow-up. Knee. 2011;18(2):94–97. [DOI] [PubMed] [Google Scholar]


