Abstract
STUDY DESIGN:
Experimental laboratory study.
OBJECTIVE:
To characterize the differences in lower extremity gait biomechanics in individuals who have knee osteoarthritis (OA) with and without self-reported knee instability.
BACKGROUND:
Individuals with knee OA who experience episodes of knee instability often report gait difficulties that interfere with their daily lives. A better understanding of the alterations in gait biomechanics may help to mitigate symptomatic knee instability in this patient population.
METHODS:
Seventeen participants with knee OA and self-reported knee instability and 36 participants with knee OA and no self-reported knee instability underwent instrumented gait analysis on level ground. Knee-specific symptoms and functional limitations were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index.
RESULTS:
Knee instability was associated with greater odds of reporting moderate to severe gait-related pain (odds ratio = 6.0; 95% confidence interval: 1.2, 28.9) and moderate to severe difficulty when walking on flat surfaces (odds ratio = 10.7; 95% confidence interval: 1.7, 69.2). During early stance, the group with self-reported knee instability walked with a greater knee flexion excursion (P = .02) and a smaller lower extremity support moment (P<.01), due to reduced contributions from the hip extensors (P<.01) and ankle plantar flexors (P = .04). The group with self-reported knee instability also walked with a greater knee extensor contribution to the lower extremity support moment (P = .04) during the initial knee extension phase of gait compared to their counterparts with good knee stability.
CONCLUSION:
These findings suggest that self-reported knee instability is associated with significant alterations in hip, knee, and ankle joint function during the stance phase of gait in individuals with knee OA.
Keywords: biomechanics, kinematics, kinetics, lower extremity
Episodes of knee instability, described as sudden loss of postural support during weight bearing as a result of buckling, shifting, or giving way of the knee joint, are commonly reported in individuals with knee osteoarthritis (OA).9,13,19,26,35 Reports from several representative cohorts from the United States,13,26 Australia,9 and the Netherlands19,35 indicate that approximately 60% to 80% of individuals with knee OA report episodes of knee instability.
To this end, knee instability has been deemed an important and relevant independent variable related to functional limitations in individuals with knee OA, even after controlling for the effects of knee pain and muscle weakness.13,35 Although knee instability can occur during any weight-bearing task, at least 2 previous cohort studies have reported that most episodes of instability occur during gait.11,19 Therefore, better characterization of gait patterns adopted by individuals with knee OA who report episodes of knee instability may provide insight that could help guide development of approaches to minimize symptomatic knee instability in this patient population.
Schmitt and Rudolph30 previously suggested that the presence of self-reported knee instability may be an important predictor of knee movement strategies during gait in individuals with knee OA. More specifically, comparing the sagittal plane excursions of the knee joint in individuals with knee OA to those of a control group without knee OA, the presence of self-reported knee instability was significantly associated with decreased knee motion excursion during the phases of gait the authors described as weight acceptance (control, 16.2°; knee OA, 13.6°) and midstance (control, 20.1°; knee OA, 14.6°).30 Similarly, previous work by the present authors has demonstrated reduced knee flexion excursion during the early stance phase of downhill gait in individuals with medial compartment knee OA and self-reports of knee instability compared to a control group without knee OA (control, 17.4°; unstable knee OA, 9.7°).10 As knee flexion excursion during the early stance phase of gait (ie, weight acceptance) provides shock absorption through eccentric quadriceps muscle activity, reductions in knee motion excursion can have important negative consequences in terms of increased impulse loading and axial compression, potentially leading to accelerated rates of disease progression.8,23,25
It is important to note, however, that the previously reported reductions in knee joint excursion during gait in individuals with knee OA and self-reported knee instability have been observed when comparisons are made to volunteers without either knee OA or self-reported knee instability.10,30 Given that reduced knee flexion excursion has also been reported in individuals with knee OA and no reported knee instability,6,7,30 the exact contribution of self-reported knee instability to the observed reductions in knee motion excursion cannot be clearly elucidated. To this end, Schmitt and Rudolph31 recently reported no statistically signifi-cant differences in knee joint excursion between individuals with knee OA with and without self-reports of knee instability during the phases of gait the authors described as weight acceptance (stable knee OA, 12.5°; unstable knee OA, 9.8°) and midstance (stable knee OA, 16.6°; unstable knee OA, 12.5°) using disturbed walking to challenge knee stability. Although a trend toward reduced knee motion excursion is evident in individuals with knee OA and self-reported knee instability, the small sample size of the study (10 individuals with knee OA per group) may have prevented these group differences from reaching statistical significance. Additionally, whether knee mo tion excursion differs during normal gait on level ground between individuals with knee OA with and without self-reported knee instability was not investigated in this study and still remains unknown.
Evidence from studies of lower extremity biomechanics in unstable knees of individuals with anterior cruciate ligament (ACL) deficiency also suggests that contributions from the hip extensors and ankle plantar flexors may be important for providing knee stability during gait. While the activity of the hip extensors during early stance stabilizes the knee by tending to rotate the femur posteriorly, activity of the plantar flexors during the single-limb stance phase provides knee stability by controlling the forward rotation of the tibia.38,39 To this end, Rudolph and colleagues28 reported a reduced contribution from the knee extensors, but a compensatory increase in hip extensors, to the total lower extremity support moment during the weight-acceptance phase of gait in individuals with ACL-deficient knees. Similarly, Hurd and Snyder-Mackler17 reported that, in the unstable limb of individuals with an ACL-deficient knee, the knee extensor contribution to the total support moment is transferred to the ankle plantar flexors during the midstance phase of gait. These studies suggest that the primary strategy of compensating for a loss of knee control in the individual with an ACL-deficient knee may be a greater reliance on the hip extensors and ankle plantar flexors, which are already the primary contributors to lower extremity stability during gait.17,24 Although the primary cause of instability in an ACL-deficient knee and in a knee with OA is most likely different, the sudden loss of postural support in the sagittal plane as a result of buckling or giving way of the knee joint may require similar compensatory strategies for stability. To date, however, it remains unknown whether individuals with knee OA and self-reported knee instability also adopt a gait pattern similar to that of patients with ACL deficiency, who compensate for the loss of knee control by relying more on their hip extensors and ankle plantar flexors.
The primary objective of this study was to determine the differences in lower extremity biomechanics during gait in individuals with knee OA with and without self-reported knee instability. We hypothesized that participants with knee OA and self-reported knee instability would exhibit the following gait deviations compared to their stable-knee counterparts: (1) reduced knee flexion excursion during the early stance (ie, weight acceptance) and initial knee extension (ie, midstance) phases of gait, (2) lower knee extensor but higher hip extensor contribution to the total support moment during the early stance phase of gait, and (3) lower knee extensor but higher ankle plantar flexor contribution to the total support moment during the initial knee extension phase of gait.
METHODS
Participants
Biomechanical data from a sub-sample of 53 participants recruited as part of a randomized clinical trial of exercise therapy for knee OA12 were analyzed in this study. Participants were included in the current study if they met the 1986 American College of Rheumatology clinical criteria for knee OA2 and had primarily medial compartment disease of grade II or greater on the Kellgren-Lawrence18 radiographic disease severity scale. Potential participants with radiographic disease severity of grade II or greater in the lateral tibiofemoral compartment were excluded. For all participants, the knee in which they reported symptoms or episodes of instability was designated as the test knee. In cases where both knees experienced symptoms or instability, the more problematic knee, as chosen by the participant, was designated as the test knee. Participants with knee OA were then stratified into 1 of 2 mutually exclusive groups: those with self-reported knee instability (unstable knee, n = 17) and those with self-reported stable knees (stable knee, n = 36). Participants with knee OA were included in the unstable-knee group if they had a self-reported knee instability rating of 3 or less on a knee stability scale, indicating that the participant perceived the symptoms of knee instability as affecting the ability to perform activities of daily living.13 The test-retest reliability of this tool has previously been determined to be adequate, with an intraclass correlation coefficient (model 2,1) of 0.72 in a population that included individuals with knee OA.13 All data reported in this study were collected at baseline and prior to the participants receiving any intervention. All participants provided written informed consent approved by the Health Sciences Institutional Review Board of the University of Pittsburgh. The protocol for this study was approved by the Health Sciences Institutional Review Board of the University of Pittsburgh.
Gait Analysis
Participants walked along an 8.5-m vinyl-tiled walkway at a self-selected pace. An 8-camera Vicon V612 (OMG plc, Oxford, UK) motion-measurement system was used to capture 3-D motion data at a sampling rate of 120 Hz, using a Plug-in Gait (OMG plc) marker set. Two Bertec (Bertec Corporation, Columbus, OH) force platforms were used to obtain ground reaction forces at a rate of 1080 Hz and were synchronized with the motion data. An average of 5 trials at each participant’s self-selected normal gait velocity were collected and averaged for analysis. Participants were instructed not to target the force platforms when walking.
Biomechanics Data Management
Analysis of gait data was performed using a custom-written code (MATLAB Version 7.0; The MathWorks, Inc, Natick, MA). Joint angle trajectories from the Plug-in Gait model and ground reaction force data were low-pass filtered (Butterworth fourth order, zero phase lag) at 6 and 40 Hz, respectively. The trajectory data from the reflective markers combined with the ground reaction forces were used to calculate the external joint moments using inverse-dynamics equations and were normalized to body mass. Lower extremity biomechanics were then quantified for 2 distinct phases of the gait cycle: (1) early stance, defined as the time between initial contact and the peak knee flexion angle; and (2) initial knee extension, defined as the time from maximum knee flexion angle to peak knee extension angle during the late stance phase of gait.
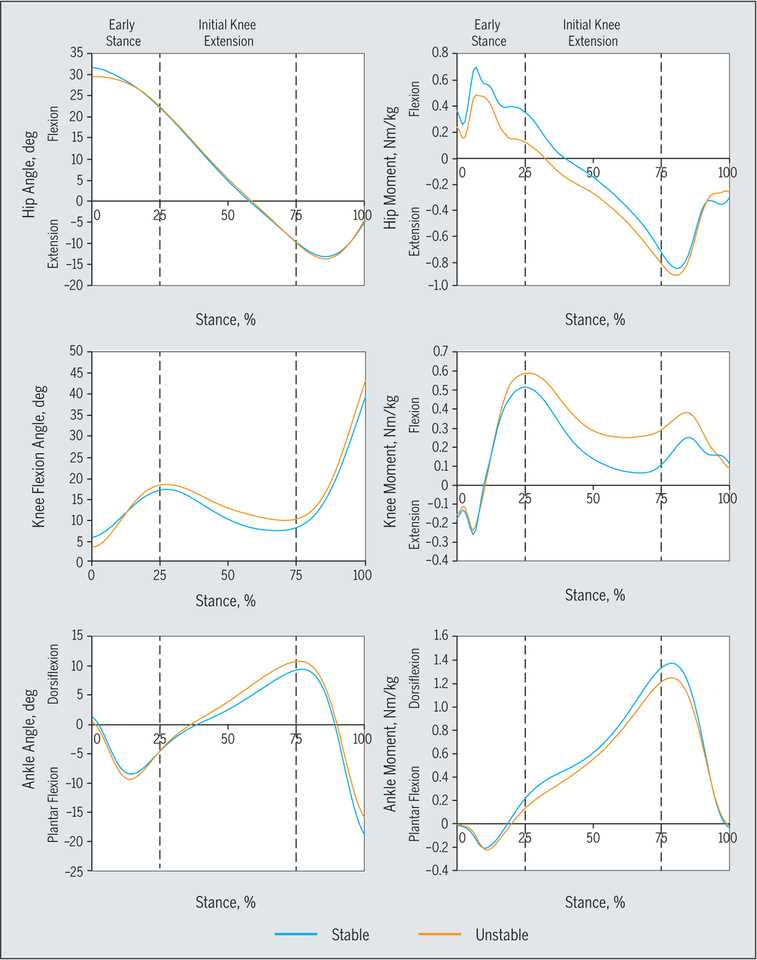
The knee joint motion excursion was defined as the maximum minus minimum joint position during the early stance and initial knee extension phases of gait. The total lower extremity support moment was also calculated for each phase of gait as a measure of stance stability and was quantified as the sum of the hip, knee, and ankle internal extensor moments, which are equal and opposite to the external flexion moments, calculated at each joint using inverse-dynamics equations (FIGURE 1).17,28,40 Individual joint contributions to the support moment were then calculated as the hip, knee, and ankle joint extensor moments divided by the total support moment and were expressed as percentages.
FIGURE 1.
Ensemble average sagittal plane joint motion and external joint moment waveforms for the hip, knee, and ankle during the stance phase of gait, based on the presence (unstable; self-reported knee instability) or absence (stable; no self-reported knee instability) of self-reported knee instability.
Self-Reported Symptoms and Functional Status
The 24-item Western Ontario and Mc-Master Universities Osteoarthritis Index (WOMAC) was used to gather knee-specific information on symptoms and limitations during performance of functional tasks. The WOMAC is a valid and reliable disease-specific measure of pain, stiffness, and physical function for individuals with knee OA.4,5,14,33 Higher scores on the WOMAC indicate increased severity of symptoms or functional limitations.
Knee Extension Strength and Range of Motion
The maximum voluntary isometric torque output for knee extension was measured using a Biodex System 3 (Bio dex Medical Systems, Shirley, NY) dynamometer. All tests were performed with the participant seated and the knee at 60° of flexion. A minimum of 3 trials and a maximum of 6 trials were performed. After 3 trials, when a trial had a maximum torque output less than the previous trial, strength testing was concluded. The highest maximum torque output from all trials was recorded as the knee extension strength score. To allow for between-participant comparisons, all knee extension torque values were normalized to the participant’s body weight. To verify the reliability of strength measurements, the maximum voluntary isometric torque tests were repeated for 40 participants on 2 different days. These data yielded a reliability intraclass correlation coefficient (model 2,1) of 0.96 (95% confidence interval [CI]: 0.94, 0.98). In addition, knee flexion and extension range of motion was measured in degrees using standard goniometric procedures. Based on previous literature, these measurements have excellent test-retest reliability (intraclass correlation coefficient = 0.96–0.99).27,37
Statistical Analysis
Independent-sample t tests and chi-square tests were used to determine group differences in demographics and medial compartment radiographic knee OA severity. Multivariable adjusted logistic regression models were used to evaluate the association between self-reported knee instability and having greater odds of experiencing pain and difficulty during gait. Self-reported pain during gait was evaluated from the response to the following question on the WOMAC pain subscale: “How much pain have you experienced over the last week while walking on flat surfaces?” Similarly, self-reported difficulty with gait was recorded from the response to the following question from the WOMAC physical function subscale: “How much difficulty have you had over the last week with walking on flat surfaces?” The answers to these questions were dichotomized into “none/mild” or “moderate/severe/extreme” and used as the outcome variables for the logistic regression models. This dichotomization scheme was used to identify individuals whose symptoms were severe enough to seek medical care, as most individuals seek treatment after they develop at least moderate levels of pain or difficulty with daily tasks. The associations between instability and reporting pain or difficulty with gait were expressed as adjusted odds ratios (ORs) and 95% CIs, accounting for age, sex, body mass index, and medial compartment radiographic disease severity as covariates in the model.
Comparisons of group differences in knee-specific impairments, WOMAC scores, and lower extremity biomechanics variables were performed using an analysis of covariance adjusted for sex and height. All biomechanical comparisons were also adjusted for gait speed, given the dependence of lower extremity kinematics and kinetics on this variable.20 All statistical comparisons were performed using the Stata Version 11.2 statistical software program (StataCorp LP, College Station, TX).
RESULTS
Participants in the unstable-knee group were more likely to be female (65% versus 36%, P = .05); were an average of 6.2 cm shorter in height (P<.01); and had higher WOMAC pain, physical function, and stiffness subscale scores (P<.01) compared to their stable-knee counterparts (TABLE 1). The results of the logistic regression analyses further revealed that self-reported knee instability was associated with greater odds of experiencing moderate/severe/extreme pain when walking (59% versus 25%; OR = 6.0; 95% CI: 1.2, 28.9; P = .03) and greater odds of reporting difficulty while walking on flat surfaces (41% versus 14%; OR = 10.7; 95% CI: 1.7, 69.2; P = .01).
TABLE 1.
Participant Characteristics*
| Stable (n = 36) | Unstable (n = 17) | P Value† | |
|---|---|---|---|
| Age, y | 63.8 ± 8.3 | 61.3 ± 6.5 | .28 |
| Female, n (%) | 13 (36) | 11 (65) | .05 |
| Height, cm | 172.7 ± 8.3 | 166.5 ± 5.4 | <01 |
| Weight, kg | 85.1 ± 14.7 | 84.6 ± 12.0 | .89 |
| Body mass index, kg/m2 | 28.6 ±5.5 | 30.6 ± 4.8 | .22 |
| Medial compartment radiographic severity, n (%)‡ | .91 | ||
| Grade II | 5 (14) | 3 (18) | |
| Grade III | 21 (58) | 9 (53) | |
| Grade IV | 10 (28) | 5 (29) | |
| Bilateral knee OA, n(%) | 10 (28) | 4 (24) | .74 |
| WOMAC | |||
| Pain score (0–20) | 4.8 ± 3.3 | 6.8 ± 2.6 | <01 |
| Physical function score (0–68) | 14.9 ± 10.6 | 24.3 ± 70 | <01 |
| Stiffness score (0–8) | 2.6 ± 1.5 | 3.8 ± 1.1 | <01 |
| Knee extension strength, Nm/kg | 1.9 ± 0.6 | 1.7 ± 0.4 | .28 |
| Knee flexion ROM, deg | 132.0 ± 10.7 | 128.9 ± 14.3 | .32 |
| Knee extension ROM, deg§ | −6.2 ± 6.0 | −5.6 ± 4.2 | .64 |
| Gait speed, m/s | 1.3 ± 0.2 | 1.2 ± 0.1 | <01 |
Abbreviations: OA, osteoarthritis; ROM, range of motion; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Values are mean ± SD unless otherwise indicated.
Analyses of the group differences in WOMAC scores and knee-specific impairments were adjusted for age, sex, body mass index, and radiographic tibiofemoral joint disease severity.
All patients had to have at least grade II knee OA to be included in the study.
Negative numbers denote limited knee extension ROM.
The unstable-knee group demonstrated greater knee motion excursion during early stance compared to the stable-knee group (mean ± SD, 15.6° ± 6.0° versus 12.1° ± 5.2°; P = .02) (FIGURE 1), but not during the initial knee extension phase of gait (9.4° ± 5.0° versus 10.6° ± 5.8°; P = .42) (FIGURE 1). The unstable-knee group also walked with significantly lower total support moment (P<.01) and reduced contributions from the hip extensors (P<.01) and the ankle plantar flexors (P = .04) during the early stance phase of gait compared to their stable-knee counterparts (TABLE 2). In contrast, although a significantly greater contribution from the knee extensors to the total support moment was observed in the unstable-knee group dur ing the initial knee extension phase of gait (P = .04), the total support moment and contributions from the hip extensors and ankle plantar flexors were not significantly different between groups (TABLE 2).
TABLE 2.
Comparisons of the Lower Extremity Total Support Moment and the Associated Contributions From the Hip, Knee, and Ankle Joints During the Early Stance and Initial Knee Extension Phases of Gait Based on the Presence or Absence of Self-Reported Knee Instability*
| Stable (n = 36) | Unstable (n = 17) | P Value | |
|---|---|---|---|
| Early stance | |||
| Hip extensor moment | 13.3 ± 6.0 (58.1) | 8.8 ± 4.5 (53.3) | <01 |
| Knee extensor moment | 73 ±5.3(32.9) | 6.7 ± 3.6 (41.4) | .69 |
| Ankle plantar flexor moment | 2.2 ±2.8 (9.0) | 0.8 ±0.7 (5.2) | .04 |
| Total support moment | 22.9 ± 6.7 (NA) | 16.4 ± 5.0 (NA) | <.01 |
| Initial knee extension | |||
| Hip extensor moment | 4.4 ± 5.9 (10.0) | 2.5 ± 3.2 (5.9) | .22 |
| Knee extensor moment | 11.8 ±9.3 (25.1) | 18.2 ± 12.6 (34.2) | .04 |
| Ankle plantar flexor moment | 29.9 ± 9.0 (64.9) | 28.4 ± 78 (59.8) | .52 |
| Total support moment | 46.2 ± 9.9 (NA) | 49.1 ± 16.1 (NA) | .43 |
Abbreviation: NA, not applicable.
Values are mean ± SD (percent contribution) Nm/kg. All analyses were adjusted for sex, height, and gait speed.
DISCUSSION
The observation of greater knee flexion excursion during the early stance phase of gait in the group with knee OA and self-reported knee instability in our study was unexpected, as it differs from current theories that associate knee instability with a joint-stiffening strategy. Evidence from previous studies in knees with OA or ACL deficiency suggests that individuals with unstable knees often adopt a combined strategy of lesser knee flexion excursion and greater muscular cocontraction to maintain knee stability in response to the high demands of the early stance phase of gait.7,17,21,22,30 Interestingly, the 3.5° of greater knee flexion excursion during the early stance phase of gait observed in our unstable-knee group is similar in magnitude to the reduction in knee flexion excursion previously reported for patients with knee OA compared to OA-free control individuals.6,7,30 This finding suggests that the frequently adopted knee-stiffen ing gait strategy thought to improve knee stability during the early stance phase of gait in individuals with knee OA was not evident in those with unstable knees, which might have contributed to their self-reported instability.
The apparent inconsistency between the knee flexion excursion during the early stance phase of gait in the unstable-knee group in the current study and that in previous reports10,30 may be due to important differences in study design. For example, the current study used a comparison group that consisted of individuals with knee OA without reports of knee instability, as opposed to a control group of volunteers without either knee OA or reports of knee instability, which has been used in previous studies.10,30 Given that participants in both of the experimental groups in our study had knee OA with similar radiographic disease severity, the biomechanical differences observed between groups are most likely unique to the presence of self-reported knee instability and not due to common degenerative joint changes that occur solely as a result of the OA process. In addition, the present study allowed participants to walk at their preferred self-selected gait velocity instead of at predetermined gait velocities (ranging from 0.75 to 1.34 m/s) as used in previous studies.7,10 Requiring individuals with knee OA to walk at velocities that are either faster or slower than their usual walking speed may result in gait patterns that the participants would not normally use in their daily lives, which could render the interpretation of the gait data difficult.
As the quadriceps muscles eccentrically control the flexion excursion of the knee joint during the early stance phase of gait, it has been suggested that alterations in knee flexion excursion may be related to the strength of the quadriceps.21 However, the lack of significant group differences in quadriceps muscle strength between the stable and unstable knee OA groups in the present study did not support this premise. Another potential explanation for the observed increase in knee flexion excursion during the early stance phase of gait in the unstable-knee group could be that higher knee flexion angles can enhance lower extremity stability during weight bearing through greater quadriceps muscle activity.16 As such, increased knee flexion excursion during the early stance phase of gait in the unstable-knee group may be a deliberate attempt to elicit greater dynamic lower extremity stability during the ensuing initial knee extension phase of gait, when the ability for compensation to enhance stability is limited due to the entire weight of the body being supported by the stance leg. This notion is supported by the greater knee extensor moment observed during the initial knee extension phase of gait in our unstable-knee group, which began at the end of the early stance phase of gait due to a greater knee flexion excursion (FIGURE 1). It is interesting to note that the greater knee extensor moments in our unstable-knee group were present despite slower gait speeds, which would theoretically lead to decreased joint moments,20 further supporting the compensatory nature of this observation.
During the initial knee extension phase of normal gait, as the center of mass moves forward and the ground reaction force moves anterior to the knee center of rotation, the knee extends passively, which diminishes the need for quadriceps activity.24 In our unstable-knee group, however, the greater knee extensor moments during the initial knee extension phase of gait denote increased quadriceps activity29 during a time in the gait cycle when the quadriceps should be inactive.24 This is a perplexing choice, as the greater associated joint compression36 due to greater knee extensor moments may be responsible for the increased knee pain reported during gait in our unstable-knee group.3,34 In fact, closer inspection of the data provides support for this assertion, as all 10 participants in the unstable-knee group who walked with a knee extensor moment during the initial knee extension phase of gait reported having moderate to extreme pain. Of the remaining 7 participants with self-reported knee instability who did not report having pain during gait, only 3 walked with a knee extensor moment instead of the normally expected knee flexor moment during the initial knee extension phase of gait.38,39
Our hypothesis that the unstable-knee group would rely more on their hip extensors during the early stance phase of gait to compensate for the loss of knee control was not supported by the data. In fact, the unstable-knee group in our study demonstrated a much smaller contribution from their hip extensors to the total support moment during the early stance phase of gait. Given that hip extensor weakness is common in patients with knee OA,1,15 it is plausible that compensatory strategies aimed at reducing the demands placed on the hip extensors during the early stance phase of gait, such as a shorter step length32 or a posterior trunk lean,24 could have resulted in the lesser hip extensor contribution to the total support moment in the unstable group. Further research is needed to determine the exact cause of the reduced hip extensor moments in individuals with knee OA and self-reported instability. Regardless of the cause, however, it has been suggested that an important function of the hip extensors’ contribution to the total support moment during the early stance phase of gait is to stabilize the femur to prevent excessive knee flexion.39 Therefore, the greater knee flexion excursions observed during the early stance phase of gait in the unstable-knee group could have been in part due to the lack of adequate hip extensor activity.
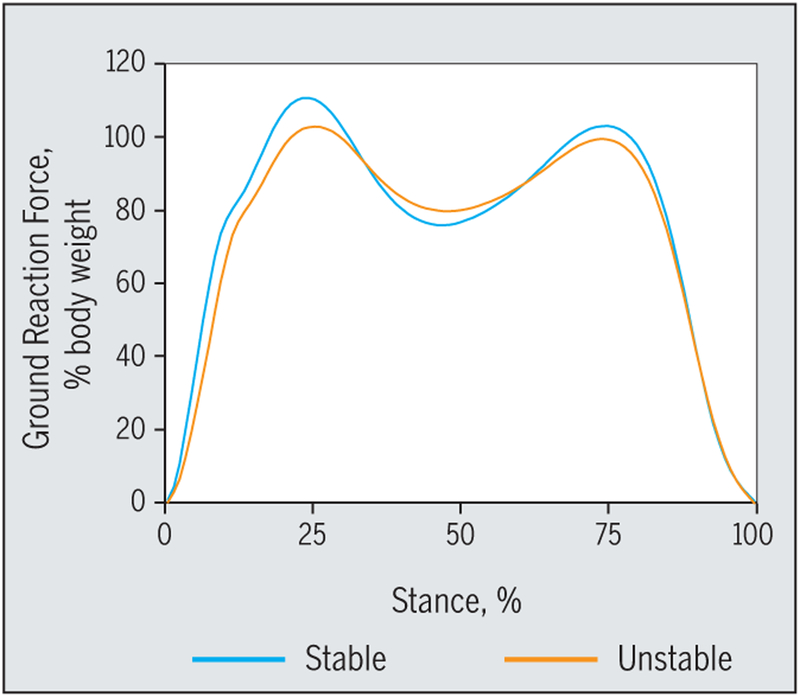
Individuals with knee OA and self-reported instability in our study also demonstrated lower total support moments compared to the stable-knee group. Given that the projection of the vertical ground reaction force vector is utilized in determining the hip, knee, and ankle extensor moments that make up the total support moment, we hypothesized that potential compensatory strategies to minimize the effects of the ground reaction forces on the lower extremity might have resulted in the lower total support moment in the unstable-knee group. To explore this hypothesis, we performed a post hoc analysis of the early stance peak vertical ground reaction force between the stable-knee and unstable-knee groups. This analysis revealed that individuals with knee OA and self-reported knee instability walked with a significantly lower early stance peak ground reaction force compared to their stable-knee counterparts (mean ± SD, 1.0 ± 0.1 versus 1.1 ± 0.1 Nm/kg; P = .005) (FIGURE 2). However, this difference was small and no longer statistically significant after accounting for the slower self-selected gait speed of the group with OA and self-reported knee instability.
FIGURE 2.
Ensemble average vertical ground reaction force profile during the stance phase of gait, based on the presence (unstable; self-reported knee instability) or absence (stable; no self-reported knee instability) of self-reported knee instability.
Although sagittal plane joint moments and, therefore, the total support moment could also decrease in magnitude as walking speed decreases, the group differences in total support moment in our study persisted even after controlling for the potential confounding effects of gait speed. It is also plausible that the compensatory strategies that reduce hip extensor activity, which is the major contributor to the total support moment during the early stance phase of gait, might have led to the lower total support moments in the unstable-knee group. As the lower total support moment can increase the probability of experiencing an instability episode during gait, further research into determining the potential underlying causes of lower total support moment in individuals with knee OA and self-reported instability is warranted.
The hypothesis that the unstable-knee group would demonstrate a lower knee extensor contribution but higher ankle plantar flexor contribution to the total support moment during the initial knee extension phase of gait to compensate for the loss of knee control was also not supported by the data. Although the total support moment was not significantly different between groups, a much higher knee extensor contribution to the total support moment was observed in the unstable-knee group during this phase of gait. This finding was unexpected, as previous research in unstable ACL-deficient knees indicates that the preferred strategy of compensating for a loss of knee control during the initial knee extension phase of gait is one of greater reliance on the ankle plantar flexors, which are normally the primary contributors to limb stability during this phase of gait.17 In our unstable-knee group, however, the preferred strategy for lower extremity stability appeared to be one of utilizing higher knee extensor moments to increase the total support moment to similar levels compared to the stable-knee OA group, despite slower gait speeds.
While greater knee extensor moment during gait may lead to enhanced lower extremity stability via greater quadriceps activity, the associated higher joint compressions36 may also result in greater pain and put the articular cartilage at higher risk for further erosion. The greater knee extensor moments and the higher associated quadriceps muscle activity may also expose the knee joint to high compressive and shear loads that can challenge the passive stability of the knee joint in individuals with knee OA and self-reported instability. However, the improved dynamic lower extremity stability provided by greater knee extensor moments during the initial knee extension phase of gait may be necessary, as the ability for compensation is limited due to the entire weight of the body being supported by the stance limb. Therefore, this gait strategy may reflect the inability of this patient population to control lower extremity stability by any other means. Further work is needed to delineate the potential positive compensatory versus maladaptive effects of higher knee extensor moments during the initial knee extension phase of gait in individuals with knee OA and self-reported knee instability.
The findings of this study should be considered in light of its limitations. Joint instability in individuals with knee OA is most likely a multifactorial prob lem that may be influenced by poor proprioception; hip and ankle joint muscle weakness; as well as altered neuromuscular control strategies, such as increased muscle cocontractions; factors that were not evaluated as a part of this investigation. Additionally, given that our study only included individuals with medial compartment knee OA, the potential role and contributions of the lateral knee compartment or patellofemoral joint disease to self-reported complaints of instability remain unknown. Radiographic and dynamic frontal plane changes in lower extremity alignment and trans-verse plane lower extremity motion may also be related to instability in individuals with knee OA but were not considered in the current study. Future efforts should consider the potential role of these factors and their possible interactions in influencing gait biomechanics to provide a clearer picture of the relative contribution of each of these impairments to symptomatic knee instability.
CONCLUSION
The FIndings of this study indicate that individuals with knee OA and self-reported knee instability experience significantly greater levels of pain and difficulty while walking on flat surfaces. Self-reported knee instability was also associated with an increased knee flexion excursion during the early stance phase of gait, a finding that differs from current theories that associate knee instability with a knee-stiffening strategy. Additionally, it appears that individuals with knee OA and self-reports of instability walk with reduced reliance on their hip extensor and ankle plantar flexor muscle groups during the stance phase of gait.
KEY POINTS
FINDINGS:
Self-reported knee instability in participants with knee OA was associated with an increased knee flexion excursion and a smaller lower extremity support moment, along with diminished stability contributions from the hip extensors during the early stance phase of gait. Additionally, the presence of self-reported instability was associated with increased knee extensor contribution to the total support moment during the initial knee extension phase of gait.
IMPLICATIONS:
The observed deviations in gait biomechanics in individuals with knee OA and instability may be related to their increased self-reported levels of pain and difficulty during gait.
CAUTION:
Joint instability in individuals with knee OA is most likely a multifactorial issue, with contributions from a number of impairments that were not considered in this study. Additional research is needed to better understand all of the contributing factors to symptomatic knee instability and their potential interactions.
Acknowledgments
The protocol for this study was approved by the Health Sciences Institutional Review Board of the University of Pittsburgh. This project was supported by the National Institutes of Health through grant numbers 1-R01-AR048760 and K12 HD055931 and by the Pittsburgh Claude D. Pepper Older Americans Independence Center through grant number P30 AG024827. The study sponsors had no role in the study design, data collection, analysis, or writing of this manuscript. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
REFERENCES
- 1.Alnahdi AH, Zeni JA, Snyder-Mackler L. Muscle impairments in patients with knee osteoarthritis. Sports Health. 2012;4:284–292. 10.1177/1941738112445726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29:1039–1049. 10.1002/art.1780290816 [DOI] [PubMed] [Google Scholar]
- 3.Amin S, Luepongsak N, McGibbon CA, LaValley MP, Krebs DE, Felson DT. Knee adduction moment and development of chronic knee pain in elders. Arthritis Rheum. 2004;51:371–376. 10.1002/art.20396 [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Bellamy N, Kean WF, Buchanan WW, Gerecz-Simon E, Campbell J. Double blind randomized controlled trial of sodium meclofenamate (Meclomen) and diclofenac sodium (Voltaren): post validation reapplication of the WOMAC Osteoarthritis Index. J Rheumatol. 1992;19:153–159. [PubMed] [Google Scholar]
- 6.Briem K, Snyder-Mackler L. Proximal gait adaptations in medial knee OA. J Orthop Res. 2009;27:78–83. 10.1002/jor.20718 [DOI] [PubMed] [Google Scholar]
- 7.Childs JD, Sparto PJ, Fitzgerald GK, Bizzini M, Irrgang JJ. Alterations in lower extremity movement and muscle activation patterns in indi viduals with knee osteoarthritis. Clin Biomech (Bristol, Avon). 2004;19:44–49. 10.1016/j.clinbiomech.2003.08.007 [DOI] [PubMed] [Google Scholar]
- 8.Cook TM, Farrell KP, Carey IA, Gibbs JM, Wiger GE. Effects of restricted knee flexion and walking speed on the vertical ground reaction force during gait. J Orthop Sports Phys Ther. 1997;25:236–244. 10.2519/jospt.1997.25.4.236 [DOI] [PubMed] [Google Scholar]
- 9.Creaby MW, Wrigley TV, Lim BW, Hinman RS, Bryant AL, Bennell KL. Self-reported knee joint instability is related to passive mechanical stiffness in medial knee osteoarthritis. BMC Musculoskelet Disord. 2013;14:326 10.1186/1471-2474-14-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farrokhi S, Tashman S, Gil AB, Klatt BA, Fitzgerald GK. Are the kinematics of the knee joint altered during the loading response phase of gait in individuals with concurrent knee osteoarthritis and complaints of joint instability? A dynamic stereo X-ray study. Clin Biomech (Bristol, Avon). 2012;27:384–389. 10.1016/j.clinbiomech.2011.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felson DT, Niu J, McClennan C, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–540. 10.7326/0003-4819-147-8-200710160-00005 [DOI] [PubMed] [Google Scholar]
- 12.Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91:452–469. 10.2522/ptj.20100188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51:941–946. 10.1002/art.20825 [DOI] [PubMed] [Google Scholar]
- 14.Hawker G, Melfi C, Paul J, Green R, Bombardier C. Comparison of a generic (SF-36) and a disease specific (WOMAC) (Western Ontario and McMaster Universities Osteoarthritis Index) instrument in the measurement of outcomes after knee replacement surgery. J Rheumatol. 1995;22:1193–1196. [PubMed] [Google Scholar]
- 15.Hinman RS, Hunt MA, Creaby MW, Wrigley TV, McManus FJ, Bennell KL. Hip muscle weakness in individuals with medial knee osteoarthritis. Arthritis Care Res (Hoboken). 2010;62:1190–1193. 10.1002/acr.20199 [DOI] [PubMed] [Google Scholar]
- 16.Houck J, Lerner A, Gushue D, Yack HJ. Self-reported giving-way episode during a stepping-down task: case report of a subject with an ACL-deficient knee. J Orthop Sports Phys Ther. 2003;33:273–282; discussion 283–286. 10.2519/jospt.2003.33.5.273 [DOI] [PubMed] [Google Scholar]
- 17.Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007;25:1369–1377. 10.1002/jor.20440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kellgren JH, Lawrence JS. Radiological as sessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knoop J, van der Leeden M, van der Esch M, et al. Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: results from the Amsterdam Osteo-arthritis cohort. Arthritis Care Res (Hoboken). 2012;64:38–45. 10.1002/acr.20597 [DOI] [PubMed] [Google Scholar]
- 20.Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture. 2003;17:106–112. 10.1016/S0966-6362(02)00060-7 [DOI] [PubMed] [Google Scholar]
- 21.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002;17:56–63. 10.1016/S0268-0033(01)00097-3 [DOI] [PubMed] [Google Scholar]
- 22.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12:745–751. 10.1016/j.joca.2004.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844. 10.1002/art.21262 [DOI] [PubMed] [Google Scholar]
- 24.Perry J Gait Analysis: Normal and Pathological Function. Thorofare, NJ: SLACK Incorporated; 1992. [Google Scholar]
- 25.Radin EL, Yang KH, Riegger C, Kish VL, O’Connor JJ. Relationship between lower limb dynamics and knee joint pain. J Orthop Res. 1991;9:398–405. 10.1002/jor.1100090312 [DOI] [PubMed] [Google Scholar]
- 26.Ramsey DK, Snyder-Mackler L, Lewek M, New-comb W, Rudolph KS. Effect of anatomic realignment on muscle function during gait in patients with medial compartment knee osteoarthritis. Arthritis Rheum. 2007;57:389–397. 10.1002/art.22608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63:1611–1615. [DOI] [PubMed] [Google Scholar]
- 28.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71. 10.1007/s001670000166 [DOI] [PubMed] [Google Scholar]
- 29.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–119. 10.1002/jor.1100090114 [DOI] [PubMed] [Google Scholar]
- 30.Schmitt LC, Rudolph KS. Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Rheum. 2007;57:1018–1026. 10.1002/art.22889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmitt LC, Rudolph KS. Muscle stabilization strategies in people with medial knee osteo-arthritis: the effect of instability. J Orthop Res. 2008;26:1180–1185. 10.1002/jor.20619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schulz BW, Ashton-Miller JA, Alexander NB. The effects of age and step length on joint kinematics and kinetics of large out-and-back steps. Clin Biomech (Bristol, Avon). 2008;23:609–618. 10.1016/j.clinbiomech.2008.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stucki G, Sangha O, Stucki S, et al. Comparison of the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index and a self-report format of the self-administered Lequesne–Algofunctional index in patients with knee and hip osteoarthritis. Osteoarthritis Cartilage. 1998;6:79–86. 10.1053/joca.1997.0097 [DOI] [PubMed] [Google Scholar]
- 34.Thorp LE, Sumner DR, Wimmer MA, Block JA. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis Rheum. 2007;57:1254–1260. 10.1002/art.22991 [DOI] [PubMed] [Google Scholar]
- 35.van der Esch M, Knoop J, van der Leeden M, et al. Self-reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clin Rheumatol. 2012;31:1505–1510. 10.1007/s10067-012-2025-1 [DOI] [PubMed] [Google Scholar]
- 36.Walter JP, D’Lima DD, Colwell CW Jr., Fregly BJ. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res. 2010;28:1348–1354. 10.1002/jor.21142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and vi sual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71:90–96; discussion 96–97. [DOI] [PubMed] [Google Scholar]
- 38.Winter DA. Kinematic and kinetic patterns in human gait: variability and compensating effects. Hum Mov Sci. 1984;3:51–76. [Google Scholar]
- 39.Winter DA. Overall principle of lower limb support during stance phase of gait. J Biomech. 1980;13:923–927. [DOI] [PubMed] [Google Scholar]
- 40.Winter DA, Eng P. Kinetics: our window into the goals and strategies of the central nervous system. Behav Brain Res. 1995;67:111–120. [DOI] [PubMed] [Google Scholar]