Abstract
Introduction
For patients with perihilar cholangiocarcinoma (CCA), surgery is the only treatment modality that can result in cure. Unfortunately, in the majority of these patients, the tumours are found to be unresectable at presentation due to either local invasive tumour growth or the presence of distant metastases. For patients with unresectable CCA, palliative chemotherapy is the standard treatment yielding an estimated median overall survival (OS) of 12–15.2 months. There is no evidence from randomised trials to support the use of stereotactic body radiation therapy (SBRT) for CCA. However, small and most often retrospective studies combining chemotherapy with SBRT have shown promising results with OS reaching up to 33–35 months.
Methods and analysis
This study has been designed as a single-centre phase I feasibility trial and will investigate the addition of SBRT after standard chemotherapy in patients with unresectable perihilar CCA (T1-4 N0-1 M0). A total of six patients will be included. SBRT will be delivered in 15 fractions of 3–4.5 Gy (risk adapted). The primary objective of this study is to determine feasibility and toxicity. Secondary outcomes include local tumour control, progression-free survival (PFS), OS and quality of life. Length of follow-up will be 2 years. As an ancillary study, the personalised effects of radiotherapy will be measured in vitro, in patient-derived tumour and bile duct organoid cultures.
Ethics and dissemination
Ethics approval for the STRONG trial has been granted by the Medical Ethics Committee of Erasmus MC Rotterdam, the Netherlands. It is estimated that all patients will be included between October 2017 and October 2018. The results of this study will be published in a peer-reviewed journal, and presented at national and international conferences.
Trial registration number
NCT03307538; Pre-results.
Keywords: perihilar cholangiocarcinoma, klatskin tumour, stereotactic body radiation oncology
Strengths and limitations of this study.
A promising local treatment option will be studied for patients with unresectable perihilar cholangiocarcinoma.
The fractionation scheme used in this trial makes it possible to deliver a relative high-radiation dose to the tumour and protect surrounding organs.
Toxicity will be closely observed.
Interfraction and intrafraction motion will be assessed using multiple CT scans during treatment.
The study population is small; therefore, no robust analysis other than feasibility and toxicity can be done.
Introduction
Cholangiocarcinoma (CCA) is the second most common primary liver tumour worldwide.1 CCA accounts for 3% of all gastrointestinal tumours.2 Of all CCA, approximately 50%–70% arise at the hilar plate of the biliary tree, and these tumours are being referred to as either perihilar CCA or Klatskin tumours.3 Resection is the only potential curative treatment for patients with perihilar CCA. Median overall survival (OS) ranges from 27 to 58 months among operated patients with negative resection margins.4 Unfortunately, the majority of patients present with unresectable disease at diagnosis.4 5 Selected patients are eligible for liver transplantation. Five-year survival rates for both margin-negative resection and neoadjuvant therapy combined with liver transplantation are similar.4
The standard treatment for patients with unresectable or metastatic perihilar CCA is chemotherapy that consists of eight courses of gemcitabine and cisplatin. The survival rates for inoperable patients who receive this chemotherapy regimen are poor: Valle et al reported in a prospective study (ABC-02 trial) a median OS of 11.7 months and a PFS of 8.0 months.6 In a retrospective study, Eckmann et al showed a median OS of 15.2 months in these patients treated with gemcitabine and cisplatin. Partial response or stable disease rates of 72% were found, with a median duration of response of 8.1 months.7
Local ablative therapies
Because of these poor OS rates for patients treated with chemotherapy, some local therapies have been investigated. One of these treatment options is ablation with irreversible electroporation (IRE), which is currently under investigation in the ALPACA trial.8 Until now there is little evidence to support the routine use of IRE for patients with perihilar CCA. One case report describes a technically successful procedure, but data on toxicity and disease outcome are lacking.9 Another local therapy option is radiofrequency ablation (RFA). Wu et al 10 published a retrospective study that showed prolongation of stent patency and better functional status and quality of life (QoL) in a group of patients treated with intraductal RFA before stent placement, compared with stent placement alone. There are no data on disease outcome after RFA. A third ablative therapy option is photodynamic therapy using temoporfin. Wagner et al report a local response after one treatment of 55%, with a median time to local tumour progression of 6.5 months, but also a high percentage of cutaneous photo toxicity (41%).11 Finally, brachytherapy has been studied mostly as a palliative treatment in combination with external beam radiotherapy or in a neoadjuvant setting. In combination with external beam radiotherapy, survival rates are poor, with a median OS of 12 months.12
Stereotactic body radiation therapy
Also, the role for radiotherapy in the treatment of CCA is currently not well defined. Various groups have tried to use stereotactic body radiation therapy (SBRT) to deliver high-radiation doses to control the disease locally. Most of the published studies have been retrospective (table 1).
Table 1.
Treatment outcomes of SBRT for CCA
| Author | Design | Location | Lesion no |
Fraction no |
Total dose (Gy) | 1-year local control (%) |
Median survival (months) |
Toxicity* |
| Kopek et al 14 | R | PH-CCA IH-CCA |
26 1 |
3 | 45 | 84 | 10.6 | 6 ulceration 3 stenosis |
| Tse et al 15 | P | IH-CCA | 10 | 6 | 28–48 | 65 | 15 | 2 liver enzymes 1 bowel obstruction |
| Polistina et al 16 | R | PH-CCA | 10 | 3 | 30 | 80† | 35.5 | 1 ulceration 2 stenosis |
| Barney et al 17 | R | IH-CCA PH-CCA EH-CCA |
6 3 1 |
3–5 | 45–60 | 100 | 15.5 | 1 biliary stenosis 2 liver failure |
| Momm et al 18 | R | PH-CCA | 13 | 8–16 | 32–56 | N.R. | 33.5 | 1 nausea 5 cholangitis |
| Jung et al 19 | R | IH-CCA EH-CCA |
33 25 |
1–5 | 15–60 | 85 | 10 | 2 ulceration 2 cholangitis 1 biliary stenosis 1 gastric perforation |
| Mahadevan et al 13 | R | IH-CCA PH-CCA |
31 11 |
1–5 | 10–45 | 88 | 17 | 2 duodenal ulceration 1 cholangitis 1 liver abscess |
| Tao et al 20 | R | IH-CCA | 79 | 15–30 | 50.4–75 | 81 | 30 | 3 cholangitis 2 gastric bleeding 7 biliary stenosis |
| Sandler et al 21 | R | IH-CCA EH-CCA |
6 25 |
5 | 40 | 78 | 15.7 | 2 duodenal obstruction 3 duodenal ulceration |
*Early and late toxicity, grade 3 or more.
†At 6 months.
EH-CCA, extrahepatic cholangiocarcinoma; IH-CCA, intrahepatic cholangiocarcinoma; N.R., not reported; P, prospective; PH-CCA, perihilar cholangiocarcinoma; R, retrospective; SBRT, stereotactic body radiation therapy.
SBRT has been explored as single-modality treatment in patients who are unsuitable for resection, although it has also been administered as adjuvant treatment after surgery with positive margins.13 The patient groups were almost invariably small and/or heterogeneous, which makes it hard to draw firm conclusions.13–21 Most studies did not limit number or size of lesions, with the exception of one study (maximum diameter of ≥6 cm was an exclusion criterion).16
High rates of 2-year local control (LC) after SBRT have been reported. In most studies, this was achieved in ≥72% of the patients. Median OS ranged between 10 and 35.5 months, with five studies reporting OS ≥15 months, and three reporting OS >24 months.13–21 Tao et al found a significant improvement in LC when high-radiation doses were delivered. When biologically effective doses (BEDs) were >80.5 Gy, 3-year LC was achieved in 78% vs 45% with lower doses.20
One of the difficulties for an SBRT treatment in the perihilar region is the proximity of organs at risk (OAR) like the common bile duct and duodenum. The hepatobiliary toxicity reported by other groups varied widely but was generally limited in most of the series. A slightly higher number of gastrointestinal toxicity has been reported, mainly duodenal obstruction and stenosis (table 1).13–21 This toxicity could potentially be limited by the application of strict dose–volume constraints.
Methods and analysis
Design
This study has been designed as a single-centre phase I feasibility trial. Six patients with unresectable perihilar CCA, who already received the standard treatment with systemic chemotherapy (cisplatin and gemcitabine), will be included.
The reason to design a feasibility study is that no data have been published about the delivery of SBRT in 15 fractions of 3–4.5 Gy in patients with perihilar CCA after chemotherapy. Data have been reported on patients with intrahepatic CCA treated with 15 fractions of radiotherapy, although the chemotherapy regimen and the timing of administration before or after the local treatment varied largely.20 The possibility of delivering the standard treatment without interferences due to potential toxicity caused by SBRT was the main reason to choose for an adjuvant approach instead of neoadjuvant or concomitant.
The trial follows the conventional ‘3+3’-design. First three patients will be included, after which the trial will temporarily be put on hold for 3 months. When two or three patients develop limiting toxicity (LT), the conclusion will be that the proposed risk-adapted radiotherapy protocol is not feasible and the trial will be ended. When 0 or 1 of 3 patients develops LT, 3 additional patients will be included. LT will be defined as grade 4 or more hepatobiliary toxicity related to study procedures, or grade 3 or more gastrointestinal toxicity related to study procedures, occurring in the period up to 3 months after the last SBRT administration. When 0 or 1 of these 6 patients develops LT, then the conclusion will be that the current risk-adapted radiotherapy protocol is feasible, and should be considered for further research in this patient population (ie, in a phase II trial). Otherwise, if two or more patients have limiting toxicity, the conclusion will be that the current risk-adapted radiotherapy protocol is not feasible. The most important toxicities are listed in box 1.
Box 1. Toxicity.
Gastrointestinal disorders
Duodenal or gastric obstruction/stenosis
Duodenal or gastric perforation
Duodenal or gastric ulcer
Hepatobiliary disorders
Bile duct stenosis
Perforation bile duct
Infections and infestations
Biliary tract infection
Toxicity will be determined based on symptoms, laboratory, imaging and endoscopic examinations. Limiting toxicity is defined as grade 4 or more hepatobiliary toxicity related to study procedures, or grade 3 or more gastrointestinal toxicity related to study procedures.
Study objectives
Primary study outcome
The primary objective of this study will be to determine feasibility and toxicity (according to the Common Toxicity Criteria for Adverse Events (CTCAE) V.4.03 grading system) of adding SBRT to standard chemotherapy, in patients with perihilar CCA ineligible for surgery.
Secondary study outcomes
LC defined as time from inclusion to local radiological progression. Definition of progression is based on response evaluation criteria in solid tumors (RECIST) 1.1.22
Progression-free survival defined as time from inclusion until radiological progression. Definition of progression is based on RECIST.
OS defined as time from inclusion until death from any cause.
QoL assessed by means of the EuroQol (EQ)-5D-5L (measure of health outcome in general population), and the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 (QoL specific for patients with cancer) with the supplementary module EORTC QLQ-BIL21 (specific for CCA and gallbladder cancer).
Cellular radiosensitivity, as a side track of this study. The effects of radiotherapy will be measured in normal bile duct organoids23 and CCA cancer-derived organoids (Broutier et al tumour-derived organoid cultures model primary human liver cancer in vitro, article in press) obtained from cells of brush cytology obtained during endoscopic retrograde cholangiopancreatography (ERCP). The goal is to set up assays to measure genomic mutations, cell death/apoptosis, cellular senescence and proliferative capacity after ionising radiation treatment ex vivo. In the future, these effects will be measured in organoids and will be correlated with tumour response on imaging (CT/MRI) in a large phase II trial. Prediction of response and toxicity before treatment will be the ultimately goal of this approach in the future.
Study population
Six patients with unresectable perihilar CCA after completion of standard chemotherapy with cisplatin and gemcitabine will be enrolled in this study. In order to be eligible, a subject must be discussed in a multidisciplinary liver tumour board and should meet all of the inclusion and exclusion criteria as listed in table 2. All types of biliary stents are accepted. The expected time to include the required patients for this trial will be 1 year.
Table 2.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|
|
*If less cycles have been given, patients are still eligible for this study.
†Before chemotherapy.
‡After chemotherapy.
§Within 6 weeks prior to inclusion.
AJCC, American Joint Committee on Cancer; ALT, alanine transaminase; AST, aspartate transaminase; CCA, cholangiocarcinoma; ECOG-PS, Eastern Cooperative Oncology Group performance status; FISH, fluorescence in situ hybridization; SBRT, stereotactic body radiation therapy.
Study outline
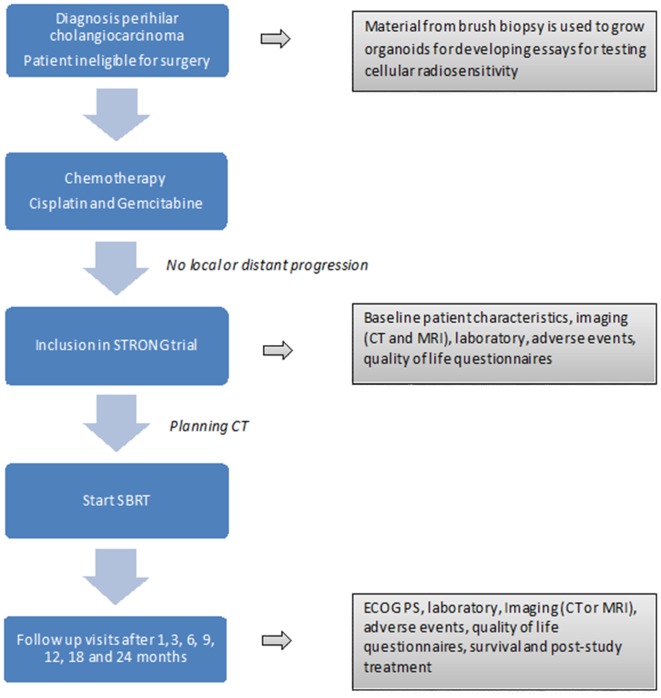
The general outline of the study procedures is presented in figure 1.
Figure 1.
Study outline. SBRT, stereotactic body radiation therapy.
Prestereotactic body radiation therapy
Chemotherapy is considered the standard treatment for unresectable perihilar CCA, and therefore will not be considered as study treatment in this trial. Cisplatin plus gemcitabine will be administered according to standard practice of the Erasmus MC Cancer Institute. Chemotherapy will be discontinued at 24 weeks (eight cycles) or earlier in case of disease progression, patient or clinician decision, or unacceptable toxic effects. Biliary obstruction per se is not considered to be disease progression in the absence of radiologically confirmed tumour progression, and treatment can be recommenced after further biliary stenting and normalisation of liver function.6 In case of unacceptable toxic effects and in absence of disease progression, the patient can proceed to SBRT without completing eight cycles of chemotherapy. In that case, no signs of progressive disease should have been observed on a chest/abdomen CT scan performed within 6 weeks before patient inclusion.
Stereotactic body radiation therapy
Treatment with SBRT will start preferably within 6 weeks after the last chemotherapy course. However, if due to toxicity or other medical or personal reasons the start of the treatment has to be postponed, the time to start can be expanded till a maximum of 12 weeks after the last course of chemotherapy.
We will use a risk-adapted dose prescription for delivering the highest possible dose to the tumour, using 15 fractions of 3–4, 5 Gy, while not exceeding widely accepted dose constraints in the surrounding OAR (tables 3 and 4). This approach has already been tested with favourable outcome and limited biliary toxicity in a multicentre retrospective study for intrahepatic CCA.20 The same radiotherapy protocol (dose and fractionation) is currently being tested in a prospective phase III trial between chemotherapy and chemotherapy combined with radiotherapy in patients with unresectable intrahepatic CCA (NRG-GI001). To the best of our knowledge, this approach for perihilar CCA has not been published yet.
Table 3.
Organs at risk constraints
| Organ at risk | Hard constraints |
| Healthy liver | ≥700 mL liver-GTV, dose <25.5 Gy26
If cirrhosis is present: NTCP liver-GTV ≤5%27 and >800 mL liver-GTV, dose <31.5 Gy28 |
| Stomach | Max point dose <57 Gy29
Volume receiving ≥41 Gy should be ≤5 cc |
| Duodenum Small and large bowel (when needed combined in one structure) |
Max point dose <57 Gy29
Volume receiving ≥41 Gy should be ≤5 cc |
| Oesophagus | Max point dose ≤50.25 Gy30 |
| Spinal cord | Max point dose ≤33.8 Gy26 |
| Kidney | 2/3 right kidney <25.5 Gy26 |
Table 4.
Organ at risk objectives
| Organ at risk | Objectives |
| Central biliary tract | Less than 0.5 cc ≥70 Gy (NRG-GI001 - http://www.cancer.gov/clinicaltrials) VBED1040<37 cc and VBED1030<45 cc31 |
| Heart | Max dose <57 Gy (RTOG 1112 - http://www.cancer.gov/clinicaltrials) |
| Gallbladder | Max dose <86.7 Gy (RTOG 1112- http://www.cancer.gov/clinicaltrials) |
| Skin (external contour) | Less than 0.5 cc ≥50.25 Gy (RTOG 1112 - http://www.cancer.gov/clinicaltrials) |
RTOG, Radiation Therapy Oncology Group.
Marker implantation
A tumour-tracking technique (Synchrony-Cyberknife, Accuray, Sunnyvale, California, USA) will be applied for daily positioning and during dose delivery. Therefore, implantation of fiducials is compulsory. For perihilar CCA, fiducials should be implanted in the liver and not in the tumour to avoid the risk of tumour seeding. A distance of around 2.0 cm from the tumour edge is recommended. The procedure will be performed by an experienced interventional radiologist. International normalised ratio (INR) should be <2.0, and platelets should be ≥50×109/L. We will plan around 1 week (minimum of 5 and maximum of 10 days) between the implantation of the fiducials and the treatment preparation (planning CT). Patients should remain hospitalised during at least 2–3 hours after the implantation in order to detect and treat unexpected complications as soon as possible. In case of lymph node involvement, no fiducials will be implanted in the affected nodes.
Tumour delineation
The gross target volume (GTV) is defined in a contrast-enhanced CT acquired in expiration and in a hepatic venous phase. An arterial phase CT with bolus-tracking technique is also performed since valuable complementary information from this phase could be valuable to better depict the tumour. The use of MRI to support the tumour delineation is recommended. In case that enlarged lymph nodes (N1) have to be considered as a target for SBRT, the venous phase of the planning CT in expiration will also be used for the delineation. No additional margin will be added around the GTV to generate the clinical target volume for both tumour and lymph nodes.
Margins
The information acquired from a 4DCT scan and from the inspiration/expiration CT will be used to establish the margin around the GTV to generate the planning target volume (PTV). This margin should ensure that despite geometrical uncertainties (ie, imaging artefacts in the planning CT scan due to respiratory tumour motion, interfraction motion of the tumour, uncertainty in the set-up, etc), the full GTV is irradiated with an adequate dose with a very high probability.
Planning protocol
Efforts should be made to deliver a BED >80.5 Gy to the tumour, since a multicentre retrospective study of intrahepatic CCA demonstrated a significant improvement in LC depending on the BED (3y 45% for BED <80.5 Gy vs 78% for BED >80.5 Gy).20 In case the tumour is located very close/adjacent to OAR as the duodenum, stomach, oesophagus or bowel, it may be impossible to deliver such high doses to the periphery of most of the tumour, and therefore, lower doses at the periphery are allowed in these cases.
Any plan delivered to a patient should adhere to the imposed OAR hard constraints (table 3). Within these constraints, ideally the full PTV is irradiated with a dose of ≥67.5 Gy (15×4.5 Gy). Due to the hard constraints and the objectives for the OARs, this ideal PTV dose may not always be achievable. In that case, compromises in PTV dose delivery can be made. First of all, the PTV coverage may be reduced, that is, only 95% of the PTV may receive ≥67.5 Gy. Second, instead of delivering 67.5 Gy (15×4.5 Gy), a dose of 60 Gy (15×4 Gy), 52.5 Gy (15×3.5 Gy) or even 45 Gy (15×3 Gy) can be chosen. An effort should be made to deliver at least 60 Gy (BED >80.5 Gy) to a large portion of the PTV without violating OAR constraints.
Fractionation and daily imaging
The total dose is delivered in 15 fractions. Time between fractions should be 24 hours (in case of a weekend in between it will be 72 hours). Effort should be made to deliver the treatment without gaps.
In order to evaluate the relationship between tumour and OAR in this perihilar location, a CT scan before and after treatment in expiration phase will be performed in treatment position the first day and on days 3, 6, 9, 12 and 15 during treatment. No intravenous contrast will be used.
Post-SBRT follow-up
Follow-up visits will be scheduled at 1, 3, 6, 9, 12, 18 and 24 months after treatment. At every visit, an MRI or CT scan will be made to detect local or distant disease progression. Also, toxicity and performance score will be scored every visit. Patients will be asked to fill out QoL questionnaires (EuroQol EQ-5D-5L, EORTC QLQ-C30 and EORTC QLQ- BIL21) at most visits. For further detailed information, see table 5. If a patient is still alive after 2 years, follow-up will be continued by the medical oncologist according current clinical practice.
Table 5.
Schedule of events
| Eligibility check | Written informed consent | Medical history | Comorbidity | ECOG PS | Laboratory* | CT/MRI† | Adverse events‡ | QOL | Survival and poststudy treatment | |
| Standard treatment (chemotherapy) 1–8 courses. No progressive disease | ||||||||||
| ≤6 weeks | X | X | X | X | X | X | X | X | X | |
| Experimental add on treatment (SBRT) | ||||||||||
| +1 month | X | X | X | X | X | X | ||||
| +3 months | X | X | X | X | X | X | ||||
| +6 months | X | X | X | X | X | X | ||||
| +9 months | X | X | X | X | X | X | ||||
| +12 months | X | X | X | X | X | X | ||||
| +18 months | X | X | X | X | X | |||||
| +24 months | X | X | X | X | X | X | ||||
*Laboratory assessments should include albumin, bilirubin, alkaline phosphatase, AST, ALT, gamma-glutamyl transferase (GGT), haemoglobin (Hb), leucocytes, platelets and CA-19.9. Notice that CA-19.9 should only be assessed during follow-up if indicated, that is, if elevated at baseline.
†Radiology report should include tumour measurement, tumour measurements should be performed according to RECIST criteria.
‡CTCAE V.4.03 should be applied for grading toxicity.
CTCAE, Common Toxicity Criteria for Adverse Events; QOL, quality of life; SBRT, stereotactic body radiation therapy.
Ancillary study: evaluating cellular radiosensitivity in patient-derived organoid models
We will grow organoids from tumour and bile duct cells collected by brush biopsies23 (Broutier et al tumour-derived organoid cultures model primary human liver cancer in vitro, article in press). For this purpose, a second brush will be obtained during the same procedure while the first brush is taken (just directly after the first one) and only for patients where a brush biopsy is considered needed as part of the diagnostic work-up. We will set up assays to measure cell survival (clonogenic assays, H&E staining of organoids), apoptosis (terminal deoxynucleotidyl transferase dUTP nick and labeling (TUNEL) staining), accumulation of DNA repair proteins on DNA double-strand breaks (gamma-H2AX, 53BP1 and RAD51 foci) and repair of the DNA damage at various time points after irradiation (loss of these foci after 24–48 hours of incubation). In addition to the functional assays, organoid cultures are also ideal sources of tumour material, such as DNA for mutation analysis and RNA for gene expression studies.24
Data analysis
This trial will be performed as a feasibility study and will focus on toxicity until 3 months after SBRT treatment. The number of patients with LT as defined before will be determined. If two or more patients have LT, the conclusion will be that the regimen is not feasible. Otherwise the conclusion will be that the regimen warrants further research in this population.
In addition, the analysis of toxicity will be done by tabulation of the incidence of adverse events CTCAE grades 3 and 4. Adverse events will be summarised by worst CTCAE grade. Demographics of the patients at study entry will be recorded, and presented as percentages in case of discrete variables, or by median and range in case of continuous variables. All patients with the baseline and at least one follow-up QoL questionnaire, separately for QLQ-C30, QLQ-BIL21 and EuroQoL-5D, will be included in the analysis. The repeated measures will be analysed using analysis of variance models. The Kaplan-Meier method will be used to estimate LC, progression-free survival and OS.
Patient and public involvement
While designing the study, our first priority was the patients’ well-being. Although we did not involve patients in the design of the trial, all information about the study is available on the website of the Dutch Hepato & Cholangio Carcinoma Group (www.dhcg.org). During the development phase, the study was discussed several times within this multidisciplinary group. A final report of the trial will also be placed at the website for patient information. At any time, participants can be informed about study outcomes through the principal investigator.
Ethics and dissemination
The STRONG trial is registered on ClincalTrials.gov (ID: NCT03307538). The results of this study will be published in an academic journal, and presented at national and international conferences.
Discussion
The STRONG trial is designed to assess feasibility and toxicity of adding SBRT to standard chemotherapy in patients with inoperable perihilar CCA. Currently, only a few prospective studies are available on the use of SBRT for treating patients with CCA in the perihilar region. These studies report promising results for LC (≥72% at 2 years) and median OS (up to 35 months), with low toxicity rates. However, the exact treatment approach (combination with chemotherapy, chemotherapy scheme, timing, SBRT fractionation) varied widely.13–21 The scarce available results suggest that the combination of chemotherapy and SBRT may improve disease control above SBRT alone.
We chose a more fractionated scheme than the other studies on SBRT for perihilar tumours because of the proximity of OAR like duodenum and bile duct to the tumour. By using 15 fractions, instead of fewer, we hope to reach an acceptable coverage of the PTV with a BED of more than 80.5 Gy, and at the same time respect the dose constraints for the OAR’s. Acceptable results have been published with this fractionating scheme for intrahepatic CCA.20
In this study, we will encounter some technical challenges and uncertainties. First of all is the assessment of the breathing motion of tumours located in the perihilar region. Since we use the Synchrony-Cyberknife system for tumour tracking, fiducial markers will have to be implanted close to the tumour. These markers will be placed in the liver in the proximity of the tumour and not in the tumour itself to avoid tumour seeding. Second, there is little known about the interfraction and intrafraction motion of OAR located in the vicinity of the perihilar region and the correlation with the tumour motion. If present, involved lymph nodes may be situated at a certain distance of the tumour. Again, motion assessment and correlation with tumour motion will be another point that should be addressed within this study. In order to measure variations in interfraction and intrafraction motion, a CT scan in expiration phase before and after treatment will be performed in treatment position the first day and on days 3, 6, 9, 12 and 15 during treatment.
Because of these technical uncertainties in combination with the experimental fractionation scheme for tumours located in the perihilar region, the first step is to complete this feasibility trial with just six patients. Since this small number results in limitations for interpreting results on disease control and QoL, our aim is to proceed to a large phase II trial if the treatment turns out to be feasible.
Supplementary Material
Footnotes
Contributors: All authors contributed to the design of the study protocol and approved the final manuscript. AMR and MSK: principal investigators, initiators of the trial. BJMH: medical physics aspects. BvdH: statistical design and data analysis. DCvG and LJWvdL: molecular genetics side study. FEJAW: radiological support. BGK: surgical aspects. FALME: systemic therapy advice. DS and J-WP: endoscopic and gastroenterological procedures.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Ethics approval for the study was granted 31 August 2017 by the Medical Ethics Committee of Erasmus MC Rotterdam, the Netherlands (ID: NL 60588.078.17).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Aitken KL, Hawkins MA. The role of radiotherapy and chemoradiation in the management of primary liver tumours. Clin Oncol 2014;26:569–80. 10.1016/j.clon.2014.05.016 [DOI] [PubMed] [Google Scholar]
- 2. Shinohara ET, Mitra N, Guo M, et al. . Radiotherapy is associated with improved survival in adjuvant and palliative treatment of extrahepatic cholangiocarcinomas. Int J Radiat Oncol Biol Phys 2009;74:1191–8. 10.1016/j.ijrobp.2008.09.017 [DOI] [PubMed] [Google Scholar]
- 3. Weiss MJ, Cosgrove D, Herman JM, et al. . Multimodal treatment strategies for advanced hilar cholangiocarcinoma. Langenbecks Arch Surg 2014;399:679–92. 10.1007/s00423-014-1219-1 [DOI] [PubMed] [Google Scholar]
- 4. Mansour JC, Aloia TA, Crane CH, et al. . Hilar cholangiocarcinoma: expert consensus statement. HPB 2015;17:691–9. 10.1111/hpb.12450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blechacz B. Cholangiocarcinoma: Current Knowledge and New Developments. Gut Liver 2017;11:13–26. 10.5009/gnl15568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Valle J, Wasan H, Palmer DH, et al. . Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 2010;362:1273–81. 10.1056/NEJMoa0908721 [DOI] [PubMed] [Google Scholar]
- 7. Eckmann KR, Patel DK, Landgraf A, et al. . Chemotherapy outcomes for the treatment of unresectable intrahepatic and hilar cholangiocarcinoma: a retrospective analysis. Gastrointest Cancer Res 2011;4(5-6):155–60. [PMC free article] [PubMed] [Google Scholar]
- 8. Coelen RJS, Vogel JA, Vroomen L, et al. . Ablation with irreversible electroporation in patients with advanced perihilar cholangiocarcinoma (ALPACA): a multicentre phase I/II feasibility study protocol. BMJ Open 2017;7:e015810 10.1136/bmjopen-2016-015810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Melenhorst MC, Scheffer HJ, Vroomen LG, et al. . Percutaneous Irreversible Electroporation of Unresectable Hilar Cholangiocarcinoma (Klatskin Tumor): A Case Report. Cardiovasc Intervent Radiol 2016;39:117–21. 10.1007/s00270-015-1126-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wu TT, Li WM, Li HC, et al. . Percutaneous intraductal radiofrequency ablation for extrahepatic distal cholangiocarcinoma: A method for prolonging stent patency and achieving better functional status and quality of life. Cardiovasc Intervent Radiol 2017;40:260–9. 10.1007/s00270-016-1483-2 [DOI] [PubMed] [Google Scholar]
- 11. Wagner A, Denzer UW, Neureiter D, et al. . Temoporfin improves efficacy of photodynamic therapy in advanced biliary tract carcinoma: A multicenter prospective phase II study. Hepatology 2015;62:1456–65. 10.1002/hep.27905 [DOI] [PubMed] [Google Scholar]
- 12. Mattiucci GC, Autorino R, Tringali A, et al. . A Phase I study of high-dose-rate intraluminal brachytherapy as palliative treatment in extrahepatic biliary tract cancer. Brachytherapy 2015;14:401–4. 10.1016/j.brachy.2014.12.002 [DOI] [PubMed] [Google Scholar]
- 13. Mahadevan A, Dagoglu N, Mancias J, et al. . Stereotactic Body Radiotherapy (SBRT) for Intrahepatic and Hilar Cholangiocarcinoma. J Cancer 2015;6:1099–104. 10.7150/jca.13032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kopek N, Holt MI, Hansen AT, et al. . Stereotactic body radiotherapy for unresectable cholangiocarcinoma. Radiother Oncol 2010;94:47–52. 10.1016/j.radonc.2009.11.004 [DOI] [PubMed] [Google Scholar]
- 15. Tse RV, Hawkins M, Lockwood G, et al. . Phase I study of individualized stereotactic body radiotherapy for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol 2008;26:657–64. 10.1200/JCO.2007.14.3529 [DOI] [PubMed] [Google Scholar]
- 16. Polistina FA, Guglielmi R, Baiocchi C, et al. . Chemoradiation treatment with gemcitabine plus stereotactic body radiotherapy for unresectable, non-metastatic, locally advanced hilar cholangiocarcinoma. Results of a five year experience. Radiother Oncol 2011;99:120–3. 10.1016/j.radonc.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 17. Barney BM, Olivier KR, Miller RC, et al. . Clinical outcomes and toxicity using stereotactic body radiotherapy (SBRT) for advanced cholangiocarcinoma. Radiat Oncol 2012;7:67 10.1186/1748-717X-7-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Momm F, Schubert E, Henne K, et al. . Stereotactic fractionated radiotherapy for Klatskin tumours. Radiother Oncol 2010;95:99–102. 10.1016/j.radonc.2010.03.013 [DOI] [PubMed] [Google Scholar]
- 19. Jung DH, Kim MS, Cho CK, et al. . Outcomes of stereotactic body radiotherapy for unresectable primary or recurrent cholangiocarcinoma. Radiat Oncol J 2014;32:163–9. 10.3857/roj.2014.32.3.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tao R, Krishnan S, Bhosale PR, et al. . Ablative radiotherapy doses lead to a substantial prolongation of survival in patients with inoperable intrahepatic cholangiocarcinoma: a retrospective dose response analysis. J Clin Oncol 2016;34:219–26. 10.1200/JCO.2015.61.3778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sandler KA, Veruttipong D, Agopian VG, et al. . Stereotactic body radiotherapy (SBRT) for locally advanced extrahepatic and intrahepatic cholangiocarcinoma. Adv Radiat Oncol 2016;1:237–43. 10.1016/j.adro.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eisenhauer EA, Therasse P, Bogaerts J, et al. . New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 23. Huch M, Gehart H, van Boxtel R, et al. . Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell 2015;160:299–312. 10.1016/j.cell.2014.11.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Blokzijl F, de Ligt J, Jager M, et al. . Tissue-specific mutation accumulation in human adult stem cells during life. Nature 2016;538:260–4. 10.1038/nature19768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Welling TH, Feng M, Wan S, et al. . Neoadjuvant stereotactic body radiation therapy, capecitabine, and liver transplantation for unresectable hilar cholangiocarcinoma. Liver Transpl 2014;20:81–8. 10.1002/lt.23757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schefter TE, Kavanagh BD, Timmerman RD, et al. . A phase I trial of stereotactic body radiation therapy (SBRT) for liver metastases. Int J Radiat Oncol Biol Phys 2005;62:1371–8. 10.1016/j.ijrobp.2005.01.002 [DOI] [PubMed] [Google Scholar]
- 27. Dawson LA, Eccles C, Craig T. Individualized image guided iso-NTCP based liver cancer SBRT. Acta Oncol 2006;45:856–64. 10.1080/02841860600936369 [DOI] [PubMed] [Google Scholar]
- 28. Son SH, Choi BO, Ryu MR, et al. . Stereotactic body radiotherapy for patients with unresectable primary hepatocellular carcinoma: dose-volumetric parameters predicting the hepatic complication. Int J Radiat Oncol Biol Phys 2010;78:1073–80. 10.1016/j.ijrobp.2009.09.009 [DOI] [PubMed] [Google Scholar]
- 29. Kavanagh BD, Pan CC, Dawson LA, et al. . Radiation dose-volume effects in the stomach and small bowel. Int J Radiat Oncol Biol Phys 2010;76(3 Suppl):S101–7. 10.1016/j.ijrobp.2009.05.071 [DOI] [PubMed] [Google Scholar]
- 30. Kong FM, Ritter T, Quint DJ, et al. . Consideration of dose limits for organs at risk of thoracic radiotherapy: atlas for lung, proximal bronchial tree, esophagus, spinal cord, ribs, and brachial plexus. Int J Radiat Oncol Biol Phys 2011;81:1442–57. 10.1016/j.ijrobp.2010.07.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Toesca DA, Osmundson EC, Eyben RV, et al. . Central liver toxicity after SBRT: An expanded analysis and predictive nomogram. Radiother Oncol 2017;122:130–6. 10.1016/j.radonc.2016.10.024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.