Abstract
OBJECTIVES
There is a seasonal variation in the incidence of some infectious diseases. We analyzed the impact of influenza season (IS) on duration of stay (DOS) and some other characteristics of patients with community-acquired pneumonia (CAP).
MATERIALS AND METHODS
In our retrospective cohort study, we analyzed data of 369 patients with CAP.
RESULTS
The mean patient age was 65.5±16.69 years, and 267 (72.4%) patients were male. There was no difference between patients with CAP admitted to hospital and intensive care unit during IS and non-influenza season (NIS) with respect to age, mortality, and DOS. There was no difference in leukocyte and neutrophil counts, C-reactive protein level, and erythrocyte sedimentation rate in different seasons. Although most comorbid disease rates were similar, only cancer, especially lung cancer, was more prevalent in NIS. Bilateral CAP confirmed using thorax computed tomography was more frequent in IS.
CONCLUSION
Although more patients with bilateral pneumonias were hospitalized in IS, DOS was not different between IS and NIS.
Keywords: Influenza, community-acquired pneumonia, hospitalization duration, season
INTRODUCTION
Seasonal variation in occurrence is a common feature of many infectious diseases. Studies on seasonal variation contribute to healthcare planning and analysis of infections.
Seasonal variation in occurrence of community-acquired pneumonia (CAP) has epidemiological significance. Bacterial, viral, or other pathogens may cause CAP. Some of these pathogens, especially respiratory viruses, exhibit seasonal variation, resulting in a higher incidence of CAP in winter and spring and a lower incidence in summer and autumn [1]. Hence, incidences of and mortality associated with sepsis and severe sepsis are seasonal and highest during winter, owing to respiratory sepsis [2].
Influenza is one of the most significant seasonal diseases [3]. It is a public health problem that affects 5%–20% of the world population. Annual epidemics result in approximately 3–5 million cases of severe illness and approximately 250,000–500,000 deaths worldwide. Diagnosis and treatment of patients with CAP are crucial during influenza epidemics. Hospitalization and death mainly occur among high-risk groups [4]. Elderly people, those with comorbidities, and pregnant women are high-risk patients. Influenza epidemics occur annually during autumn and winter in temperate regions [5]. Typical and atypical bacteria and viruses are the cause of primary CAP. However, it may be difficult to distinguish seasonal influenza pneumonia from bacterial pneumonia [6].
Outbreak of influenza increases hospital admissions due to pneumonia. Longer duration of stay (DOS) in hospital may lead to problems in the allocation of beds in health care institutions and result in higher health care costs. Determining DOS in hospital for patients with CAP in influenza season (IS) will help in efficient management of resources. Although it is difficult to precisely document primary influenza infection, some characteristics of CAP may be different in IS. The aim of our study was to determine the duration of hospital stay for patients with CAP admitted during “IS” and to compare it with the remaining period in which influenza infection is rare.
MATERIALS AND METHODS
This is a retrospective cohort study on DOS of patients with CAP hospitalized in the pulmonary diseases ward of a tertiary chest diseases and surgery training hospital. We retrospectively examined all computer-based data of patients with CAP from January 2010 to March 2015 for study variables. Ethics committee approval was not required for this retrospective study, and patient’s confidentiality was maintained.
Variables
Age, gender, comorbid diseases, age ≥65 years, duration of hospital and intensive care unit (ICU) stays, blood leukocyte and neutrophil counts, C-reactive protein levels, sputum cultures, chest radiographs, and mortality were analyzed.
We compare these variables with respect to the “season” in which patients were hospitalized. Each year is divided into “IS” and “non-influenza season” (NIS). IS is defined as the period between December 1 and April 30, and NIS is defined as period between May 1 and November 30. We derived these time intervals from data from a study by Puig-Barbera [4] and an influenza surveillance report in Turkey [7].
Patients
CAP was defined using the following:
Pneumonic infiltration in chest X-rays and one major criteria: cough, sputum expectoration, and fever or two minor criteria: dyspnea, pleuritic chest pain, physical examination findings compatible with consolidation, and white blood cell count >12000/mm3
The authors reviewed the files from the patient data system of the hospital and recorded the patients with a diagnosis of pneumonia (ICD code J18). One pulmonologist reviewed chest X-rays for the diagnosis. Patients aged <16 years, cases with bronchiectasis, patients discharged from hospital on their own will, immunosuppressed patients, patients with hospital-acquired pneumonia, and patients with healthcare-related pneumonia were excluded.
Data Analysis
Data were recorded and analyzed using the SPSS (Statistical Packagefor Social Sciences) version 18.0 (IBM Corp.; Armonk, NY, USA) program. Continuous variables (mean, standard deviation, median, and minimum and maximum values) and categorical variables (frequencies and percentages) were presented. Independent variables with normal distributions were analyzed using independent samples t-test; independent variables with non-normal distributions are analyzed using Mann-Whitney U test. Categorical variables were presented as frequencies and percentages in cross tables, and group differences for categorical values were analyzed using Χ2 test. Type 1 error is α=0.05, and it was tested in two ways. A p<0.05 was considered to indicate significance.
RESULTS
A total of 1170 patients were hospitalized at our clinic during the study period; 427 patients were diagnosed with pneumonia. We excluded 44 patients with hospital-acquired pneumonia, 10 patients with immunosuppression, and 4 patients with healthcare-related pneumonia. Overall, 369 patients with CAP were enrolled in the study. Table 1 shows their demographic and clinical characteristics.
Table 1.
Demographic features of patients with CAP (n=369)
| Age (years) [mean±SD (min–max)] | 65.5±16.69 (16–102) |
| Duration of stay in hospital (days) [mean±SD (min–max)] | 11.96±8.57 (1–82) |
| Duration of stay in ICU (days) [mean±SD (min–max)] | 8.15±8.56 (1–40) |
| Leukocyte count (×103/μL) [mean±SD (min–max)] | 13307.1±7917.9 (1690–85200) |
| Neutrophil count (×103/μL) [mean±SD (min–max)] | 97555.4±5928.4 (650–40100) |
| CRP (mg/dL) [mean±SD (min–max)] | 15.7±12.4 (0.32–55.3) |
| Erythrocyte sedimentation rate (mm/h) [mean±SD (min–max)] | 59.87±30.4 (2–140) |
| Number of patients aged ≥65 years [n (%)] | 205 (56) |
| Males [n (%)] | 267 (72) |
| ICU admission [n (%)] | 20 (5) |
| Mortality [n (%)] | 28 (8) |
| Comorbid diseases [n (%)] | 307 (83) |
| Availability of thorax CT [n (%)] | 275 (75) |
| Availability of sputum culture [n (%)] | 180 (49) |
| Availability of hemoculture [n (%)] | 79 (21) |
CAP: community-acquired pneumonia; ICU: intensive care unit; CRP: C-reactive protein; CT: computed tomography
In total, 247 (66.9%) patients showed pneumonic infiltration, 10 (2.7%) showed empyema findings, and 17 (4.6%) showed lung abscess in their thorax computed tomography (CT). Overall, 109 (29.5%) cases were bilateral and 260 (70.5%) were unilateral.
We obtained sputum cultures of 180 (48.8%) patients, and growth was observed in 166 (91.7%) cultures; 163 (90.1%) and 3 (1.7%) cultures showed the growth of a single and two agents, respectively. No growth was observed in 15 (8.3%) cultures. Figure 1 shows the growing microorganisms in sputum cultures. We collected samples for hemoculture from 79 (21.4%) patients, and growth was observed in 15 (19%) of them. Staphylococcus spp. grew in 11 hemocultures, and Bacillus, Corynebacterium, diphtheroid bacilli, and Streptococcus pneumoniae grew in each of the remaining four hemocultures.
Figure 1.
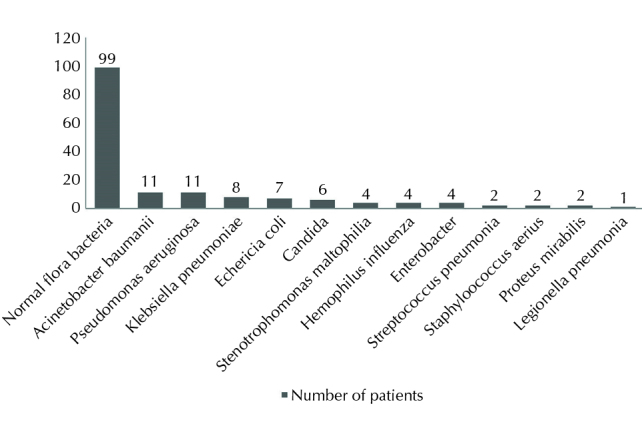
Microorganisms detected in sputum cultures
Overall, 197 (53.4%) patients were hospitalized during IS and 172 (46.6%) were hospitalized during NIS. Table 2 shows their features. DOS in hospital or ICU did not differ among the patients in IS. Furthermore, there were no differences regarding age, age≥65 years, gender, and mortality. No association was observed between season and blood test or sputum culture results.
Table 2.
Variables according to the season
| IS | NIS | p | |
|---|---|---|---|
| Mean age±SD | 66.79±16.01 | 64.04±17.37 | 0.114 |
| Number of patients aged ≥65 years [n (%)] | 118 (59.9) | 87 (50.6) | 0.072 |
| Gender (male) [n (%)] | 138 (70.1) | 129 (75) | 0.289 |
| Mortality [n (%)] | 14 (7.1) | 14 (7.1) | 0.86 |
| Median duration of hospitalization (days) | 10.0 (1–50) | 9.0 (1–82) | 0.676 |
| Median duration of ICU stay (days) | 5.0 (1–10) | 6.0 (2–40) | 0.206 |
| Median leukocyte count (×103/μL) | 11400 (1690–56100) | 11900 (1900–85200) | 0.755 |
| Median neutrophil count (×103/μL) | 8360 (850–37100) | 8410 (650–40100) | 0.868 |
| Mean CRP (mg/dL) | 15.59±12.31 | 15.79±12.5 | 0.895 |
| Mean ESR±SD (mm/h) | 57±30 | 63±30 | 0.068 |
| Sputum culture positivity [n (%)] | 82 (49.9) | 84 (50.6) | 0.83 |
| Blood culture availability [n (%)] | 30 (15.2) | 49 (28.5) | 0.002* |
| Blood culture positivity [n (%)] | 7 (23.3) | 8 (16.3) | 0.63 |
| Pneumonia in thorax CT [n (%)] | 130 (66) | 117 (68) | 0.679 |
| Bilateral localization in thorax CT [n (%)] | 67 (34) | 42 (24.4) | 0.044* |
| Empyema [n (%)] | 4 (2) | 6 (3.5) | 0.524 |
| Lung abscess [n (%)] | 6 (3) | 11 (6.4) | 0.200 |
(Significance: p<0.05) CU: intensive care unit; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; CT: computed tomography; IS: influenza season; NIS: non-influenza season
A thorax CT of patients with CAP in IS showed mostly bilateral lesions (p=0.044). Comorbid disease frequency was similar in both seasons (p=0.387). The frequency of cancer (p=0.027), especially that of lung cancer (p=0.007), was high in NIS. Table 3 lists the comorbid diseases.
Table 3.
Comorbidities according to the season
| IS [n (%)] | NIS [n (%)] | p | |
|---|---|---|---|
| COPD | 81 (41.1) | 59 (34.3) | 0.178 |
| Diabetes mellitus | 36 (18.3) | 22 (12.8) | 0.149 |
| Chronic renal failure | 9 (4) | 12 (7) | 0.441 |
| Congestive heart failure | 28 (14.2) | 21 (12.2) | 0.680 |
| Neurological disorders | 27 (13.7) | 26 (15.1) | 0.813 |
| Hypertension | 37 (18.8) | 29 (16.9) | 0.631 |
| Asthma | 8 (4.1) | 2 (1.2) | 0.113 |
| Carcinoma | 18 (9.1) | 30 (17.4) | 0.027* |
| Lung carcinoma | 8 (4.1) | 21 (12.2) | 0.007* |
| Prostate carcinoma | 4 (2) | 2 (1.2) | 0.689 |
| Larynx carcinoma | 2 (1) | 6 (3.5) | 0.153 |
(Significance: p<0.05) COPD: chronic obstructive pulmonary disease; IS: influenza season; NIS: non-influenza season
DISCUSSION
Hospital admissions due to pneumonia increase during influenza outbreaks. Longer DOS may lead to problems in the allocation of beds. No study has so far examined DOS of patients with CAP during IS and NIS The aim of our study was to determine the duration of hospital stay for patients admitted with CAP during IS. We found no difference in DOS between IS and NIS.
The appropriate duration of treatment for patients with CAP varies. This duration is 10.8–16 days in Turkey [8]. Mean DOS of our patients was consistent with that reported in previous studies. It is recommended to determine the responsible pathogen for CAP treatment [9,10]. However, diagnostic tests are optional for hospitalized patients without severe CAP. Most hospitalized patients with CAP are treated empirically with no etiological diagnosis. Diagnostic yield of microbiological tests is low, and pathogen detection rates vary [11]. In addition, identifying the etiological agent is confounded by limitations in diagnostic tests and by poor-quality specimens contaminated with bacteria colonizing the upper airway [6].
Influenza surveillance studies are performed to determine the circulating influenza virus type. However, viruses other than influenza virus (respiratory syncytial virus, human metapneumovirus, human parainfluenza virus, and coronavirus) as well as typical and atypical bacteria are the responsible pathogens during influenza season. In addition, laboratory facilities are mostly inefficient, and pathogens may not be determined. Consequently, influenza tests are not performed in 25%–60% of patients hospitalized for influenza, even in the United States. Furthermore, low-sensitivity tests lead to false-negative results [12]. Influenza either remains undiagnosed or under coded in a substantial proportion of critical illnesses [13]. In the Netherlands, only 40% of patients admitted to ICU for CAP were tested for influenza [14]. It is difficult to detect some pathogens using laboratory tests [6]. In addition, influenza virus acts synergistically with certain bacteria to increase the infectivity, and influenza is often complicated by bacterial superinfection. The rate of mixed viral-bacterial infection is 20%, and CAP caused by mixed infections is associated with more severe symptoms and longer hospitalization than that caused by bacterial infection alone [15].
In as much as one-third of pneumococcal pneumonia cases, atypical bacterial pathogens coinfect patients with CAP. New polymerase chain reaction tests are now available for detecting Chlamydia pneumoniae and Mycoplasma pneumoniae as well as 14 respiratory tract viruses. These tests are rapid, sensitive, and specific [16]. Use of such tests can aid in the rapid diagnosis of viral pneumonia and reduce the unnecessary use of antibacterial agents, but they are not available in most centers. Therefore, it is usually not possible to distinguish whether the patient had influenza infection or any other infection before CAP in daily practice. Clinicians usually treat patients with CAP empirically with no etiological diagnosis.
Blood cultures are positive in only 3%–14% of patients hospitalized with CAP [6]. In our daily practice, we collect blood samples for cultures from patients with high fever. In our study, more samples for blood cultures were obtained in NIS than in IS. There might be more patients with pneumonia with high fever in NIS and more cases of atypical clinical presentation during IS. However, blood culture positivity did not differ between both the seasons.
Community-acquired pneumonia is more prevalent in elderly patients and risk of its occurrence increases with age [6]. Similarly, influenza affects older age groups more frequently. In a study conducted in Germany, children aged <18 years and people aged >60 years had the highest rate of influenza-related hospitalizations [17]. Relative frequency of influenza-related hospitalizations was highest among patients aged >60 years (5.5%). Patients aged >60 years stayed in hospital for a mean of 13.1 days, whereas children aged 2–6 years stayed in hospital for a mean of 6.6 days for influenza-related hospitalization. That study was performed based on a population database including 4 million people. Our study included 55.6% patients aged >65 years, and we did not observe any increase in the number of older patients in IS. However, our study was conducted including limited number of patients and was based on the data of a tertiary hospital.
Chest X-ray is generally adequate for clinical care of patients with CAP. If the clinical presentation favors pneumonia but X-ray is negative, a CT scan can be performed as it has a higher sensitivity and accuracy than chest X-rays [18]. Chest X-rays were performed for all of our study patients. There were more thorax CT-confirmed patients with pneumonia in IS than in NIS, and these thorax CTs showed mostly bilateral lesions. During IS, there were more incidences of primary influenza pneumonia or atypical pneumonia; they appear as a ground-glass attenuation on X-ray and may be difficult to identify using only chest X-rays. Atypical pneumonia incidence was more predominant and the main radiological findings were ground-glass opacities during IS. For these reasons chest x-ray is insufficient diagnostic tool. In addition, influenza might complicate and facilitate severe bilateral pneumonia.
Although chronic obstructive pulmonary disease (COPD) is an important risk factor for adverse outcomes with influenza infection, COPD rate was not higher in IS than in NIS in our study. This might be because COPD exacerbations were often associated with bacterial agents. Furthermore, patients might be externalized after their pneumonia resolves, and malignancies might be diagnosed in the follow-up period as an outpatient. Only carcinoma rate, especially lung cancer rate, was higher in NIS. This may be due to the relative increase in hospitalization of patients with pneumonia in IS. Furthermore, our hospital is a tertiary chest disease center, and patients with other malignancies are less frequently hospitalized.
Annual surveillance studies show that the timeline of IS changes every year. This minimal change occurs in terms of weeks. We analyzed data from previous studies and defined “IS” in Turkey as the common period in all years: December 1–April 30 [4,7]. It would be more precise to define IS on a weekly basis and perform analysis in terms of the weeks during which the patients were hospitalized
Our study has several limitations. As it is a retrospective study, data collection may be defective. We could not perform tests for viral and atypical agents. We could not precisely distinguish primary influenza pneumonia from secondary bacterial pneumonia. Thus, it was not clear whether our bacterial pneumonia cases were secondary to influenza. Since information regarding serologic diagnoses was limited and because of our focus on culture results, we likely underestimated the incidence of atypical pathogens. However, the aim was to determine whether DOS and other parameters changed in IS irrespective of the etiological agent. DOS in hospital might be affected by multiple factors, such as socioeconomical factors. Varying discharge practices of physicians during the study period might also affect the length of hospital stay. Another confounding factor is air pollution. Air pollution rate is higher during IS. Further studies may enlighten the relationship between hospital admissions in IS and air pollution. Our study was conducted in a single tertiary hospital, and there might be difficulties in generalizing our results to other centers.
In conclusion, an influenza outbreak takes place every year, causing an increase in hospital admissions and hospitalizations. Also, it is difficult to determine the pathogen. There was no difference in DOS of patients with CAP between IS and NIS. The length of stay did not increase in older patients. Furthermore, bilateral pneumonia was more prevalent in IS, whereas lung cancer was more frequent in NIS.
Acknowledgements
The authors would like to thank the support and help of Professor Sonia Buist and ATS-MECOR family for their guidance and contributions to our study.
Footnotes
This study was presented in the “Turkish Thoracic Society 16th Annual congress” April 3–7, 2013, Antalya, Turkey, and “European Respiratory Society Annual Congress” September 7–11, 2013, Barcelona, Spain
Ethics Committee Approval: Authors declared that the research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”, (amended in October 2013).
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - E.T; Design - E.T; Supervision - E.T; Resource - G.B., A.M.; Materials - G.B.; Data Collection and/or Processing - E.T., G.B.; Analysis and/or Interpretation - E.T.,A.M.; Literature Search - E.T.; Writing - E.T.; Critical Reviews - E.T.,A.M.
Conflict of Interest: Authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Lieberman D, Lieberman D, Porath A. Seasonal variation in community-acquired pneumonia. Eur Respir J. 1996;9:2630–4. doi: 10.1183/09031936.96.09122630. [DOI] [PubMed] [Google Scholar]
- 2.Danai PA, Sinha S, Moss M, et al. Seasonal variation in the epidemiology of sepsis. Crit Care Med. 2007;35:410–5. doi: 10.1097/01.CCM.0000253405.17038.43. [DOI] [PubMed] [Google Scholar]
- 3.Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respir Viruses. 2009;3:37–49. doi: 10.1111/j.1750-2659.2009.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puig-Barberà J, Tormos A, Sominina A, et al. First-year results of the Global Influenza Hospital Surveillance Network: 2012–2013 Northern hemisphere influenza season. BMC Public Health. 2014;14:564. doi: 10.1186/1471-2458-14-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamerius J, Nelson MI, Zhou SZ, et al. Global Influenza Seasonality: Reconciling Patterns across Temperate and Tropical Regions. Environ Health Perspect. 2011;119:439–45. doi: 10.1289/ehp.1002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haessler S, Schimmel JJ. Managing community-acquired pneumonia during flu season. Cleve Clin J Med. 2012;79:67–78. doi: 10.3949/ccjm.79a.11108. [DOI] [PubMed] [Google Scholar]
- 7.T.C. Ministry of Health Refik Saydam Hıfzıssıhha Center Presidency. [Influenza Surveillance Report in Turkey]. 2010–2011:37–9. [Article in Turkish: Türkiye İnfluenza Surveyans Raporu] [Google Scholar]
- 8.Özlü T, Bülbül Y, Özsu S. [Community Acquired pneumonia based on the Turkish national data]. Tüberküloz ve Toraks. 2007;55:191–21. [Article in Turkish: Ulusal verilerle toplum kökenli pnömoniler] [PubMed] [Google Scholar]
- 9.Musher DM, Thorner AR. Community-acquired pneumonia. N Engl J Med. 2014;371:1619–28. doi: 10.1056/NEJMra1312885. [DOI] [PubMed] [Google Scholar]
- 10.Baron EJ, Miller JM, Weinstein MP, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2013 recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM)(a) Clin Infect Dis. 2013;57:22–121. doi: 10.1093/cid/cit278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Eerden MM, Vlaspolder F, de Graaff CS, et al. Value of intensive diagnostic microbiological investigation in low- and high-risk patients with community-acquired pneumonia. Eur J Clin Microbiol Infect Dis. 2005;24:241–9. doi: 10.1007/s10096-005-1316-8. [DOI] [PubMed] [Google Scholar]
- 12.Gilca R, Amini R, Douville-Fradet M, et al. Other respiratory viruses are important contributors to adult respiratory hospitalizations and mortality even during peak weeks of the influenza season. Open Forum Infect Dis. 2014;1:ofu086. doi: 10.1093/ofid/ofu086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ortiz JR, Neuzil KM, Shay DK, et al. The burden of influenza-associated critical illness hospitalizations. Crit Care Med. 2014;42:2325–32. doi: 10.1097/CCM.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Someren Gréve F, Ong DSY, Cremer OL, et al. Clinical practice of respiratory virus diagnostics in critically ill patients with a suspected pneumonia: A prospective observational study. J Clin Virol. 2016;83:37–42. doi: 10.1016/j.jcv.2016.08.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansson N, Kalin M, Hedlund J. Clinical impact of combined viral and bacterial infection in patients with community-acquired pneumonia. Scand J Infect Dis. 2011;43:609–15. doi: 10.3109/00365548.2011.570785. [DOI] [PubMed] [Google Scholar]
- 16.Waterer GW, Rello J, Wunderink RG. Management of community acquired pneumonia in adults. Am J Respir Crit Care Med. 2011;183:157–64. doi: 10.1164/rccm.201002-0272CI. [DOI] [PubMed] [Google Scholar]
- 17.Haas J, Braun S, Wutzler P. Burden of influenza in Germany: a retrospective claims database analysis for the influenza season 2012/2013. Eur J Health Econ. 2016;17:669–79. doi: 10.1007/s10198-015-0708-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Claessens YE, Debray MP, Tubach F, et al. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am J Respir Crit Care Med. 2015;192:974–82. doi: 10.1164/rccm.201501-0017OC. [DOI] [PubMed] [Google Scholar]


