Abstract
OBJECTIVES
Chronic respiratory diseases exert a global health burden with high health care costs, morbidity, and mortality. The aim of the present study was to investigate the effect of pulmonary rehabilitation (PR) on emergency admission and hospitalization rates of patients with chronic respiratory disease.
MATERIALS AND METHODS
In this retrospective cohort study, hospitalization rates and emergency admissions of patients before (December 2014–December 2015) and after PR (January 2015–December 2016) were investigated. Patients with chronic respiratory diseases were included. Chronic obstructive pulmonary disease (COPD) patients were classified based on the Global Initiative Chronic Obstructive Pulmonary Disease assessment scheme. PR was applied by three physiotherapists over 8 weeks (2 days/week). Data on patient demographics, clinical and anthropometric data, spirometry, exercise capacity, and quality of life before and after PR were acquired.
RESULTS
This study evaluated 51 patients, of whom 76% were men. A total of 37 (73%) COPD patients and 14 (27%) non-COPD patients (7 bronchiectasis, 4 interstitial lung disease, and 3 kyphoscoliosis) were included. The patients exhibited significantly improved incremental shuttle walk test (ISWT) and endurance test scores (p<0.05) after PR. Similar to exercise capacity, the patients exhibited significantly improved Modified Medical Research Council (mMRC) score, St. George’s Respiratory Questionnaire (SGRQ), anxiety and depression scores (p<0.05) after PR. In COPD patients, differences in pre- and post-PR ISWT, COPD assessment test, mMRC, and SGRQ scores were statistically significant (p=0.001). The number of emergency admissions and hospitalizations significantly decreased after PR (p=0.001; p=0.001). The post-PR FEV1% of COPD significantly increased (p=0.029).
CONCLUSION
Pulmonary rehabilitation leads to an increase in exercise capacity as well as improved quality of life, resulting in a decrease in emergency admissions and hospitalization rates. Considering the cost of hospitalization, it is important to add PR to the management of patients with chronic respiratory diseases, in addition to medical therapy.
Keywords: Pulmonary rehabilitation, exercise treatment, quality of life, emergency application, hospitalization
INTRODUCTION
Chronic respiratory diseases exert considerable global health burden and are associated with high health care costs, mortality, and morbidity [1,2]. Despite receiving optimal medical care, limited daily life activity, social isolation, and depression result in reduced quality of life (QoL) [3]. Moreover, frequent emergency and hospital admissions for chronic respiratory diseases result not only from exacerbation of the disease but also due to anxiety, lack of knowledge regarding the disease, and care problems [4,5].
Pulmonary rehabilitation (PR) is a non-pharmacological, extensive interdisciplinary program for patients with reduced daily life activity. The primary goal of PR is to restore the patient’s optimal functional level and QoL [3]. PR programs are evidence-based and are individualized for each patient [6,7]. Nevertheless, data on the effects of PR on emergency admission and hospitalization rates in Turkey are limited [8].
The object of this study was to investigate the effect of PR on emergency admission and hospitalization rates of patients with chronic respiratory diseases.
MATERIALS AND METHODS
The study was planned as a retrospective cohort study and was conducted in the PR unit of a tertiary training hospital for chest diseases. Patients with hospital and emergency admissions before PR (December 2014–December 2015) and whose emergency and hospital admission information were available after PR (January 2015–December 2016) were recruited.
The study was approved by the ethics committee of Health Sciences University Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital (protocol code: 116.2017.022). The study was conducted in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent.
Patients
Patients with chronic respiratory diseases were included in the PR program in a day-hospital setting. Patients with unstable cardiac disorders, cognitive disorders, neurological disorders, or orthopedic diseases were excluded from the program. Before PR, cardiological evaluation was performed for all patients.
Patients with chronic obstructive pulmonary disease (COPD) were diagnosed in accordance with the Global Initiative Chronic Obstructive Pulmonary Disease (GOLD) assessment scheme. All recruited patients were >40 years old, with a forced expiratory volume in the first minute (FEV1) of <80% of the predicted value and a ratio of FEV1 to forced vital capacity of ≤0.7 [9].
Patients with COPD were evaluated on the basis of the refined GOLD assessment scheme and COPD assessment test (CAT) [10]. Dyspnea was assessed in accordance with the Modified Medical Research Council (mMRC) [11]. The GOLD system has four grades, which are based on the assessment of symptoms/risk of exacerbations. Highly symptomatic (mMRC ≥2, CAT ≥10) patients were classified into grades D and B [12].
Patients with diseases other than COPD, such as bronchiectasis, kyphoscoliosis, and interstitial lung disease, were referred for PR.
This study included patients who completed the 8-week PR program between December 2014 and December 2015. The recruited patients had chronic respiratory diseases, were >18 years old, and had at least one emergency and/or hospital admission 1 year before the PR program.
Patients were excluded if their emergency application and hospital admission data were missing, if they were candidates for surgery due to malignancy or other causes, if they were candidates for surgery and had undergone short-term PR program before surgery, or if they could not perform a walking test because they were bed-bound.
Measurements
Spirometry was performed before and after PR with ZAN 300. Body mass index and fat-free mass index were calculated with a bioelectrical impedance analyzer (Tanita Body Composition Analyzer, Model TBF-300).
Exercise capacity was evaluated through the incremental shuttle walk test (ISWT). Patients with low exercise capacity and high disease burden were evaluated through the 6-min walk test (6MWT).
Incremental shuttle walk test was conducted according to the guidelines set by the European Respiratory Society/American Thoracic Society [13]. Modified Borg dyspnea score and blood pressure were recorded before and after the walking test [14]. The patients were informed about the test; the test was performed in a corridor between two cue cones (the distance between the two cones was set at 10 m) with guidance of voice signals in time to a set of beeps on a CD in. The walking speed was increased at 1-min intervals. The test was discontinued if the patient felt too breathless to continue the test or when the patient failed to walk 10 m in the allowed time. Heart rate and oxygen saturation were also monitored during the entire walking test. The total walking distance was recorded in meters [15]. ISWT was used to measure the sub-maximal exercise capacity of the patient.
Similar to ISWT, the endurance shuttle walk test (ESWT) was developed to evaluate the sub-maximal exercise capacity of a patient. First, ISWT was performed before ESWT. Then, walking speed was calculated as 85% of peak VO2 sustained in ISWT. ESWT included a “warm-up” period to allow the patient to adapt to the test. The patient then walked at a constant speed. The test was discontinued if the patient felt too breathless to continue or if the test time of 20 minutes had elapsed. The primary measurement of the test was the duration of walking expressed in seconds [15,16].
6MWT was performed in accordance with the guidelines of the American Thoracic Society. The patients were guided to walk back and forth in a 30-m-long corridor. Modified Borg dyspnea score and arterial blood pressure were also recorded before and after the walking test. The total walking distance at the end of 6 min was recorded. The test was repeated, and the best results were recorded [17,18].
Health-related QoL was assessed through the St. George’s Respiratory Questionnaire (SGRQ). The total score was calculated from subcategory scores (symptoms, activity, and impact).The scores ranged from 0 (no impairment) to 100 (maximum impairment). A change of four units was considered as minimally clinically significant [19,20]. Anxiety and depression were evaluated using the hospital anxiety and depression questionnaire (HADS), which has 14 items and scores between 0 and 21 for either anxiety or depression [21].
The outpatient PR program was delivered by three physiotherapists in 8 weeks (2 days/week). Exercise programs and workload intensity were targeted at 60%–85% of the maximal workload information gathered from 6MWT and ISWT results. The PR sessions included upper and lower limb strengthening and breathing exercises (0.5–1 kg dumbbell/Cosfer dumbbell sets) and cycle ergometer and treadmill training for 30 min. Workload intensity was increased in accordance with each patient’s improvement. The program also included bronchial clearance techniques and energy conservation methods depending on the patients’ needs [22].
During the sessions, patients receiving long-term oxygen therapy (LTOT) at home also received O2. The rest of the patients received O2 if SpO2 decreased below 90%.
The patients were encouraged to exercise at home apart from the designated session days; for this purpose, a written home-exercise program diary, including exercise figures, were given to all patients. Besides the exercise program, patients’ medical therapies were also optimized, and disease-related educational sessions were held and inhaler medication techniques were taught to the patients and their relatives. Educational sessions were repeated at the beginning of the PR program and weekly between the sessions by the training nurse. Psychological and nutritional support was provided to the patients when needed.
The study is summarized in the flowchart (Figure 1).
Figure 1.
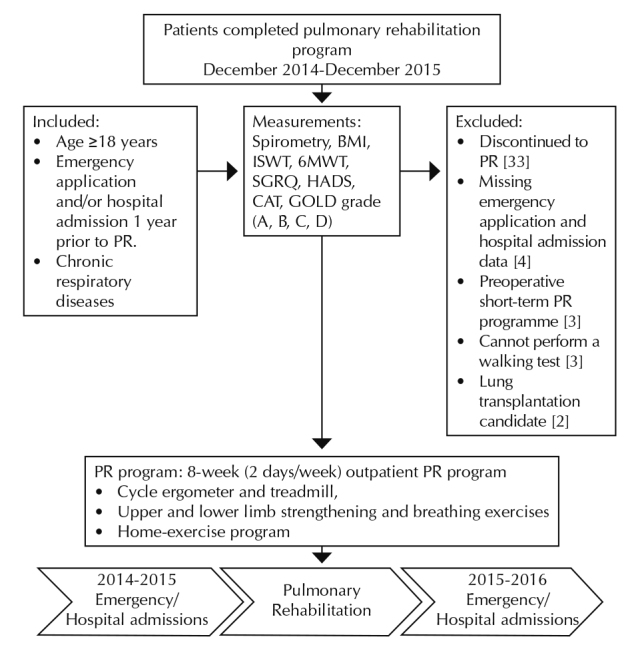
The flowchart of the study
COPD: Chronic obstructive pulmonary disease; mMRC: modified medical research council; COPD assessment test; GOLD: Global Initiative Chronic Obstructive Pulmonary Disease; ISWT: incremental shuttle walk test; 6MWT: six-minute walk test; SGRQ: St. Georg’s Respiratory Questionnaire; HADS: hospital anexiety and depression questionmaire; BMI: body mass index; FFMI: fat-free mass index
Data Collection
Patient demographics, clinical and anthropometric data, exercise capacity, and spirometry and QoL data were obtained before and after PR. Data on emergency and hospital admissions were collected by accessing the hospital registration system and medication records and by calling the patients by telephone.
Outcomes
The primary outcome was hospital admissions and the secondary outcome was emergency admissions.
Statistical Analysis
The SPSS (Statistical Packege for Social Sciences) portable 20.0 package program (IBM Corp.; Armonk, NY, USA) was used for statistical analysis. The median with interquartile range was employed for non-parametric continuous variables, and mean ± standard deviation was used for parametric continuous variables. The non-parametric changes within the groups were analyzed through the Wilcoxon test, and the parametric changes within the groups were analyzed through the t-test. Count and percentage were used when applicable. A p<0.05 was accepted as statistically significant.
RESULTS
This study evaluated 51 patients, of whom 39 (76%) were men and 12 (24%) were women. The patients had a mean age of 60±8 years. A total of 37 (73%) COPD patients and 14 (27%) non-COPD patients (7 bronchiectasis, 4 interstitial lung disease, and 3 kyphoscoliosis) were included. Out of all recruited patients, 23 (45%) received LTOT and 11 (22%) received noninvasive ventilation (NIV) at home. Table 1 summarizes patients’ demographics.
Table 1.
Demographics of pulmonary rehabilitation patients (n=51)
| Age (mean±SD) | 60±8 |
| Sex, n (%) | |
| Female | 12 (24) |
| Male | 39 (76) |
| Chronic pulmonary disease, n (%) | |
| COPD | 37 (73) |
| Non-COPD | 14 (27) |
| Bronchiectasis | 7 (14) |
| Interstitial lung disease | 4 (8) |
| Kyphoscoliosis | 3 (6) |
| Smoking history, n (%) | 42 (82) |
| Smoking (pack-year), median (IQR) | 35 (10–50) |
| LTOT, n (%) | 23 (45) |
| NIV, n (%) | 11 (22) |
| BMI (kg/m2)* | 26±6 |
| FFMI (kg/m2) | 20±3 |
| mMRC, median (IQR) | 2.5 (2–3) |
| FEV1 %* | 40±17 |
mean±SD; LTOT: long-term oxygen therapy; NIV: noninvasive ventilation; FFMI: fat-free mass index; BMI: body mass index
The exercise capacity and QoL of patients before and after PR are shown in Table 2. The patients exhibited significant improvement in walking distance in ISWT and endurance time test scores (p=0.001, p=0.037) after PR. Eight patients were subjected to 6MWT, given that they were unable to carry on to ISWT as they had reduced effort capacity. The improvement in 6MWT after PR was not statistically significant (p=0.08), whereas minimal clinically important difference (MCID) (30 m) was established.
Table 2.
Exercise capacity and quality of life of patients before and after pulmonary rehabilitation (n=51)
| Before PR | After PR | p | |
|---|---|---|---|
| ISWT (m),* | 296±114 | 366±106 | 0.001 |
| Endurance time,(min)* | 6.9±5.3 | 10.2±7.3 | 0.037 |
| 6MWT (m),* | 234±50 | 310±81 | 0.08 |
| BMI (kg/m2),* | 26±6 | 26±6 | 0.13 |
| FFMI (kg/m2),* | 20±3 | 20±2 | 0.39 |
| mMRC, median IQR | 2.5(2–3) | 2(1–2) | 0.001 |
| SGRQ score,* | |||
| Symptom | 65±17 | 56±18 | 0.001 |
| Activity | 73±19 | 64±19 | 0.001 |
| Impact | 53±24 | 39±23 | 0.001 |
| Total | 61±19 | 49±18 | 0.001 |
| HADS,* | |||
| Anxiety | 10±5 | 7±5 | 0.003 |
| Depression | 9±5 | 7±4 | 0.022 |
mean±SD; HADS: hospital anxiety and depression questionnaire; SGRQ: St. George’s Respiratory Questionnaire; FFMI: fat-free mass index; BMI: body mass index; ISWT: incremental shuttle walk test; 6MWT: 6-min walk test was performed in 8 patients; IQR: interquartile range
Similar to exercise capacity, the patients exhibited significantly improved mMRC, SGRQ, and anxiety and depression scores (p=0.001, p=0.001, p=0.003, and p=0.022, respectively) after PR.
Changes in exercise capacity, QoL, emergency and hospitalization characteristics before and after completion of the PR program of 37 COPD patients are defined in Table 3 in accordance with the GOLD grade.
Table 3.
Exercise capacity and quality of life characteristics before and after the pulmonary rehabilitation program of COPD patients n=37
| Before PR | After PR | p | |
|---|---|---|---|
| ISWT (m),* | 302±118 | 373±111 | 0.001 |
| Endurance time (min), median IQR | 5.5(3.5–9.2) | 6.6(4.2–20) | 0.050 |
| 6MWT (m),* | 227±72 | 302±114 | 0.47 |
| BMI (kg/m2),* | 26±6 | 27±6 | 0.46 |
| FFMI (kg/m2),* | 20±3 | 20±3 | 0.88 |
| mMRC, median IQR | 2(2–3) | 2(1–2) | 0.001 |
| CAT, median IQR | 17(15–24) | 11(8–17) | 0.001 |
| FEV1%* | 38±15 | 46±16 | 0.029 |
| SGRQ score,* | |||
| Symptom | 63±18 | 52±19 | 0.001 |
| Activity | 71±19 | 59±19 | 0.001 |
| Impact | 53±20 | 35±24 | 0.001 |
| Total | 50±21 | 44±20 | 0.001 |
| HADS,* | |||
| Anxiety | 9±5 | 7±4 | 0.014 |
| Depression | 9±6 | 7±3 | 0.027 |
| COPD GOLD grade, n (%) | |||
| GOLD B | 20 (54) | 26(70) | 0.11 |
| GOLD C | 0 | 5(14) | 0.025 |
| GOLD D | 17(46) | 6(16) | 0.001 |
mean±SD; GOLD: global initiative for obstructive lung disease grade; HADS: hospital anxiety and depression questionnaire; CAT: COPD assessment test; BMI: body mass index; FFMI: fat-free mass index; ISWT: Incremental shuttle walk test; 6MWT: 6-min walk test was performed in 4 patients; IQR: interquartile range
The differences in pre and post-PR ISWT, CAT, mMRC, and SGRQ scores were statistically significant (p=0.001). The post-PR FEV1% of COPD significantly increased (p=0.029). The depression and anxiety scores of COPD patients significantly improved after PR (p=0.014, p=0.027).
Before PR, COPD patients were more likely to be in the GOLD grade B (n=20, 54%) and D (n=17.46%). After PR, however, the number of patients in the GOLD grade D significantly decreased (p=0.001), whereas those in grades B and C significantly increased (p=0.11, p=0.001).
Changes in emergency admissions and hospitalization rates before and after PR are shown in Table 4. The number of emergency admissions and hospitalization rates significantly decreased after PR (2 vs 0.1 vs 0; p=0.001, p=0.001, respectively). Similarly, the emergency admissions and hospitalization rates of patients with COPD post-PR significantly decreased (p=0.001).
Table 4.
Changes in emergency admissions and hospitalization rates in 1 year: before and after pulmonary rehabilitation
| Before PR | After PR | p | |
|---|---|---|---|
| Emergency applications* | |||
| All patients, (n=51) | 2(1–4) | 0(0–1) | 0.001 |
| COPD patients, (n=37) | 2(1–5) | 0(0–1) | 0.001 |
| Hospitalizations* | |||
| All patients, (n=51) | 1(0–2) | 0(0–1) | 0.001 |
| COPD patients, (n=37) | 1(0–2) | 0(0–1) | 0.001 |
median; IQR: interquartile range
DISCUSSION
The present study demonstrates that PR decreases emergency and hospital admissions of patients with chronic respiratory diseases. In addition, PR improves the exercise capacity and QoL of the studied patient group.
Gas exchange restriction, cardiac restriction, ventilatory limitation, malnutrition, hypoxia, systemic inflammation, and lower extremity and respiratory muscle dysfunctions are the major reasons for shortness of breath and movement restrictions experienced by patients with chronic respiratory disease [6,23]. O2 and NIV support, although sometimes necessary, restrict the patient’s mobility, consequently causing the patient to stay at home frequently, to become withdrawn and socially isolated. These social effects create a vicious circle that must be broken through PR. On the basis of GOLD guidelines, PR has been approved as a non-pharmacological comprehensive treatment in addition to medical therapy [10]. Recent studies have shown that PR has positive effects on older patients with COPD [20,21]. The present study included patients with COPD, as well as those with chronic respiratory diseases other than COPD. The results suggested that PR is suitable not only for COPD but also for other chronic lung diseases. Thus, patients with early-stage interstitial lung disease should undergo PR [24].
The walking distance in ISWT and endurance time in ESWT significantly improved. Although pre- and post-PR results of 6MWT, which was performed by only six patients, were not statistically different, they exhibited minimal clinical significance. An increase in the walking distance of 47.5 m in ISWT in the whole study group and in the COPD sub-group was established [25,26]. There is no MCID value for endurance time obtained with ESWT for PR yet [27]. The difference in walking distance obtained by 6MWT between pre- and post-PR exceeded the proposed 30 m, which is the MCID value suggested for all chronic respiratory diseases [18]. A score of 1.5 for HADS, 4 for SGRQ, and 2 for CAT are all clinically important values [16,19,21,26].
Dyspnea, the need for medication and care, social isolation, emergency admissions, and hospital admissions often result in depression and anxiety among patients with chronic respiratory disease [28,29]. The patients’ relatives and caregivers also exhibit emotional disorders. In this study, the anxiety and depression scores of patients significantly improved after PR (p=0.003, p=0.022). The anxiety and depression scores and exercise capacity of patients who can cope with illness-related complaints, such as frequent coughing and increased sputum production, significantly improved after PR. Inadequate medical treatments and the fear of the disease often create anxiety and even panic in patients with interstitial lung diseases. Depression should not be ignored while following up with these patients, and psychological support should be recommended if necessary.
The significant improvements in SGRQ score indicated that PR achieved its main objective of ensuring that patients with chronic respiratory disease become active and independent. In addition to the 8-week (2 days/week) PR program provided at the hospital, patients were encouraged to apply and practice PR at home using a printed home-exercise program diary including exercise figures. Patients who exercise regularly are convinced that exercise should be a permanent behavioral change when they witness their gains.
Patients with COPD and bronchiectasis are often housebound, especially during autumn and winter, due to frequent attacks of their illness. The implementation of PR increases the awareness and ability of patients to control their disease as well as improves relationship between patients and their physicians. These effects collectively decrease the number of hospital and emergency appointments [30]. Man et al. [29] reported the importance of early PR after exacerbations; moreover, they reported that hospitalization rates decreased within the first 3 months after the implementation of PR. Although PR is an effective procedure, adherence to the program is still below expectations [9,31,32]. Golmohammadi et al. [33] mentioned the cost effectiveness of PR for patients with COPD and for those who had frequent emergency and hospital admissions. However, the duration and components of PR should be developed and optimized to enable its application in real clinical practice [34].
Educational sessions on inhaler drug techniques, O2 therapy, and energy conservation methods were provided as a component of rehabilitation to the patients and their caregivers. These sessions applied at first days in the PR program and repeated weekly between sessions by the training nurse. The sessions positively affected patients’ compliance. Spencer et al. [31] emphasized the importance of education as a PR component in decreasing healthcare costs [4,35]. In this study, the FEV1% of COPD patients significantly increased (p=0.029) after PR. Although it has not been reported that PR increases respiratory function, in this study, we observed improvement in FEV1% values. This result can be attributed to an increase in compliance with treatment as a result of educational sessions on inhaler drug techniques and O2 therapy and the positive effect of exercise on hyperinflation [13,36].
The present study has some limitations. This is a retrospective study conducted at one center. In addition, the small sample size of this study may limit the identification of small but potentially significant associations; the number of interstitial lung disease is inadequate; and there is no control group. The strength of this study based on its collected data, which indicated the importance of PR among patients with chronic respiratory diseases.
In conclusion, PR increases the exercise capacity and QoL of patients with chronic respiratory diseases. These positive effects will collectively decrease the emergency admission and hospitalization rates of this patient population. Therefore, PR should be added to the management of patients with chronic respiratory diseases in conjunction with medical therapy to decrease hospitalization costs. Furthermore, PR should be promoted among pulmonologists to facilitate its use in real-life settings.
Footnotes
The study was presented in 20th Annual congress of the Turkish Thoracic Society, April 5–9, 2017, Antalya, Turkey.
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Health Sciences University Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital (Approval No: 116.2017.022)
Informed Consent: Written informed consent was obtained from all patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept – İ.Ö.; Design – İ.Ö.; E.Y.; Supervision – İ.Ö., E.Y., M.Ö., B.O.; Resource – E.Y., Ö.Y., M.K., R.A., E.A.; Materials – M.Ö., Ö.Y., M.K., R.A.; Data Collection and/or Processing – Ö.Y., M.K., R.A., R.Y., B.O.; Analysis and/or Interpretation – İ.Ö., E.Y., B.O., E.A.; Literature Search – R.Y., E.Y., M.Ö., B.O.; Writing – İ.Ö., E.Y.; Critical Reviews – İ.Ö, E.Y.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.World Health Organization. Burden of COPD. [Last accessed on 2017 July]. Available from: http://www.who.int/respiratory/copd/burden/en/
- 2.Cruz A. A global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. World Health Organization; 2007. [Accessed: 06.06.2017]. http://www.who.int/respiratory/publications/global_surveillance/en/ [Google Scholar]
- 3.Dourado VZ, Tanni SE, Vale SA, et al. Systemic manifestations in chronic obstructive pulmonary disease. J Bras Pneumol. 2006;32:161–71. doi: 10.1590/S1806-37132006000200012. [DOI] [PubMed] [Google Scholar]
- 4.Bove DG, Midtgaard J, Kaldan G, et al. Home-based COPD psychoeducation: A qualitative study of the patients’ experiences. J Psychosom Res. 2017;98:71–7. doi: 10.1016/j.jpsychores.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Howcroft M, Walters EH, Wood-Baker R, et al. Action plans with brief patient education for exacerbations in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005074. doi: 10.1002/14651858.CD005074.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Celli BR. Pathophysiological basis of pulmonary rehabilitation in chronic obstructive pulmonary disease. In: Donner CF, Goldstein RS, Ambrosino N, editors. Pulmonary Rehabilitation. Hodder Education; Great Britain: 2005. pp. 18–26. [Google Scholar]
- 7.Casaburi R. A brief history of pulmonary rehabilitation. Respir Care. 2008;53:1185–9. [PubMed] [Google Scholar]
- 8.Sahin H, Varol Y, Naz I, et al. The effect of pulmonary rehabilitation on COPD exacerbation frequency per year. Clin Respir J. 2018;12:165–74. doi: 10.1111/crj.12507. [DOI] [PubMed] [Google Scholar]
- 9.Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global strategy for the diagnosis, management and prevention of Chronic Obstructive Pulmonary Disease. [Accessed:7.10.2016]. [Internet] Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/
- 10.Yorgancıoğlu A, Polatlı M, Aydemir Ö, et al. Reliability and validity of Turkish version of COPD assessment test. Tuberk Toraks. 2012;60:314–20. doi: 10.5578/tt.4321. [DOI] [PubMed] [Google Scholar]
- 11.Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–6. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. Respirology. 2017;22:575–601. doi: 10.1111/resp.13012. [DOI] [PubMed] [Google Scholar]
- 13.Spruit MA, Singh SJ, Garvey C, et al. An Official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:13–64. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 14.Wilson RC, Jones PW. A comparison of the visual analogue scale and modified Borg scale for the measurement of dyspnoea during exercise. Clin Sci (Lond) 1989 Mar;76:277–82. doi: 10.1042/cs0760277. [DOI] [PubMed] [Google Scholar]
- 15.Revill SM, Morgan MD, Singh SJ, et al. The endurance shuttle walk: A new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax. 1999;54:213–22. doi: 10.1136/thx.54.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1447–78. doi: 10.1183/09031936.00150414. [DOI] [PubMed] [Google Scholar]
- 17.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 18.Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1428–46. doi: 10.1183/09031936.00150314. [DOI] [PubMed] [Google Scholar]
- 19.Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation: The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145:1321–7. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 20.Polatlı M, Yorgancıoğlu A, Aydemir Ö, et al. Validity and reliability of Turkish version of St. George’s respiratory questionnaire. Tuberk Toraks. 2013;61:81–7. doi: 10.5578/tt.5404. [DOI] [PubMed] [Google Scholar]
- 21.Puhan MA, Frey M, Büchi S, et al. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2008;6:46. doi: 10.1186/1477-7525-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nici L, Donner C, Wouters E, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 23.Macintyre NR. Muscle dysfunction associated with chronic obstructive pulmonary disease. Respir Care. 2006;51:840–7. [PubMed] [Google Scholar]
- 24.Vainshelboim B, Oliveira J, Yehoshua L, et al. Exercise training-based pulmonary rehabilitation program is clinically beneficial for idiopathic pulmonary fibrosis. Respiration. 2014;88:378–88. doi: 10.1159/000367899. [DOI] [PubMed] [Google Scholar]
- 25.Redelmeier DA, Bayoumi AM, Goldstein RS, et al. Interpreting small differences in functional status: the Six Minute Walk test in chronic lung disease patients. Am J Respir Crit Care Med. 1997;155:1278–82. doi: 10.1164/ajrccm.155.4.9105067. [DOI] [PubMed] [Google Scholar]
- 26.Singh SJ, Jones PW, Evans R, et al. Minimum clinically important improvement for the incremental shuttle walking test. Thorax. 2008;63:775–7. doi: 10.1136/thx.2007.081208. [DOI] [PubMed] [Google Scholar]
- 27.Pepin V, Laviolette L, Brouillard C, et al. Significance of changes in endurance shuttle walking performance. Thorax. 2011;66:115–20. doi: 10.1136/thx.2010.146159. [DOI] [PubMed] [Google Scholar]
- 28.Janssen DJ, Spruit MA, Leue C, et al. Ciro network. Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chron Respir Dis. 2010;7:147–57. doi: 10.1177/1479972310369285. [DOI] [PubMed] [Google Scholar]
- 29.Man WD, Polkey MI, Donaldson N, et al. Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. BMJ. 2004;329(7476):1209. doi: 10.1136/bmj.38258.662720.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Özgün Niksarlioglu EY, Özkan G, Günlüoğlu G, et al. Factors related to depression and anxiety in adults with bronchiectasis. Neuropsychiatr Dis Treat. 2016;12:3005–10. doi: 10.2147/NDT.S121147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spencer LM. Rehabilitation following hospitalization in patients with COPD: Can it reduce readmissions? Respirology. 2015;20:357–8. doi: 10.1111/resp.12491. [DOI] [PubMed] [Google Scholar]
- 32.Moore E, Newson R, Joshi M, et al. Effects of Pulmonary Rehabilitation on Exacerbation Number and Severity in People With COPD: An Historical Cohort Study Using Electronic Health Records. Chest. 2017;152:1188–202. doi: 10.1016/j.chest.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Golmohammadi K, Jacobs P, Sin DD. Economic evaluation of a community-based pulmonary rehabilitation program for chronic obstructive pulmonary disease. Lung. 2004;182:187–96. doi: 10.1007/s00408-004-3110-2. [DOI] [PubMed] [Google Scholar]
- 34.Kon SS, Canavan JL, Man WD. Pulmonary rehabilitation and acute exacerbations of COPD. Expert Rev Respir Med. 2012;6:523–31. doi: 10.1586/ers.12.47. [DOI] [PubMed] [Google Scholar]
- 35.Maddocks M, Kon SS, Singh SJ, et al. Rehabilitation following hospitalization in patients with COPD: can it reduce readmissions? Respirology. 2015;20:395–404. doi: 10.1111/resp.12454. [DOI] [PubMed] [Google Scholar]
- 36.Ergün P, Kaymaz D, Günay E, et al. Comprehensive out-patient pulmonary rehabilitation: Treatment outcomes in early and late stages of chronic obstructive pulmonary disease. Ann Thorac Med. 2011;6:70–6. doi: 10.4103/1817-1737.78420. [DOI] [PMC free article] [PubMed] [Google Scholar]


