Abstract
Intermittent hypoxia (IH) that resulted from obstructive sleep apnea (OSA) has been found to be a risk factor of coronary artery disease. IH and the receptor for advanced glycation end products (RAGE) expression are known to activate monocyte/macrophage and associated with atherosclerosis development, while their effects on monocyte adhesion, chemotaxis to the endothelium, and macrophage polarization remain unknown. In the present study, RAGE in THP-1 monocytes was inhibited by shRNA lentiviral particles, followed by exposure to IH. Cell adhesion assay, transwell migration assay, and macrophage polarization assays were performed to study the effects of IH and RAGE. The mRNA and protein expression levels were investigated by RT/real-time PCR and western blot analysis, respectively. We found that IH increased RAGE expression and activated NF-кB signalling in THP-1 monocytes. The results also revealed that IH enhanced the MCP-1-mediated THP-1 monocyte adhesion and chemotaxis and promoted macrophage polarization toward a proinflammatory phenotype, which was mediated by RAGE activity. Additionally, inhibition of chemokine receptor type 2 (CCR2) suppressed the IH-induced monocyte adhesion and chemotaxis. These results demonstrated a potential role of monocyte adhesion, chemotaxis, and macrophage polarization in the development cardiovascular diseases induced by IH and identified that RAGE could be a promising therapeutic target to prevent atherosclerosis in patients with OSA.
1. Introduction
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated episodes of obstructive apnea and hypopnea during sleep [1]. The patients often present symptoms of daytime sleepiness or altered cardiopulmonary function, which have been reported to be affecting more than 10% of the adult population [2]. Besides these, it increases the risk of numerous clinical conditions including diabetes mellitus, dyslipidemia, and cardiovascular diseases. Moreover, it has been suggested that OSA is closely associated with atherosclerosis and detrimental cardiovascular events [3].
Intermittent hypoxia (IH) has been identified as one of the hallmark characteristics of OSA. The relationship between IH and atherosclerosis has been verified by many in vivo studies [4, 5], which showed that IH induced vascular inflammation and atherosclerotic plaques formation in mice. Additionally, clinical studies have reported that IH increases the levels of serum advanced glycation end products (AGE) in people with OSA [6]. Furthermore, a growing body of evidences suggested that the activation of the specific cell-surface receptor for AGE (RAGE) plays a critical role in the development of atherosclerotic lesion [7, 8]. For example, hypoxia-induced inflammation could be attenuated in RAGE-deficient mice [9]. However, the molecular mechanisms underline that these observations remain poorly understood.
Macrophage is the key regulator in all phases of atherosclerosis, from initial fatty streaks formation to vascular lesions. The formation of atherosclerotic plaque is a highly complex process. The adhesion of monocytes to the endothelium and subsequent transmigration through the vascular endothelial wall are central to the development of atherosclerosis [10]. It has been established that the monocytes are attracted and activated by chemokines released from inflamed endothelial cells, especially, the monocyte chemotactic protein-1 (MCP-1), which is abundantly found in atherosclerotic plaques in human [11, 12]. Also, in response to stimulus, the monocytes differentiate and polarize into inflammatory (M1) or anti-inflammatory (M2) macrophages [13]. M1 macrophages play critical roles in diseases progression by inducing an inflammatory state, which is characterized by upregulated expression of proinflammatory mediators, while M2 macrophages contribute to inflammation resolution via secretion of anti-inflammatory cytokines [14]. M1/M2 ratio is believed to be a major determinant of atherosclerotic lesions [13]. It has been showed that RAGE mediates monocyte differentiation and lipids accumulation in macrophages that lead to foam cell formation [15]. However, few study has investigated the possible regulatory role of RAGE in monocyte adhesion, migration, and macrophage polarization in IH, which are required for an improved understanding of the mechanisms that how atherosclerosis develops in patients with OSA.
Therefore, the aims of the present study were to investigate the RAGE expression in monocytes and to elucidate its roles in monocyte adhesion, migration, and macrophage polarization in IH using an in vitro THP-1 monocytes model and monocyte-endothelia cell coculture model.
2. Materials and Methods
2.1. Reagents and Antibodies
Monocyte chemoattractant protein-1 (MCP-1) was purchased from R&D Systems (MN, USA). Primary antibodies for human RAGE, IkBα, NF-κB p65, phosphorylated NF-κB p65, CCR2, and GAPDH were purchased from Abnova (Taipei, Taiwan). Alexa 488 conjugated secondary antibody, Alexa Fluor 555 Phalloidin, and DAPI were purchased from Beyotime (Shanghai, China). The siRNA duplexes against human RAGE (ID: 110859) were purchased from Ambion Life Technologies (NY, USA). The RAGE shRNA lentiviral particles and control shRNA lentiviral particles were purchased from Santa Cruz Biotechnology (USA). The CCR2 neutralizing antibody and CCR2 Isotype control were purchased from Santa Cruz Biotechnology (USA). The CCR2 antagonist (C28H34F3N5O4S, CAS 445479-97-0) was purchased from Merck Millipore (USA).
2.2. Cell Culture and Treatment
THP-1 cells (human monocytic leukemia cell line) were purchased from the American Type Culture Collection (ATCC) and cultured in suspension in T-75 culture flasks with RPMI 1640 medium containing 10% fetal bovine serum, 100 U/mL penicillin, 100 μg/ml streptomycin, 1 mM glutamine, 10 mM HEPES, 50 μM β-mercaptoethanol, and 1 mM sodium pyruvate. For macrophage polarization experiments, THP-1 monocytes were treated with 10 ng/ml Phorbol 12-myristate 13-acetate (PMA, Sigma Aldrich, USA) for 48 h to differentiate into adherent macrophage-like cells prior to exposure to IH for 24 hours and analysis of macrophage markers. Human vascular endothelial cells (HUVECs) were grown in EGM-2 medium (Lonza, USA). HUVECs at passages 3-7 were used in the experiments. The cells were maintained in a humidified incubator with 5% CO2/95% air at 37°C.
2.3. RNA Interference (RNAi)
For siRNA tests, THP-1 monocytes were pretreated with NF-kB siRNA or control siRNA using the Cell Line Nucleofector (Lonza, USA) and buffer kit V (Lonza, USA) according to the manufacturer's protocol. After 48 h, treated cells were exposed to IH for 24 h followed by protein samples collection for western blot assays.
To silence the RAGE gene, THP-1 monocytes at a density of 2 × 105 cells/well in a 6-well plate were first suspended in growth media supplemented with 5 μg/mL polybrene and incubated overnight. Then RAGE shRNA lentiviral particles or control shRNA lentiviral particles were added. After 48 h of incubation at 37°C, the viral load was removed by centrifugation. THP-1 monocytes were washed with PBS and cultured in growth media. Successfully transfected THP-1 monocytes were selected by treatment with 10 μg/mL puromycin (Santa Cruz Biotechnology, USA) until all cells in the control flask were confirmed dead.
2.4. Conditions of Normoxia and Intermittent Hypoxia
Condition of normoxia or IH was conducted in a specifically designed gas flow chamber modified from In Vivo 400 Hypoxic Work Station (Biotrace, Cincinnati, OH). Treated cells were cultured in condition of normoxia (21% O2, 5% CO2) or IH (6 cycles of 35 min of hypoxia [0.1% or 5% O2 and 5%CO2] followed by 25 min of normoxia; CO2 was maintained at 5% throughout the exposure). The chamber was placed in a standard humidified incubator at 37°C.
2.5. Western Blotting
Protein samples were extracted from THP-1 monocytes according to the method established previously [16]. The cell lysates were collected and protein concentration was determined using standard BCA assay. Equal amounts of protein (20 μg/sample) were subjected to SDS-PAGE (4–10%) followed by electrophoretic transfer to nitrocellulose membranes. In order to block the nonspecific binding, the membranes were incubated with skim milk (5%) for 1 h at room temperature. After that, the blot was incubated with one of the following primary antibodies overnight at 4°C: rabbit anti-RAGE IgG (1:500), anti-phosphorylated NF-κB p65 (1:1000), anti-IκBα IgG (1: 1000), anti-CCR2 IgG (1:1000), and anti-GAPDH IgG (1:3000). After that, membranes were incubated with suitable HRP-conjugated second antibody (1:2000) at 37°C for 1 h, followed by washing and reacting with the ECL detection reagents followed by scanning on a densitometer. The signals specific for target proteins on the gel were then analyzed.
2.6. Total RNA Extraction and RT-PCR
Total RNA from THP-1 monocytes/macrophages was extracted using the RNeasy Plus Mini kit (Qiagen). The RNA was quantified using Thermo Bio-Mate3 and diluted into 1 mg/mL. Total RNA (0.5 μg) was processed directly to cDNA synthesis using the oligo (dT) 15 primer and SuperScript™ II reverse transcriptase reagents (TaKaRa, Dalian, China) according to the manufacturer's protocol. Real-time PCR was performed using qSYBR Green PCR Kit (Dongsheng, Guangzhou, China). All PCR primers were designed using software PrimerExpress or published sequence data from the NCBI database. The sequences of forward and backward primers are listed in Table 1. All these primers were synthesized from Invitrogen (USA). All reactions were performed in triplicate in an ABI PRISM 7900HT Sequence Detection system. Data are calculated by the 2−ΔΔCT method and are presented as the fold induction to GAPDH compared with THP-1 monocytes/macrophages cultured in normoxia.
Table 1.
Forward and backward sequences of the primers used in this study.
| Gene | Forward | Reverse | Genbank ID |
|---|---|---|---|
| RAGE | CTC GAA TGG AAA CTG AAC AC | CTG GTA GTT AGA CTT GGT CTC | 177 |
| CCR2 | AGT GCT TCG CAG ATG TCC TT | TAG TTC CCA AGT TGC CTG GT | 729230 |
| IL-1β | TGTGCAAGTGTCTGAAGCAGC | TGGAAGCAGCCCTTCATCTT | 3553 |
| IL-6 | CTGTTGACAAGCAATGAGACGATGAGG | GAGGATACCACTCCCAACAGACC | 3569 |
| IL-10 | GCC TAA CAT GCT TCG AGA | TGA TGT CTG GGT CTT GGT TC | 3586 |
| Nf-κB | CTGGTGATCGTGGAACAGCC | CAGAGCCTGCTGTCTTGTCC | 4790 |
| TNF-α | ACA ACC TTC TTG CAG CTC CTC | TGACCCATACCCACCATCAC | 7124 |
| TGF-β | GGACACCAACTATTGCTTCAG | TCCAGGCTCCAAATGTAGG | 7040 |
| CD80 | TGGTGCTGGCTG GTCTTTC | CTGTGCCACTTCTTTCACTTCC | 941 |
| ARG-1 | TACTAGGAAGAAAGAAAAGGCCAATTC | GTAGCCCTGTTTTGTAGATTTCTTCTGT | 383 |
| CD163 | CCAGTCCCAAACACTGTCCT | ATGCCAGTGAGCTTCCCGTTCAGC | 9332 |
| GAPDH | GGC ATG GAC TGT GGT CAT GAG | TGC ACC ACC AAC TGT TAG C | 2597 |
2.7. Cell Adhesion Assay
THP-1 monocytes were first activated by 20 ng/ml MCP-1 for 12 h. Then 2 × 105 THP-1 monocytes were added to each well containing a monolayer of confluent HUVECs in a 24-well tissue culture plate. THP-1 monocytes and HUVECs cells were incubated at 37°C in normoxia or IH with nonadhered cells removed by gentle washing with warm PBS twice after 30 min. The number of adhered THP-1 monocytes was then counted using the inverted microscope.
2.8. THP-1 Monocytes Migration
A transwell migration assay was applied to study the transmigration behaviour of THP-1 monocytes. 24-transwell inserts with pore sizes of 3 μm (Corning, USA) were employed. The lower surface of the insert was coated with gelatin solution (1 mg/mL) and allowed to dry for 15 min before experiments. 106 THP-1 monocytes in 200 μl of serum-free RPMI 1640 were loaded into the upper chamber of the transwell insert. 600 μl RPMI medium containing 10 ng/ml MCP-1 (R&D Systems, USA) was added to the lower chamber. The cells were then allowed to migrate in normoxia or IH for 8 h. The number of cells that had migrated across the membrane to the lower chamber was counted microscopically using a Motic AE30/31 inverted microscope (Motic Co, China).
2.9. Immunofluorescence Staining
THP-1 cells were fixed with 4% paraformaldehyde (Beyotime, China) and permeabilized with 0.5% Triton X-100 (Beyotime, China). PBS with 5% BSA was used to block the nonspecific binding sites. Monoclonal anti-NF-κB primary antibody in PBS with 1% BSA was incubated with the sample overnight. After this, cells were washed and incubated for 1 h at room temperature in Alexa 488 conjugated anti-Mouse IgG as secondary antibody. To visualize the F-actin, the samples were incubated with 200 μl of Alexa Fluor 555 Phalloidin at room temperature for 20 mins in the dark. Cell nuclei were stained by incubation with 5 μg/ml DAPI for 5 min. Slides were then visualized with a fluorescence microscope (SP2, Leica, Germany) using x40 objective.
2.10. Data Analysis
The results are presented as mean ± SEM for each treatment group in each experiment with all experiments repeated for at least three times. Statistical significance was analyzed by one-way analysis of variance using computer software SPSS (Version 20). The data between different experimental groups were analyzed by Student's Newman-Keuls test and p < .05 was considered statistically significant.
3. Results
3.1. Intermittent Hypoxia Upregulated RAGE Expression and Activated NF-кB Pathway in THP-1 Monocytes
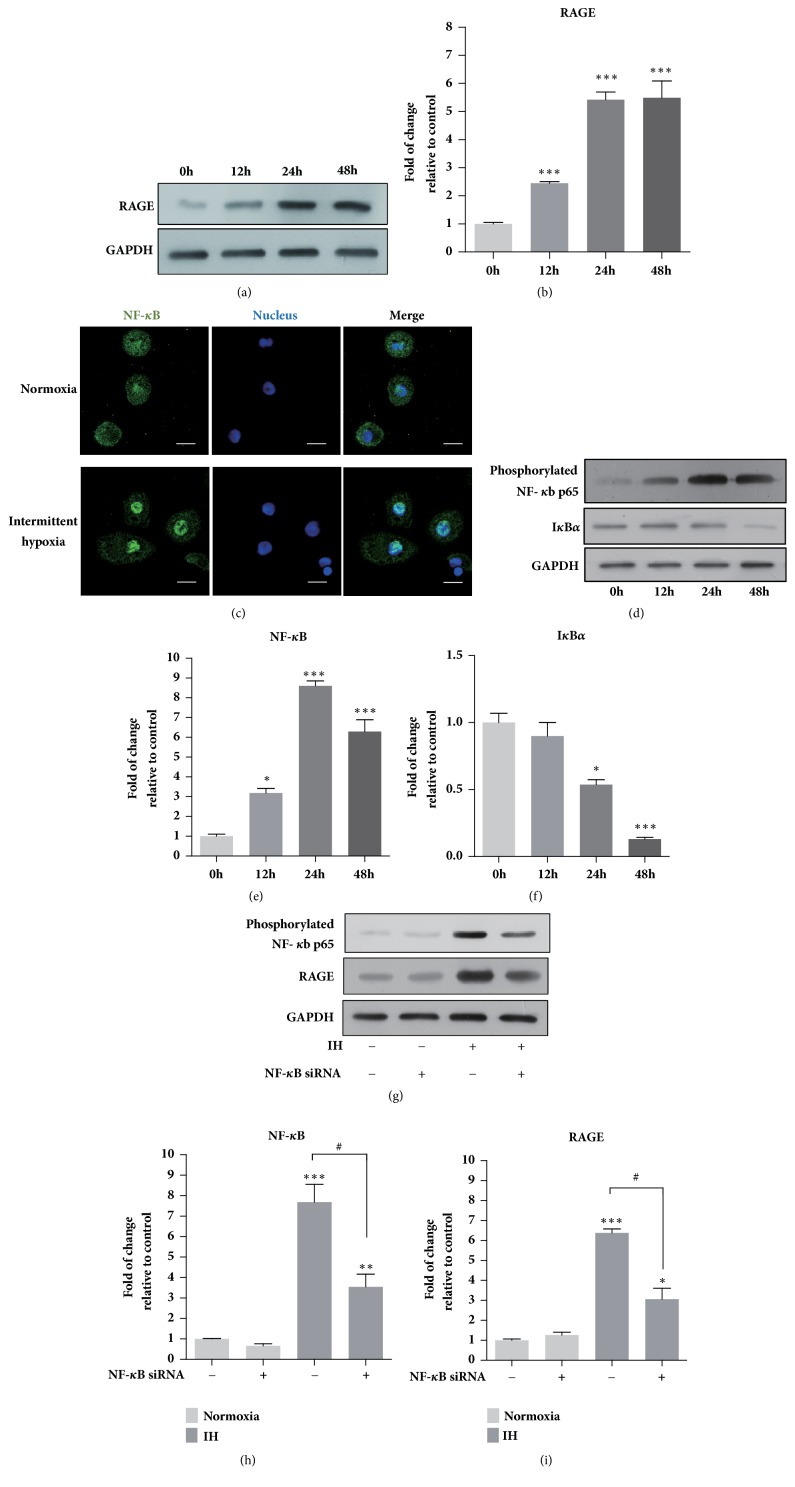
According to the time course experiment shown in Figures 1(a) and 1(b), in the IH-exposed THP-1 monocytes, the level of RAGE was increased in a time-dependent manner. The expression of RAGE in THP-1 cells was increased by around 3-fold after 12 h in IH. Then RAGE protein level reached a peak value of increase after 24 h incubation and remained at that level for the next 24 h. In addition, after exposure to IH for 24 h, NF-κB translocated and accumulated into the nucleus of THP-1 cells (Figure 1(c)). Also, the protein level of phosphorylated NF-κB p65 was increased while IkBα was decreased in a similar time-dependent manner in IH (Figures 1(d)–1(f)) thus confirming the activation of NF-κB signalling. Furthermore, by using NF-κB siRNA to downregulate NF-κB (Figures 1(g) and 1(h)), it was observed that NF-κB siRNA was able to significantly reduce the upregulation of RAGE expression that resulted from IH (Figures 1(g) and 1(i)), which suggested that NF-κB signalling played a positive role in the activation of RAGE in IH.
Figure 1.
Intermittent hypoxia increased RAGE expression and activates the NF-кB pathway in THP-1 monocytes. (a and b) RAGE expression of THP-1 cells exposed to IH compared to cells in normoxia over a period of 48 h. (c) Representative images of immunofluorescence staining showing the nuclear translocation of NF-кB p65 (green) in THP-1 cells. Scale bars indicate 10 μm. (d–f) Phosphorylated NF-κB p65 and IkBα protein expression and quantification of THP-1 cells exposed to IH compared with cells cultured under normoxia over a period of 48 h. (g–i) Phosphorylated NF-κB p65 and RAGE protein expression and quantification of NF-κB siRNA treated cells compared to untreated cells exposed to normoxia or IH. Data were represented as mean + SEM. ∗ represents significant difference compared with normoxic group, ∗/#p<.05, ∗∗p<.01, ∗∗∗p<.001.
3.2. Knockdown of RAGE Inhibited Adhesion and Chemotaxis of THP-1 Monocytes Exposed to Intermittent Hypoxia
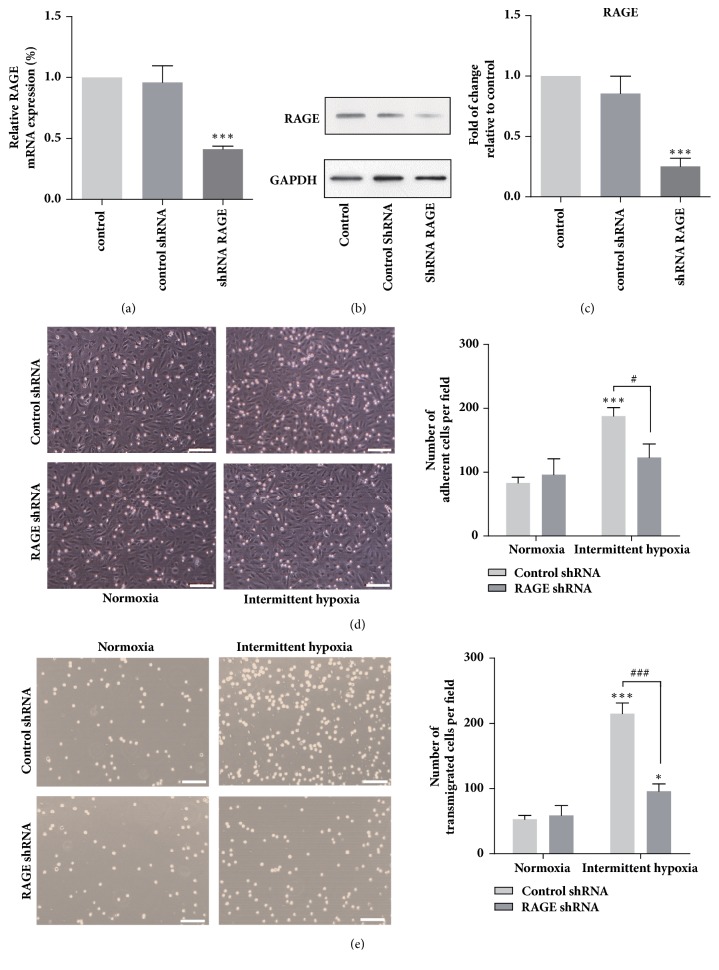
To investigate the role of RAGE in THP-1 cells, lentiviral shRNA targeting RAGE was introduced. We first verified that the RAGE shRNA lentiviral particles significantly inhibited the mRNA expression (Figure 2(a)) and protein expression levels of RAGE in THP-1 cells compared with the cell treated by control shRNA (Figures 2(b) and 2(c)). These results demonstrated that the RNAi strategies were effective. It has been established that the adhesion of monocytes to the vascular endothelial cells triggered by MCP-1 contributes to the early development of atherosclerosis [10]. In addition, monocyte chemotactic protein-1 (MCP-1) is responsible for the recruitment of monocytes, which is abundantly present in macrophage-rich atherosclerotic plaques [11, 12]. Therefore, the adhesion of monocytes to the endothelia activated with MCP-1 and the chemotaxis of treated THP-1 monocytes toward MCP-1 in IH was examined. To investigate the adhesion of THP-1 cells to endothelium, the cells were first stimulated by MCP-1 and then adhesion assay was conducted under normoxia or IH. We observed that IH exposure led to an approximately 90% increase in the number of the THP-1 cell adhered to endothelial cells while RAGE knockdown markedly reduced the IH-induced upregulation of cell adhesion (Figure 2(d)). It is further showed in Figure 2(e) that IH promoted the chemotaxis of THP-1 cells toward MCP-1 with the number of cells successfully migrated through the transwell membrane increased by approximately 3-fold compared with cells in normoxia. Furthermore, knockdown of RAGE reduced the number of migrated cells exposed to IH by around 55%.
Figure 2.
RAGE knockdown inhibited chemotaxis and adhesion of THP-1 cells exposed to intermittent hypoxia. Knockdown of RAGE in THP-1 cells was verified via qRT-PCR (a) and western blotting (b and c). Representative images with quantification of the results for THP-1 cells (d) transwell migration assay and adhesion assay (e) in presence of MCP-1. Data were represented as mean + SEM. ∗ represents significant difference compared with untreated cells under normoxia condition; ∗/#p<.05, ∗∗∗/###p<.001. Scale bars indicate 100 μm.
3.3. Intermittent Hypoxia Promoted CCR2 Expression via RAGE, Which Mediated Adhesion and Chemotaxis of THP-1 Monocytes
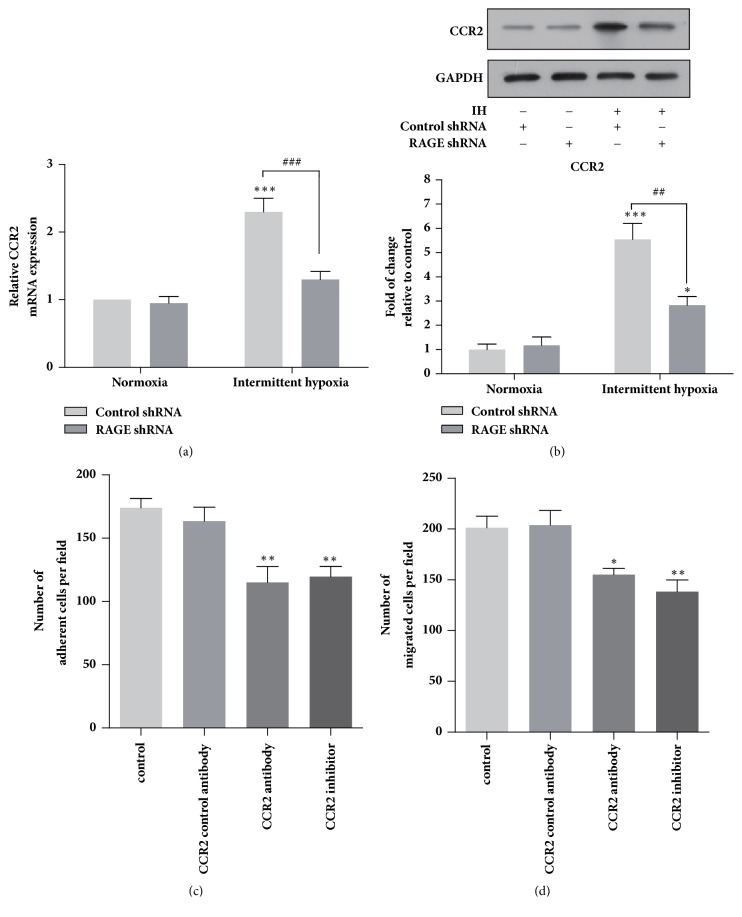
Chemokines and their receptors are responsible for the attraction, chemotaxis, and adhesion of monocytes that trigger the development of atherosclerosis [10]. Among the chemokine receptors, chemokine receptor type 2 (CCR2) is expressed in almost all circulating monocytes, which plays an essential role for the chemotaxis of monocytes toward the inflamed sites. We observed that both mRNA and protein expression level of CCR2 were significantly increased in THP-1 monocytes when cultured under IH (Figures 3(a) and 3(b)). Moreover, knockdown of RAGE markedly reduced IH-induced CCR2 expression in THP-1 cells. In order to determine the role of CCR2 in IH-induced monocyte adhesion and migration, we further treated the THP-1 cell with CCR2 neutralizing antibody (10 μg/m) or CCR2 inhibitor (10 nM) for 1 h prior to chemotaxis and adhesion assays. As showed in Figures 3(c) and 3(d), the monocyte adhesion to HUVECs promoted by IH was significantly downregulated by blocking CCR2 with CCR2 neutralizing antibodies and inhibitor. Similarly, the migration of THP-1 cells was reduced by approximately 30 and 42% with CCR2 antibodies and inhibitor treatment, respectively, compared with cells only exposed to IH.
Figure 3.
Intermittent hypoxia promoted CCR2 expression via RAGE, which mediated chemotaxis and adhesion of THP-1 cells. Expression levels of CCR2 in THP-1 cells exposed to normoxia and intermittent hypoxia determined by qRT-PCR (a) and western blotting (b). The effects of CCR2 neutralizing antibody (10 μg/m) and CCR2 inhibitor (10 nM) on (c) the adhesion of THP-1 monocytes to HUVECs and the cell transwell migration (d). Data were represented as mean + SEM. ∗ represents significant difference compared with control group under normoxia condition; ∗p<.05, ∗∗/##p<.001, ∗∗∗/###p<.001.
3.4. RAGE Plays an Indispensable Role in THP-1 Macrophages Polarization in Intermittent Hypoxia Condition
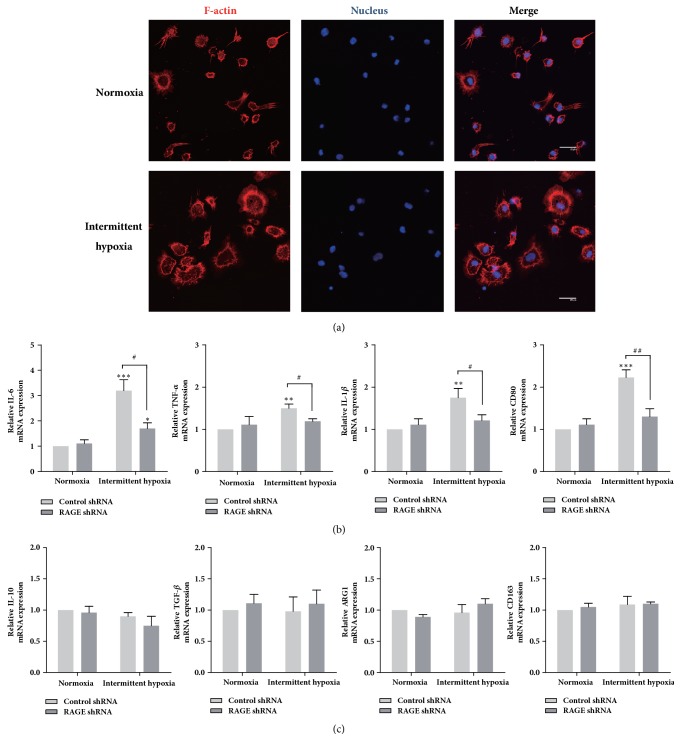
M1 macrophage releases higher level of TNF-α, IL-1β, IL-6 with higher expression of clusters of differentiation CD80, while M2 macrophage expresses higher level of IL-10, TGF-β, arginase 1 (ARG1), and CD163. In order to investigate the effect of RAGE on macrophage polarization, THP-1 monocytes were first treated with PMA, which activates protein kinase C (PKC) and induces macrophage differentiation [17], to acquire phenotypic and functional characteristics that resemble those of primary macrophages. As showed by the representative images of THP-1 macrophage (Figure 4(a)), there were dramatic changes in cell morphology after exposure to IH, which caused the cells to spread and flatten into a round and pancake-like shape suggesting the maturation of THP-1 macrophages. Our qPCR results also showed that IH substantially and significantly enhanced the expression of M1 markers in THP-1 macrophages. Most significantly, IL-6 mRNA expression was increased by approximately 3.2-fold following IH. TNF-α, IL-1β, and CD80 expression was also upregulated by around 40%, 75%, and 120%, respectively, versus normoxia group (Figure 4(b)). However, we did not observe any significant changes in the expression of M2 macrophage markers (Figure 4(c)). Furthermore, as shown in Figure 4(b), IH-induced M1 polarization was markedly attenuated by knockdown of RAGE. Additionally, the expression of IL-10 mRNA level was slightly decreased in RAGE shRNA-treated cells, although this effect was not statistically significant (Figure 4(c)).
Figure 4.
Intermittent hypoxia polarizes macrophages to an M1 phenotype, which was mediated by RAGE. (a) Morphology of THP-1 macrophage cultured in normoxia or IH. F-actin cytoskeleton of the cells were labelled with phalloidin (red) and nuclei stained with DAPI (blue). Scale bar: 20 μm. (b) mRNA expression levels of M1 expression markers. (c) mRNA expression levels of M2 expression markers. ∗ represents significant difference compared with control group under normoxia condition; ∗p<.05, ##p<.001, ∗∗∗/###p<.001.
4. Discussion
In spite of the importance of OSA in cardiovascular diseases development, the mechanisms of IH-induced atherosclerosis were not fully understood. There have been growing evidences to support the hypothesis that IH induces atherosclerosis in vivo [5, 18, 19]. Previous in vitro studies have also revealed that IH activates macrophage and affects macrophage polarization. For example, IH induces lipid-laden macrophages (foam cells) formation in murine macrophages by activating the IKK-β-dependent NF-κB pathway [20]. In addition, IH leads to significant increase in IL-6 expression in macrophages and promotes M1 macrophage polarization [21], which reveal the mechanisms by which OSA enhances inflammation and fibrosis in patients with fatty liver disease, while it has been shown that tumor-associated macrophages (TAMs) exhibit reductions in M1 macrophage markers in IH-exposed tumors [22]. Further, our results indicate that IH enhances monocyte adhesion and chemotaxis and promotes M1 macrophage polarization, which unravelled the relation between OSA and monocyte/macrophage recruitment and activation.
Firstly, we revealed that IH exposure promoted the activation of RAGE in THP-1 monocytes. This is in line with the report that AGEs level is increased in OSA condition, which enhances the expression and activation of RAGE [6]. RAGE activates many downstream signalling pathways, among which NF-κB is known as the most critical one [23]. As expected, IkB proteins, as the key inhibitor of the NF-κB pathway, were downregulated and NF-κB activity was increased (Figures 1(c) and 1(d)). Additionally, it has been suggested that NF-κB promotes the transcription of some inflammation factors including the RAGE [24]. Thus we treated the THP-1 cells with NF-κB siRNA and observed that inhibition of NF-κB significantly reduced IH-induced upregulation of RAGE expression at protein levels. Therefore, these results demonstrated that NF-κB pathway played an important role in IH-induced RAGE upregulation in THP-1 monocytes.
It has been documented that IH exposure induces foam cell formation in the THP-1 cells [20]. In addition, monocytes adhesion and transendothelial migration paly an indispensable role in the foam cell formation in vivo. How monocytes adhesion and migration would be altered by IH and the key regulators in this process remain largely unknown. In this study, we demonstrated that IH dramatically promoted the adhesion of THP-1 cells to endothelia cells. In addition, chemotaxis ability of THP-1 cells was significantly enhanced by IH. Moreover, we revealed that RAGE played a central role in the IH-induced THP-1 cells adhesion and migration. These results suggested that monocytes exposed to IH could be more easily adhered to endothelial cells and transmigrate into the subendothelium, which would directly trigger the formation of atherosclerotic plaque in OSA patients. CCR2, which is expressed in almost all circulating monocytes, regulates the chemotaxis of monocytes and the pathogenesis of various inflammatory diseases [25]. It was intriguing for our study to unravel the increase of CCR2 expression and its essential role in regulating the adhesion and chemotaxis of THP-1 cells exposed to IH. These findings are consistent with the report that CCR2 gene expression and macrophage infiltration in carotid body were increased in rat exposed to chronic intermittent hypoxia [26].
The leukocyte response to IH in vitro was not restricted to cell adhesion and migration. Atherosclerotic lesions are also associated with an increase of M1 macrophages expressing proinflammatory markers in the atherosclerotic plaque [27]. We observed the proinflammatory M1 macrophage polarization in IH. This finding provides the evidence for how IH promotes inflammation via enhancing the formation of activated M1 macrophages in patients with OSA. Previous studies have shown that RAGE activation promotes macrophages to secret proinflammatory cytokines [28], such as IL-1β, IL-6, and TNF-α, while the role of RAGE on macrophage polarization remains unknown. In this study, we further found that knockdown of RAGE significantly attenuated gene expression of M1 markers of THP-1 macrophages exposed to IH. Therefore, our data proved that IH induced M1 macrophage polarization, which was mediated by RAGE signalling.
The present study indicated that IH enhanced monocytes adhesion and chemotaxis and promoted macrophage polarization toward a proinflammatory M1 phenotype, which was mainly mediated by RAGE activity. These results strongly suggest an important role of RAGE in the cardiovascular diseases of severe OSA patients and provide a promising strategy to prevent atherosclerosis development in patients with OSA.
Acknowledgments
This study was supported by the project of National Natural Science Foundation of China (no. 81360017).
Data Availability
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors have declared that no conflicts of interest exist.
Authors' Contributions
Jing Zhou and Wei Bai contributed equally to this work.
References
- 1.Epstein L. J., Kristo D., Strollo P. J., Jr., et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Journal of Clinical Sleep Medicine. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 2.Senaratna C. V., Perret J. L., Lodge C. J., et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Medicine Reviews. 2016 doi: 10.1016/j.smrv.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Drager L. F., Polotsky V. Y., Lorenzi-Filho G. Obstructive sleep apnea: an emerging risk factor for atherosclerosis. CHEST. 2011;140(2):534–542. doi: 10.1378/chest.10-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savransky V., Nanayakkara A., Li J., et al. Chronic intermittent hypoxia induces atherosclerosis. American Journal of Respiratory and Critical Care Medicine. 2007;175(12):1290–1297. doi: 10.1164/rccm.200612-1771OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song D., Fang G., Mao S. Z., et al. Chronic intermittent hypoxia induces atherosclerosis by NF-κB-dependent mechanisms. Biochimica et Biophysica Acta. 2012;1822(11):1650–1659. doi: 10.1016/j.bbadis.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Tan K. C. B., Chow W.-S., Lam J. C. M., et al. Advanced glycation endproducts in nondiabetic patients with obstructive sleep apnea. SLEEP. 2006;29(3):329–333. doi: 10.1093/sleep/29.3.329. [DOI] [PubMed] [Google Scholar]
- 7.Basta G., Lazzerini G., Massaro M. Advanced glycation end products activate endothelium through signal-transduction receptor RAGE: a mechanism for amplification of inflammatory responses. Circulation. 2002;105(7):816–822. doi: 10.1161/hc0702.104183. [DOI] [PubMed] [Google Scholar]
- 8.Coughlan M. T., Thorburn D. R., Penfold S. A., et al. Rage-induced cytosolic ROS promote mitochondrial superoxide generation in diabetes. Journal of the American Society of Nephrology. 2009;20(4):742–752. doi: 10.1681/asn.2008050514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tafani M., Schito L., Pellegrini L., et al. Hypoxia-increased RAGE and P2X7R expression regulates tumor cell invasion through phosphorylation of Erk1/2 and Akt and nuclear translocation of NF-κB. Carcinogenesis. 2011;32(8):1167–1175. doi: 10.1093/carcin/bgr101. [DOI] [PubMed] [Google Scholar]
- 10.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362(6423):801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 11.Amasyali B., Kose S., Kursaklioglu H., Barcin C., Kilic A. Monocyte chemoattractant protein-1 in acute coronary syndromes: Complex vicious interaction. International Journal of Cardiology. 2009;136(3):356–357. doi: 10.1016/j.ijcard.2008.04.080. [DOI] [PubMed] [Google Scholar]
- 12.Tieu B. C., Lee C., Sun H., et al. An adventitial IL-6/MCP1 amplification loop accelerates macrophage-mediated vascular inflammation leading to aortic dissection in mice. The Journal of Clinical Investigation. 2009;119(12):3637–3651. doi: 10.1172/jci38308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leitinger N., Schulman I. G. Phenotypic polarization of macrophages in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2013;33(6):1120–1126. doi: 10.1161/atvbaha.112.300173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parisi Luca, Gini Elisabetta, Baci Denisa, et al. Macrophage Polarization in Chronic Inflammatory Diseases: Killers or Builders? Journal of Immunology Research. 2018;2018:25. doi: 10.1155/2018/8917804.8917804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu L., Wang Y.-R., Li P.-C., Feng B. Advanced glycation end products increase lipids accumulation in macrophages through upregulation of receptor of advanced glycation end products: Increasing uptake, esterification and decreasing efflux of cholesterol. Lipids in Health and Disease. 2016;15(1, article no. 161) doi: 10.1186/s12944-016-0334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bai W., Zhou J., Zhou N., et al. Hypoxia-increased RAGE expression regulates chemotaxis and pro-inflammatory cytokines release through nuclear translocation of NF-κB and HIF1α in THP-1 cells. Biochemical and Biophysical Research Communications. 2018;495(3):2282–2288. doi: 10.1016/j.bbrc.2017.12.084. [DOI] [PubMed] [Google Scholar]
- 17.Asseffa A., Dickson L. A., Mohla S., Bremner T. A. Phorbol myristate acetate-differentiated THP-l cells display increased levels of MHC class I and class II mRNA and interferon-γ-inducible tumoricidal activity. Oncology Research : Featuring Preclinical and Clinical Cancer Therapeutics. 1993;5(1):11–18. [PubMed] [Google Scholar]
- 18.Jun J., Reinke C., Bedja D., et al. Effect of intermittent hypoxia on atherosclerosis in apolipoprotein E-deficient mice. Atherosclerosis. 2010;209(2):381–386. doi: 10.1016/j.atherosclerosis.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang G., Song D., Ye X., Mao S.-Z., Liu G., Liu S. F. Chronic intermittent hypoxia exposure induces atherosclerosis in ApoE knockout mice: role of NF-κB p50. The American Journal of Pathology. 2012;181(5):1530–1539. doi: 10.1016/j.ajpath.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 20.Imamura T., Poulsen O., Haddad G. G. Intermittent hypoxia induces murine macrophage foam cell formation by IKK-β-dependent NF-κB pathway activation. Journal of Applied Physiology. 2016;121(3):670–677. doi: 10.1152/japplphysiol.00307.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schaefer E., Wu W., Mark C., et al. Intermittent hypoxia is a proinflammatory stimulus resulting in IL-6 expression and M1 macrophage polarization. Hepatology Communications. 2017;1(4):326–337. doi: 10.1002/hep4.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almendros I., Wang Y., Becker L., et al. Intermittent hypoxia-induced changes in tumor-associated macrophages and tumor malignancy in a mouse model of sleep apnea. American Journal of Respiratory and Critical Care Medicine. 2014;189(5):593–601. doi: 10.1164/rccm.201310-1830OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soro-Paavonen A., Watson A. M. D., Li J., et al. Receptor for advanced glycation end products (RAGE) deficiency attenuates the development of atherosclerosis in diabetes. Diabetes. 2008;57(9):2461–2469. doi: 10.2337/db07-1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds P. R., Wasley K. M., Allison C. H. Diesel particulate matter induces receptor for advanced glycation end-products (RAGE) expression in pulmonary epithelial cells, and RAGE signaling influences NF-κB-mediated inflammation. Environmental Health Perspectives. 2011;119(3):332–336. doi: 10.1289/ehp.1002520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deshmane S. L., Kremlev S., Amini S., Sawaya B. E. Monocyte chemoattractant protein-1 (MCP-1): an overview. Journal of Interferon & Cytokine Research. 2009;29(6):313–326. doi: 10.1089/jir.2008.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lam S.-Y., Liu Y., Ng K.-M., et al. Chronic intermittent hypoxia induces local inflammation of the rat carotid body via functional upregulation of proinflammatory cytokine pathways. Histochemistry and Cell Biology. 2012;137(3):303–317. doi: 10.1007/s00418-011-0900-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chistiakov D. A., Bobryshev Y. V., Nikiforov N. G., Elizova N. V., Sobenin I. A., Orekhov A. N. Macrophage phenotypic plasticity in atherosclerosis: the associated features and the peculiarities of the expression of inflammatory genes. International Journal of Cardiology. 2015;184:436–445. doi: 10.1016/j.ijcard.2015.03.055. [DOI] [PubMed] [Google Scholar]
- 28.Pertyńska-Marczewska M., Kiriakidis S., Wait R., Beech J., Feldmann M., Paleolog E. M. Advanced glycation end products upregulate angiogenic and pro-inflammatory cytokine production in human monocyte/macrophages. Cytokine. 2004;28(1):35–47. doi: 10.1016/j.cyto.2004.06.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.