ABSTRACT
Background: Resident physicians are known to be infrequent reporters of patient safety events (PSE). Previous studies assessing barriers to resident PSE reporting have not considered possible cultural barriers faced by international medical graduates (IMG). This study aimed to assess the knowledge and attitudes of residents regarding PSE and possible barriers contributing to poor resident reporting.
Methods: A cross sectional survey of all house staff undergoing post-graduate residency training at two independent community hospital based academic medical centers was conducted through an online questionnaire. Sample case vignettes were created to assess the residents’ ability to identify safety events and classify them as near miss, adverse events or sentinel events and decide whether they were reportable.
Results: The Reporting of PSE increased significantly by year of residency training (p < 0.005), with time taken to file a PSE being the strongest perceived barrier. There was no difference in PSE reporting between IMG’s and non- IMG’s. We identified major knowledge gaps with only 73.9%, 79.6% and 94.3% of respondents correctly identifying sentinel events, adverse events, and near misses, respectively. 58.1% of respondents did not think near misses were reportable.
Conclusions: A lack of knowledge is the most important barrier towards PSE reporting. A different cultural background and lack of previous exposure to patient safety report by IMGs is not a significant barrier towards safety event reporting. In the short-term, it appears that focusing limited institutional resources on education rather than acculturation issues would have the greatest benefit.
KEYWORDS: Patient safety event reporting, patient safety, house staff, general hospital, medical residency, residency
1. Introduction
With their 1999 report, ‘To Err is Human: Building a Safer Health System’ and their 2001 follow-up, ‘Crossing the Quality Chiasm: A New Health System for 21st Century’, the Institute of Medicine exposed the issues of medical error and patient safety reporting directly to the public, leading to a practice and policy shift within healthcare organizations [1,2]. Since that time, patient safety events have been increasingly recognized as an opportunity to improve patient care and are an area of risk to health systems and providers, given the close attention paid in the media to high profile error events, e.g., those of Joan Rivers and Michael Jackson. With increased public awareness and accountability, multiple societies have been attempting to improve the reporting of such events, and there is a trend towards creating institutional processes to better collect patient safety data, and improve patient safety through root cause analysis [3–5]. Electronic portals are used across health care organizations to provide a formal platform for health care providers to report patient safety related events (PSEs). The goals of event reporting portals are to facilitate problem identification and mitigation of risk in order to minimize and prevent patient harm by gathering data regarding near misses and actual adverse events experienced by patients for teaching, accreditation, and oversight purposes [1]. In 2005, the Joint Commission created a taxonomy for patients safety events with the aim to standardize the lexicon and facilitate incorporation and assessment of patient safety data over time [6].
While systems to report adverse events continue to evolve, poor physician participation in the process is a persistent problem. Nyugen, et al., found only 1.7% of all adverse event reports were submitted by physicians (7). Schectman, et al., found 65% of 120 responding physicians had not reported any adverse events though 60% of respondents had come across 3 or more safety events in the previous one year [7,8]. Resident physicians are front-line providers in many health-care systems and are intimately involved in patient care. It would be reasonable to think that they would be involved or witness several patient safety events, either directly or indirectly. Schectman, et al., and Bump, et al., found trainees to have a more favorable perception of patient safety culture and higher reporting than senior physicians [8,9]. However, multiple studies have shown that residents are not frequent event reporters either. Kaldjian, et al. noted that residents are more likely to report hypothetical adverse events as compared to senior physicians; however, all groups still significantly under report these events using a formal safety reporting portal [10]. Salem, et al. compiled the results of resident event reporting across 26 US hospitals and >90,000 reported events and documented only a 1.4% reporting rate by resident trainees and senior physicians [11]. Similarly, Dunbar, et al., found 3% of event reports were filed by resident and faculty physicians [12]. Vohra, et al., optimistically hypothesized that exposure of house staff and medical students to adverse events and the institutional response to these events may decrease error reporting and willingness to adopt safety practices [13].
Rochester Regional Health contains two university-affiliated community teaching hospitals with ACGME-accredited residency programs. In preparation for site visits, patient safety surveys were performed at both hospitals. At Rochester General Hospital (RGH), a 528-bed hospital, residents had filed only 29 safety event reports in the preceding three years. During academic year 2016–17, residents and faculty at Unity Hospital, a 351-bed hospital, had submitted 22 out of 2133 patient safety reports. Discussion raised several possible reasons for poor participation in reporting process, ranging from lack of clarity on the reporting process and lack of belief in reporting system to fear of retribution to self and others. It was hypothesized that a significant number of the residents in both institutions were international medical graduates (IMG’s), and knowledge of patient safety principles and reporting expectations in this country might not have been part of their previous training. It was also felt that many of the residents came from a culture with a more defined hierarchy and either fear of reporting superiors or feeling that this showed a lack of respect was a possible contributing factor. On literature review, this is in line with a recent systematic review of 47 studies which concluded that IMG’s faced difficulties with a loss of status and less defined hierarchies with respect to their patients, staff and supervisors as compared to home countries [14]. As far as we are aware, no studies had looked at the cultural background of residents with respect to safety event reporting.
This study was conducted with a goal to assess the knowledge and attitudes regarding patient safety events (such as near misses, adverse events and sentinel events) among residents. Identification of gaps in knowledge and barriers to reporting could allow targeted interventions to bridge the gaps.
2. Materials and methods
This prospective cross-sectional survey was conducted at Rochester General and Unity Hospitals between May-Sept 2017. The study included all house staff currently undergoing post-graduate resident training as of Aug 1st, 2017 at RGH and Unity Hospital, Rochester, New York. Residents from internal medicine (58 residents and 5 chief residents), radiology (16), obstetrics and gynecology (16), dentistry (5) and podiatry (4) residency programs at RGH and internal medicine residency program at Unity Hospital (41) were included in the study. All residency programs across both hospitals are ACMGE accredited and provide education and other clinical experiences as outlined by ACMGE guidelines. All residents are evaluated for quality and risk management which is one of the core competencies proposed by ACGME. Considering the novelty of looking at the role of acculturation on PSE reporting, publication of findings was a strong possibility, and therefore it fell under the Common Rule of HSR 45 CFR 46 and an IRB approval was sought at the beginning of the study. The study was approved by Rochester Regional Health Institutional Review Board.
A thorough review of literature was conducted to find out the reasons for poor reporting among physicians already reported by previous authors. Our literature search revealed other studies where similar questionnaires were distributed amongst participants to gauge their knowledge regarding reporting PSE. Louis et al used a similar survey and graded their responses on a similar Likert scale with responses ranging from strongly disagree, disagree, strongly agree and agree [15]. Kaldjian et al explored residents’ views on patient safety across the specialties of internal medicine, general surgery, and diagnostic radiology, focusing on common themes and differences by conducting in-person interviews to ask questions similar to the questions that were asked in our survey [10]. The possible attitudes chosen from literature and our own discussions were set on a Likert scale to help measure this as ordinal data and a 10-question survey was designed. We designed our survey aiming to include all possible explanations to determine the cause for the discrepancy in PSE reporting by resident physicians. Apart from identifying the respondent’s perceived barriers to reporting, the questions assessed the respondent’s demographic data such as specialty, current level of training and medical school background. The collected demographic data was such that individual respondents could not be identified and they were given the choice of not disclosing their specialty, current level of training or gender.
Three sample case vignettes were created to assess the residents’ ability to identify safety events and classify them as near miss, adverse events or sentinel events and decide whether they were reportable or not. Draft questions were carefully reviewed by the Designated Institutional Officer/Associate CMO for Education as well as the Associate Director of Quality and Safety at Rochester General Hospital.
A survey was created online and the final questionnaire was emailed to all participants via their official Rochester Regional Health email addresses. Participation in the survey was voluntary and anonymous, and there were no incentives or disincentives for participation. Three reminders were sent at weekly intervals to all potential respondents.
We used simple descriptive statistics including frequency distribution tables and cross-tabulations to present our findings. The responses on the Likert scale were interpreted as seldom (0–25%), sometimes (26–50%), often (51–75%) or most of the time (76–100%). We used the Fischer’s exact test to compare responses. Statistical significance was defined as p-value <0.05. SPSS 25 software IBM version 25.0.0.0 was used to compile and tabulate the results.
3. Results
A total of 98 residents responded to the survey with an over-all response rate of 67.6%. The responses were almost uniformly distributed between first three years of residency training (29.6%, 30.6% and 30.6% respectively). 3% of respondents were from dentistry, 73% from internal medicine, 11% from OB/GYN, 2% from podiatry and 10% from radiology. Male and female distribution was 55.1% and 43.9% respectively. 70.4% where non-US citizens from international medical school, 13.3% were US citizens from international medical school and 16.3% where US citizens from American medical schools (Table 1).
Table 1.
Demographics of respondents.
| Respondent Demographics | |
|---|---|
| Resident Specialty | |
| Internal Medicine | 72 (73.47%) |
| Obstetrics and Gynecology | 11 (11.22%) |
| Dentistry | 3 (3.06%) |
| Podiatry | 2 (2.04%) |
| Radiology (including both diagnostic and Interventional) | 10 (10.20%) |
| Total | 98 |
| Year of training | |
| PGY1 | 29 (29.59%) |
| PGY2 | 30 (30.61%) |
| PGY3 | 30 (30.61%) |
| PGY4 | 8 (8.16%) |
| PGY5 & Up | 1 (1.02%) |
| Total | 98 |
| Citizenship/Country of medical school | |
| USA medical graduate | 16 (16.33%) |
| USA Citizen- international medical graduate | 13 (13.27%) |
| Non-USA Citizen international medical graduate | 69 (70.41%) |
| Total | 98 |
| Self-identified gender | |
| Male | 54 (55.10%) |
| Female | 43 (43.88%) |
| Prefer not to answer | 1 (1.02%) |
| Total | 98 |
| Career plans after graduation | |
| Pursue office based practice | 8 (8.25%) |
| Pursue hospital based practice | 34 (35.05%) |
| Pursue further subspecialty training | 55 (56.70%) |
| Total | 97 |
Among the respondents who had reported PSEs, 80.8% residents had submitted 1 to 2 patient safety reports, 3.8% had submitted 3 to 4 patient safety reports and 3.8% had >5 patient safety reports (Table 2). The barriers to reporting PSEs were expressed on a Likert scale as seldom (0–25%), sometimes (26–50%), often (51–75%) or most of the time (76–100%). We considered any response greater than 0–25% (seldom) as a significant barrier for our study.
Table 2.
Percentage of respondents in different years of training who have submitted a safety event report.
| Submitted a PSE | Yes | % | No | % |
|---|---|---|---|---|
| PGY1 | 1 | 3.4% | 28 | 96.6% |
| PGY2 | 9 | 30.0% | 21 | 70.0% |
| PGY3 | 10 | 33.3% | 20 | 66.7% |
| PGY4 | 6 | 75.0% | 2 | 25.0% |
| PGY5 | 0 | 0.0% | 1 | 100.0% |
Based on this cut-off, time taken to submit a patient safety event was the most cited barrier, reported by 79.5% of the respondents. 59.2% of residents expressed uncertainty about how to submit a patient safety report. 51.7% of respondents expressed uncertainty regarding what is considered as a patient safety event. A lack of perceived change after reporting a PSE proved to be a barrier for 66.3% of the respondents while 64.8% of were concerned that a reported medical error could be seen as a sign of incompetence. A fear of violating hierarchy was a barrier for 59.3% of respondents while 54.5% felt increased scrutiny threatens autonomy. A fear of retribution to others was perceived as a barrier more often than a fear of retribution to self, by 46.1% and 56.2% of the respondents respectively (Figure 1).
Figure 1.
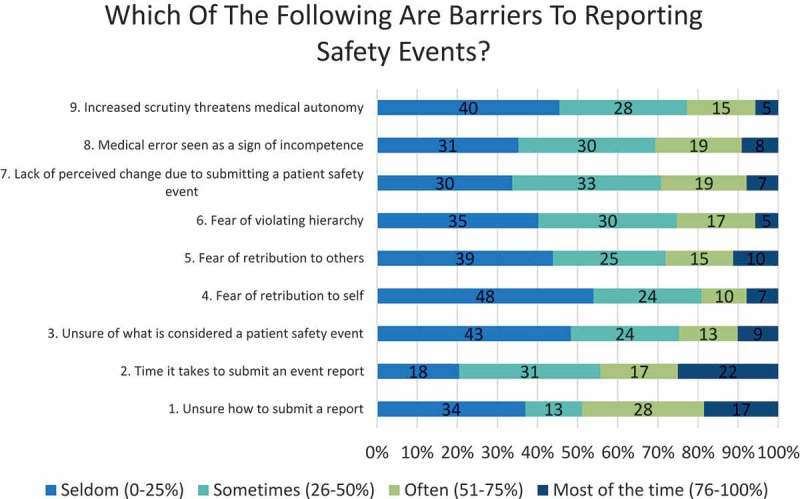
Barriers to safety event reporting.
While 94.3% of residents were able to correctly identify a near miss, only 73.9% and 79.6% of respondents who answered the vignettes, were able to correctly identify an adverse event or a sentinel event (Table 3). All respondents (100%) would report a sentinel event, even if they did not correctly recognize it as a sentinel event. However, 25.6% of the respondents who answered the vignettes, did not think an adverse event was reportable, while more than half (58.1%) did not think near misses were reportable (Figure 2).
Table 3.
Clinical vignettes to assess knowledge of sentinel events, adverse events and near misses.
| 1. Patient is admitted to the medical service with severe symptomatic anemia. Patient is receiving the blood transfusion when he develops fevers, chills and hypotension. Blood transfusion is immediately stopped, and the blood products are again verified. It is noticed that the patient’s blood and the transfusion blood are not compatible. Patient becomes severely hypotensive, unresponsive and progresses to shock requiring intubation and transfer to the intensive care unit. Despite resuscitative efforts, patient expires (Sentinel event). |
| 2. 36 year old female with history of DVT/PE on warfarin comes to clinic for treatment of bacterial vaginosis. She is prescribed metronidazole. Patient presents to the emergency department with moderate-severe epistaxis and is found to have an INR of 6.5. She is observed overnight and discharged home the next day with a dose reduction for her warfarin (Adverse event). |
| 3. Radiologist is reviewing images when he is asked to review an emergency department image. He begins dictation of the read and impression, prior to signing the charge notices that he is in the wrong chart. He is able to correct the impression prior to finalizing the read and places the correct read in the correct chart (Near miss). |
Figure 2.

Percentage of residents correctly reporting safety events.
There was no significant difference in the number of safety events reported by American medical graduates and International medical graduates (p-value 0.88) nor was there any difference in their knowledge about what constitutes a safety event (p-value 0.30). There was however, a statistically significant difference between reporting and level of training, with a higher level corresponding to a higher likelihood of having filed a patient safety report (p-value 0.001) but there were no significant differences when other barriers and knowledge was compared between different PGY levels (Table 2 and Figure 3).
Figure 3.
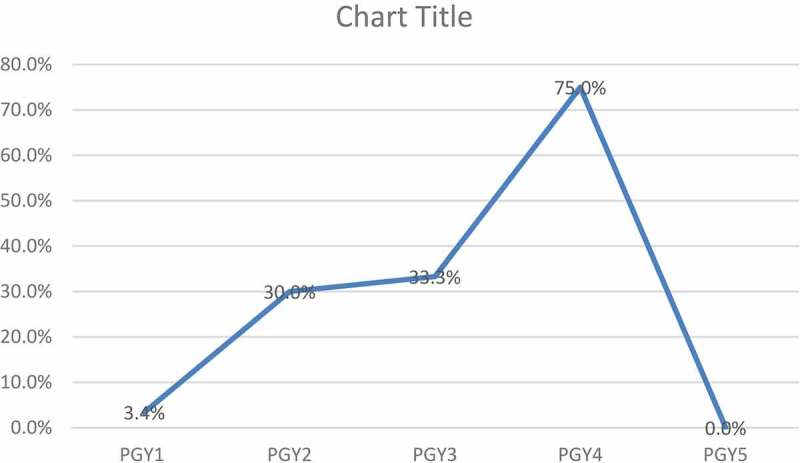
Improvement in safety events reporting with advancement in training: Percentage of respondents in different years of training who have reported a patient safety event.
4. Discussion
Previous studies exploring the causes of under-reporting by resident physicians found technical difficulties with the reporting process, limited amounts of time, fear of retribution and a personal knowledge gap regarding what qualifies as a reportable safety as common themes [16,17]. We tried to explore the factors behind poor reporting at our institution with the aim of designing future targeted interventions to improve the resident participation in safety event reporting.
Previous authors have commented on the differences between international medical graduates and US medical graduates and the cultural challenges faced by non-US trained medical graduates in terms of communication skills, knowledge of the working of the system and support system [18–21]. Similar to these previous studies, we had hypothesized that the attitudes towards hierarchy and a culture of ‘not creating noise’ among international medical graduates, who form a significant portion of residents, may partly be responsible for the low level or reporting at our institutions. This assumes significance as one in four practicing physicians in the US are graduates of medical schools in other countries and may help fill critical gaps in the health system. However, no significant difference was found between adverse event reporting by international medical graduates and US graduates. Therefore, the problem of not reporting safety events is not unique or restricted to IMG’s and targeting interventions at this population is unlikely to change overall knowledge and reporting.
It has been assumed that a busy work flow and subsequent inability or lack of motivation to report would be an important barrier, as well. Time taken to file a safety report was indeed reportedas the strongest barrier, with almost 80% of respondents finding it to play a role more often than seldom. We did not find any significant difference in safety events reporting between residents in different specialties, some of which may be considered to have more opportunities to come across or report safety events. Therefore, targeting interventions based on time on task and opportunity to exposure in high volume specialties would likely not be successful in increasing reporting rates.
Unlike previous studies, we did not find in our resident population that a fear of retribution to self or others, fear of violating hierarchy, or fear of being considered incompetent to be a significant barrier to reporting. This may have been due to fear of answering the anonymous survey honestly or may have been secondary to the success of the system in creating a ‘just culture.’ Further study is needed to determine which of these diametrically-opposed possibilities is more accurate, but the finding highlights again that targeted interventions directed at potentially misguided cultural and educational expectations about IMG residents would be unlikely to be successful.
The respondents of the survey did not think that being unsure of what constitutes a safety event proved to be a barrier for them. However, 26.1% of respondents could not identify a sentinel event, while 20.5% and 5.7% of respondents could not identify an adverse event and near miss, respectively. While all respondents would report a sentinel event, adverse events and near misses were not thought to be reportable by 25.6% and 58.1% of respondents respectively. Thus, a respondent who correctly recognized a near miss, was still more likely to not report the event. This, in conjunction with a significant rise in safety events reporting with progression of level of training, suggests that poor knowledge about what constitutes a safety event and whether they are reportable or not may be one of the biggest factors playing a role amongst our respondents, regardless of their cultural and specialty background.
Our study may have been limited by the small sample size of the potential respondents (145 residents) and being limited to two centers across a single institution. A total of 98 residents responded to the survey with an over-all response rate of 67.6%. About 1/3rd of our intended survey population did not respond to the survey. Reasons for lack of participation were not looked into but may include lack of time to participate due to busy rotations, not checking their emails frequently or simply unwillingness to participate in a survey. It can be speculated that exclusion of the 1/3 non-participants may have potentially skewed our results. However, our responses were almost uniformly distributed between first three years of residency training (29.6%, 30.6% and 30.6% respectively) and we had participation across 5 different sub-specialties with similar findings regarding physician reporting of PSE which makes us believe that the data truly reflects the results from our institutions. Our respondents also included 16 American medical graduates and 13 US citizen IMG’s (16.3 and 13.3% respectively) adding to almost 30% of respondents, and likely provide a healthy comparison to IMG respondents. Residents from General surgery and anesthesia, two specialties noted for their safety efforts, were not part of the study, which could have skewed the results [22,23]. However, we did include residents from obstetrics and gynecology, a specialty believed to have a strong safety culture and found to report the most near- misses on review of English National Reporting and Learning System Data, and did not find any significant difference in reporting [24].
5. Conclusion
Our study shows that a lack of knowledge seems to be the most important barrier towards safety event reporting. The lack of knowledge extends to both recognizing safety events correctly and understanding the need to report them. Our study shows that a different cultural background and lack of previous exposure to patient safety report by IMGs is not a significant barrier towards safety event reporting.
In the absence of findings other than knowledge-based deficits, we agree with the suggestions of Fox., et al., and Louis, et al., and recommend that, in the short-term, programs follow and invest their limited institutional resources for training in case-based educational modules to have the greatest benefit [15,25].These methodologies have been shown to increase resident participation in event reporting, and, until larger scale multi-center studies are performed, remain the best available evidence for improving resident reporting of patient safety events.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental Material
Supplemental data for this article can be accessed here.
References
- [1].Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is human: building a safer health system (Vol. 627). Washington (DC); 2000. [PubMed] [Google Scholar]
- [2].Committee on Quality Health Care in America, Institute of Medicine.Crossing the quality Chasm: a new health system for the 21st century. Washington (DC); 2001. [Google Scholar]
- [3].Davila Torres J.To err is human, but to not put processes in place to avoid errors from becoming fatal is inhumane. 5th international summit of the patient safety movement (PSM), California, USA, 2017. Cir Cir. 2017Mar-Apr;85(2):101–103. . PubMed PMID: 28325209. [DOI] [PubMed] [Google Scholar]
- [4].Hinkel JM. Report on the NCCN third annual patient safety summit. J Natl Compr Canc Netw. 2008July;6(6):528–535. quiz 534-5 PubMed PMID: 18597708. [DOI] [PubMed] [Google Scholar]
- [5].McCarter TG, Centafont R, Daly FN, et al. Reducing medication errors: a regional approach for hospitals. Drug Saf. 2003;26(13):937–950. PubMed PMID: 14583069. [DOI] [PubMed] [Google Scholar]
- [6].Chang A, Schyve PM, Croteau RJ, et al. The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care. 2005April;17(2):95–105. PubMed PMID: 15723817. [DOI] [PubMed] [Google Scholar]
- [7].Nguyen QT, Weinberg J, Hilborne LH. Physician event reporting: training the next generation of physicians In: Henriksen K, Battles JB, Marks ES, et al editors. Advances in patient safety: from research to implementation (volume 4: programs, tools, and products). Advances in patient safety. Rockville (MD); 2005. [Google Scholar]
- [8].Schectman JM, Plews-Ogan ML. Physician perception of hospital safety and barriers to incident reporting. Jt Comm J Qual Patient Saf. 2006June;32(6):337–343. PubMed PMID: 16776388. [DOI] [PubMed] [Google Scholar]
- [9].Bump GM, Coots N, Liberi CA, et al. Comparing trainee and staff perceptions of patient safety culture. Acad Med. 2017January;92(1):116–122. PubMed PMID: 27276009. [DOI] [PubMed] [Google Scholar]
- [10].Kaldjian LC, Jones EW, Wu BJ, et al. Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med. 2008January14;168(1):40–46. PubMed PMID: 18195194. [DOI] [PubMed] [Google Scholar]
- [11].Milch CE, Salem DN, Pauker SG, et al. Voluntary electronic reporting of medical errors and adverse events. An analysis of 92,547 reports from 26 acute care hospitals. J Gen Intern Med. 2006February;21(2):165–170. PubMed PMID: 16390502; PubMed Central PMCID: PMCPMC1484668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dunbar AE 3rd, Cupit M, Vath RJ, et al. An improvement approach to integrate teaching teams in the reporting of safety events. Pediatrics. 2017February;139(2). PubMed PMID: 28123045 DOI: 10.1542/peds.2015-3807. [DOI] [PubMed] [Google Scholar]
- [13].Vohra PD, Johnson JK, Daugherty CK, et al. Housestaff and medical student attitudes toward medical errors and adverse events. Jt Comm J Qual Patient Saf. 2007August;33(8):493–501. PubMed PMID: 17724946. [DOI] [PubMed] [Google Scholar]
- [14].Michalski K, Farhan N, Motschall E, et al. Dealing with foreign cultural paradigms: A systematic review on intercultural challenges of international medical graduates. PLoS One. 2017;12(7):e0181330 PubMed PMID: 28715467; PubMed Central PMCID: PMCPMC5513557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Louis MY, Hussain LR, Dhanraj DN, et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016Spring;16(1):73–80. PubMed PMID: 27046410; PubMed Central PMCID: PMCPMC4795509. [PMC free article] [PubMed] [Google Scholar]
- [16].Boike JR, Bortman JS, Radosta JM, et al. Patient safety event reporting expectation: does it influence residents’ attitudes and reporting behaviors? J Patient Saf. 2013June;9(2):59–67. PubMed PMID: 23697981. [DOI] [PubMed] [Google Scholar]
- [17].Jericho BG, Tassone RF, Centomani NM, et al. An assessment of an educational intervention on resident physician attitudes, knowledge, and skills related to adverse event reporting. J Grad Med Educ. 2010June;2(2):188–194. PubMed PMID: 21975618; PubMed Central PMCID: PMCPMC2941378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gozu A, Kern DE, Wright SM. Similarities and differences between international medical graduates and U.S. medical graduates at six Maryland community-based internal medicine residency training programs. Acad Med. 2009March;84(3):385–390. . PubMed PMID: 19240453. [DOI] [PubMed] [Google Scholar]
- [19].Hall P, Keely E, Dojeiji S, et al. Communication skills, cultural challenges and individual support: challenges of international medical graduates in a Canadian healthcare environment. Med Teach. 2004March;26(2):120–125. PubMed PMID: 15203520. [DOI] [PubMed] [Google Scholar]
- [20].Meghani SH, Rajput V. Perspective: the need for practice socialization of international medical graduates–an exemplar from pain medicine. Acad Med. 2011May;86(5):571–574. . PubMed PMID: 21436666. [DOI] [PubMed] [Google Scholar]
- [21].Zulla R, Baerlocher MO, Verma S. International medical graduates (IMGs) needs assessment study: comparison between current IMG trainees and program directors. BMC Med Educ. 2008August29;8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lanier WL. A three-decade perspective on anesthesia safety. Am Surg. 2006November;72(11):985–989. discussion 1021-30, 1133-48 PubMed PMID: 17120937. [DOI] [PubMed] [Google Scholar]
- [23].Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009January29;360(5):491–499. PubMed PMID: 19144931. [DOI] [PubMed] [Google Scholar]
- [24].Howell AM, Burns EM, Bouras G, et al. Can patient safety incident reports be used to compare hospital safety? Results from a quantitative analysis of the english national reporting and learning system data. PLoS One. 2015;10(12):e0144107 PubMed PMID: 26650823; PubMed Central PMCID: PMCPMC4674095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fox MD, Bump GM, Butler GA, et al. Making residents part of the safety culture: improving error reporting and reducing harms. J Patient Saf. 2017January30PubMed PMID: 28141697 DOI: 10.1097/PTS.0000000000000344. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


