ABSTRACT
Introduction: Only 12% of Americans have proficient health literacy (HL). Patients hide this fact from others including physicians. This quality improvement (QI) project was developed to compare internal medicine (IM) resident physicians’ (RPs) ability to accurately predict patients with low HL and to improve IM-RPs’ understanding of low HL and its impact on patients.
Aim statement: Over six-months, our aim was to increase the IM residents’ HL-knowledge by 30% as measured by an HL-Knowledge-Based-Survey.
Methods: After IRB exemption, patients visiting the residency-clinic within a two-week period were screened for low HL with the REALM-R, a validated tool. Post-visit, IM-RPs were asked to predict their patients’ HL. A comparison of predicted-HL and measured-HL was made. IM-RPs were emailed an HL-Knowledge-Based-Survey (pre-education and post-education) to measure their background knowledge of HL. Education included HL-workshop, pre-clinic conference and lectures. Pre-education and post-education scores were compared.
Results: HL-RPs’ prediction and patients’ REALM-R results were completed by 108 RP-patient pairs. IM-RPs correctly identified 5 of 40 patients who were at risk for low HL (sensitivity = 12.5%). They correctly identified 97.1% of 68 who were not at risk (specificity = 97.1%). Our residents’ knowledge pre-education and post-education did not improve – 58% (n = 18) vs 62% (n = 10).
Conclusion: Our QI result verified that IM-RPs overestimate patients’ HL and do not understand the magnitude or consequences of low HL nor techniques to improve such patients’ understanding. This suggests an area for residency curricular development in order to improve patients’ ability to navigate the healthcare system successfully.
KEYWORDS: Resident physicians, health literacy, education
1. Background
Health literacy (HL) is defined as ‘the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.’ [1]
Only 12% of Americans are found to have proficient HL, making this a monumental issue [2]. Medical terminology is a precise and efficient language for communication with other health professionals. However, it is often difficult for health professionals to ‘switch’ to lay language and they often comingle medical terminology in their patient education efforts. Further complicating the issue of low HL is health professionals’ lack of awareness. Consequently, poor HL, and absence of sufficient attention to it, often lead to adverse health-related outcomes including inability to adopt healthy behaviors, poor treatment adherence, medication errors, greater use of medical services (outpatient and ER visits, hospitalizations), less utilization of preventive services (mammograms, pap smears and vaccinations), adverse disease outcomes and increased mortality [3–5].
Based on our experience, many physicians, especially RPs, are not familiar with the concept of HL, and hence, they are unable to perceive or anticipate the needs of patients with low HL. Moreover, there is not enough focus in current graduate medical education curricula specifically addressing communication skills to overcome patients’ low HL. In addition, the literature shows that, even when aware of the concept of HL, RPs overestimate their patients’ HL skills and hence fail to tailor information according to their needs [6]. Low HL is a universal problem. The purpose of this QI project was to compare the ability of IM-RPs to accurately identify their patients with low HL as assessed by a validated tool [7]. We wanted to measure RPs’ baseline HL-knowledge and their understanding of the consequences of low HL, so we designed an evaluation instrument similar to the one used in the pharmacy literature for continuing education [8]. We also held teaching sessions including workshops and didactics on health literacy.
2. Methods
This multistep project was completed in our IM residency-clinic between February 2017 and July 2017 after IRB exemption. The project was completed in two parallel sections (Prediction section and Educational section). In the first section, we evaluated RPs’ ability to predict their continuity patients’ HL based upon our assumption and the literature that indicates RPs overestimate it [6]. We queried 113 RP-patient pairs in a 2-week interval (RP to patient ratio, 1:3–4), i.e. all patients who agreed to participate. Patients who presented in this non-consecutive 2-week period (convenience sample) completed a Patient-Visit-Questionnaire after obtaining a verbal consent. This questionnaire was administered to collect their perceived barriers to effective communication. In addition to their demographics (age, gender and educational status), we asked them, ‘How well can you understand your doctor?’ ‘Tell us what makes it difficult to understand your doctor.’ Before clinical interaction with RPs, patients were screened for their low HL risk with REALM-R (Rapid Estimate of Adult Literacy in Medicine-Revised) by medical assistants [7]. REALM-R, a short screening tool, has 8-word items; each item is scored with one point if pronounced correctly using a dictionary standard (maximum score 8, health illiterate if score ≤ 6). Based on the REALM-R score (used as a standard for HL-measurement), patients were labeled adequately or inadequately health literate. After this screening, there was a routine RP-patient encounter. Following this interaction, RPs were asked to predict their patients’ HL on a Resident-Questionnaire, ‘Do you think this patient is literate enough to understand and follow-through on his plan of care?’ They were also asked about their satisfaction with a specific clinical interaction using a rating scale, ‘How comfortable are you with this patient interaction?’ Later, a comparison of predicted (resident’s assessment) and measured-HL (REALM-R score) was made for each RP-patient pair. RPs received confidential feedback regarding their accuracy of HL-prediction to promote learning about, and sensitivity to, low-HL.
During the educational section of this QI project, RPs baseline and post-intervention knowledge of HL and its implications were assessed using an HL-Knowledge-Based-Survey (adapted from a pharmacy continuing education literature) [8], administered via Survey Monkey® during a pre-education and post-education phase. HL-Knowledge-Based-Survey was adapted from the survey or assessment found at the end of a review article written by Dr. Ngoh, an associate professor from the Ferris State University [8]. This survey comprising 20 multiple-choice questions assesses the knowledge and common facts of HL, ways of how to assess HL of a particular patient, identification or red flags of patients who are at risk for low HL, medication non-adherence issues and strategies to improve communication with patients of low HL. Our survey, though adapted from the same survey, contained 27 questions (multiple choice questions, true or false and brief open-ended questions) generated utilizing common literature facts including a definition of HL, risk factors, the prevalence of adequate and inadequate HL and its consequences. A cumulative pre-education score was generated by Survey Monkey®. Following pre-education scoring, RPs underwent an educational intervention spanning a period of 2-months comprising of various educational methods. Common educational modalities that have been used to teach health professionals about HL include workshops, didactics, small group-role play, video reviews, simulated patient encounters, direct observation, modeling, feedback and exposure to health illiterate (HI) individuals [9,10]. After disclosing the fact that our RPs lacked HL-knowledge, they underwent an HL-workshop, pre-clinic conference based upon discussion of an article whose target audience was pharmacists and multiple interactive lectures or QI presentations (performed by HL-QI team leader and team members). The HL-workshop was conducted by an HL-expert in an online video conference. The purpose of this HL-workshop was to provide RPs with a comprehensive overview of HL topic and give them basic information on its background, significance and implications. Apart from this, our QI involved three interactive lectures; those were performed as the part of residency-based interval QI workshops. These QI workshops are conducted by the faculty and are compulsory for all residents to attend. Each year, 4–6 QI projects are completed. Each project is supervised by one or two faculty members; QI team leaders are generally from second-year who work in close collaboration with their supervising faculty member. During these workshops, QI team leaders from each project discuss literature, background and significance of their project. The purpose of QI team leader is to educate other RPs and update IM faculty on their projects using Microsoft ® PowerPointTM presentations. After the end of each QI presentation, the questions are answered and feedbacks on QI projects are received. HL-project followed the same structure for their HL interactive lectures. In IM residency, pre-clinic conferences are an integral part of a usual continuity-clinic day that covers almost all RPs with only a few exceptions. HL-article was assigned to discuss in this pre-clinic conference for a one-week period. RPs participated in the discussion based on this article with their respective clinic attending on their respective clinic day before the clinical work was begun. Pre and post-education aggregate scores were compared. In a final QI presentation, anonymity was again maintained with the discussion of both knowledge-based and HL prediction results with the IM-RPs. (See Figure 1 for method section.)
Table 4.
Resident’s prediction of HL compared with actual HL (2x2 contingency table) †.
| Resident’s Prediction | Illiterate (REALM-R score ≤ 6) | Literate (REALM-R score ≥ 7) | Total |
|---|---|---|---|
| No (Patient is not literate) | 5 (True positive) | 2 (False positive) | 7 |
| Yes (Patient is literate) | 35 (False negative) | 66 (True negative) | 101 |
| Total | 40 | 68 | 108* |
| Sensitivity = 12.5% | Specificity = 97.1% | P-value = 0.09 |
†Fisher’s Exact Test was applied.
*Five patients refused to undergo REALM-R screen, total convenience sample 113.
3. Results
During the two-week prediction period, 113 patients presented in residency-clinic and completed the Patient-Visit-Questionnaire which included 53 men and 58 women (2 Patient-Visit-Questionnaires had missing gender information). Average age was 56, range 20–94 (13 Patient-Visit-Questionnaires had missing age information). Sixteen Patient-Visit-Questionnaire (14%) had missing educational level information. However, 65% of patients had reached 11th grade or higher. (See Table 1) The association of these demographic variables with literacy status as measured by REALM-R is shown in Table 2.
Table 1.
Demographic variables of 113 patients.
| Demographic variables | Number of Patients (%)* |
|---|---|
| Gender, n (%) | |
| Male | 53 (47) |
| Female | 58 (51) |
| Unreported† | 2 (2) |
| Age in years, n (%) | |
| Average Age | 56 |
| Range of Age | 94–20 |
| ≥ 50 | 74(66) |
| < 50 | 26 (23) |
| Unreported† | 13 (11) |
| Educational level, n (%) | |
| Advanced Degree | 5 (5) |
| Some College and Bachelor’s Degree | 38 (33) |
| 11th, 12th Grade, Completed High School | 38 (33) |
| ≤ 10th Grade | 16 (15) |
| Unreported† | 16 (14) |
*Percentages have been rounded off and do not represent the exact value.
†Patients did not report these variables.
Table 2.
Association of demographic variables with REALM-R.
| Demographic Variable | Literate | Illiterate | System missing values† | P-value (< 0.05) |
|---|---|---|---|---|
| Gender | 0.276 | |||
| Male | 31 | 21 | 5 | |
| Female | 39 | 17 | ||
| Total | 70 | 38 | ||
| Age | 0.969 | |||
| < 50 years | 16 | 10 | ||
| ≥ 50 years | 44 | 27 | 16 | |
| Total | 60 | 37 | ||
| Educational Status | 0.016* | |||
| ≤ 10th Grade | 3 | 8 | ||
| 11th, 12th Grade, completed High School | 23 | 17 | 19 | |
| Some College, Bachelor’s Degree | 27 | 11 | ||
| Advanced Degree | 5 | 0 | ||
| Total | 58 | 36 |
† 113 patients filled Patient-Visit-Questionnaire but not all the patients responded to all the questions. Similarly, REALM-R was refused by five patients. System missing values represent collective missing information on these variables.
*Statistical significant association between educational level and REALM-R. Pearson chi-square value is 10.326.
Majority of patients (59% of 80 respondents) perceived no communication barrier with their RPs whereas 41% reported perceiving ‘somewhat difficulty’ in understanding their doctor. Only 22 patients specified a reason for their inadequate understanding, the commonest reasons being doctor’s accent in 12 patients followed by other less common causes (see Table 3); 89% of our RPs had their primary language other than English. Seventeen patients had suggestions to promote effective communication.
Table 3.
Patient’s perceived barriers of communication.
| Perceived Communication Barriers | Number of Patients (%)* |
|---|---|
| How well can you understand your doctor? | |
| Non-respondents, n (%) | 33 (29) |
| Respondents, n (%)† | 80 (71) |
| I cannot understand most of what my doctor says. | 0 (0) |
| I cannot understand some of what my doctor says. | 3 (4) |
| I can understand most of what my doctor says. | 30 (37) |
| I can understand all of what my doctor says. | 47 (59) |
| Tell us what makes your doctor difficult to understand. | |
| Non-respondents, n (%) | 58 |
| Overall respondents, n (%) | 55 |
| Respondents for individual barriers, n (%)† | |
| No problem during communication | 33 (60) |
| Doctor’s accent | 10 (19) |
| Too many medical words | 2 (3.6) |
| Hearing problem | 2 (3.6) |
| Too much information | 2 (3.6) |
| Doctor talks too quietly | 2 (3.6) |
| Doctor’s accent and goes over information too quickly | 1 (1.8) |
| Doctor’s accent and talks too fast | 1 (1.8) |
| Doctor goes over information too quickly | 1 (1.8) |
| Lack of visual aids | 1 (1.8) |
| How can we help you to better understand your health? | |
| Non-Respondents, n (%) | 64 (57) |
| Respondents, n (%) | 49 (43) |
| No suggestion made by respondents, reported satisfaction | 32 (65) |
| Suggestions made for improvement | 17 (35) |
|
Suggestions included but not limited to: Ongoing communication, waiting time reduction, adequately extended but a precise explanation, medication rationale, sufficiently loud speech, understanding of patient’s social context, access to electronic health material, print out plan of care, and copies of labs. |
*Percentages have been rounded off to simplify figures and avoid confusion
†Percentages represent among respondents, the sum may not be exactly equal to 100%.
During HL screening, five patients refused to undergo REALM-R but stated no specific reason. Hence, 108 RP-patient pairs were available for comparison of predicted and measured HL. Of these 108 screened patients, REALM-R was positive in 40 patients, subsequently labeled as HI. Out of 40 HI patients, RPs were able to predict 5 patients accurately (true positive) (sensitivity of 12.5%, p-value = 0.09). Correspondingly, thirty-five patients were false negative and hence considered health literate by RPs. On the other hand, REALM-R screen was negative for 68 patients (health literate); RPs predicted 66 health literates (true negative) (specificity = 97%, p-value = 0.09, see Table 4)
During Resident-Questionnaire administration, either ‘Not Comfortable’ or ‘Somewhat Comfortable’ with communication was reported on Resident-Questionnaire for seven RP-patient pairs. For five other RP-patient interactions, RPs response was neutral (neither comfortable nor uncomfortable). The remaining interactions were reported without any difficulty (‘Very Comfortable’ or ‘Comfortable’) (Figure 2). There was no significant association of resident’s satisfaction during communication and REALM-R, p-value of 0.424.
Figure 1.
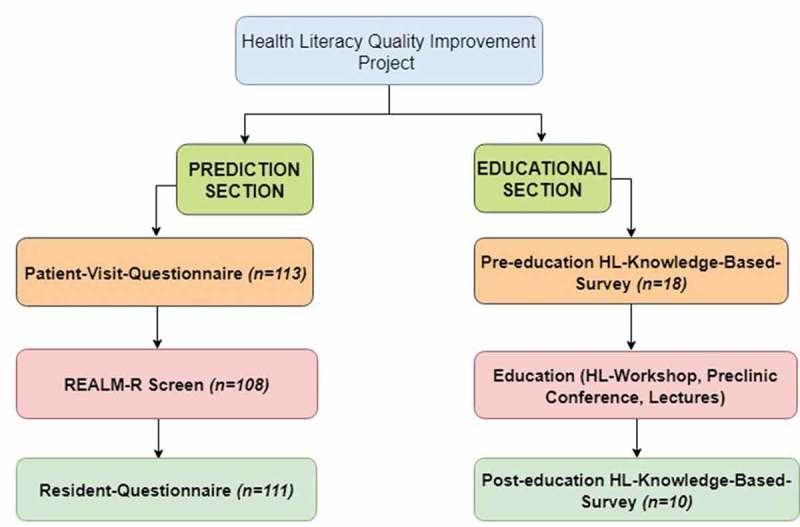
A schematic diagram showing methods of health literacy QI.
Figure 2.
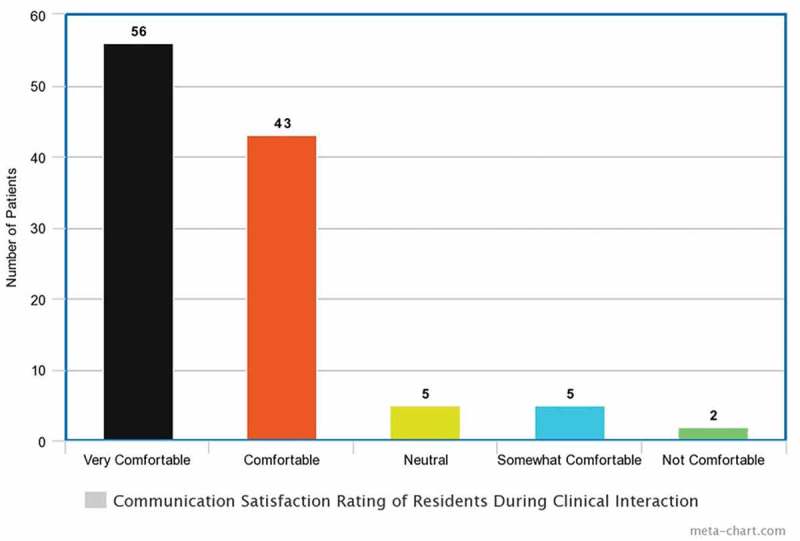
Resident satisfaction results in patient encounters.
RPs received an HL-Knowledge-Based-Survey as an online link in their emails; the survey was sent to all 35 IM-RPs irrespective of their training year (first and second years had 12 residents each whereas third-year had 11 residents, n = 35). The data was collected without identifiers to maintain their anonymity. Only 18 residents (51%) responded to the pre-intervention survey. The survey had 27 questions; each question had multiple options and more than one option was acceptable. Survey Monkey® generated a pre-education cumulative knowledge-based score of 58% for the 18 RPs. After the educational period of two months, the same HL-Knowledge-Based-Survey was administered. The survey was anonymous and voluntary; only ten RPs (29%) participated in the post-education survey. The post-education cumulative score generated by Survey Monkey® was 62%.
4. Discussion
Our study was designed to test RPs ability to predict health literacy of their patients and to determine knowledge-base of RPs pre-education and post-educational interventions. We found that there were a sensitivity and specificity of 12.5% and 97% respectively in RPs’ prediction of low HL compared to measured HL by REALM-R. RPs’ knowledge-base regarding HL was 58% (n = 18) and 62% (n = 10), pre and post-educational intervention, respectively, showing a low baseline HL knowledge-base with very little improvement.
Our residents identified 12.5% of illiterate patients correctly compared to 20% of the Louisville residents described by Bass et al. [6] In both cases there were a majority of patients who might have benefitted from special educational methods known to be effective with HI patients who probably did not receive that special attention. We attempted to improve our residents’ knowledge and understanding of low HL and gave them feedback about their poor predictive abilities, showing them how they could effectively and efficiently screen their patients for HL.
The literature shows that less than 50% of residency programs provide any formal education to residents to improve their knowledge of HL [11]. Of note, the methods of HL teaching are also not consistent among these training programs. This means there is an inevitable need to add it to the existing curricula of residency training. According to a survey completed by 33 residency program directors and associate program directors, commonly used methods to teach RPs include didactics or lectures, observations with feedbacks and role plays [11]. On the other hand, the least focus is on educating residents how to help patients with limited HL navigate through the health system so that they can make independent and appropriate health choices. Though the interpersonal and communication skills is a part of ACGME core competencies, there are no objective parameters which can help faculty measuring residents’ knowledge of HL or their communication skills with patients of inadequate HL [12]. According to Ali et al, the majority of faculty uses observation as the most common method of RPs assessment [11]. According to Powell et al, only a few medical trainees can find clues of low HL as a potential problem in a patient’s case history and even fewer know how to cope with such kind of situation [13]. Compared to residents, interns are more likely to miss this valuable information probably due to their lack of experience [13]. As our study did not collect residents’ demographics, we could not make such comparisons. This is to be noted that though residents could detect a patient with some literacy problem, they might just rely on written instructions as the only tool to cope with this problem [13]. This means they are unaware of other important supplemental techniques which will fulfill these patient’s requirements. One study queried medical trainees via a structured questionnaire regarding their confidence of HL-knowledge and their ability to accurately identify or communicate with HI patients and found that only less than 10% trainees were confident of their abilities and even less than 1.4% were confident enough to find appropriate HL-resources [14].
To date, many attempts have been made to incorporate the concept and skills of HL into residency training. However, still, there is a widespread need for its application in the practical world [13]. Adopting HL-skills is more than knowing the HL-concept and involves the implementation of strategies or behaviors which can foster clear communication with the patients of inadequate HL [10]. Our study provides an insight into the behavior of RPs as the first step toward the implementation of these behaviors or strategies required to compensate for their patient’s low HL. There is a statistically significant association between the REALM-R score and educational level. Therefore, the low educational level perhaps can be used as a red flag to alert physicians to make their communication more simplified and clearer, especially if more complicated and time-consuming tools are not possible.
In addition to the comparison of RPs’ prediction with REALM-R, this study examines the other aspects of the resident-patient relationship, i.e. residents’ satisfaction and patients’ satisfaction. Of 89% encounters, RPs were either comfortable or very comfortable. This means they perhaps faced no difficulty while interacting with these patients. Contrary to this, only 59% patients (out of 80 respondents) felt no communication problem whereas 41% felt somewhat difficulty in understanding and many of them had pointed to some specific problems with the communication (Table 3) and even suggested to resolve those issues with some extra help. In other words, though RPs might not perceive it, many patients might be perceiving communication barriers during the same clinical encounters.
This study also evaluated the knowledge-base of RPs via Survey Monkey® Though our goal was to improve RPs knowledge-base up to 30%, we failed to achieve that goal. There could be several reasons responsible for this failure. First, RPs might need multiple workshops conducted by HL-experts as they were naïve to the concept of HL. Second, the teaching should have been supplemented with diverse modalities such as videos, role plays and reflective writing. Third, the 2-month educational period might have been too short to provide us with the required knowledge-base change. Lastly, resident-related factors such as lack of interest or motivation might have played some role.
There are several limitations of our study. First, the sample size of RP-Patient pairs was small, and that might have impacted our ability to achieve a statistical significance (See Table 4). Nevertheless, our findings are educationally concerning, i.e. RPs ability to predict their patients’ low HL lacked sensitivity (12.5%). This means, more than 87% of HI-patients are likely to be neglected by RPs and this can result in negative health outcomes. Second, the lack of a validated instrument for measuring RPs’ knowledge about HL and its effects resulted in the developing of an instrument that has not been validated for that purpose. Nevertheless, our tool was similar to an instrument used to grant continuing education to pharmacists who read the article discussed in our pre-clinic conference, making the use of this instrument reasonable [7]. Third, our literature search did not show evidence that HL knowledge-base or behavior can be improved by educational interventions targeting health professionals. Fourth, in our study, the participation in the knowledge-based survey was low, approximately 50% pre-education, but dropped to only about 28% post-education with those RPs not necessarily representing the same physicians in a true pre and post-measurement. This presents an additional limitation in demonstrating a true change in RP knowledge-base. However, we have no reason to believe that representatives of the group who participated in the knowledge-based survey post-education, were less knowledgeable than the group at large. In fact, one could make a reasonable argument that those who were most confident in their knowledge-base improvement were most willing to take the knowledge-based test post-education. To our understanding, multiple modalities will be required to improve HL knowledge-base and validated tests will be needed to check the knowledge-base. Finally, even if knowledge base can be objectively documented by computer testing to show improvement after educational interventions, the more relevant question is whether physicians can effectively apply their HL knowledge-base in the real world with their patients to result in improvement of patient self-care behavior. We believe that a check-list of behaviors critical to bridging low HL can be developed and applied in a real-world context with RP-Patient pairs during video review in our clinic and propose this as the next phase of our project.
5. Conclusion
Our RPs were not accurate in predicting low HL in their own continuity patients. Furthermore, they had a low knowledge-base of this condition. Based on this, we can assume that they are not adapting their educational strategies for HI patients if they have not identified them, i.e. they do not recognize their patients’ needs for special educational strategies. Therefore, we believe that this unidentified patient population may be at risk for the poor health outcomes known to accrue to patients with low HL. And, finally, we believe that this is a widespread unaddressed need in graduate medical education.
Acknowledgments
Authors of this article used REALM-R for the assessment of patient’s health literacy. The permission was obtained for the use of REALM-R from the primary author. Dr. Pat F. Bass MD, MS III who designed and validated this instrument. The original article can be accessed and cited as Bass PF, Wilson JF, Griffith CH. A shortened instrument for literacy screening. Journal of general internal medicine. 1 December 2003;18(12):1036-8.REALM-R is available on various websites. This tool can be accessed here. http://adultmeducation.com/AssessmentTools_1.html
Authors also assessed the health literacy knowledge by using various multiple-choice questions at the end of the article written by Dr. Lucy N. Ngoh. We also extracted the data from the original article to add a few more questions in addition to those given at the end of the article. Because of the death of the primary author, we could not take permission from her. However, the permission for the reuse of these multiple-choice questions was obtained from the copyright holders. The original article can be accessed and cited as Ngoh LN. Health literacy: a barrier to pharmacist–patient communication and medication adherence. Journal of the American Pharmacists Association. 1 September 2009;49(5):e132-49.1.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Ratzan SC, Parker RM.. Health literacy. National library of medicine current bibliographies in medicine. Bethesda: National Institutes of Health, US Department of Health and Human Services; 2000February. [Google Scholar]
- [2].Kutner M, Greenburg E, Jin Y, et al. The health literacy of America’s adults: results from the 2003 national assessment of adult literacy. National Center for Education Statistics; 2006. (NCES 2006-483). [Google Scholar]
- [3].DeWalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes. J Gen Intern Med. 2004;19(12):1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. [DOI] [PubMed] [Google Scholar]
- [5].Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. [DOI] [PubMed] [Google Scholar]
- [6].Bass III PF, Wilson JF, Griffith CH, et al. Residents’ ability to identify patients with poor literacy skills. Acad Med. 2002;77(10):1039–1041. [DOI] [PubMed] [Google Scholar]
- [7].Bass PF, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18(12):1036–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ngoh LN. Health literacy: a barrier to pharmacist–patient communication and medication adherence. J Am Pharm Assoc. 2009September1;49(5):e132–49. [DOI] [PubMed] [Google Scholar]
- [9].Coleman C. Teaching health care professionals about health literacy: a review of the literature. Nurs Outlook. 2011April30;59(2):70–78. [DOI] [PubMed] [Google Scholar]
- [10].Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006August1;21(8):888–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ali NK. Are we training residents to communicate with low health literacy patients? J Community Hosp Internal Med Perspect. 2013January1;2(4):19238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Holmboe ES, Edgar L, Hamstra S. The milestones guidebook. Am Counc Graduate Med Educ. 2016. Available at: http://www.acgme.org/Portals/0/MilestonesGuidebook.pdf. [Google Scholar]
- [13].Powell CK, Kripalani S. Brief report: resident recognition of low literacy as a risk factor in hospital readmission. J Gen Intern Med. 2005November;20(11):1042–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ali NK, Ferguson RP, Mitha S, et al. Do medical trainees feel confident communicating with low health literacy patients? J Community Hosp Internal Med Perspect. 2014January1;4(2):22893. [DOI] [PMC free article] [PubMed] [Google Scholar]


