Abstract
Purpose
We measured waste from glaucoma surgeries at an eye care facility in Southern India and compared these results to a community hospital in the United States.
Methods
The waste produced in the glaucoma operating room at Aravind Eye Hospital, Madurai, India from June 22 to July 15, 2015 was weighed and compared to the waste produced in the glaucoma surgical clinic in a Baltimore-area community hospital from one day of surgeries in August 2015.
Results
The average waste produced per trabeculectomy at Aravind was 0.5 ± 0.2 kg, compared to an average of 1.4 ± 0.4 kg per trabeculectomy (p < 0.05) at the Baltimore-area hospital. Waste from device surgeries and trabeculectomy with phacoemulsification was also quantified at Aravind, with averages of 0.4 ± 0.2 kg and 0.7 ± 0.2 kg respectively.
Conclusions and importance
The amount of waste per trabeculectomy at the Aravind Eye Hospital was significantly lower than the waste per trabeculectomy in the Baltimore-area hospital, even though the used and the apparent complication rates between Aravind and American eye hospital are comparable. Given efforts to decrease the environmental impact of health care, it is necessary to examine the waste produced from surgeries to determine if policy and legal changes in the United States could decrease surgical waste while not affecting the surgical complication rate.
Keywords: Glaucoma, Surgical waste, Trabeculectomy, Efficiency, Environmental impact
1. Introduction
Environment and climate change are some of the greatest public health care challenges of the 21st century, and they have the ability to impact the health of billions of people worldwide.1,2 The scientific community has generally recognized the anthropogenic effects of climate change; some within the medical community are focusing on the impact of healthcare provision itself on the environment.3, 4, 5, 6 According to one study, the healthcare sector in the United States is responsible for 10% of the country's total greenhouse gas emissions.7,8 For comparison, 5% of Britain's GHG emissions and 7% of Australia's GHG emissions arise from the country's healthcare sector.9, 10, 11 As ophthalmic procedures are some of the most widely conducted, we should try to determine the impact of eye care on global and planetary health. Others have already begun to do so. A study of cataract surgery in the United Kingdom (UK) found that procurement of largely disposable supplies results in over half the carbon footprint of that surgery.12
One major aspect of healthcare having a significant environmental and economic impact is medical waste.13,14 Medical waste is a rarely studied aspect of surgical procedures and has never been studied in glaucoma surgery. We sought to compare surgical waste from glaucoma surgery between a US hospital and a Indian hospital as the health care system within the United States has many regulations that closely govern the use and disposal of instruments, supplies, and pharmaceuticals.14,15 The purpose of these laws is ostensibly to ensure that surgical materials are utilized and disposed of safely, thus decreasing the potential for complications and patient harm.15 Many other countries do not have such regulations, and many private hospitals overseas attempt to minimize the amount of hazardous waste produced to make their care more cost-effective by reducing the number of disposable supplies needed to purchase and reducing the economic costs of disposing of medical waste.16,17 Indeed, resource-constrained facilities may present good examples for medical systems in developed countries who are seeking to become more “environmentally sustainable” or efficient.
India is one such country that has fewer restrictions and regulations on the use and production of medical waste, when compared to the US.18 As a result, we studied the medical waste produced from glaucoma surgeries in an Indian eye hospital. The purpose of this study was to compare the waste from trabeculectomies at a private high-volume eye hospital in India to the waste from trabeculectomies at a US hospital with an ophthalmic subspecialty. This comparison would help illuminate whether US laws governing medical waste actually are necessary to prevent post-operative complications or if the laws merely contribute to the production of excessive waste, leading to additional environmental and economic costs.
2. Materials and methods
2.1. Study setting
In this pilot study, we quantified the medical waste produced from trabeculectomies, trabeculectomies combined with phacoemulsification, and glaucoma drainage device surgery in the “paying section” of the Aravind Eye Hospital in Madurai, India. Aravind is a network of five large hospitals and several smaller institutions throughout southern India. In total over 475,000 eye surgeries are performed at Aravind hospitals annually, including more than 2000 glaucoma surgeries in the paying section of the Aravind Eye Care System in Madurai. At Aravind, thousands of surgeries are performed annually without charge to patients in a separate “free section,” which was not considered in this study. Only patients who paid Indian market value for glaucoma surgery at Aravind were studied.
As the highest volume eye care center in the world, Aravind Eye Care System values efficiency. However, quality is paramount, with a major emphasis on patient safety; as such, Aravind has a relatively low complication rate, similar, if not better, than that of US eye hospitals.19
To serve as a point of comparison to the Aravind Eye Hospital trabeculectomy without phacoemulsification medical waste data, we also measured the amount of waste produced during one day of trabeculectomies without phacoemulsification at a private, not-for-profit mid-Atlantic community hospital that handles over 25,000 cases annually. This hospital was chosen because it is a private hospital that is not affiliated with any medical schools, similar to Aravind. Although we only collected data on trabeculectomy without phacoemulsification at the mid-Atlantic hospital, trabeculectomies combined with phacoemulsification and drainage device surgeries are also performed there, in roughly the same ratio as at Aravind. Roughly forty to seventy glaucoma surgeries are performed at the mid-Atlantic hospital monthly.
2.2. Study design
This is a prospective, observational pilot study. We collected and weighed the waste generated in each case in the glaucoma clinic at the paying section of Aravind Eye Hospital—Madurai from June 22, 2015 to July 10, 2015 (102 cases total). At Aravind Eye Hospital, medical waste data was recorded for thirty-eight trabeculectomies, forty-four trabeculectomies combined with phacoemulsification, and twenty glaucoma drainage device surgeries. In addition, we collected and weighed the waste from all glaucoma operations performed in the mid-Atlantic hospital operating room on August 24, 2015 (5 cases total). At the mid-Atlantic hospital, medical waste data was recorded for five trabeculectomies, the total number of trabeculectomies performed that day. Due to limitations in the length of the study period, it was not possible to observe further types of surgeries at the mid-Atlantic hospital. Each surgery was observed from the pre-operative stage through the end of the procedure.
At both facilities, through observation of each surgery, we compiled lists of all surgical supplies used during each type of surgery whether or not they were discarded (including medicines, caps and gowns, etc.). Aravind's purchasing department supplied the cost paid for each item in our supply list (we were unable to procure this data from the mid-Atlantic hospital). These costs were then added and averaged to ascertain the total cost of materials for each surgery and converted to US Dollars (1 US Dollar = approximately 65 Indian Rupees).
In each operating room at Aravind, separate disposal bins are kept for the waste; these disposal bins delineate infectious waste to be incinerated, waste for the landfill, and non-infectious/non-human waste to be recycled. At Aravind, surgeons and technicians who dispose of surgical waste are trained to differentiate between different types of waste, with up to 2/3 of the waste being recycled.17 We closely observed each surgery to ensure that both physicians and nurses disposed of the waste in the proper containers. In addition, qualitative observations during each surgery recorded which materials were discarded and the frequency of disposal of medications used during the surgery.
After each surgery, the waste in each bin was weighed on an analog, calibrated weighing scale to determine the weight of the waste to the nearest 0.1 g. The container weight was not included. For each surgery, the weights from each type of waste were added together to determine the total weight of the waste for that case.
At the mid-Atlantic hospital, waste was not divided into categories beyond separating biohazard waste from non-hazardous waste, which was sent directly to the landfill. Thus, after each surgery, the total amount of waste produced from that surgery was weighed on an analog scale to the nearest 0.1 g.
At Aravind Eye Hospital, an internal system of record keeping is used to specify when complications occur following each glaucoma surgery, and the hospital tracks all patients for six weeks after surgery. We were given access to this internal system and compiled this glaucoma surgery complication data from the entirety of the year 2014. We were not able to procure glaucoma surgical complication information from the mid-Atlantic hospital, so we will utilize published glaucoma surgical complication rates in the United States as a point of comparison.
2.3. Statistical analysis
All statistical analysis was carried out using R version 3.3.0 (Baltimore, MD). Descriptive statistics were used to analyze the average and variation of waste generated for each procedure type at Aravind. A Mann-Whitney U test was performed to determine the statistical significance of the difference in mean weight of waste from plain trabeculectomy at Aravind and the mid-Atlantic hospital. We considered a p < 0.05 as statistically significant.
3. Results
We weighted solid waste at AEH for 102 surgeries; 38 trabeculectomies, 44 trabeculectomies combined with phacoemulsification, and 20 drainage device surgeries. Trabeculectomies with phacoemulsification at Aravind produced significantly more waste than plain trabeculectomies and drainage device surgeries, as seen in Table 1.
Table 1.
Mean weight and variance of surgical waste at Aravind Eye Hospital.
| Trabeculectomy (38 surgeries) | Trabeculectomy combined with phacoemulsification (44 surgeries) | Drainage device surgery (20 surgeries) | |
|---|---|---|---|
| Non-infectious/non-human | 0.3 ± 0.2 kg | 0.33 ± 0.14 kg | 0.18 ± 0.18 kg |
| Infectious waste (incineration) | 0.07 ± 0.03 kg | 0.11 ± 0.06 kg | 0.08 ± 0.07 kg |
| Infectious waste (landfilled) | 0.13 ± 0.06 kg | 0.3 ± 0.2 kg | 0.13 ± 0.12 kg |
| Total Waste | 0.5 ± 0.2 kg | 0.7 ± 0.2 kg | 0.4 ± 0.2g |
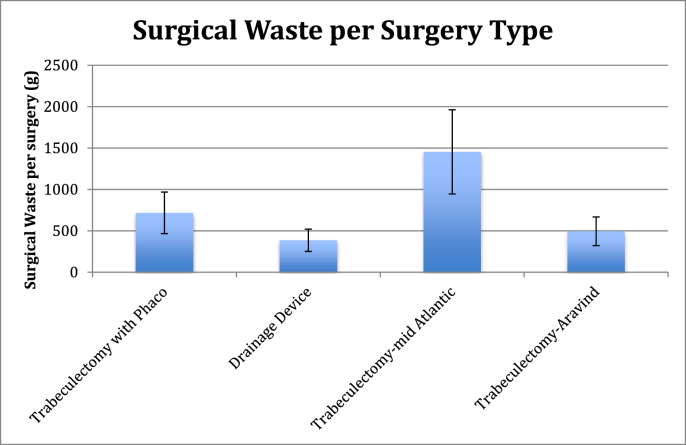
The average waste from trabeculectomies at the mid-Atlantic hospital was 1.4 ± 0.4 kg per surgery, shown in Fig. 1. Thus, the mid-Atlantic hospital had, on average, 3.76 times more surgical waste produced per trabeculectomy compared to Aravind Eye Hospital for the same type of surgery.
Fig. 1.
A comparison of mean waste generation and variation at Aravind and the mid-Atlantic hospital.
At the AEH Madurai paying section, a total of 376 trabeculectomies were performed in 2014, with eleven patients having intraoperative complications and twenty-three patients having post-operative complications (up to six weeks after the initial surgery), including the need for a second operation. Thus, the overall complication and need for more surgery for trabeculectomies in the year 2014 at the paying section of Aravind Eye Hospital—Madurai was 9.0%. For comparison, Jampel, et al. found in the Collaborative Initial Glaucoma Therapeutic Study, the intra-operative complication rate in a randomized sample of 290 trabeculectomies in the United States to be 12% and the early post-operative (up to one-month post-op) complication rate to be 50%.19 Furthermore, when comparing specifically the rates of endophthalmitis infection post-operatively, in the year 2015 Aravind had an endophthalmitis infection rate of 0.27% following trabeculectomy. Meanwhile, a study of 300 patients in the United States in 2013 found that the post-trabeculectomy endophthalmitis rate would be estimated to be 1.1%.20
4. Discussion
We found that surgeries at the mid-Atlantic hospital produced significantly more waste per surgery in trabeculectomies than Aravind (p < 0.05). In addition, all of the non-biohazard waste at the mid-Atlantic hospital was headed directly to the landfill, which is less environmentally friendly than the recycling options at Aravind. The surgical techniques between the two hospitals are quite similar, and though they both use the same instruments, Aravind reuses materials such as sanitized surgical instruments and medications, resulting in far lower waste generation rates.21,22
Assuming that the number of trabeculectomies performed at the mid-Atlantic hospital is five per day and that there are 260 workdays in a year, the predicted total waste produced from trabeculectomies over the course of one year would be 1899 kg. The waste at AEH is 26% of that at the US institution. Meanwhile, the same number of trabeculectomies at Aravind would lead to a predicted total waste production of 502.6 kg.
US law requires that pharmaceuticals, such as midazolam, dilating drops, and certain antibiotics, be disposed after every single case, even though significant amounts of medicines are often left over in the bottles.22 The law in question is the Federal Food and Drug Cosmetic Act, specifically Sections 501 and 502, as these sections stringently require that all drugs and devices that are labeled as single use be used only once, even if they could safely be used again.23 At Aravind, these medicines are re-used in patients until the bottles are empty, thus decreasing the amount of physical waste produced per patient. In the context of our pilot project, there appeared to be no complications (such as endophthalmitis) or other adverse events associated with multiple use fluids for phacoemulsification or medications used in association with surgery.19
Indeed, it is encouraging to compare the glaucoma surgery complication rates at AEH to published rates in the United States.19 The primary reason that is cited for the presence and enforcement of stringent laws governing surgical waste in the United States is that these laws prevent unnecessary patient harm.14,15 Our results suggest quite a different finding, however. The case of Aravind demonstrates that it is possible to decrease glaucoma surgical waste beyond that which is currently produced in American hospitals without any associated increase in harm to the patient. This manuscript is the first to demonstrate this finding, which would then lead to many questions about the necessity of specific surgical waste laws and whether further studies should be done on the efficacy of these laws.
5. Conclusion
The preliminary data from this study suggest that it may be possible for US surgical centers to decrease the amount of unnecessary waste they produce and continue to attain excellent surgical outcomes. This would, of course, require rethinking the process of surgical care delivery and perhaps restructuring the laws governing the production of medical waste. There is the risk of US hospitals taking shortcuts and compromising patient safety in order to minimize the medical waste they produce and pay to dispose of, leading to higher complication rates.
While this study exposes the need to examine surgical waste and the use and disposal of glaucoma surgery products, it has some limitations. One limitation is the single study location and small number of surgeries included in the United States. Examining more surgeries would increase the statistical power of the results and allow us to see variability across surgical facilities. Another limitation of this study was that we were unable to follow the patients whose surgeries we observed to determine the rate at which they developed post-operative complications; instead, we had to examine historical complication rates to compare the hospitals. Future studies should include the environmental impact of this surgical discipline and should test methods to safely reduce surgical waste.
The objective of this pilot study is to call attention to the fact that certain regulations in the US lead to the production of potentially unnecessary waste. Previous studies have examined the waste produced from operations such as hysterectomies and cataract surgeries, but this paper is the first to examine waste from glaucoma surgery.12,17 Our study and others demonstrate that we must continue to specifically and precisely examine the laws governing medical waste and the effect they have on our resource efficiency and costs. To do so, we must not only gather medical waste data for glaucoma surgeries but also for all medical procedures, until we can conclusively and empirically study the efficacy of current regulations. With healthcare practices contributing to climate change and climate change affecting the future of healthcare, it is economically and environmentally necessary to begin this process now.
Patient consent
This report does not contain any personal information that could lead to identification of patients. Therefore, patient consent was not obtained.
Acknowledgments
No funding or grant support was provided. The authors have no relevant financial information to disclose. All authors attest that they meet the current ICMJE criteria for authorship.
The authors would like to thank the staff at Aravind Eye Hospital and Greater Baltimore Medical Center for their support.
References
- 1.Pradumnya A., Guinto R. Climate change and health. Lancet. 2016;387(10017):430–431. doi: 10.1016/S0140-6736(16)00171-9. [DOI] [PubMed] [Google Scholar]
- 2.Patz J.A., Campbell-Lendrum D., Holloway T., Foley J. Impact of regional climate change on human health. Nature. 2005;438:310–317. doi: 10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- 3.Fitzpatrick J. The impact of healthcare on the environment: improving sustainability in the health service. Nursing. 2010;106(9):18–20. [PubMed] [Google Scholar]
- 4.Sarfaty M., Bloodhart B., Ewart G. American Thoracic Society member survey on climate change and health. Ann of the Am Thor Soc. 2005;12(2):274–278. doi: 10.1513/AnnalsATS.201410-460BC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarfaty M., Mitchell M., Bloodhart B., Maibach E.W. A survey of African American physicians on the health effects of climate change. Int Jour of Environ Res and Pub Health. 2014;11(12):12473–12485. doi: 10.3390/ijerph111212473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thiel C., Duncan P., Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Pol. 2017;22(3):162–167. doi: 10.1177/1355819617697353. [DOI] [PubMed] [Google Scholar]
- 7.Chung J.W., Meltzer D.O. Estimate of the carbon footprint of the US health care sector. J Am Med Assoc. 2009;302(18):1970–1972. doi: 10.1001/jama.2009.1610. [DOI] [PubMed] [Google Scholar]
- 8.Eckelman M.J., Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PloS One. 2016;11(6) doi: 10.1371/journal.pone.0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS England. Sustainable, resilient, healthy people and places. Available at www.sduhealth.org.uk. Accessed May 5, 2017.
- 10.Sustainable Development Unit . 2016. Carbon Footprint Update for NHS in England 2015.http://www.sduhealth.org.uk/documents/publications/2016/Carbon_Footprint_summary_NHS_update_2015_final_v2.pdf [Google Scholar]
- 11.Malik A., Lenzen M., McAlister S., McGain F. The carbon footprint of Australian health care. The Lan Plan Heal. 2018;2(1):e27–e35. doi: 10.1016/S2542-5196(17)30180-8. [DOI] [PubMed] [Google Scholar]
- 12.Thiel Cl, Eckelman M., Guido R. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49(3):1779–1786. doi: 10.1021/es504719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris D.S., Wright T., Sommer J.E.A., Connor A. The carbon footprint of cataract surgery. Eye. 2013;27:495–501. doi: 10.1038/eye.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martini C.L. Medical waste regulation in the United States: a dire need for recognition and reform. Northwestern Jour Int Law and Bus. 1993;14(1):206–230. [Google Scholar]
- 15.Lee C.C., Huffman G.L. Medical waste management/incineration. J Hazard Mater. 1996;48(1):1–30. [Google Scholar]
- 16.Reddy K.S. India's aspirations for universal health coverage. N Engl J Med. 2015;373(1):1–5. doi: 10.1056/NEJMp1414214. [DOI] [PubMed] [Google Scholar]
- 17.Thiel Cl, Schehlein E., Ravilla T. Cataract surgery and environmental sustainability: waste and life cycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391–1398. doi: 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patil A.D., Shekdar A.V. Health-care waste management in India. J Environ Manag. 2011;63(2):211–220. doi: 10.1006/jema.2001.0453. [DOI] [PubMed] [Google Scholar]
- 19.Jampel H.D., Musch D.C., Gillespie B.W., Lichter P.R., Wright M.W., Guire K.E. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS) Am J Ophthalmol. 2005;40(1):16–22. doi: 10.1016/j.ajo.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Zahid S., Musch D.C., Niziol L.M., Lichter P.R. Risk of endophthalmitis and other long-term complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS) Am J Ophthalmol. 2013;155(4):674–680. doi: 10.1016/j.ajo.2012.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le H., Ehrlich J.R., Venkatesh R. A sustainable model for delivering high-quality, efficient cataract surgery in southern India. Health Aff. 2016;35(10):1783–1790. doi: 10.1377/hlthaff.2016.0562. [DOI] [PubMed] [Google Scholar]
- 22.Drug Enforcement Administration. Final rule: placement of alfaxalone into schedule IV. Available at www.deadiversion.usdoj.gov. Accessed May 5, 2017.
- 23.Food and Drug Administration. Food, Drug, and Cosmetic Act. Available at www.fda.gov. Accessed May 5, 2017.