Abstract
Objective
This study aimed to present middle-term functional and radiological outcomes of the transfer of the lesser tuberosity in the management of reverse Hill-Sachs lesions following posterior dislocations of the shoulder.
Patients and methods
With a diagnosis of neglected posterior shoulder dislocation (8 locked, 5 recurrent), 13 male patients (age range: 28–72; mean age: 39.3 years) who underwent the transfer of the lesser tuberosity due to reverse Hill-Sachs lesions, were retrospectively reviewed based on functional and radiological data. The etiologies were: epilepsy in 9 patients, a traffic accident in 2 patients, and fall in 2 patients. To assess the patients' functional level, American Shoulder and Elbow Surgeons (ASES) and Constant Scores were used, and the patients' range of motion at the last follow-up was measured. To evaluate the development of arthrosis, the final follow-up control plain radiographs were examined. The average size of the defects calculated from the axial computed tomography sets was 27% (range: 20%–40%).
Results
The average length of follow-up was 30 months (range: 12–67 months). At the last follow-up visit, the main ASES and Constant Scores were 78 and 85, respectively, and the average degrees of flexion, abduction, and external rotation were 163°, 151°, and 70° respectively. The concentric reduction was observed postoperatively.
Conclusion
McLaughlin procedure appears to be a safe and effective method in the treatment of neglected posterior shoulder dislocations with reverse Hill-Sachs lesion.
Level of Evidence
Level IV, Therapeutic study.
Keywords: Posterior shoulder dislocation, Reverse Hill-Sachs lesion, McLaughlin procedure, Transfer of the lesser tuberosity
Introduction
With a 2% incidence, posterior shoulder dislocations are considerably less common than anterior dislocations. Although trauma is the principal cause of posterior dislocations, other causes, such as epilepsy and electric shock, which generate severe contractions throughout the entire body, have been identified.1 The posterior dislocation of the shoulder may be easily missed in an emergency room because its clinical and radiological signs are not as remarkable as the signs for anterior shoulder dislocations. Therefore, a high index of clinical suspicion and the appropriate imaging modality are necessary to ensure correct diagnosis and appropriate treatment.2
Operative and non-operative treatments are employed in the management of posterior shoulder dislocation by considering the size of the humeral impression fracture, the duration of the dislocation, and the activity and age of the patient.1, 2, 3, 4 When choosing the appropriate treatment, the size of the humeral head defect is the most practical guideline. Additionally, in order to diagnose and treat posterior dislocation of the shoulder relevant to defects ranging in size between 25% and 50%, it is recommended that the modified McLaughlin procedure be used; this involves the transfer of the lesser tuberosity with the attached subscapularis tendon into the defect.5
This present study aimed to conduct an investigation regarding middle-term functional and radiological outcomes of the transfer of the lesser tuberosity in the management of posterior dislocation of the shoulder with reverse Hill-Sachs lesion, with defects ranging in size from 20% to 40%.
Patients and methods
We retrospectively reviewed the medical records of 23 patients who were diagnosed and treated for posterior dislocation of the shoulder between 2009 and 2012 at our institution. Of the 23 patients, 4 underwent shoulder hemiarthroplasty due to reverse Hill-Sachs lesions with a defect size greater than 40%, and 6 were treated by arthroscopic posterior Bankart repair due to reverse Hill-Sachs lesions with a defect size less than 10%. After excluding those patients, a total of 13 patients who were treated using the transfer of the lesser tuberosity (the modified McLaughlin procedure) were included in the present study.
All the patients included in the study were recalled for subjective, objective, and functional evaluation. The study protocol involved functional condition, range of motion (ROM), American Shoulder and Elbow Surgeons (ASES) and Constant Scores in addition to plain radiograph (Fig. 1) and computed tomography (CT) scans of the shoulder (Fig. 2). According to the Kellgren and Lawrence radiological classification system, any development of arthrosis was assessed at the last follow-up.
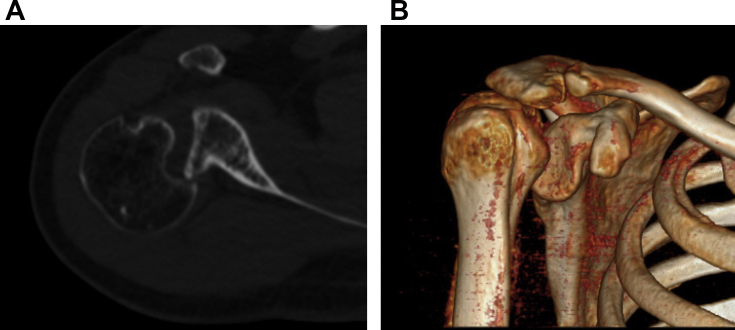
Fig. 1.
Preoperative anteroposterior radiograph of right shoulder of patient number twelve.
Fig. 2.
(A) Computed tomography scan of right shoulder of patient number twelve demonstrating remarkable reverse Hill-Sachs lesion in axial plane. (B) Three-dimensional computed tomography reconstruction of right shoulder of patient number eight displaying locked posterior shoulder dislocation.
The average length of follow-up was 30 months (range: 12–67 months). All the patients were male, and the mean age was 39.3 years, with an age range from 28 to 72. Locked posterior dislocation following the first dislocation was determined in 8 patients. The remaining 5 patients presented with the recurrent posterior shoulder dislocation. The etiologies were: epilepsy in 9 patients, a traffic accident in 2 patients, and falling down in 2 patients.
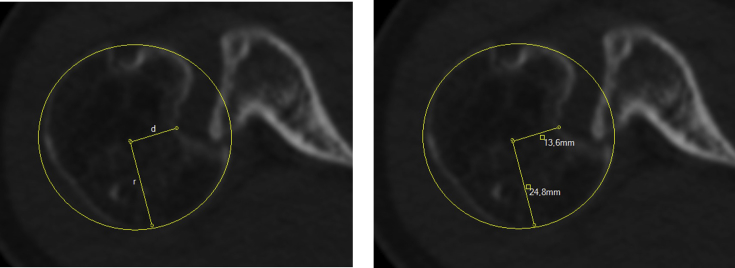
The size of the reverse Hill-Sachs lesions was quantified using axial CT sets, as described by Moroder et al.6 (Fig. 3) and the average size of the defects was 27%, with a defect size range varying from 20% to 40%. Furthermore, the prime indication for using the modified McLaughlin procedure was reverse Hill-Sachs lesion, with a defect size ranging from 20% to 40%, whether the posterior dislocation was locked or recurrent.
Fig. 3.
According to Moroder et al, to estimate the maximum relative depth of the defect in the axial CT image, line is drawn from the center of the best-fit circle to the base of the defect (d). Then, distance d is removed from the radius of the circle (r), and the result is divided through the diameter of the circle (2r).
Surgical technique
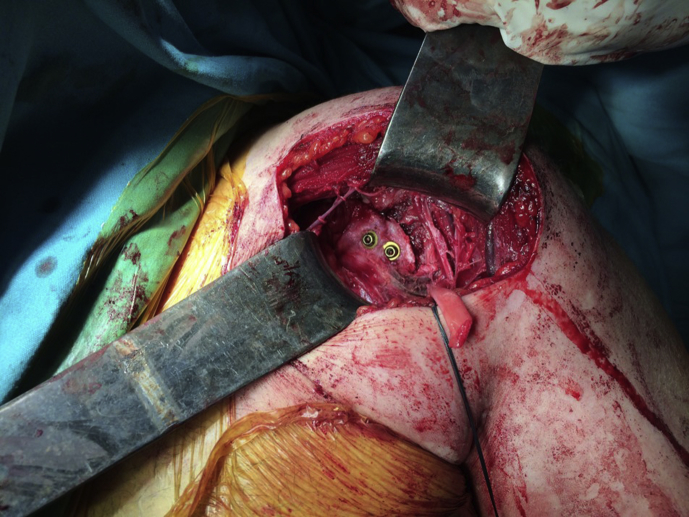
Under general anesthesia, and with the patient in the beach-chair position, the standard deltopectoral approach was used to expose the patient's shoulder joint. Then, the subscapularis tendon was identified, and the posterior dislocated humeral head was reached using the rotator interval. The reduction was accomplished by placing a Cobb elevator between the glenoid and the humeral head, paying attention to avoid creating any fracture. The next step was to confirm the defect of the humeral head, which was quantified using a CT scan before the operation. The long head of the biceps tendon was released from its attachment close to the glenoid, and it was reattached to its groove on the humerus at the end of the operation. Osteotomy of the lesser tuberculum was accomplished by using a bone saw without detaching the subscapularis tendon from its attachment. The osteotomized lesser tuberculum was slid into the defect area, which was fixed with two, 4 mm cannulated screws (DePuy Synthes Companies®, Zuchwil, Switzerland) (Fig. 4). Fluoroscopy was used to control the directions of the screws, and no joint penetration was detected. The construction and stability were evaluated via direct observation and fluoroscopic imaging intraoperatively. After certifying the stability, wound closure was performed using a suction drain at the end of the operation. A double dose of a second-generation cephalosporin was ordered for the perioperative antibiotics prophylaxis.
Fig. 4.
Intraoperative imagine showing fixation of the osteotomized lesser tuberculum with 2 cannulated screws.
Postoperative rehabilitation protocol
Postoperatively, the shoulder joint was immobilized at 30° abduction and neutral rotation with a shoulder sling brace for 6 weeks. Internal rotation was not allowed; only wrist and hand exercises were permitted during this period. After 6 weeks, active-assisted physical therapy was initiated. After 12 weeks, all active motions were allowed.
Results
The results obtained from the analysis of 13 patients that underwent the modified McLaughlin procedure are presented in Table 1. With satisfactory functional conditions, all the patients returned to their daily life without any limitations. No subluxation or dislocation was observed postoperatively. At the last follow-up, the main ASES and Constant Scores were 78 and 85, respectively, and the average degrees of flexion, abduction, and external rotation were 163°, 151°, and 70°, respectively. Moreover, ranges of internal rotation were the seventh thoracic vertebra (T7) in 2 patients, the twelfth thoracic vertebra (T12) in 4 patients, the third lumbar vertebra (L3) in 4 patients, the buttock in 2 patients, and the lateral thigh in 1 patient.
Table 1.
Clinical and demographic profile analysis of patients.
| Patient | Sex | Age (years) | Etiology | Follow-up time (month) | Flexion (°) | External rotation (°) | Abduction (°) | Internal rotation | Size of humeral impaction (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 72 | Fall | 25 | 170 | 90 | 160 | L3 | 29 |
| 2 | M | 28 | Car accident | 60 | 180 | 85 | 170 | T12 | 26 |
| 3 | M | 36 | Epilepsy | 20 | 130 | 90 | 150 | L3 | 20 |
| 4 | M | 38 | Epilepsy | 24 | 170 | 70 | 140 | Buttock | 22 |
| 5 | M | 37 | Epilepsy | 16 | 160 | 35 | 150 | T12 | 25 |
| 6 | M | 38 | Epilepsy | 14 | 150 | 45 | 130 | Lateral thigh | 28 |
| 7 | M | 63 | Epilepsy | 67 | 160 | 50 | 155 | L3 | 33 |
| 8 | M | 31 | Epilepsy | 12 | 180 | 90 | 170 | T7 | 25 |
| 9 | M | 35 | Epilepsy | 36 | 175 | 80 | 160 | T12 | 35 |
| 10 | M | 30 | Car accident | 48 | 170 | 75 | 145 | T7 | 25 |
| 11 | M | 40 | Fall | 36 | 160 | 70 | 155 | L3 | 24 |
| 12 | M | 28 | Epilepsy | 24 | 170 | 80 | 160 | T12 | 29 |
| 13 | M | 35 | Epilepsy | 12 | 150 | 50 | 120 | Buttock | 28 |
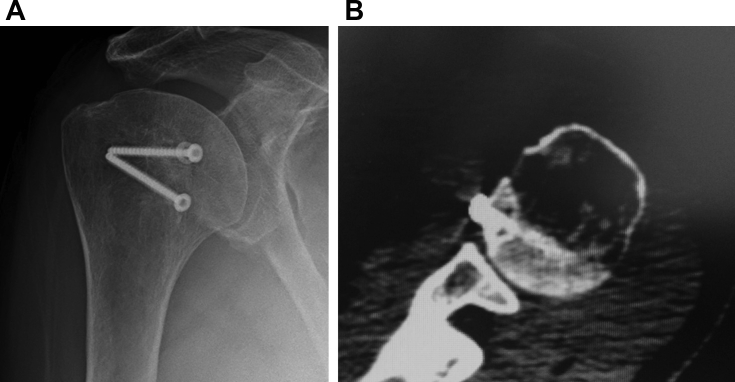
In the final follow-up control radiographic evaluation, the concentric reduction was maintained for all patients, and the union of the transferred lesser tuberosity was recognized in all patients (Fig. 5). There was no evidence of arthrosis on the plain radiography according to the Kellgren and Lawrence radiological classification system, all of which were grade 0.
Fig. 5.
(A) Postoperative anteroposterior radiograph of patient number seven displaying concentric reduction. (B) Postoperative axial view of CT scan illustrating replacement of the lesser tuberosity into the defect area.
Discussion
Initially, over half of all posterior shoulder dislocations are unrecognized due to obscure clinical and radiological signs.1, 2, 3, 4, 5, 7, 8 A high index of clinical suspicion and a suitable imaging modality are essential for correct diagnosis and appropriate treatment.2
Posterior shoulder dislocation is frequently accompanied by an anteromedial impression fracture of the humeral head, which is also known as a reverse Hill-Sachs lesion. This defect has long been cited as a cause of recurrent instability and early-onset osteoarthrosis of the shoulder. Thus, specific treatment should be provided to address this potential problem.2, 5, 7
Most previous studies have used the size of the defect to determine the choice of treatment because the size plays a pivotal role as a practical guideline for selecting the treatment option.5, 9, 10, 11, 12 Regarding the management of posterior shoulder dislocations, treatment approaches vary, based on the size of the defect. In small impression defects that are less than 15%, closed reduction alone can be easily performed for acute cases that are not complicated. However, open reduction is often necessary for chronic cases with a similar defect size. In large impression defects greater than 40%, total shoulder arthroplasty or hemiarthroplasty is generally the recommended and accepted procedure, depending on the functional status of the patient.2
The literature is conflicting as to the management of defects that range in size between 20% and 40%. It is a well-known that enlargement of the size of the defect following reposition significantly increases the risk of instability. Therefore, the refill of the defect plays a pivotal role in resolving this problem. A variety of techniques, such as transfer of the lesser tuberosity, rotational osteotomy of the humerus, and allograft or autograft reconstruction, have been used to refill the defect.5
With respect to the use of autologous or allogenic bone graft, several techniques have been described in the literature. However, some complications, such as graft collapse, screw loosening, avascular necrosis of the femoral head, and osteoarthrosis, limit use of these techniques.13
Subscapularis tenodesis is another option that can be used to refill the defect. First described by McLaughlin,3 this technique is used to perform an open transfer of the subscapularis tendon by detaching it from its attachment to the bone defect.3 Most recently, this procedure was performed arthroscopically through the only plication into the bone defect without detaching from its attachment.7 Furthermore, Hawkins and Neer (1987) presented a new design of McLaughlin's procedure. This modification consisted of a simultaneous transfer of the subscapularis tendon and lesser tuberosity. They noted that this modified procedure provides some advantages, such as more secure bone fixation and better filling of the defect with the osteotomized bone fragment.1 In addition, while the authors of some studies prefer to use of one or two screws for fixation, others suggest using only a suture anchor.9 With the goal of increasing rotational stability, two, 4 mm cannulated screws were preferred in our study.
Although the literature contains many case reports dealing with the neglected posterior shoulder dislocation,9, 11, 14, 15, 16 only a limited number of case series are available that report on the transfer of the lesser tuberosity.1, 12, 17 In the study by Hawkins et al, satisfactory outcomes were reported in 4 patients with a mean follow-up of 5.5 years.1 Similarly, Kokkalis et al reported that 5 patients were managed using the same technique, and no recurrent instability was seen during a 20-month follow-up period.9
An argument can be made that the present study, which addresses the issue of neglected posterior shoulder dislocations, makes an important contribution to the existing literature because it reports on a higher number of patients with successful middle-term functional and radiological outcomes using the modified McLaughlin procedure.
However, this present study has a number of important limitations that must be considered. First, only the size of the defect was considered when determining the appropriate treatment. However, Moroder et al6 reported that, in addition to the size of the defect, settlement also played a crucial role in the treatment selection. Second, the follow-up period in this study was limited to the middle-term functional and radiological outcomes. Third, this study did not include a control group. Finally, all the patients included in this study were male.
Conclusion
The size and settlement of the defect are critical factors for selecting the appropriate course of treatment for neglected posterior shoulder dislocations. However, the settlement of the defect was not considered in this study. Therefore, further work is required to examine that factor. All in all, this study showed that the modified McLaughlin procedure is an appropriate technique for neglected posterior shoulder dislocations with size defects ranging between 20% and 40%, even though the study had no control group. Therefore, future studies on the current topic that include with control groups are required.
Conflict of interest
The authors “Mehmet DEMİREL, Ali ERŞEN, Gökhan KARADEMİR, Ata Can ATALAR, Mehmet Demirhan” individually declare that they have no conflict of interest.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Mehmet Demirel, Email: dr88.mehmet.demirel@gmail.com.
Ali Erşen, Email: ali_ersen@hotmail.com.
Gökhan Karademir, Email: dr@gokhankarademir.com.
Ata Can Atalar, Email: atalar.ac@gmail.com.
Mehmet Demirhan, Email: mdemirhan@ku.edu.tr.
References
- 1.Hawkins R., Neer C., Pianta R., Mendoza F. Locked posterior dislocation of the shoulder. J Bone Jt Surg Am. 1987;69(1):9–18. PMID: 3805075. [PubMed] [Google Scholar]
- 2.Gavriilidis I., Magosch P., Lichtenberg S., Habermeyer P., Kircher J. Chronic locked posterior shoulder dislocation with severe head involvement. Int Orthop. 2010;34(1):79–84. doi: 10.1007/s00264-009-0762-9. PMID: 19300999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLAUGHLIN H.L. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952 Jul:584–590. PMID: 14946209. [PubMed] [Google Scholar]
- 4.Cheng S.L., Mackay M.B., Richards R.R. Treatment of locked posterior fracture-dislocations of the shoulder by total shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6(1):11–17. doi: 10.1016/s1058-2746(97)90065-3. PMID: 9071677. [DOI] [PubMed] [Google Scholar]
- 5.Cicak N. Posterior dislocation of the shoulder. J Bone Joint Surg Br. 2004;86(3):324–332. doi: 10.1302/0301-620x.86b3.14985. PMID: 15125117. [DOI] [PubMed] [Google Scholar]
- 6.Moroder P., Tauber M., Hoffelner T. Reliability of a new standardized measurement technique for reverse Hill-Sachs lesions in posterior shoulder dislocations. Arthrosc: J Arthrosc Relat Surg. 2013;29(3):478–484. doi: 10.1016/j.arthro.2012.10.016. PMID: 23351729. [DOI] [PubMed] [Google Scholar]
- 7.Charalambous C., Gullett T., Ravenscroft M. A modification of the McLaughlin procedure for persistent posterior shoulder instability: technical note. Arch Orthop Trauma Surg. 2009;129(6):753–755. doi: 10.1007/s00402-008-0721-8. PMID: 18709379. [DOI] [PubMed] [Google Scholar]
- 8.Checchia S.L., Santos P.D., Miyazaki A.N. Surgical treatment of acute and chronic posterior fracture-dislocation of the shoulder. J Shoulder Elbow Surg. 1998;7(1):53–65. doi: 10.1016/s1058-2746(98)90183-5. PMID: 9524341. [DOI] [PubMed] [Google Scholar]
- 9.Kokkalis Z.T., Mavrogenis A.F., Ballas E.G., Papanastasiou J., Papagelopoulos P.J. Modified McLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics. 2013;36(7):e912–e916. doi: 10.3928/01477447-20130624-22. PMID: 23823049. [DOI] [PubMed] [Google Scholar]
- 10.Khiami F., Suprun K., Sari-Ali E., Rolland E., Catonné Y. Traitement chirurgical de la luxation post-traumatique gléno-humérale postérieure. J Traumatol Sport. 2006;23(2):89–95. [Google Scholar]
- 11.Ivkovic A., Boric I., Cicak N. One-stage operation for locked bilateral posterior dislocation of the shoulder. J Bone Joint Surg Br. 2007;89(6):825–828. doi: 10.1302/0301-620X.89B6.18842. PMID: 17613513. [DOI] [PubMed] [Google Scholar]
- 12.Gustavo A., Calvo E., Bonilla L., Espejo L., Box R. Neglected traumatic posterior dislocations of the shoulder: controversies on indications for treatment and new CT scan findings. J Orthop Sci. 2000;5(1):37–42. doi: 10.1007/s007760050006. PMID: 10664437. [DOI] [PubMed] [Google Scholar]
- 13.Diklic I., Ganic Z., Blagojevic Z., Nho S., Romeo A. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br. 2010;92(1):71–76. doi: 10.1302/0301-620X.92B1.22142. PMID: 20044682. [DOI] [PubMed] [Google Scholar]
- 14.Elmalı N., Taşdemir Z., Sağlam F., Gülabi D., Baysal Ö. One-stage surgical treatment of neglected simultaneous bilateral locked posterior dislocation of shoulder: a case report and literature review. Eklem Hastalik Cerrahisi: Jt Dis Relat Surg. 2015;26(3):175–180. doi: 10.5606/ehc.2015.36. PMID: 26514224. [DOI] [PubMed] [Google Scholar]
- 15.Torrens C., Santana F., Melendo E., Marlet V., Cáceres E. Osteochondral autograft and hemiarthroplasty for bilateral locked posterior dislocation of the shoulder. Am J Orthop (Belle Mead NJ) 2012;41(8):362–364. PMID: 22900247. [PubMed] [Google Scholar]
- 16.Kokkalis Z.T., Mavrogenis A.F., Ballas E.G., Papagelopoulos P.J., Zoubos A.B. Bilateral neglected posterior fracture–dislocation of the shoulders. Orthopedics. 2012;35(10):e1537–e1541. doi: 10.3928/01477447-20120919-26. PMID: 23027494. [DOI] [PubMed] [Google Scholar]
- 17.Gerber C., Lambert S.M. Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Jt Surg Am. 1996;78(3):376–382. doi: 10.2106/00004623-199603000-00008. PMID: 8613444. [DOI] [PubMed] [Google Scholar]