Abstract
Objective
The aim of this study was to develop a new calcaneal fracture classification system which will consider sustentacular fragment configuration and relation of posterior calcaneal facet to calcaneal body.
Methods
The new classification system used sustentacular fragment configuration and relation of posterior calcaneal facet fracture with fracture components of calcaneal body as key aspects of main types and subtypes. Between 2000 and 2014, 126 intraarticular calcaneal fractures were classified according to the new classification system by using computed tomography images. The new classification system was studied in term of reliability, correlation to choices of treatment, implant fixation and quality of fracture reduction.
Results
Types of sustentacular fragment comprised type A, B and C. Type A sustentacular fragment included sustentacular tali containing middle calcaneal facet. In Type B and C fractures sustentacular fragment included medial aspect and entire posterior calcaneal facet as a single unit, respectively. The fractures with type A, B and C sustentacular fragments were classified as main type A, B and C intra-articular calcaneal fractures. The main type A and B comprised 4 subtypes. Subtypes A1, A3, B1, and B3 associated with avulsion and bending fragments of calcaneal body. Subtype A2, B2, and B4 associated with burst calcaneal body. Subtype B4 was not found in the study. Main type C had no subtype and associated with burst calcaneal body. The data showed good reliability.
Conclusion
The study showed that our new intra-articular calcaneal fracture classification system correlates to choices of treatment, implant fixation and quality of fracture reduction.
Level of Evidence: Level IV, Study of Diagnostic Test
Keywords: Intra-articular calcaneal fracture, Classification system, Sustentacular fragment, Posterior calcaneal facet fracture, Choices of treatment, Quality of fracture reduction
Introduction
Intra-articular calcaneal fractures (IACF) under compressive load creates a sustentacular fragment (SF), fractures of posterior calcaneal facet (PCF) and of calcaneal body. The SF is a medial fragment of the calcaneal body fracture and remains attached to talus.1, 2 The PCF fracture creates incongruent posterior subtalar joint in form of either displaced articular surface or intra-articular fracture. The previous reports showed that restoration of calcaneal morphology and anatomic articular surface reduction of PCF provide good outcomes.3, 4, 5 Therefore, understanding IACF in term of SF configurations and association of calcaneal facet fracture with fracture components of the calcaneal body has benefit for surgical treatment. There are many existing intra-articular calcaneal fracture classification systems, such as those by Sanders and Essex-Lopresti, do not correlate to choices of treatment.3, 6, 7 Sanders classification provides information about the calcaneal facet fracture which affected the development of late post-traumatic subtalar arthritis but no association of PCF fracture with fracture patterns of calcaneal body. This is the importance of the calcaneal morphology restoration.3 Essex-Lopresti classification provides only limited information about the calcaneal body and calcaneal facet fractures. It mainly described the treatment of tongue fragment by “Essex-Lopresti procedure” but the consideration on PCF even SF still be overlooked.6 The recent fracture classification system of Harnroongroj provides only information about fractures of the calcaneal body but no details regarding calcaneal facet fractures. Those classification systems did not consider the SF configuration and relation between calcaneal facet and body fractures which was important for preoperative planning for the treatment of IACFs.8, 9 Therefore, we developed a new IACF classification system in term of SF configuration and incorporation of posterior calcaneal facet fractures with fracture components of calcaneal body. The classification system was studied in term of reliability, correlation to choices of treatment, implant fixation and quality of fracture reduction.
Materials and methods
We developed the new IACF classification as followings. Calcaneal facet fracture was defined as the fracture at the level of calcaneal facets that included displaced intact articular surface and intra-articular fracture of PCF. SF was defined as a medial fragment of calcaneal body with constantly containing middle calcaneal facet and remained attached to talus. Calcaneal body fracture components were defined as followings: avulsion fracture fragment was the fracture fragment that involves tendoachillis insertion at posterior tubercle and anteriorly extends to included PCF.1 A bending fragment is same as avulsion fragment, but the fracture included inferior aspect of posterior calcaneal tubercle and extends anteriorly to include PCF.1 Burst of the calcaneus is comminuted fracture with displaced fractures of lateral and/or medial calcaneal walls and/or longitudinal fracture of the calcaneal body.1
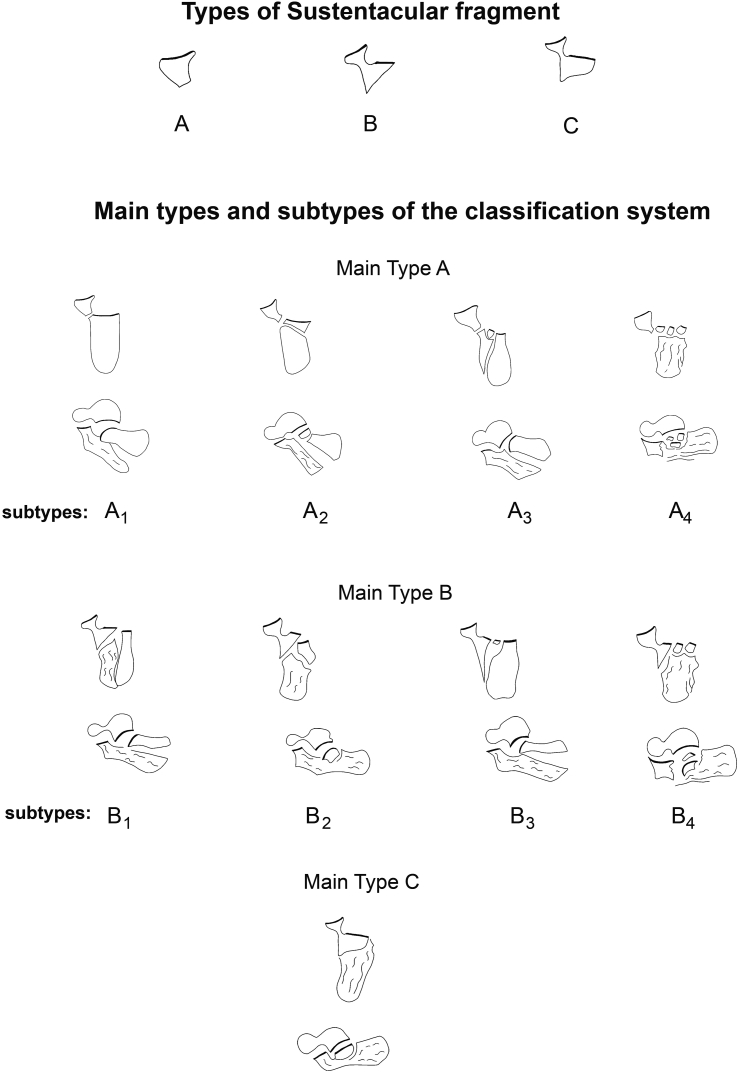
Using axial CT images, the configuration of SF was identified and typed for using as the key aspect of main types of the classification. The SF configuration was typed as the followings; SF type A was a sustentacular tali fragment containing middle calcaneal facet. Type B was medial calcaneal fragment which consisted of sustentacular tali containing middle calcaneal facet and included medial aspect of PCF as a single unit. Whereas, type C sustentacular fragment was medial calcaneal fragment which consisted of sustentacular tali containing middle calcaneal facet and entire PCF as a single unit (Fig. 1, above). The fractures with SF type A, B and C were classified as main type A, B and C IACF respectively (Fig. 1).
Fig. 1.
Diagram showed new intra-articular calcaneal fracture classification system in term of sustentacular fragment types and incorporation of posterior calcaneal facet fracture with fracture components of calcaneal body.
Using axial and sagittal CT images, subtype of main type A and B were classified by using configuration of the PCF fracture in term of intact articular surface or intra-articular fracture of PCF and the association with fracture components of calcaneal body as the key aspect of the subtype classification. By the way, main type C had no separated PCF fragment, so it had no subtype (Fig. 1).
Subtype A1 IACF comprised SF type A and entire PCF with intact articular surface as the separated fragment from the SF. The PCF associated with avulsion or bending fracture fragments of calcaneal body by its articular surface was anterior surface of avulsion or bending fragments (Fig. 1).
Subtype A2 was the same as A1 but the separated PCF fragment associated with burst calcaneal body by forming a free articular fragment in burst calcaneal body (Fig. 1).
Subtype A3 was the same as A1 but medial aspect of the PCF had intra-articular fracture. Whereas, the lateral aspect had intact articular surface and associated with avulsion fragment as subtype A1 (Fig. 1).
Subtype A4 was the same as A1 but the PCF had comminuted intra-articular fracture and associated with burst calcaneal body by forming multiple free articular fragments in burst calcaneal body (Fig. 1).
In the same manner of main type A, main type B IACF consisted of subtype B1, B2, B3 and B4. The subtype B1, B2, B3 and B4 comprised SF type B and the separated lateral PCF which associated with fracture components of calcaneal body same as subtypes A1, A2, A3 and A4 respectively. For subtype B2, the separated lateral PCF fragment associated with burst calcaneal body by forming a large thalamic fragment (Fig. 1).
Radiographs, CT images, and medical records of patients who were treated for acute displaced intra-articular calcaneal fracture at our institutions between 2000 and 2014 were reviewed retrospectively.
Inclusion criteria were age 18–80 years and acute displaced IACF less than 2 weeks after injury. Exclusion criteria were non-displaced intra-articular fracture, the fracture more than 2 weeks after injury, fracture associated with metabolic bone disease, pathological fracture, ankle osteoarthritis, deformed foot, and incomplete medical records or plain calcaneal radiographs or CT images.
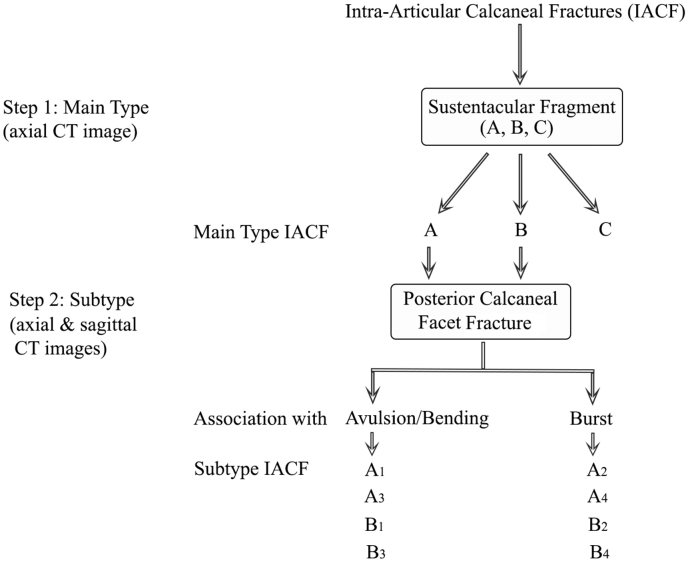
Using axial and sagittal CT images of IACF, the fracture were classified according to the new classification system (Fig. 2).
Fig. 2.
Flow chart for classifying intra-articular calcaneal fractures according to the new classification system.
Demographic data of patients, causes of accident leading to fracture were recorded. Main types and subtypes associated with fracture components of calcaneal body were studied. Surgical technique and implant fixation of the fractures were reviewed and recorded. Using axial and lateral calcaneal radiographs and digital Programmable Automation Controller system and measurement tools, preoperative and 6-month-postoperative calcaneal fracture parameters were measured. Gissane and Böhler angles were measured according to standard techniques. Calcaneal length was measured as a distance between anterior calcaneal process and posterior most of posterior calcaneal tubercle from lateral calcaneal radiograph. Using axial calcaneal radiographs, calcaneal varus was measured as the angle between longitudinal trabeculae of posterior calcaneal tubercle and a line drawn perpendicular to apex curve of lateral cortex of lateral malleolus minus 90°.10 Calcaneal body burst was measured as lateral displacement of the lateral calcaneal wall, which was measured by drawing a line between the lateral aspect of the posterior calcaneal tubercle and lateral cortex of anterior calcaneus. Lateral calcaneal wall displacement was then measured as the distance between maximum displacement of the lateral calcaneal wall and the line drawn. Congruent articular surfaces of posterior subtalar joint was measured from lateral calcaneal radiograph as an angle between straight lines drawn between both end of talar and calcaneal posterior facets. Comminuted intra-articular fracture of subtalar joint was evaluated by using axial and lateral calcaneal radiographs. The fracture configuration and quality of fracture reduction were evaluated by pre- and postoperative radiographic calcaneal fracture scores (Table 1).
Table 1.
Radiographic calcaneal fracture scores.
| Calcaneal fracture parameters | Scores | |
|---|---|---|
| Bohler angle | <20° | 1 |
| ≥20° | 0 | |
| Gissane angle | <95° | 1 |
| ≥95° | 0 | |
| Congruent posterior subtalar joint | >5°, comminuted intra-articular fracture | 3 |
| ≤5° | 0 | |
| Varus angle | >10° | 2 |
| ≤10° | 0 | |
| Burst | Burst calcaneal body including lateral calcaneal wall displacement/No postoperative decrement of lateral wall displacement | 3 |
| No burst calcaneal body/Postoperative decrement of lateral wall displacement | 0 | |
| Length | Displaced calcaneal body fracture/No postoperative increment | 1 |
| Postoperative increment | 0 | |
| Total scoresa | 11 |
Higher scores indicate more complex fracture configurations.
Types and subtypes of the new classification system were performed in a 6-week interval including fracture parameter measurements by 2 orthopaedic surgeons. The data were statistically analysed.
Results
One hundred and twelve patients (mean age 36.83 years [range, 18–72 years]; 88 males, 24 females) with 126 acute displaced IACFs were enrolled. Causes of fractures were falls from a height in 92 patients and motor vehicle accidents in 20 patients. SF of the IACFs were typed as 51, 53 and 22 of type A, B and C respectively.
In Table 2, of the 126 IACFs showed 51 (40.48%), 53 (42.06%) and 22 (17.45%) main type A, B and C IACF respectively.
Table 2.
Main and subtype characteristics of the new intra-articular calcaneal fracture classification system including surgical technique and implant fixation.
| Main type | Characteristic of main type | No. of fractures (%) | Subtype (n, %) (n = 126) |
Characteristics of subtype | Association with fracture components of calcaneal body | Surgical technique | Implant fixation |
||
|---|---|---|---|---|---|---|---|---|---|
| Screw | Plate | Cast | |||||||
| A | Type A sustentacular fragment, 4 subtypes | 51/126 (41.48) | A1, (32/126, 25.39%) | Type A sustentacular fragment, the entire posterior calcaneal facet has intact articular surface as anterior surface of avulsion or bending fracture fragment of calcaneal body. | 20 avulsion and 12 bending fragments | Percutaneous reduction and fixation of avulsion and bending fragments | 32 | – | – |
| A2, (4/126, 3.17%) | Type A sustentacular fragment, the entire posterior calcaneal facet forms a free articular fragment from calcaneal body. | Burst of calcaneal body | Percutaneous reduction and fixation of calcaneal body | 4 | – | – | |||
| A3 (15/126, 11.90%) | Type A sustentacular fragment, the posterior calcaneal facet has intra-articular fracture at medial most aspect creating small free articular fragments. Later almost posterior calcaneal facet has intact articular surface as anterior surface of avulsion fracture fragment of calcaneal body. | Avulsion fragment | Percutaneous reduction and fixation of avulsion fragment | 15 | – | – | |||
| A4 | Type A sustentacular fragment, comminuted intra-articular fracture of the posterior calcaneal facet and forms multiple free articular fragment from calcaneal body (Not found in the study). | – | – | – | – | – | |||
| B | Type B sustentacular fragment, 4 subtypes | 53/126 (42.06%) | B1 (4/126, 3.17%) | Type B sustentacular fragment. The separated lateral posterior calcaneal facet has intact articular surface as anterior surface of avulsion fracture fragment of calcaneal body. | Avulsion fragment | Percutaneous reduction and fixation of avulsion fragment | 4 | – | – |
| B2 (32/126, 25.39%) | Type B sustentacular fragment. The lateral posterior calcaneal facet with intact articular surface is a free articular fragment from calcaneal body. The articular fragment depresses into the burst calcaneal body, creating a large thalamic fragment. | Burst of calcaneal body | Percutaneous reduction and fixation of calcaneal body including reduction and fixation of the thalamic fragment via sinus tarsi approach | 28 | 4 | – | |||
| B3 (7/126, 5.56%) | Type B sustentacular fragment. Medial most aspect of the lateral posterior calcaneal facet has intra-articular fracture creating small free articular fragments from the calcaneal body. Whereas, later almost aspect with intact articular surface as anterior surface of avulsion fracture fragment of the calcaneal. | Avulsion fragment | Percutaneous reduction and fixation of avulsion fragment | 7 | – | – | |||
| B4 (10/126, 7.94) | Type B sustentacular fragment. The separated lateral posterior calcaneal facet has comminuted intra-articular fracture and creating small free articular fragments. The free articular fragments depress into the burst calcaneal body, creating small thalamic fragments. | Burst of calcaneal body | Percutaneous reduction and fixation of calcaneal body, addressing articular fragments of posterior calcaneal facet via sinus tarsi approach or reduction and casting in severe fracture. | 1 | 3 | 6 | |||
| C | Type C, sustentacular fragment, no subtype Type C sustentacular fragment. The sustentacular fragment depresses into the burst calcaneal body, creating a large thalamic fragment. |
22/126 (17.46%) | – | – | Burst of calcaneal body | Percutaneous reduction and fixation of calcaneal body | 16 | 6 | – |
The main type A comprised 32, 4 and 15 of subtype A1, A2 and A3 respectively. Whereas, subtype A4 was not found in the study. Thirty two subtype A1 IACF associated with 20 avulsion and 12 bending fracture fragments. Fifteen subtype A3 associated with avulsion fragments.
In 32 A1 and 15 A3 subtype IACFs, the PCF fragment created incongruent posterior subtalar joint with 23.63° (4°–59°) and 25.13° (11°–45°) on axial and sagittal CT images. Whereas, all 4 subtype A2, the PCF fragment remained its congruent posterior subtalar joint with 0.38° (0°–1°) and 0.25° (0°–1°) on axial and sagittal views.
The fractures of subtype A1 and A3 were reduced by percutaneous pin of avulsion and bending fragments for restoring abnormal fracture parameters. Avulsion and bending fragments were fixed to calcaneal body by percutaneous screws. Then, spontaneous reduction of posterior subtalar joint including calcaneal morphology and alignment were obtained (Fig. 3, Table 2).
Fig. 3.
Subtype A1 intra-articular calcaneal fracture, calcaneal radiographs showed burst of lateral calcaneal wall (U) and bending fracture fragment (E) created incongruent posterior subtalar joint (2 pictures above). CT images showed that subtype A1 comprised type A sustentacular fragment (SFA) and entire posterior calcaneal facet (PCF) had intact articular surface (I) and associated with bending fragment of calcaneal body by its articular surface was anterior surface of the bending fragment (2 pictures middle). Percutaneous reduction and 2 screw fixations of the bending fragment were performed (2 pictures below). Pre- and postoperative calcaneal fracture scores improved from 8 to 1 points.
The subtype A2 fracture associated with burst calcaneal body. Percutaneous pin reduction of calcaneal body for restoring abnormal fracture parameters without addressing posterior subtalar joint were performed. Because articular surfaces of the PCF fragment maintained congruent posterior subtalar joint. The fractures were fixed by percutaneous insertion of screws between posterior calcaneal tubercle and inferior calcaneal cortex. Calcaneal morphology and alignment were then obtained (Table 2).
At 6-month follow-up of 51 main type A IACFs, the healed fracture showed postoperative fracture parameter improvements. Radiographic calcaneal fracture scores were improved from 8.33 (4–11) to 3.55 points (0–10) (Table 3).
Table 3.
Fracture parameters and radiographic calcaneal fracture scores of main type A, B and C intra-articular calcaneal fractures.
| Preoperation |
Postoperation |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gissane (°) | Bohler (°) | Varus (°) | Burst (mm) | Length (mm) | Posterior subtalar joint (°) | Fracture scores (points)∗∗ | Gissane (°) | Bohler (°) | Varus (°) | Burst (mm) | Length (mm) | Posterior subtalar joint (°) | Fracture scores (points)∗∗ | |
| Main type A | 97.10 | 3.75 | 9.75 | 7.98 | 79.30 | 29.13 | 8.33 | 112.41 | 21.13 | 5.50 | 5.83 | 83.48 | 2.63 | 3.55 |
| (73–136) | (−9–12) | (−13–18) | (0–13.50) | (64.85–93.23) | (0–47) | (4–11) | (87–127) | (2–40) | (1–9) | (0–11.78) | (65.84–97.10) | (0–9) | (0–10) | |
| Main type B | 96.36 | 10.09 | 3.64 | 8.61 | 80.84 | 16.77 | 8.94 | 110.85 | 15.45 | 3.36 | 6.83 | 82.10 | 6.61 | 4.28 |
| (68–132) | (1–27) | (0–10) | (5.44–13.56) | (70.25–88.68) | (1–42) | (5–11) | (80–119) | (1–26) | (1–11) | (4.85–10.67) | (72.25–93.33) | (1–38) | (0–10) | |
| Main type C | 115.33 | 2 | 4 | 7.22 | 81.34 | 2.60 | 5.95 | 113.33 | 21 | 5.60 | 5.17 | 82.19 | 2.20 | 1.09 |
| (98–120) | (−12–16) | (−15–14) | (3.19–11.38) | (70.25–91.91) | (0–5) | (4–8) | (100–117) | (17–27) | (0–10) | (2.55–10.83) | (65.84–93.69) | (0–4) | (0–5) | |
| Intraobserver I∗ | 0.70 | 0.78 | 0.65 | 0.71 | 0.81 | 0.72 | – | 0.76 | 0.80 | 0.66 | 0.73 | 0.83 | 0.76 | – |
| Intraobserver II∗ | 0.79 | 0.81 | 0.69 | 0.73 | 0.83 | 0.74 | – | 0.81 | 0.85 | 0.67 | 0.74 | 0.86 | 0.75 | – |
| Interobserver∗ | 0.65 | 0.72 | 0.61 | 0.70 | 0.74 | 0.71 | – | 0.69 | 0.75 | 0.63 | 0.72 | 0.73 | 0.72 | – |
∗Intraclass correlation coefficient for reliability of fracture parameters.
∗∗Preoperative calcaneal fracture scores: Bonferroni test for main type A vs. C (p < 0.001), main type B vs. C (p < 0.001) and main type A vs. B (p = 0.999).
∗∗Postoperative calcaneal fracture scores: Bonferroni test for main type A vs. C (p < 0.001), main type B vs. C (p = 0.002) and main type A vs. B (p = 0.999).
In Table 2, main type B IACFs comprised 4, 32, 7 and 10 of subtype B1, B2, B3 and B4 respectively.
The fractures of 4 subtype B1 and 7 B3 associated with avulsion fragment of calcaneal body as subtype A1.
The fractures of 32 subtype B2 and of 10 subtype B4 associated with burst calcaneal body formed a thalamic fragment and multiple articular fragments in calcaneal body respectively. The subtype B4 should similar to subtype A4 although subtype A4 was not found in the study.
In subtype B1, B2 and B3, the lateral PCF fracture created incongruent posterior subtalar joint with 23.11° (3°–55°) and 15.11° (12°–20°) on axial and sagittal views. Whereas, subtype B4 created an intra-articular fracture of the posterior subtalar joint.
The fractures of subtype B1 and B3 were treated by the same surgical technique as subtype A1 and A3. Calcaneal morphology and alignment with spontaneous reduction of posterior subtalar joint were obtained.
The fracture of subtypes B2, was restored to obtain calcaneal morphology by the same surgical technique as subtype A2. Additionally, the thalamic fragment was reduced via 4 cm incision sinus tarsi surgical approach and fixed with SF by screws. The subtype B4 were addressed percutaneously to obtain calcaneal morphology and congruent posterior subtalar joint via sinus tarsi approach. For severe subtype B4, the reduction and casting were done as possible to obtain calcaneal morphology (Fig. 4, Table 2).
Fig. 4.

Subtype B2 intra-articular calcaneal fracture, calcaneal radiographs showed burst of lateral calcaneal wall (U) and a large thalamic fragment (T) created incongruent posterior subtalar joint (2 pictures above). CT images showed that subtype B2 comprised type B sustentacular fragment (SFB) and lateral posterior calcaneal facet (PCF) with intact articular surface (I) associated with burst calcaneal body by a large thalamic fragment (2 pictures middle). Percutaneous reduction and screw fixations were performed. Thalamic fragment was reduced and fixed by a screw via sinus tarsi approach (2 pictures below). Pre- and postoperative calcaneal fracture scores improved from 9 to 1 points.
In main type B IACF, 40 were fixed with percutaneous screws, 7 with percutaneous plating. 6 subtype B4 with severe comminution were treated by casting (Table 2).
At 6-month follow up of main type B, the healed fracture showed postoperative fracture parameter improvements. The calcaneal fracture scores were improved from 8.94 (5–11) to 4.28 points (0–10) (Table 3).
In Table 2, 22 main type C IACF had no subtype. The SF of main type C maintained congruency of posterior subtalar joint with 1° (0°–2°) and 0.25° (0°–1°) on the axial and sagittal CT images respectively. The SF was depressed into the burst calcaneal body and associated with burst calcaneal body by forming a large thalamic fragment.
Percutaneous reduction of the fracture were performed to restore abnormal fracture parameters as subtype A2. Calcaneal morphology and alignment were obtained and no needed addressing posterior subtalar joint. Sixteen fractures were fixed with percutaneous screws and six with percutaneous plating (Fig. 5, Table 2).
Fig. 5.
Main type C intra-articular calcaneal fracture. Calcaneal radiographs showed burst of lateral calcaneal wall (U) and large thalamic fragment (T) (2 pictures above). CT images showed that main type C comprised type C sustentacular fragment without the separated posterior calcaneal facet fragment from the sustentacular fragment. The main type C maintained congruent posterior subtalar joint (2 pictures middle). Percutaneous reduction and 2 screw fixations of calcaneal body were performed without addressing of posterior subtalar joint (2 pictures below). Pre- and postoperative calcaneal fracture scores improved from 5 to 1 points.
At 6-month follow-up, the healed fracture showed postoperative fracture parameter improvements. The calcaneal fracture scores were improved from 5.95 (4–8) to 1.09 points (0–5) (Table 3).
Statistical analyses showed that main type C intra-articular calcaneal fractures had lowest pre- and postoperative fracture scores (p < 0.05). Whereas, main type B, the fractures showed the highest fracture scores (Table 3). Kappa value of inter- and intraobserver reliability were 0.69 (0.62–0.80), 0.82 (0.76–0.89) for main types and 0.58 (0.52–0.68), 0.81 (0.75–0.89) for subtypes. Intraclass correlation coefficients of the fracture parameter measurements were shown in Table 3.
Discussion
The study showed IACFs create 3 different SF configurations including type A, B and C. The SF type A, B and C are used as the key fragments for classifying main type A, B and C IACFs.
Harnroongroj IACF classification system, the fracture is classified based on fracture components of the calcaneal body including avulsion and bending fragments as well as burst calcaneal body.1 The system correlates to reduction technique and choices of treatment.1 So, subtype of the new IACF classification system was classified by incorporation of PCF fractures with Harnroongroj fracture components of calcaneal body. This new classification system provides information of IACF in term of types of SF and PCF fracture associated with fracture components of calcaneal body. These are advantages of the classification system comparing with previous classification systems which did not consider the whole fracture components as this new classification.
In 2009, Schepers, et al reported a comparative study of 49 radiographic and 15 computerized tomographic scan classification systems. The study showed that the most prevalent systems such as Essex-Lopresti, Zwipp, Crosby, and Sanders classifications had no correlation with treatment and moderate interobserver reliability for the Crosby and Sanders classifications.8 When, comparing with the existing classification systems, our new classification system showed correlation with choices of treatment, implant fixation and quality of fracture reduction (Table 2, Table 3). Moreover, interobserver reliability of the new classification system showed substantial and moderate reliability for main types and subtypes which were higher than of existing classifications.11, 12
The next advantage of this classification over previous classifications is about the application in the treatment of IACFs with minimal invasive surgical technique. Minimal invasive surgery is current popular technique for the fracture treatment.4, 5, 6 The technique uses SF as a reference. So, the information about the SF especially type of SF can be achieved from the new classification system and allow the PCF fracture associating with fracture components of calcaneal body to be addressed for restoring posterior subtalar joint.
Pre- and postoperative radiographic calcaneal fracture scores showed the lowest fracture scores for main type C and the highest for main type B. These mean that main type C was simple fracture configuration and had the best quality of fracture reduction. While, main type B had the most complex fracture configuration and had the worst quality of fracture reduction. It could be assumed that the new classification system can provide correlation of fracture configuration of the main types to quality of fracture reduction.
In conclusion, this preliminary study demonstrated that our novel classification system in term of type of SF and incorporation of PCF fracture with fracture components of calcaneal body can be used for classifying IACFs. The classification system correlates to choices of treatment, implant fixation and quality of fracture reduction that might benefit for surgical treatment especially minimal invasive surgery.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Harnroongroj T., Chuckpaiwong B., Angthong C., Nanakorn P., Sudjai N., Harnroongroj T. Displaced articular calcaneus fractures: classification and fracture scores: a preliminary study. J Med Assoc Thai. 2012;95:366–377. [PubMed] [Google Scholar]
- 2.Gitajn I.L., Abousayed M., Toussaint R.J., Ting B., Jin J., Kwon J.Y. Anatomic alignment and integrity of the Sustentaculum tali in intra-articular calcaneal fractures: is the Sustentaculum tali truly constant? J Bone Jt Surg Am. 2014;96:1000–1005. doi: 10.2106/JBJS.M.00330. [DOI] [PubMed] [Google Scholar]
- 3.Sanders R., Fortin P., DiPasquale T., Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 4.Wallin K.J., Cozzetto D., Russell L., Hallare D.A., Lee D.K. Evidence-based rationale for percutaneous fixation technique of displaced intra-articular calcaneal fractures: a systematic review of clinical outcomes. J Foot Ankle Surg. 2014:740–743. doi: 10.1053/j.jfas.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Abdelgaid S.M. Closed reduction and percutaneous cannulated screws fixation of displaced intra-articular calcaneus fractures. Foot Ankle Surg. 2012:164–179. doi: 10.1016/j.fas.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis, 1951–52. Clin Orthop Relat Res. 1993;290:3–16. [PubMed] [Google Scholar]
- 7.Zwipp H., Tscherne H., Thermann H., Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res. 1993;290:76–86. [PubMed] [Google Scholar]
- 8.Schepers T., van Lieshout E.M., Ginai A.Z., Mulder P.G., Heetveld M.J., Patka P. Calcaneal fracture classification: a comparative study. J Foot Ankle Surg. 2009;48:156–162. doi: 10.1053/j.jfas.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Swords M.P., Alton T.B., Holt S., Sangeorzan B.J., Shank J.R., Benirschke S.K. Prognostic value of computed tomography classification systems for intra-articular calcaneus fractures. Foot Ankle Int. 2014;35:975–980. doi: 10.1177/1071100714548196. [DOI] [PubMed] [Google Scholar]
- 10.Harnroongroj T., Tangmanasakul A., Choursamran N., Sudjai N., Harnroongroj T. Measurement technique of calcaneal varus from axial view radiograph. Indian J Orthop. 2015;49:223–226. doi: 10.4103/0019-5413.152489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landis J.R., Koch G.G. The measurements of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 12.Fleiss J.L., Levin B., Paik M.C. 3rd ed. John Wiley & Sons; New Jersey: 2003. Statistical Methods for Rates and Proportions; p. 604. [Google Scholar]