Abstract
Objective
We investigated causes and results of revision surgeries after artificial disc replacement of cervical spine (C-ADR).
Methods
Twenty-one patients (mean age: 52.8) who underwent revision surgery after C-ADR and who had a minimum 2-year of follow-up were included into this study. The mean time between the primary and revision surgeries was 21 months. During their primary surgeries, 14 patients underwent single level C-ADR, 2 two-level C-ADR, and 5 two-level hybrid surgery for 16 radiculopathy, 3 myelopathy, and 2 adjacent segment diseases. Causes for revision surgeries were at least one of the followings: 17 poor patient selections, 7 insufficient decompressions, 7 malpositions, 6 subsidences, 3 osteolysis, and 1 postoperative infection.
Results
Sixteen patients underwent anterior removal of C-ADR, one-level discectomy and fusion (N = 11), two-level discectomy (N = 3) or one-level corpectomy (N = 2) and fusion. Three patients of keel type C-ADR with heterotopic ossification underwent posterior laminoforaminotomy and fusion. Two patients underwent combined procedures due to infection or severe subsidence and osteolysis. At the 2-year follow-up, neck (7.3 vs 1.6) and arm (7.0 vs 1.3) visual analog scales and Neck Disability Index score (46.7 vs 16.32) were improved (all, p < 0.05). According to Odom's criteria, 86% of the patients were satisfied and 91% achieved solid fusion. No major complications developed except for transient dysphagia in 6 patients (29%).
Conclusions
In this small case series, revision surgeries provided successful outcomes in failed C-ADR without major complications. Careful patient selection and meticulous surgical techniques are important to avoid disappointing clinical outcome or even failure of C-ADR.
Level of evidence
Level IV, Therapeutic study.
Keywords: Revision surgeries, Artificial disc replacement, Cervical spine
Introduction
Artificial disc replacement of cervical spine (C-ADR) has been developed to maintain range of motion at operated segment to avoid development of adjacent segment disease (ASD) due to anterior cervical discectomy fusion (ACDF).1, 2, 3 Another goal of C-ADR is to achieve satisfactory outcomes for cervical radiculopathy or myelopathy caused by soft disc herniation or mild spondylosis.4, 5 Many previous studies have reported successful clinical outcomes and maintenance of segmental motion of various types of C-ADR.6, 7 However, some patients also have undergone revision surgeries after C-ADR surgeries including persistence or recurrence of symptoms and complications.
Revision surgeries after C-ADR is technically demanding and regardless of types and designs of C-ADR, previous study on primary C-ADR have resulted in higher rate of revision surgeries compared to ACDF.8, 9, 10 In addition, revision surgeries after C-ADR are reportedly associated with greater hospital costs, longer length of hospital stay, and complications.8 Increasing implantation rates of C-ADR may lead to an increase in revision procedures. However, previous studies were coding data analyses limited to nationwide inpatient sample of USA, but not studies of clinical case series. Therefore, little information is available about clinical and radiological results of revision surgeries after C-TDR. Therefore, it is important to evaluate clinical and radiological outcomes of revision surgeries so as to decide decision-making strategy. In addition, it is essential to investigate causes of failure of C-ADR surgeries to avoid revision surgeries. We performed the current study to investigate these two issues.
Materials and methods
In this retrospective study we reviewed medical records and imaging studies of 21 consecutive patients who underwent revision surgeries after C-ADR. Thirteen patients were male and 8 patients were female. The mean age was 52.8 years (range, 43–63 years) and mean time to revision surgeries was 21 months (range, 4–84 months). All patients had a minimum 2-year follow-up after revision surgeries. All demographic data, clinical and radiological results were summarized in Table 1. During their primary C-ADR surgeries, 14 patients underwent single-level C-ADR (3 C4-5, 8 C5-6, and 3 C6-7), 2 patients had two-level C-ADR (C5-6 and C6-7), and 5 patients had two-level hybrid surgery (3 C6-7 ADR + C5-6 ACDF and 2 C5-6 ADR + C4-5 ACDF). C-ADR prostheses used in these patients were 8 MobiC, 6 Discovery, 3 Prodisc-C, 2 Prestige LP, and 2 Bryan. The indications for the primary C-ADR surgeries were 16 cervical radiculopathy, 3 myelopathy, and 2 adjacent segment disease with radiculopathy.
Table 1.
Summary of demographic data, clinical and radiological results.
| No. | Sex | Age | C-ADR device | Failure level(s) | Time to revision surgery (months) | Revision surgery approach | Overall satisfaction (Odom's criteria) | Fusion status |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 43 | Prodisc-C | C5-6, C6-7 | 20 | Posterior | Good | Fusion |
| 2 | F | 48 | Prodisc-C | C5-6, C6-7 | 34 | Posterior | Good | Fusion |
| 3 | F | 58 | Mobi-C | C5-6 | 27 | Anterior | Fair | Pseudoarthrosis |
| 4 | M | 55 | Bryan | C4-5, C5-6 | 18 | Anterior | Good | Fusion |
| 5 | M | 57 | Discocerv | C5-6, C6-7 | 5 | Anterior | Good | Fusion |
| 6 | F | 53 | Prodisc-C | C4-5, C5-6 | 6 | Anterior | Good | Fusion |
| 7 | M | 43 | Mobi-C | C5-6, C6-7 | 6 | Anterior | Good | Fusion |
| 8 | M | 63 | Prestige LP | C5-6, C6-7 | 13 | Posterior | Fair | Fusion |
| 9 | M | 61 | Discocerv | C5-6 | 18 | Combined | Good | Fusion |
| 10 | M | 53 | Mobi-C | C4-5 | 84 | Anterior | Excellent | Fusion |
| 11 | M | 48 | Mobi-C | C5-6 | 25 | Anterior | Good | Fusion |
| 12 | M | 55 | Discocerv | C5-6, C6-7 | 21 | Anterior | Good | Fusion |
| 13 | F | 52 | Prestige LP | C6-7 | 8 | Anterior | Excellent | Fusion |
| 14 | M | 55 | Discocerv | C6-7 | 4 | Combined | Fair | Fusion |
| 15 | M | 53 | Mobi-C | C4-5 | 20 | Anterior | Good | Fusion |
| 16 | F | 59 | Mobi-C | C5-6 | 17 | Anterior | Good | Fusion |
| 17 | M | 50 | Bryan | C6-7 | 32 | Anterior | Good | Fusion |
| 18 | M | 48 | Discocerv | C5-6 | 22 | Anterior | Good | Pseudoarthrosis |
| 19 | F | 55 | Mobi-C | C5-6 | 10 | Anterior | Good | Fusion |
| 20 | M | 51 | Mobi-C | C6-7 | 16 | Anterior | Excellent | Fusion |
| 21 | F | 49 | Discocerv | C5-6 | 23 | Anterior | Good | Fusion |
Failure of primary C-ADR surgeries was defined as persistence or recurrence of clinical symptoms, such as radiculopathy or myelopathy, due to remained or new pathologies at the same operated level(s). Among 21 patients, 14 temporarily recovered symptoms after primary C-ADR surgeries but had recurrence of symptoms. The remaining 7 patients did not obtain symptom relief immediately after primary C-ADR surgery. Twenty-one patients had additional conservative treatments at least for 3 months but symptoms were not resolved. Therefore, all patients were transferred to the authors' tertiary hospitals and underwent revision surgeries.
Follow-up measurements for clinical and radiological evaluations were taken before surgery and postoperatively at 1, 3, 6, 12, and 24 months as well as at last follow-up. Clinical evaluation was done by neck and arm visual analog scales (VAS) and neck disability index (NDI). At the 24-month of follow-up, the patients' overall satisfaction was graded using Odom's criteria. “Excellent” and “good” were classified as satisfying outcomes and “fair” and “poor” as unsatisfying outcomes. Radiological evaluation for fusion status was done by lateral radiographs of neutral, flexion, and extension positions. Fusion criteria used in current study were less than 2° of movement on the flexion and extension lateral radiographs, and presence of bridging trabecular bone between the endplates on the lateral radiograph. Computed tomography was also used to investigate final fusion status in 19 cases except 2 posterior revision cases.
For statistical analysis, the Wilcoxon signed rank test was used to evaluate the degree of improvement in neck and arm VAS and NDI score following revision surgeries at each time point of follow-up. P-values<0.05 were considered statistically significant.
Results
Causes for failure of C-ADR were at least one of the following: 17 poor patient selections, 7 insufficient decompressions, 7 malpositions with heterotopic ossification, 6 subsidences, 3 osteolysis, and 1 postoperative infection (Fig. 1). The most cause of failure of C-ADR was poor patient selection (81%); 17 patients with severe spondylosis or ossification of posterior longitudinal ligament (OPLL)had persistence (N = 5) or recurrence (N = 12) of clinical symptoms after primary C-ADR surgeries. Seven patients (33%)showed no or little improvement of clinical symptoms due to insufficient decompression after primary C-ADR surgeries. Seven patients (33%) showed malposition of C-ADR including 4 kyphosis and 3 hyperlordosis with heterotopic ossification. Six patients (29%) showed subsidence of C-ADR and three patients (14%) showed osteolysis around C-ADR during follow-up period. Postoperative infection developed in 1 patient (5%) at 4 months after primary C-ADR surgery.
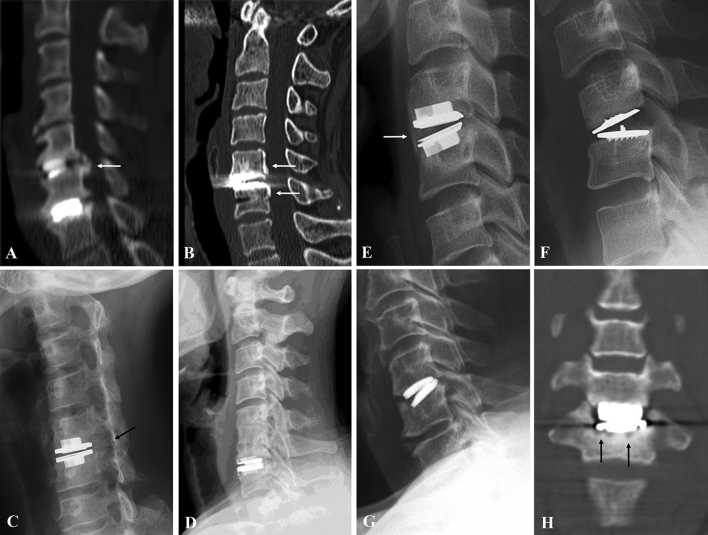
Fig. 1.
Causes of failure of artificial disc replacement of cervical spine: severe spondylosis (white arrow) (A), ossification of posterior longitudinal ligament (white arrows) (B), Foraminal stenosis (black arrow) (C), severe spondylosis adjacent to previous fusion (D), hyperlordotic positioning with heterotopic ossification (white arrow) (E), kyphotic positioning (F), subsidence (G), and osteolysis (black arrows) (H).
Sixteen patients underwent anterior removal of C-ADR device (8 Mobi-C, 4 Discocerv, 2 Bryan, 1 Prodisc-C, and 1 Prestige LP). Among them, eleven patients underwent one-level discectomy and fusion with plate (N = 11) (Fig. 2). Five patients underwent two-level discectomy (N = 3) or one-level corpectomy (N = 2)and fusion with plate (Fig. 3). In three patients with keel type C-ADR device (2 Prodisc-C and 1 Prestige LP), it was difficult to remove C-ADR device due to severe heterotopic ossification or secure fixation. Therefore, three patients were treated by posterior laminoforaminotomy and fusion (Fig. 4). Two patients (2 Discocerv) were treated by combined anterior and posterior approaches due to kyphosis and severe bone loss caused by infection or subsidence (Fig. 5). The types of bone graft used in these patients were 11 freeze-dried allograft plus demineralized bone matrix, 6 cages plus autogenous chip bone, and 4 autogenoustricortical iliac bones.
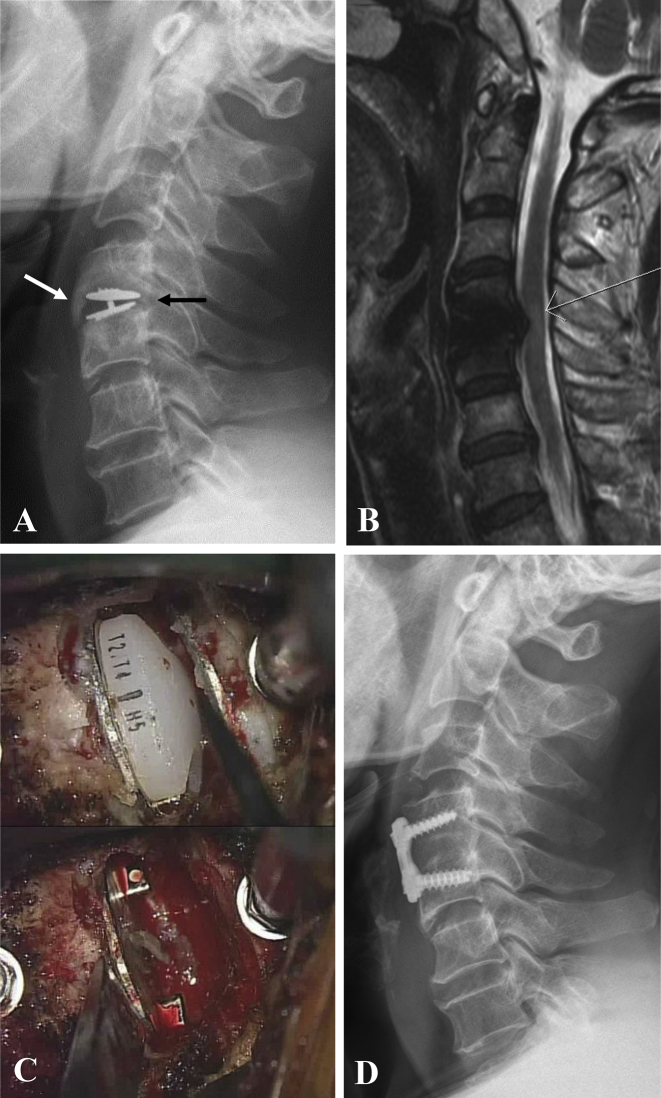
Fig. 2.
Lateral radiograph of cervical spine showed hyperlordotic positioning of prosthesis with extensive heterotopic ossification (white arrow) and incomplete decompression (black arrow) at C4-5 (A). Magnetic resonance imaging showed herniated disc compressing cord at C4-5 (B). Intraoperative photo showed removal of prosthesis (C). Lateral radiograph of 2-year follow-up showed anterior removal of prosthesis, decompression with solid fusion at C4-5 (D).
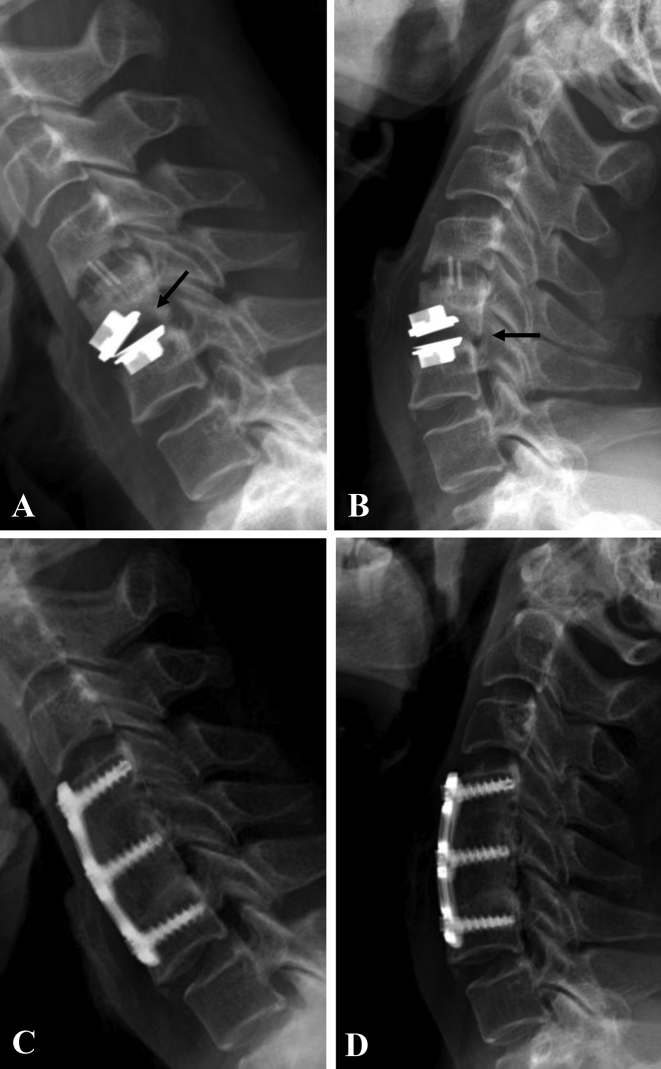
Fig. 3.
Flexion and extension lateral radiographs of cervical spine showed kyphotic positioning of prosthesis with subsidence and incomplete decompression (black arrow) at C5-6 and pseudoarthrosis at C4-5 (A and B). Flexion and extension lateral radiographs of 2-year follow-up showed anterior removal of prosthesis, decompression with solid fusion at C4-5 and C5-6 (C and D).
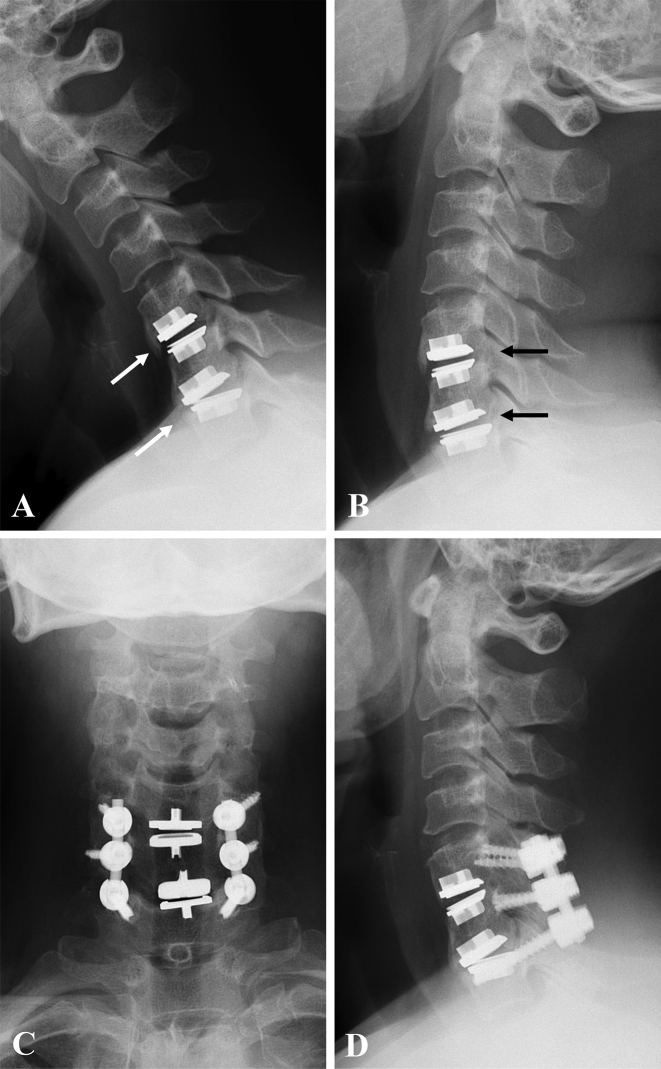
Fig. 4.
Flexion and extension lateral radiographs of cervical spine showed kyphotic positioning of prosthesis with extensive heterotopic ossification (white arrows) and incomplete decompression at C5-6 and C6-7 (black arrows) (A and B). Flexion and extension lateral radiographs of 2-year follow-up showed laminoforaminotomy and posterior fusion at C5-6 and C6-7 (C and D).
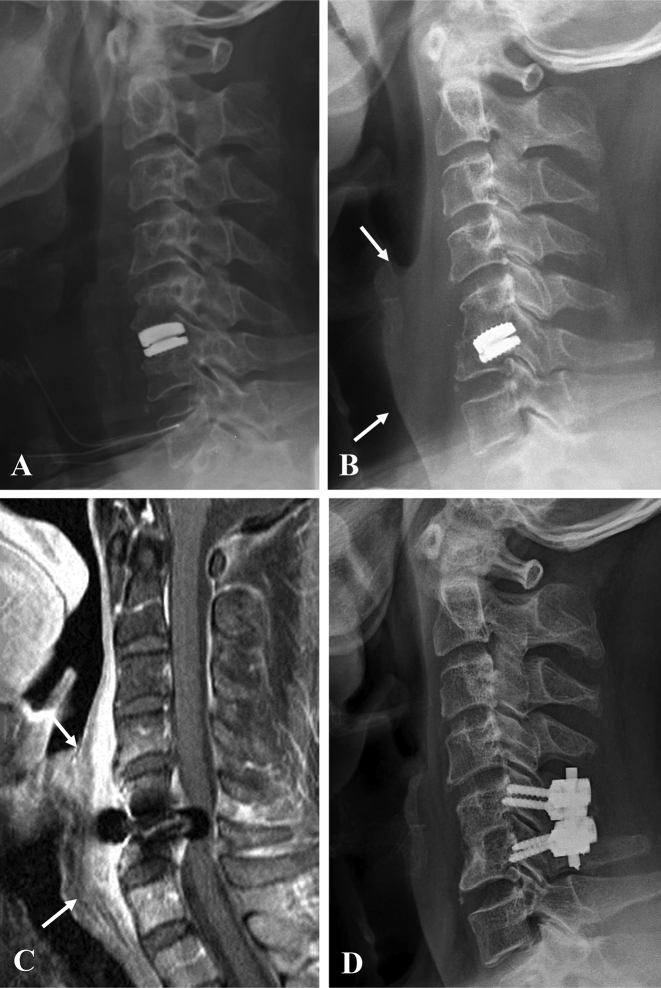
Fig. 5.
Postoperative lateral radiograph of cervical spine showed anterior discectomy and implantation of prosthesis at C5-6 (A). Lateral radiograph of 4-month follow-up showed anterior soft tissue swelling (white arrows) and severe subsidence and retropulsion of prosthesis (B). Magnetic resonance imaging showed anterior abscess formation (white arrows) of C4-7 (C). Lateral radiograph of 2-year follow-up showed anterior removal of prosthesis, decompression and solid fusion, and posterior fixation at C5-6 (D).
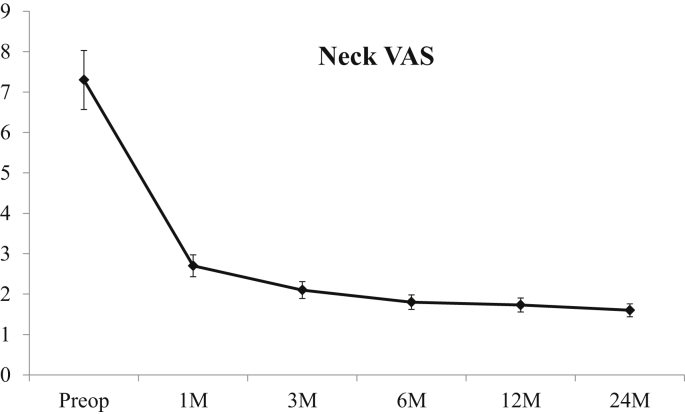
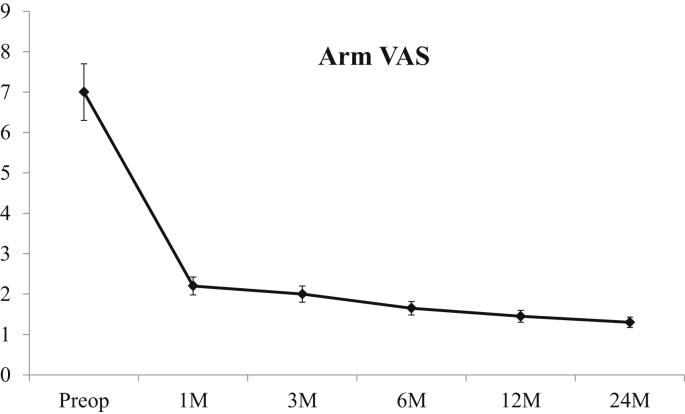
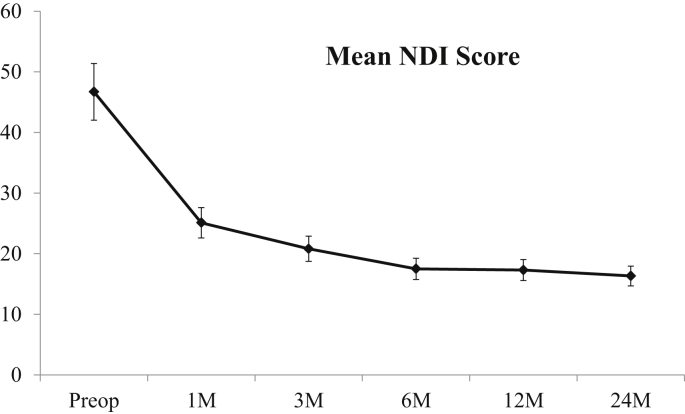
Neck VAS was significantly improved after revision surgeries at 1, 3, 6, and 12 months as well as 24 months (7.3 ± 0.43 vs. 1.6 ± 0.37) (all P < 0.05) (Fig. 6). Arm VAS was significantly improved after revision surgeries at postoperative 1, 3, 6, and 12 months as well as 24 months (7.0 ± 0.38 vs. 1.3 ± 0.37) (all P < 0.05) (Fig. 7). NDI score was also improved after revision surgeries at 1, 3, 6, and 12 months as well as 24 months (46.7 ± 2.85 vs. 16.32 ± 3.19) (all P < 0.05) (Fig. 8). At the 24-month follow-up, 86% (N = 18) of the patients was satisfied with 3 “excellent” and 15 “good” results. However, 14% (N = 3) of the patients showed “fair” results due to myelopathy (N = 2) and pseudoarthrosis (N = 1). Ninety-one percent (N = 19) of the patients achieved solid fusion. However, 2 patients with pseudoarthrosis did not have severe clinical symptoms to warrant the operative repair of the psuedoarthrosis (Fig. 9). Six patients (29%) complained of dysphagia postoperatively but resolved by conservative treatment with mean time of 1.7 months (range, 1–4 months). No major neurologic and wound complications developed.
Fig. 6.
Line graph showing the mean Neck VAS in revision surgeries after artificial disc replacement of cervical spine over time. * indicates p < 0.05.
Fig. 7.
Line graph showing the mean Arm VAS in revision surgeries after artificial disc replacement of cervical spine over time. * indicates p < 0.05.
Fig. 8.
Line graph showing the mean NDI scores in revision surgeries after artificial disc replacement of cervical spine over time. * indicates p < 0.05.
Fig. 9.
Preoperative lateral radiograph of cervical spine showed incomplete decompression with subsidence and kyphosis of C-ADR device (A). Flexion and extension lateral radiographs at postoperative 2-year showed significant instability more than 10 °(black arrows) at C5-6 (B and C). Computed tomography demonstrated pseudoarthrosis at C5-6 (D).
Discussion
The current study was conducted on 21 cases transferred from other hospitals after primary C-ADR surgeries. All patients underwent revision surgeries for failure of primary C-ADR surgeries in authors' hospitals. First, we identified causes of failure of primary C-ADR surgery in these cases. The most common cause was poor patient selection, which meant wrong indication for C-ADR surgery. Here as elsewhere, appropriate patient’ selection is one of the most important factors for the success of C-ADR surgery. However, despite severe spondylosis or OPLL, 81% of the patients underwent C-ADR surgeries for cervical radiculopathy or myelopathy instead of ACDF. In severe spondylosis or OPLL cases, it is difficult to sufficiently decompress pathologies compressing roots or cord. It can result in no or little improvement of clinical symptoms. In addition, maintained range of motion by C-ADR device can cause progression of uncovertebral osteophytes or OPLL with time, which can also result in recurrence of clinical symptoms. Therefore, C-ADR should be applied to strictly limited indications, such as soft disc herniation or mild spondylosis.
The next common causes were insufficient decompression (33%) and malposition of C-ADR (33%). In one third of all failures, the skills of the surgeons should be blamed but not the C-ADR device. These findings suggest that meticulous surgical techniques of experienced spine surgeons are important to avoid failure of C-ADR compared to ACDF. Adequate decompression of nerve root and spinal cord is mandatory to achieve neurologic recovery in C-ADR surgery. In addition, C-ADR device should be ideally placed into the rectangular disc space complying with three conditions: midline centering, lordotic sagittal alignment, and use of maximum size. Malposition of C-ADR causes damages to the normal kinematics of C-ADR device at operated segment so that can cause abnormal biomechanical stress on operated segment more severely.10 This can increase the risk of failure of C-ADR. In addition, preservation of subchondral bone is essential to avoid subsidence or osteolysis of C-ADR device. Finally, postoperative infection can be reduced by minimizing soft tissue damage and reducing bleeding and operation time.
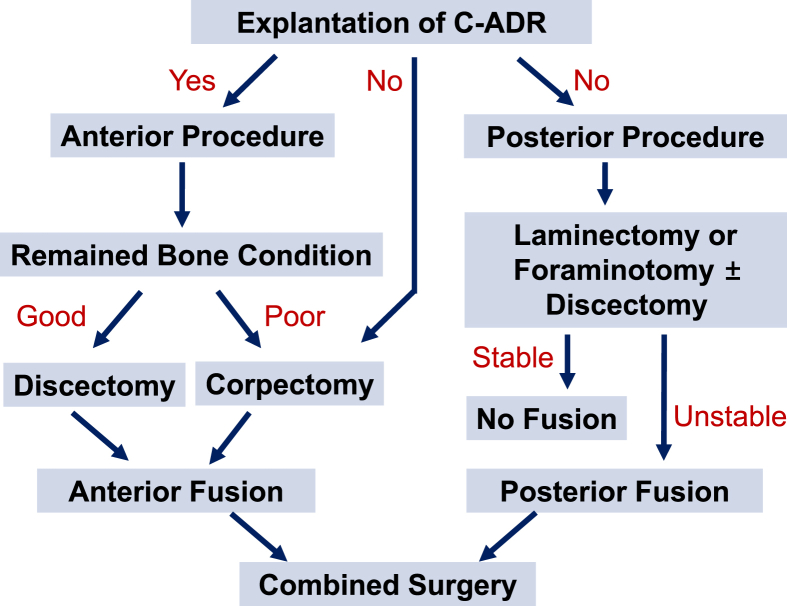
To date, little information is available about revision strategy and the decision-making process to manage failure of C-ADR surgeries. A recent review article addressed reoperations following cervical disc replacement.9 We definitely agree with the author's suggestions about approaches and techniques to manage failure of C-ADR surgeries. Therefore, we summarized algorism of revision strategy to manage failure of C-ADR surgeries in Fig. 10. In the current study, we decide on revision strategy for failure of C-ADR surgeries considering the nature of failure of C-ADR and clinical and radiological pictures of the patients. The first and most important factor to decide approaches is possibility of explantation of the C-ADR device. If possible, the most suitable option is anterior removal of C-ADR device followed by additional decompression and fusion with plate. Sixteen patients (76%; N = 16)were treated with anterior removal of C-ADR device, followed by one-level (52%; N = 11) or two-level decompression (24%; N = 5), and fusion with plate. In 5 patients with two-level decompression and fusion with plate, 3 underwent two-level discectomy and fusion, and 2 underwent one-level corpectomy and two-level fusion due to excessive bone loss caused by explantation of C-ADR device. Three patients with keel type C-ADR device (2 Prodisc-C and 1 Prestige LP) underwent posterior laminoforaminotomy and fusion with lateral mass and pedicle screw fixation. In these 3 patients, heterotopic ossification and secure fixation with keel made it difficult to explant the device. If we maintained resolve for removal of C-ADR device, at least two-level corpectomy and three-level fusion should be done. Therefore, we choose posterior laminoforaminotomy and fusion as less extensive surgery for these patients and achieved satisfactory outcomes. Our rationale of the posterior approach is consistent with previous studies that recommend posterior for aminotomy as a salvage procedure in cases of persistent clinical symptoms following C-ADR surgery. In two cases with kyphosis and bone loss due to infection or severe subsidence and osteolysis, we first performed anterior removal of C-ADR device, debridement of infected bone or subtotal corpectomy, and autogenous tricortical iliac bone graft. In these two extreme cases, the anterior cervical plate could not fit. Therefore, posterior instrumentation and fusion was additionally performed to correct kyphosis and to enhance fusion.
Fig. 10.
Algorism of revision strategy after artificial disc replacement of cervical spine (C-ADR).
The current study demonstrated successful clinical outcomes in terms of neck and arm VAS, NDI score, and overall patient satisfaction using Odom's criteria. Solid fusion was achieved in 91% of the patients based on strict fusion criteria using flexion and extension lateral radiographs and computed tomography. Two patients (9%) showed pseudoarthrosis similar to fibrous union but did not have severe clinical symptoms to warrant the operative repair. No major neurologic and wound complications developed, except for transient dysphagia in 6 patients (29%) with a mean recovery time of 1.7 months (range, 1–4 months). We think that successful outcomes of revision surgeries for failed C-ADR surgeries depend on careful preoperative radiographic review and surgical planning, as well as meticulous surgical techniques of highly experienced cervical spine surgeons in a tertiary hospital setting. The limitation of current study is relatively small number of revision cases. We think that just 21 revision cases are not sufficient to fully discuss causes of failure of C-ADR surgeries and results, such as clinical outcomes, radiological outcomes, and complications, of revision surgeries. Therefore, more large case series are needed to thoroughly investigate these two issues and to establish the revision strategy and decision-making process to manage failure of C-ADR surgeries.
In conclusion, revision surgeries provide successful outcomes in failure of C-ADR surgeries in terms of neck and arm VAS, NDI score, overall patient satisfaction, and fusion status without major neurologic and wound complications. Careful patient selection and meticulous surgical techniques are important to avoid disappointing clinical outcome or even failure of C-ADR surgeries.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Sasso R.C., Best N.M., Metcalf N.H., Anderson P.A. Motion analysis of Bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech. 2008;21(6):393–399. doi: 10.1097/BSD.0b013e318150d121. [DOI] [PubMed] [Google Scholar]
- 2.Cheng L., Nie L., Zhang L., Hou Y. Fusion versus bryan cervical disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009;33(5):1347–1351. doi: 10.1007/s00264-008-0655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Y.C., Nie L., Cheng L., Hou Y. Clinical and radiographic reports following cervical arthroplasty: a 24-month follow-up. Int Orthop. 2009;33(4):1037–1042. doi: 10.1007/s00264-008-0571-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riew K.D., Buchowski J.M., Sasso R., Zdeblick T., Metcalf N.H., Anderson P.A. Cervical disc arthroplasy compared with arthrodesis for the treatment of myelopathy. J Bone Jt Surg Am. 2008;90(11):2354–2364. doi: 10.2106/JBJS.G.01608. [DOI] [PubMed] [Google Scholar]
- 5.Sekhon L.H. Cervical arthroplasty in the management of spondylotic myelopathy. J Spinal Disord Tech. 2003;16(4):307–313. doi: 10.1097/00024720-200308000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Burkus J.K., Traynelis V.C., Haid R.W., Jr., Mummaneni P.V. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial. J Neurosurg Spine. 2014;21(4):516–528. doi: 10.3171/2014.6.SPINE13996. [DOI] [PubMed] [Google Scholar]
- 7.Sasso R.C., Smucker J.D., Hacker R.J., Heller J.G. Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow-up. J Spinal Disord Tech. 2007;20(7):481–491. doi: 10.1097/BSD.0b013e3180310534. [DOI] [PubMed] [Google Scholar]
- 8.Nandyala S.V., Marquez-Lara A., Fineberg S.J., Singh K. Comparison of revision surgeries for one- to two-level cervical TDR and ACDF from 2002 to 2011. Spine J. 2014;14:2841–2846. doi: 10.1016/j.spinee.2014.03.037. [DOI] [PubMed] [Google Scholar]
- 9.Skovrlj B., Lee D.H., Caridi J.M., Cho S.K. Reoperations following cervical disc replacement. Asian Spine J. 2015;9(3):471–482. doi: 10.4184/asj.2015.9.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh K., Phillips F.M., Park D.K., Pelton M.A., An H.S., Goldberg E.J. Factors affecting reoperations after anterior cervical discectomy and fusion within and outside of a Federal Drug Administration investigational device exemption cervical disc replacement trial. Spine J. 2012;12(5):372–378. doi: 10.1016/j.spinee.2012.02.005. [DOI] [PubMed] [Google Scholar]