Abstract
This article presents a 48-year-old male patient who presented with pain in the left forearm and weakness and clumsiness in the left hand of 6 months' duration. Flexor motor strength loss of the thumb and the index finger was present and neurophysiologic tests showed findings compatible with axonal injury in the anterior interosseous nerve (AIN) innervated muscles. Magnetic resonance imaging revealed a space-occupying lesion in the proximal forearm resembling a glomus tumor. Excision of the mass and release of the AIN were performed. Histopathology confirmed a glomus tumor, and the patient remains asymptomatic at 1 year postoperatively. We stress the importance of imaging studies in patients when a suspected secondary nature of nerve entrapment is present.
Keywords: Glomus tumor, Anterior interosseous nerve syndrome
Introduction
Glomus tumors are mostly benign, rare lesions originating from the neuromyoarterial glomus body. The normal glomus body is a specialized arteriovenous anastomosis that plays a role in thermoregulation in reticular dermis. Glomus tumor was first clinically and pathologically described by Masson in 1923.1 Glomus tumors are usually found in the subcutaneous layer of the subungual or digital pulp.1 Extradigital glomus tumors have been also reported in the palm, wrist, forearm, foot, bone, stomach, colon, cervix, and mesentery.2 Glomus tumors generally present with solitary, bluish subcutaneous lesions with the classic triad of pin point tenderness, severe pain, and cold intolerance.2
Anterior interosseous nerve syndrome (AINS) is a rare entrapment peripheral neuropathy of the upper extremity. Anterior interosseous nerve innervates the flexor pollicis longus (FPL), the flexor digitorum profundus (FDP) of the index and middle finger, and the pronator quadratus (PQ) muscles.3 It also provides sensation to the radiocarpal, intercarpal, carpometacarpal, and radioulnar joints. The most frequent clinical features are localized pain in the forearm, spontaneous weakness or motor loss of the FPL, the FDP of the index finger, and PQ, and occasionally FDP of the middle finger.3 The incidence of the AIN palsy is low and is less than 1% off all entrapment neuropathies in the upper extremity.4 Since the AIN does not innervate the skin, AINS is not associated with sensory loss.
This study presents a rare case of a patient with AINS caused by a glomus tumor in the forearm, a rare localization.
Case report
A 48-year-old man presented with pain in the flexor aspect of the left forearm and loss of strength with clumsiness in the left hand that started 6 months ago. The pain had worsened over time. On clinical examination, local tenderness was present in the anterior proximal forearm and the symptoms exacerbated with palpation over the tender area. Tinel's sign was also strongly positive over this area. The flexor motor strength of the thumb and the index finger was Medical Research Council Scale for Muscle Strength grade 3/5. No sensory deficit was observed.
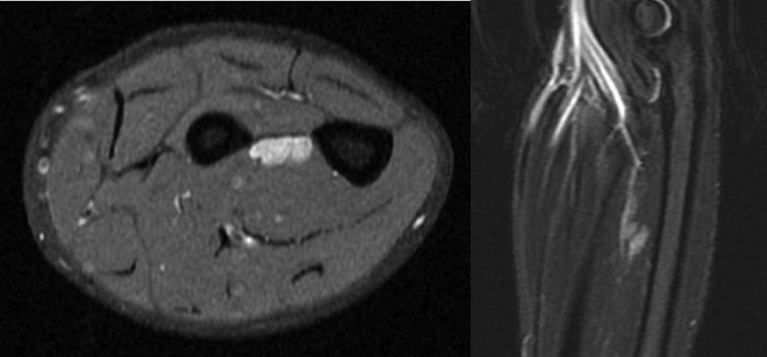
On neurophysiological examination, nerve conduction studies of the median and ulnar nerves revealed normal motor and sensory nerve velocities. F responses were normal. Needle electromyography (EMG) of the PQ muscle showed denervation patterns and moderate reduced motor unit action potential activity. Needle examination of the FPL and the FDP muscles showed intense positive sharp waves and fibrillation potentials. The EMG findings were pathological and were compatible with axonal injury. Magnetic resonance imaging (MRI), obtained in search of a morphological etiology, revealed a deep mass of 13 × 6 × 30 mm in size in the proximal forearm, just anterior to the interosseous membrane, adjacent to the interosseous neurovascular bundle (Fig. 1).
Fig. 1.
MR images revealing a deep space-occupying lesion localized in the proximal flexor aspect of the forearm, just anterior to the interosseous membrane.
Marginal excision of the mass and release of the AIN were performed (Fig. 2). Histopathological evaluation confirmed a glomus tumor, appearing as a well circumscribed, encapsulated lesion composed of monomorphic round cells with centrally located round nuclei and capillary size vessels lined by flattened endothelium surrounding the mass (Fig. 3). The patient's symptoms were completely resolved and he remains asymptomatic at 1 year postoperatively.
Fig. 2.
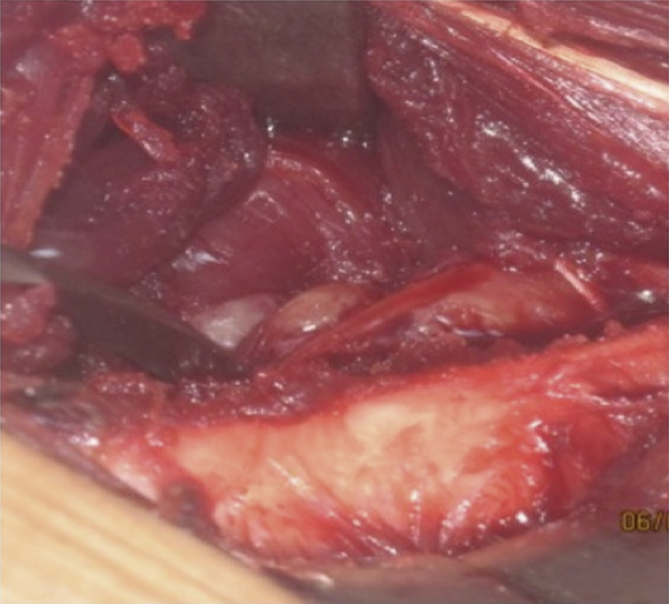
Intraoperative photograph of the lesion.
Fig. 3.
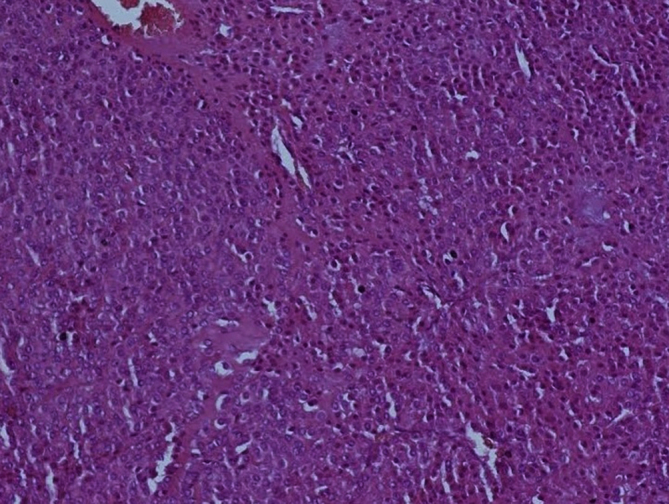
A high-power microscopic view shows uniform cells, intermixed with the blood vessels (Stain, hematoxylin and eosin; original magnification, ×200).
Discussion
Glomus tumors (also known as glomangiomas or nonchromaffin paraganglioma) can present with severe functional disability and severe pain in the involved extremity, localized tenderness, and cold intolerance.2 Seventy-five per cent of glomus tumors are found in the hand, and 65% are located in the fingertip.5 Occurrence of glomus tumors in atypical localizations other than the hand may lead to difficulties in diagnosis. Physical examination is unremarkable in 50% of lesions.6
Folpe et al examined 52 extradigital atypical glomus tumors and found that none of the lesions were located in the forearm.7 Previously, 2 cases of superficial glomus tumors in the forearm have been described, but the pain was not caused by tumor-induced compression of a major nerve or the tumor had no connections with major blood vessels at that level.8, 9 A few cases of intravascular glomus tumors of the forearm have been reported as well.10, 11
Only a few studies have reported nerve entrapment syndromes due to glomus tumors localized in the forearm. In their study, Martínez-Villén et al retrospectively reviewed 541 patients who were operated on due to nerve compressions and tumors of the forearm and the hand.12 They have found that 22 patients showed compression neuropathy associated with 17 tumors and 6 tumor-like lesions, with 13 different histopathology. Of these, 2 were due to glomus tumors localized in the distal forearm. The superficial branch of the radial nerve was compressed in one patient and the dorsal sensory branch of the ulnar nerve was compressed in the other. Jiga et al reported a case of venous glomangioma causing chronic compression of the radial sensory nerve in the forearm.13 The compressed nerve was a sensory nerve in all of these patients and compression of the AIN was not mentioned.
In recent studies, the etiology of AINS is suggested to be a typical transient neuritis and likely to be related to Parsonage-Turner syndrome (PTS).2 Parsonage-Turner syndrome is caused by neuralgic amyotrophy and the symptoms may be pain and motor and/or sensory dysfunction in one or in multiple peripheral nerves of the upper extremity, including isolated AIN palsy.3 The etiology of PTS remains unknown but appears to be immune mediated. Differential diagnosis is crucial in PTS patients, as they would not benefit from local decompression.
A recent study, using high-resolution magnetic resonance neurography, claimed that diagnostic evidence for the existence of fascicular or partial median nerve lesions could be shown and that AINS is not an entrapment neuropathy of the AIN itself, but is a motor fascicular neuropathy of the median nerve trunk. The authors strongly suggested that AINS is actually an immune mediated inflammatory disorder and cautioned against surgical treatment options.14 However, we, as well as others, believe that operative decompression of the AIN is indicated when the symptoms persist more than 3 months.3, 4
Gantzer muscles, which are two different anomalous bellies in the deep flexor region of the forearm inserting into either the FDP or the FPL muscles, are another proposed etiology for AINS, but although Gantzer muscles are frequent finding (almost 50% in cadaver studies), AINS is a rare entity.2 Although a compressing mass may be the etiology of AINS and may present the typical clinical symptoms, it has not been reported yet in the literature.
Trauma is another common etiology for AINS.3 Surgery in the forearm, dressings, slings, and venipuncture are suggested as the reasons for iatrogenic injury.3 Anterior interosseous nerve dysfunction was also reported after shoulder arthroscopy.3
However, local compression of the AIN in the forearm may often be associated with space-occupying lesions or fibrous bands of the pronator teres muscle. Preoperative MRI can reveal any existing space-occupying lesions and if any, delineate the relationship between the lesion and adjacent structures allowing the surgeon to plan the operation. It is also possible to detect glomus tumors with MRI. T1-weighted MR images show glomus tumors as dark, well-delineated lesions with low signal intensity and T2-weighted images show them as bright lesions with high signal intensity. Glomus tumors as small as 5 mm in the fingertip has been successfully shown with MRI.15 On the other hand, MRI can also help for identifying AINS. Diffuse edema of AIN innervated muscles on T2-weighted fat-saturated images that is apparent with increased signal intensity is a frequent finding in favor of AINS.16
Here, we describe a rare case of a glomus tumor in an atypical localization, causing severe atypical pain and neurologic dysfunction by compression of the anterior interosseous nerve. In the literature, glomus tumors are rarely reported to localize in the forearm and have not been reported yet as an etiological factor for AINS or any other nerve compression syndrome.
In conclusion, we report a case of an extradigital glomus tumor arising in the proximal anterior aspect of the forearm and causing a rare nerve entrapment syndrome. Atypical tumor localizations and varying symptoms may interfere with the diagnosis and the treatment of extradigital glomus tumors. Therefore, although glomus tumors are most commonly located in the digits, probability of atypical localizations should be kept in mind. A detailed medical history, a through physical examination, and appropriate imaging modalities may be helpful for the correct diagnosis.
Conflicts of interest
No funds were received in support of this work. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Steffen C. The man behind the eponym: C. L. Pierre Masson. Am J Dermatopathol. 2003;25:71–76. doi: 10.1097/00000372-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Weiss S.W., Goldblum J.R., Folpe A.L. Perivascular tumors. In: Weiss S.W., Goldblum J.R., editors. Enzinger and Weiss's Soft Tissue Tumours. 5th ed. Mosby; Philadelphia, PA: 2007. pp. 751–769. [Google Scholar]
- 3.Rodner C.M., Tinsley B.A., O'Malley M.P. Pronator syndrome and anterior interosseous nerve syndrome. J Am Acad Orthop Surg. 2013;21:268–275. doi: 10.5435/JAAOS-21-05-268. [DOI] [PubMed] [Google Scholar]
- 4.Ulrich D., Piatkowski A., Pallua N. Anterior interosseous nerve syndrome: retrospective analysis of 14 patients. Arch Orthop Trauma Surg. 2011;131:1561–1565. doi: 10.1007/s00402-011-1322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carroll R.E., Berman A.T. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Jt Surg Am. 1972;54:691–703. [PubMed] [Google Scholar]
- 6.Rettig A.C., Strickland J.W. Glomus tumor of the digits. J Hand Surg Am. 1977;2:261–265. doi: 10.1016/s0363-5023(77)80121-4. [DOI] [PubMed] [Google Scholar]
- 7.Folpe A.L., Fanburg-Smith J.C., Miettinen M., Weiss S.W. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1–12. doi: 10.1097/00000478-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Nigam J.S., Misra V., Singh A., Karuna V., Chauhan S. A glomus tumour arising from the flexor aspect of the forearm: a case report with review of the literature. J Clin Diagn Res. 2012;6:1559–1561. doi: 10.7860/JCDR/2012/4233.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoenleber S.J., Rosenberg A.E., Temple H.T. Painful forearm mass in a 75-year-old man. Clin Orthop Relat Res. 2014;472:776–780. doi: 10.1007/s11999-013-3409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acebo E., Val-Bernal J.F., Arce F. Giant intravenous glomus tumor. J Cutan Pathol. 1997;24:384–389. doi: 10.1111/j.1600-0560.1997.tb00808.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee S.K., Song D.G., Choy W.S. Intravascular glomus tumor of the forearm causing chronic pain and focal tenderness. Case Rep Orthop. 2014;2014 doi: 10.1155/2014/619490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martínez-Villén G., Badiola J., Alvarez-Alegret R., Mayayo E. Nerve compression syndromes of the hand and forearm associated with tumours of non-neural origin and tumour-like lesions. J Plast Reconstr Aesthet Surg. 2014;67:828–836. doi: 10.1016/j.bjps.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Jiga L.P., Rata A., Ignatiadis I., Geishauser M., Ionac M. Atypical venous glomangioma causing chronic compression of the radial sensory nerve in the forearm. A case report and review of the literature. Microsurgery. 2012;32:231–234. doi: 10.1002/micr.20983. [DOI] [PubMed] [Google Scholar]
- 14.Pham M., Bäumer P., Meinck H.M. Anterior interosseous nerve syndrome: fascicular motor lesions of median nerve trunk. Neurology. 2014;82:598–606. doi: 10.1212/WNL.0000000000000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matloub H.S., Muoneke V.N., Prevel C.D., Sanger J.R., Yousif N.J. Glomus tumor imaging: use of MRI for localization of occult lesions. J Hand Surg Am. 1992;17:472–475. doi: 10.1016/0363-5023(92)90353-q. [DOI] [PubMed] [Google Scholar]
- 16.Dunn A.J., Salonen D.C., Anastakis D.J. MR imaging findings of anterior interosseous nerve lesions. Skelet Radiol. 2007;36:1155–1162. doi: 10.1007/s00256-007-0382-7. [DOI] [PubMed] [Google Scholar]