Abstract
Objective
Idiopathic flexible pes planus (IFPP) is a common foot problem in adolescents and young adults. Hypothesis for the present study was that combination of procedures for IFPP can achieve results in adolescents and young adults that are as good as those seen in adult-acquired pes planovalgus (AAPP) treatment in adults.
Methods
A total of 21 feet of 18 patients (10 boys, 8 girls) with mean age of 15.6 years underwent surgical reconstruction for flatfoot deformity. Symptomatic patients who had been unresponsive to conservative treatment were included in study group. Mean follow-up time was 39.2 months. American Orthopedic Foot and Ankle Society (AOFAS) scores were calculated for all patients, and based on final results, all families were asked whether or not they would elect to have the surgery again in same circumstances.
Results
All procedures were performed by the same surgeon: lateral column calcaneal lengthening osteotomy on 21 feet; percutaneous lengthening or gastrocnemius recession for Achilles tendon on 21 feet; medializing calcaneal osteotomy on 15 feet; flexor digitorum longus tendon transfer on 15 feet; medial cuneiform opening wedge osteotomy on 5 feet, spring ligament plication on 3 feet, and accessory navicular bone excision on 2 feet.
Preoperative mean AOFAS score increased significantly from 56.76 to 95.29. All parents stated that they were satisfied with surgery results and would choose to have the same surgery performed again.
Conclusion
Soft tissue and bony procedures used for reconstruction of AAPP can be used safely for IFPP in adolescents and young adults.
Level of clinical evidence
Level IV, Therapeutic study.
Keywords: Adolescent, Flexible flatfoot, Osteotomy, Pes planus
Idiopathic flexible pes planus (IFPP) is a common foot problem in adolescents and young adults.1 Although IFPP resolves spontaneously in most cases, surgery may be necessary if conservative treatment fails.2 Surgical indications, timing, and procedures for IFPP remain controversial.3, 4
Management of symptomatic IFPP begins with education of the patient and parents.1 Foot orthoses, stretching, shoe modifications, activity modifications, manipulation, serial casting, weight regulation in obese patients, and medications for pain relief and inflammation are conservative treatment modalities.2, 5
Symptomatic IFPP patients who are unresponsive to conservative treatment and have symptoms such as pain or early deformation of the shoe may be candidates for surgical treatment. Although there is still no consensus about indications, efficacy, or type of procedure for surgical IFPP reconstruction, there are several options for surgical treatment in adolescents and young adults. Several authors recommend use of arthroereisis, while others prefer to use osteotomy or soft tissue procedures.6, 7
Osteotomy combined with soft tissue procedures is rarely performed on young patients,8, 9 but there are several arguments that perhaps it should be.10 Present study hypothesis was that combined procedures for IFPP can achieve results in adolescents and young adults as good as those seen in adult-acquired pes planovalgus (AAPP) treatment in adults.
Patients and methods
Patients with symptomatic, flexible, idiopathic flatfoot were included in this retrospective study. Institutional review board approved the study, and written, informed consent was obtained from all study participants. Between June 2005 and January 2013, 18 patients with 21 affected feet (10 boys, 8 girls), who had mean age of 15.6 years (range: 9–25 years), underwent surgical reconstruction for flatfoot deformities at university hospital. Postoperative follow-up was conducted at 6, 12, and 24 weeks. After last follow-up, all patients were called annually. Mean total follow-up time was 51.2 months (range: 13.7–104.6 months). All procedures were performed by the same surgeon. Procedures were: lateral column calcaneal lengthening (LCL) osteotomy in 21 (100%) feet, percutaneous Achilles tendon lengthening or gastrocnemius recession in 21 (100%), medializing calcaneal osteotomy in 15 (71.4%), flexor digitorum longus tendon (FDL) transfer in 15 (71.4%), medial cuneiform opening wedge (Cotton) osteotomy in 5 (23.8%), spring ligament plications in 3 (14.3%), and accessory navicular bone excision in 2 (9.5%) feet. For autograft, preferred material to be used for LCL osteotomy was bone harvested from iliac crest, but in 7 patients, tricortical allograft was used due to parent preference.
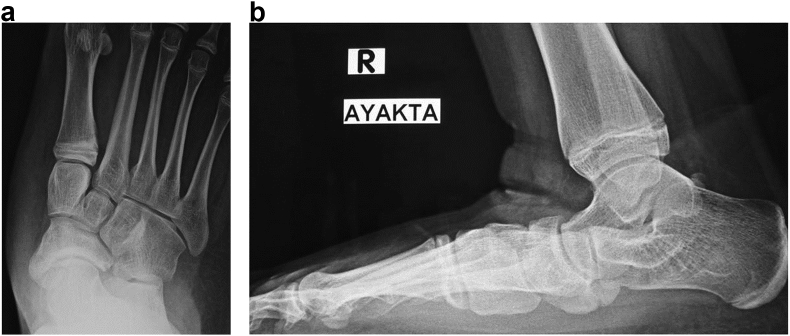
All patients had received conservative treatment for at least 12 months, including methods such as custom-made insoles and Achilles tendon stretching exercises. Patients and their parents were educated about natural course of condition by the senior surgeon. Patients who were still symptomatic after conservative treatment period of 12 months and who had radiographic changes like increased talonavicular uncoverage, decreased calcaneal inclination and talo-first metatarsal angles were accepted as candidates for surgery. Radiographic measurements were taken with standing anteroposterior (AP) and lateral radiographs (Fig. 1a and b). Patients with tarsal coalitions and congenital vertical talus were excluded from the study.
Fig. 1.
a. Preoperative anteroposterior x-ray of foot. Notice accessory navicular bone. b. Preoperative lateral x-ray of foot. Notice accessory navicular bone and talar sag.
Operative technique
All patients were operated on under general anesthesia in supine position. First, Achilles tendon examination was made using Silfverskiöld test to determine selection of gastrocnemius recession or percutaneous Achilles lengthening. Once Achilles procedure was completed, harvesting of autologous bone graft from iliac crest was performed in autograft cases.
When Achilles procedure and graft harvest were complete, thigh tourniquet was inflated. LCL was chosen as first step because forefoot abduction and talonavicular coverage was insufficient in all patients. Osteotomy site was located approximately 1.5 cm proximal to calcaneocuboid joint, and before osteotomy was completed, calcaneocuboid joint was temporarily stabilized with K-wire. Lamina spreader was used to determine adequate graft size. Usually, 8–11 mm grafts were sufficient, depending on degree of deformity. After application of graft, K-wire or cannulated screw was used in retrograde fashion to stabilize graft.
Following LCL procedure, hindfoot valgus was checked clinically. If it persisted, then medializing calcaneal osteotomy was performed. Subsequent to osteotomy, posterior fragment was displaced medially to achieve at least 8–10 mm of displacement, and fixation was achieved with 1 or 2 cannulated screws.
FDL tendon was then transferred. It was placed at level distal to Henry's knot, as described by Haddad and Mann,11 and prepared tendon was passed through hole in navicular bone and sutured to itself under tension. Before harvesting FDL tendon, spring ligament and posterior tibial tendon (PTT) were examined. If loose, spring ligament was plicated with 2 non-absorbable, braided sutures. Minimal PTT degeneration was noted in <50% of the patients; no PTTs were sacrificed.
If supination deformity of forefoot remained, next step was Cotton osteotomy. Required distraction was determined under fluoroscopy and graft was placed at osteotomy site.
For patients with accessory navicular, resection of accessory bone was followed by fixation of PTT with suture anchor. Before fixation of PTT, spring ligament was checked for rupture; if it was ruptured, tendon fixation was performed after spring ligament repair. When all incisions were closed, bulky cotton padding and short leg splint were applied.
Postoperative care
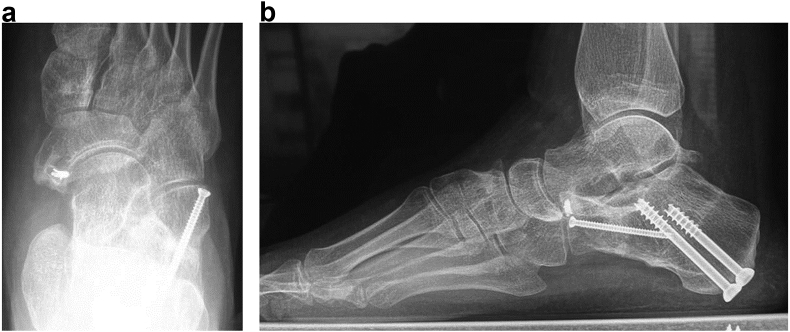
Patients were not permitted to bear weight for 6 weeks. At 6 weeks, when adequate consolidation was observed at osteotomy sites, temporary fixation materials were removed and patients were allowed to bear weight, as tolerated, in walking boot for 4-week period (Fig. 2a and b). At postoperative week 10, patients were told to wear sports shoes and return on week 12 for follow-up X-ray. On AP radiograph, talonavicular coverage, talocalcaneal, and talo-first metatarsal angles were measured. Talocalcaneal angle, talo-first metatarsal angle, talohorizontal angle, and calcaneal inclination were measured on lateral radiographs. In addition to radiographic measurements, AOFAS hindfoot and ankle scores were calculated for all patients preoperatively and at final follow-up examination.
Fig. 2.
a. Postoperative anteroposterior x-ray of right foot. Excision of navicular accessory bone and repair of posterior tibial tendon with suture anchor was achieved. b. Postoperative lateral x-ray of right foot. Procedures performed were: medializing calcaneal osteotomy, lateral column lengthening, medial cuneiform osteotomy, flexor digitorum longus tendon transfer, and percutaneous Achilles tendon lengthening.
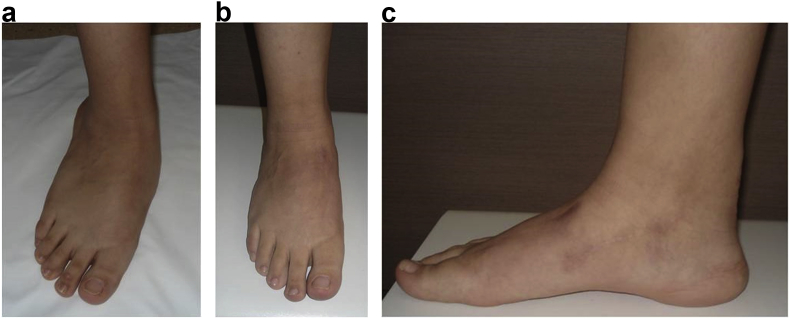
Patients and their parents were asked whether they were pleased with surgery results and whether they would choose to undergo the surgery again in similar circumstances (Fig. 3a, b, c). Wilcoxon signed-rank test was used to compare numerical parameters in statistical analysis and p < 0.05 was accepted as statistically significant. Pillai's Trace test was used for repeated measures analysis and Bonferroni correction was applied to paired comparisons. All analyses were performed using SPSS software (version 11.5; SPSS Inc., Chicago, IL, USA).
Fig. 3.
a. Preoperative front view of right foot. b. Postoperative front view of right foot. c. Postoperative lateral view of right foot.
Results
Radiographic analysis revealed significant improvements in talo-first metatarsal (p = 0.002), calcaneal inclination (p = 0.005), and talohorizontal angles (p = 0.002) in lateral radiographs, and talo-first metatarsal (p = 0.001) and talonavicular coverage angles (p = 0.007) in AP radiographs. Although improvement was seen in lateral talocalcaneal and AP talocalcaneal angles, difference was not statistically significant (Table 1). All patients were evaluated at final follow-up visits in January 2014. Preoperative mean AOFAS score increased significantly from 56.76 (range: 48–73) to 95.29 (range: 90–100; p = 0.001). All patients and their parents stated that they were satisfied with surgery results and would undergo the surgery again in the same circumstances. Three patients with symptomatic bilateral deformities requested surgery on the other foot.
Table 1.
Preoperative and postoperative measurements.
| Mean preop value (degrees) | Mean postop value (degrees) | p-value | ||
|---|---|---|---|---|
| Lateral | Talo–first metatarsal angle | 12.9 | 3.7 | 0.002 |
| Calcaneal inclination angle | 12.9 | 19.5 | 0.005 | |
| Talocalcaneal angle | 36.9 | 39.4 | 0.217 | |
| Talohorizontal angle | 28.0 | 19.7 | 0.002 | |
| AP | Talo-first metatarsal angle | 12.3 | 6.4 | 0.018 |
| Talonavicular coverage angle | 25.0 | 12.6 | 0.007 | |
| Talocalcaneal angle | 25.7 | 21.5 | 0.142 | |
p 0.05 was accepted as statistically significant.
AP: Anteroposterior.
Procedures performed were: LCL osteotomy in 21 (100%) feet, percutaneous lengthening or gastrocnemius recession for Achilles tendon in 21 (100%), medializing calcaneal osteotomy in 15 (71.4%), FDL tendon transfer in 15 (71.4%), Cotton osteotomy in 5 (23.8%), spring ligament plications in 3 (14.3%), and accessory navicular bone excision in 2 (9.5%). For autografts, harvested bone from iliac crest was the preferred material used for lateral column lengthening osteotomy, but in 7 cases, tricortical allograft was used due to parent preference.
Complications occurred in 2 patients. There was pain at osteotomy site related to implant in 1 patient, which was relieved after implant removal. Second complication was non-union of allograft used in LCL procedure. As patient was asymptomatic, no intervention was performed and patient was still happy with the result.
Discussion
In this study, it has been demonstrated that surgical approach used to treat adult-acquired IFPP can also be used safely for adolescents and young adults, thereby supporting study hypothesis.
Discussion as to whether children with IFPP require treatment is ongoing and no optimal standard for treatment yet exists.12, 13 Surgical treatment is indicated when conservative treatments fail.14 However, this algorithm is not always useful because decision to operate on a child with symptomatic flatfoot does not depend just on the knowledge and experience of the surgeon; it also depends on subjective aspects of medicine and surgery. Thus, surgeons who are not familiar with flatfoot surgery and who have not followed a child with severe flatfoot for at least a decade may prefer conservative treatment regardless of symptoms or deformity. However, we believe that symptomatic patients are candidates for surgical intervention to relieve symptoms and prevent permanent deformities, as well as to provide a better quality of life for the future.
For adolescents and young adults with IFPP, same procedures typically performed for treatment of AAPP were applied and were successful.
After calcaneal osteotomy and Cotton osteotomy, there should be improvement in calcaneal inclination, talonavicular coverage, and in talometatarsal and talocalcaneal angles. Our findings demonstrate efficacy of osteotomy, as seen in previous studies.8, 9 We also found significant improvement in lateral talo-first metatarsal angle (p = 0.002) and in lateral talohorizontal angle (p = 0.002), confirming radiological indication of effectiveness of combined treatment.
Cotton osteotomy decreases pressure in lateral column of the foot.15 Reduction in pressure is thought to be source of reduced lateral column pain. Although we did not document preoperative or postoperative baropedographic measurements, none of present study patients had lateral column pain, even those who did not undergo Cotton osteotomy. This could be due to young age and greater soft tissue flexibility of study participants. This was also surmised in previous studies,8, 9 but cannot be verified as result of limited study populations.
Improvements achieved in present study group were not limited to radiography results. There were also significant improvements in AOFAS scores. Patient pain diminished or disappeared, and they achieved better walking distance. In addition, all patients and their families are satisfied with surgery results and stated that they would undergo the same surgery again in same circumstances (3 patients, as noted, were operated on bilaterally). Two complications were encountered. One was a painful implant used in medializing calcaneal osteotomy; pain resolved after implant removal. The other complication was allograft non-union, which was noticed in follow-up radiographs. It was not symptomatic, so no other intervention was performed and patient had no complaint during continued follow-up. This complication may have been due to premature removal of fixation material; more time may have been required for allograft to become incorporated. Allografts and autografts don't differ in terms of non-union, and thus allografts may be an alternative.16 In addition, K-wires may be used to fix graft material.1, 17 It is opinion of the authors that non-union may be related to longer time required for allograft to become incorporated.18 However, to prove this, a much larger study group would be required.
There is an association between accessory navicular bone and flatfoot. However, less than 1% of patients with accessory navicular bone are symptomatic.19 Relationship between accessory bones and flatfoot may be related to altered pull of PTT at the insertion site. As a result, mechanically inefficient PTT allows foot to deviate into valgus, and this may cause painful or symptomatic flatfoot.20 However, Sullivan and Miller21 suggested the opposite and concluded that presence of accessory navicular played no role in development of flatfoot. Although controversy persists about any relationship, when there is symptomatic flatfoot deformity related to symptomatic accessory navicular, then reconstruction of longitudinal arch will be required in addition to resection of accessory navicular and reinsertion or advancement of PTT. As previously mentioned, though symptomatic accessory navicular removal will often help relieve pain, it will not be sufficient with coexisting flatfoot deformity.22 In the present study, 2 patients who had symptomatic accessory navicular bone with flatfoot were treated with LCL osteotomy, accessory navicular excision, and FDL transfer. In addition, 1 patient had gastrocnemius recession, and the second had medializing calcaneal osteotomy, percutaneous Achilloplasty, Cotton osteotomy, and spring ligament plication. Again, current study patient group is too small to reach any robust conclusion, but combined treatments do seem to be useful for such patients.
Lateral column osteotomy is preferred treatment in IFPP cases and combination surgeries have not typically been preferred for this population.8, 9, 23 After LCL, medial longitudinal arch is re-established and soft tissues of medial foot usually require stretching. Thus, we decided to perform combination surgeries. Surgeries such as Kidner procedure are commonly used to stretch medial soft tissue, but current study authors believe that using FDL, as reported in this study, is a more anatomically correct procedure, supporting PTT without harmful effect on foot function,24 while simultaneously checking spring ligament.25 Thus, we prefer to use FDL tendon transfer, as is performed on adults.8, 9
More than 50% of PTT is degenerated in majority of AAPP cases, such that tendon may be sacrificed. However, in present sample, minimal PTT degeneration (<50%) was observed and no tendons sacrificed8; this may have been due to increased tendon flexibility of younger cohort.
This study was limited by its relatively small sample size and absence of additional objective measurements (such as baropedography) and a control group. A further limitation was that preoperative degree of deformity differed among patients; therefore, they did not all undergo identical surgeries. Even when similar procedures were performed, soft tissue condition, degree of correction, and initial deformity conferred variability.
In conclusion, soft tissue and bony procedures used to reconstruct AAPP can also be safely applied to adolescents and young adults. Both radiological and clinical improvements were observed in present study group.
Conflict of interest
None declared.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Blitz N.M., Stabile R.J., Giorgini R.J., DiDomenico L.A. Flexible pediatric and adolescent pes planovalgus: conservative and surgical treatment options. Clin Podiatr Med Surg. 2010;27:59–77. doi: 10.1016/j.cpm.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Yeagerman S.E., Cross M.B., Positano R., Doyle S.M. Evaluation and treatment of symptomatic flatfoot. Curr Opin Pediatr. 2011;23:60–67. doi: 10.1097/MOP.0b013e32834230b2. [DOI] [PubMed] [Google Scholar]
- 3.Mosca V.S. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4:107–121. doi: 10.1007/s11832-010-0239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manusov E.G., Lillegard W.A., Raspa R.F., Epperly T.D. Evaluation of pediatric foot problems: Part II. The hindfoot and the ankle. Am Fam Physician. 1996;54:1012–1026. [PubMed] [Google Scholar]
- 5.Rome K., Ashford R.L., Evans A. Non-surgical interventions for paediatric pes planus. Cochrane Database Syst Rev. 2010;7:CD006311. doi: 10.1002/14651858.CD006311.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Roth S., Sestan B., Tudor A., Ostojic Z., Sasso A., Durbesic A. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int. 2007;28:991–995. doi: 10.3113/FAI.2007.0991. [DOI] [PubMed] [Google Scholar]
- 7.Jay R.M., Din N. Correcting pediatric flatfoot with subtalar arthroereisis and gastrocnemius recession: a retrospective study. Foot Ankle Spec. 2013;6:101–107. doi: 10.1177/1938640012470714. [DOI] [PubMed] [Google Scholar]
- 8.Oh I., Williams B.R., Ellis S.J., Kwon D.J., Deland J.T. Reconstruction of the symptomatic idiopathic flatfoot in adolescents and young adults. Foot Ankle Int. 2011;32:225–232. doi: 10.3113/FAI.2011.0225. [DOI] [PubMed] [Google Scholar]
- 9.Akimau P., Flowers M. Medium term outcomes of planovalgus foot correction in children using a lateral column lengthening approach with additional procedures ‘a la carte’. Foot Ankle Surg. 2014;20:26–29. doi: 10.1016/j.fas.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Roye D.P., Jr., Raimondo R.A. Surgical treatment of the child's and adolescent's flexible flatfoot. Clin Podiatr Med Surg. 2000;17:515–530. [PubMed] [Google Scholar]
- 11.Haddad S.L., Mann R. Flatfoot deformity in adults. In: Coughlin M.J., Mann R.A., Saltzman C.L., editors. Surgery of the Foot and Ankle. Mosby Elsevier; Philadelphia: 2007. pp. 1033–1039. [Google Scholar]
- 12.D'Amico J.C. The flat-footed child-to treat or not to treat: what is the clinician to do? J Am Podiatr Med Assoc. 2008;98:386–393. doi: 10.7547/0980386. [DOI] [PubMed] [Google Scholar]
- 13.Harris E.J. The natural history and pathophysiology of flexible flatfoot. Clin Podiatr Med Surg. 2010;27:1–23. doi: 10.1016/j.cpm.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Moraleda L., Salcedo M., Bastrom T.P., Wenger D.R., Albiñana J., Mubarak S.J. Comparison of the calcaneo-cuboid-cuneiform osteotomies and the calcaneal lengthening osteotomy in the surgical treatment of symptomatic flexible flatfoot. J Pediatr Orthop. 2012;32:821–829. doi: 10.1097/BPO.0b013e3182648c74. [DOI] [PubMed] [Google Scholar]
- 15.Yarmel D., Mote G., Treaster A. The Cotton osteotomy: a technical guide. J Foot Ankle Surg. 2009;48:506–512. doi: 10.1053/j.jfas.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Templin D., Jones K., Weiner D.S. The incorporation of allogenic and autogenous bone graft in healing of lateral column lenghtening of the calcaneus. J Foot Ankle Surg. 2008;47:283–287. doi: 10.1053/j.jfas.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 17.Kwon J.Y., Myerson M.S. Management of the flexible flat foot in the child: a focus on the use of osteotomies for correction. Foot Ankle Clin. 2010;15:309–322. doi: 10.1016/j.fcl.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Ehrler D.M., Vaccaro A.R. The use of allograft bone in lumber spine surgery. Clin Orthop. 2000;371:38–45. doi: 10.1097/00003086-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Senses I., Kiter E., Gunal I. Restoring the continuity of the tibialis posterior tendon in the treatment of symptomatic accessory navicular with flat feet. J Orthop Sci. 2004;9:408–409. doi: 10.1007/s00776-004-0793-4. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs A.M. Soft tissue procedures for the stabilization of medial arch pathology in the management of flexible flatfoot deformity. Clin Podiatr Med Surg. 2007;24:657–665. doi: 10.1016/j.cpm.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Sullivan J.A., Miller W.A. The relationship of the accessory navicular to the development of the flat foot. Clin Orthop Relat Res. 1979;144:233–237. [PubMed] [Google Scholar]
- 22.Prichasuk S., Sinphurmsukskul O. Kidner procedure for symptomatic accessory navicular and its relation to pes planus. Foot Ankle Int. 1995;16(8):500–503. doi: 10.1177/107110079501600807. [DOI] [PubMed] [Google Scholar]
- 23.Viegas G.V. Reconstruction of the pediatric flexible planovalgus foot by using an Evans calcaneal osteotomy and augmentative medial split tibialis anterior tendon transfer. J Foot Ankle Surg. 2003;42:199–207. doi: 10.1016/s1067-2516(03)70029-5. [DOI] [PubMed] [Google Scholar]
- 24.van der Krans A., Louwerens J.W., Anderson P. Adult acquired flexible flatfoot, treated by calcaneocuboid distraction arthrodesis, posterior tibial tendon augmentation, and percutaneous Achilles tendon lengthening: a prospective outcome study of 20 patients. Acta Orthop. 2006;77:156–163. doi: 10.1080/17453670610045858. [DOI] [PubMed] [Google Scholar]
- 25.Den Hartog B.D. Flexor digitorum longus transfer with medial displacement calcaneal osteotomy. Biomechanical rationale. Foot Ankle Clin. 2001;6:67–76. doi: 10.1016/s1083-7515(03)00079-2. [DOI] [PubMed] [Google Scholar]