Abstract
Objective
The aim of this study was to compare the unilateral and bilateral approaches in treating osteoporotic vertebral compression fractures.
Methods
Based on the principles and methods of the Cochrane systematic reviews, the records of the Cochrane Library, PubMed, Web of Science, Chinese Bio-medicine database, China Journal Full-text Database, VIP database, and Wanfang database were reviewed until October 2014. The randomized controlled trials on unilateral and bilateral approaches to percutaneous vertebroplasty (PVP)/percutaneous kyphoplasty (PKP) for osteoporotic vertebral compression fractures were included. The risk of bias of included trials was assessed based on the Cochrane Handbook for Systematic Reviews of Interventions Version. The RevMan Software 5.0 was used for meta-analysis.
Results
Fifteen randomized controlled trials with a total of 850 patients were included. Risk of bias in the included studies was inevitable. There was no statistically significant difference in visual analog scale, vertebral height, kyphotic angular, and quality of life. The main operative complications were bone cement leakage and adjacent vertebral fracture, without difference between the two groups.
Conclusions
In view of the current evidence, there is insufficient evidence to show any difference between the unilateral and bilateral approaches in both the PVP and PKP treatment in osteoporotic vertebral compression fractures.
Level of Evidence
Level I, Therapeutic study.
Keywords: Minimally invasive surgery, Osteoporotic vertebral compression fracture, Percutaneous kyphoplasty, Percutaneous vertebroplasty, Systematic review
Osteoporosis is a skeletal disease with the characteristic of low bone mass and micro architectural deterioration of bone tissue, which increases the risk of fracture.1 With the aging of society, the incidence rate tends to increase yearly. One of the most common complications,2 osteoporotic vertebral compression fracture (OVCF), leads to persistent chest and/or waist pain. It has severe consequences for patient quality of life.
Conservative treatment takes a long time to achieve pain relief, while open surgery has slow recovery. In addition, open surgery can have many complications, such as hypostatic pneumonia or urinary tract infection as result of long-term bed rest. Therefore, minimally invasive surgery (MIS) has been increasingly favored. Percutaneous vertebroplasty (PVP) was first used in the 1980s, and was used in OVCF shortly thereafter. Addition of percutaneous kyphoplasty (PKP) represented an improvement that was also applied in clinical practice.3 PVP and PKP have been shown to be effective in the reinforcement of a fractured vertebral body.4, 5 In addition, quick remission of pain and long-term analgesic effect effectively improve the quality of life of patients.6, 7
In the early stage, bilateral approach was used for procedure. However, due to advantages of simple surgery and short operative time, unilateral approach has also been widely accepted. Therefore, systematic review was designed to provide the highest level quality of evidence in determination of superior approach in MIS for OVCF.8 The goal of this systematic review of randomized controlled trials (RCT) was to identify differences between unilateral and bilateral approaches in treating OVCF, and to establish a reference for clinicians.
Patients and methods
Criteria for considering studies for this review
-
1
Types of studies
Relevant RCT were included; controlled clinical trials and quasi-randomized studies were excluded.
-
2
Types of participants
Patients who were diagnosed with OVCF were included without discrimination based on age, sex, or race. Vertebral compression fracture was diagnosed based on imaging. Osteoporosis was defined as decreased bone mineral density diagnosed using World Health Organization guidelines.9
-
3
Types of interventions
Unilateral approach and bilateral approach were compared.
-
4Types of outcome measures
- Primary outcomes
-
a)Visual analog scale (VAS) score
-
b)Vertebral height
-
c)Kyphotic angle
-
a)
- Secondary outcomes
-
d)Quality of life
-
e)Complications
-
d)
Search method for identification of studies
The Cochrane Library, PubMed, Web of Science, Chinese Bio-medicine database, China Academic Journals Full-text Database, VIP database, and Wanfang database were searched using the search terms “osteoporosis,” “osteoporoses,” “osteoporotic,” “fractures, compression,” “spinal fractures,” “percutaneous vertebroplasty,” “percutaneous vertebroplasty,” “vertebral plasty,” “percutaneous kyphoplasty,” “percutaneous kyphoplasty,” “unilateral,” “unipedicular,” “unilateraly,” “bilateral,” “bipedicular,” and “bipediculary.” Entries of all databases through October 2014 were searched. The search strategy to identify randomized trials was implemented according to the description in the Cochrane Handbook for Systematic Reviews of Interventions.10 In addition, references cited in articles were checked manually to identify other eligible studies.
Data collection and analysis
-
1
Selection of studies
The title, abstract, and keywords of every record were scanned by 2 authors independently to determine whether the studies should be assessed further. The full article was then examined to decide if it met the inclusion criteria. When there was disagreement, the reviewers resolved it through discussion. The reviewers attempted to contact article authors by e-mail if any information was not available.
-
2
Assessment of risk of bias
Two authors assessed risk of bias of included trials independently as described in the Cochrane Handbook for Systematic Reviews of Interventions10 using the following criteria: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias.
-
3
Data analysis
Review Manager (RevMan) 5.0 software (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was used to perform statistical analysis. For dichotomous data, relative risk and associated 95% confidence interval (CI) were calculated, while weighted mean difference and 95% CI were calculated for continuous data. When there was no statistically significant heterogeneity (p ≥ 0.10, I2 ≤ 50%), meta-analysis was conducted using fixed-effect model; otherwise, possible reasons were explored or random-effect model was used for significant heterogeneity (p < 0.10, I2 > 50%). When data could not be extracted for meta-analysis, the data from these trials were assessed as descriptive data and still considered in the results of the review.
Results
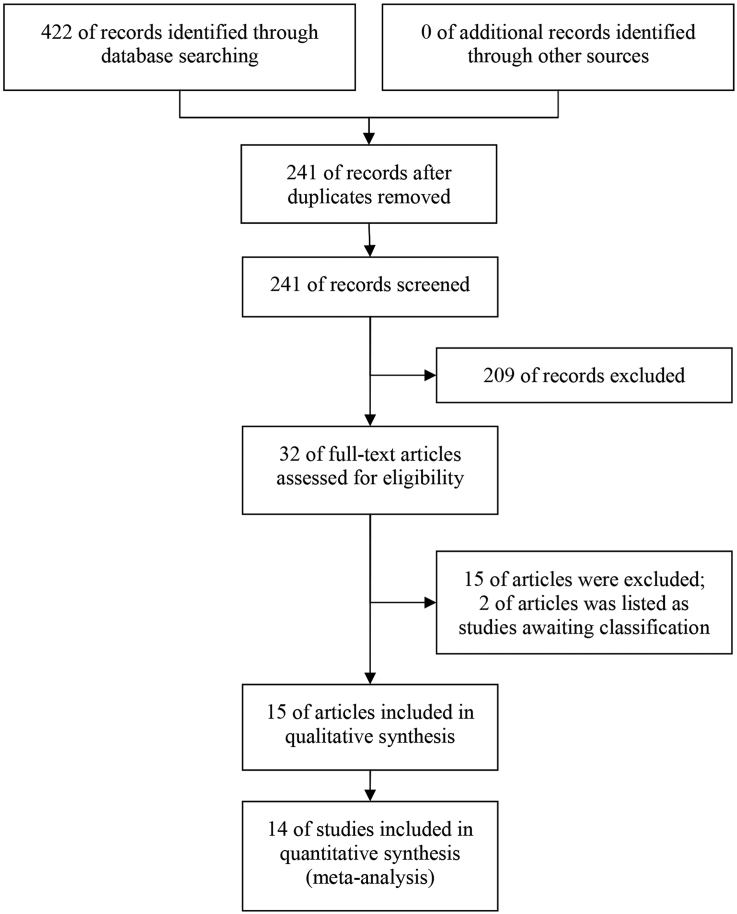
Description of studies
The initial search identified 422 references; 390 articles were subsequently excluded after reading titles and abstracts because they were duplicates or inconsistent with study objectives for the review. Thirty-two references were retrieved for further assessment, and 15 references11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 were excluded because they did not meet the inclusion criteria. Two references26, 27 were listed as studies awaiting classification, because those articles lacked information and we could not get in touch with the authors. Finally, 15 studies28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 were included. Fig. 1 illustrates flowchart of literature screening as described in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.43
Fig. 1.
Flowchart of literature screening.
A total of 850 OVCF patients were included and follow-up period ranged from 2 weeks to 54 months. Groups were well matched at the baseline based on information obtained from studies. Table 1 provides details of the included studies.
Table 1.
Characteristics of included studies.
| Study | Year | Operative methods | Groups | Number of patients (male/female) | Number of vertebrals | Age, mean (SD), yrs | BMI, mean (SD), kg/m2 | Follow-up | Outcomes* |
|---|---|---|---|---|---|---|---|---|---|
| Huang S28 | 2013 | PVP | Unilateral | 9/13 | 22 | 67.9 (9.6) | NR† | (25.0 ± 8.1) months | a, b, c, d, e |
| Bilateral | 11/13 | 24 | 65.7 (10.0) | NR | (26.9 ± 8.1) months | ||||
| Kong JJ29 | 2012 | PVP | Unilateral | 26/20 | NR | 63.5 (14.5) | NR | NR | a |
| Bilateral | 25/21 | NR | 64.5 (15.5) | NR | NR | ||||
| Wang W30 | 2013 | PVP | Unilateral | 10/15 | 51 | 66.9 | NR | 1 year | a, b, d, e |
| Bilateral | 8/14 | 45 | 68.7 | NR | |||||
| Zhang CL31 | 2013 | PVP | Unilateral | 7/21 | NR | 65.68 (5.31) | NR | NR | a, d |
| Bilateral | 6/18 | NR | 65.13 (5.26) | NR | |||||
| Zhang JX32 | 2009 | PVP | – | 11/32 | NR | 71.4 | NR | NR | a, e |
| Zhang LG33 | 2014 | PVP | Unilateral | 36 | NR | 70.0 (2.9) | NR | 1 year | a, d, e |
| Bilateral | 32 | NR | 70.7 (2.5) | NR | |||||
| Zhang X34 | 2014 | PVP | – | 25/28 | 62 | 70 (0.27) | NR | 1 year | a, b, e |
| Zeng ZJ35 | 2013 | PKP, PVP | – | 27/33 | NR† | 64.26 (3.37) | NR | 3 years | b, d |
| Chen CM36 | 2010 | PKP | Unilateral | 33 | 38 | 67.73 (7.05) | −3.08 (0.47) | 2 weeks | a, b, d, e |
| Bilateral | 25 | 28 | 68.52 (7.26) | −2.89 (1.38) | |||||
| Chen L37 | 2011 | PKP | Unilateral | 4/20 | NR | 70.4 | NR | 2 years | a, b, c, d, e |
| Bilateral | 4/21 | NR | 72.4 | NR | |||||
| Gu XH38 | 2009 | PKP | – | 17/35 | 52 | 71.3 | NR | (10–18) months | a, b, c, e |
| Li GZ39 | 2012 | PKP | – | 11/29 | 55 | 69.3 | NR | (6–22) months | a, b, c, e |
| Mao JG40 | 2013 | PKP | Unilateral | 34/16 | 56 | 64.2 (1.7) | NR | 3 months | a, c |
| Bilateral | 31/19 | 52 | 61.3 (1.9) | NR | |||||
| Zhang QG41 | 2012 | PKP | – | 6/17 | 32 | 76.4 | NR | 1 month | a, b, d, e |
| Zhou MW42 | 2013 | PKP | – | 36/31 | 97 | 67.1 | NR | (18–54) mouths | a, b, c, d |
*: a: VAS; b: vertebral height; c: kyphotic angular; d: quality of life; e: complications.
†: NR: no report.
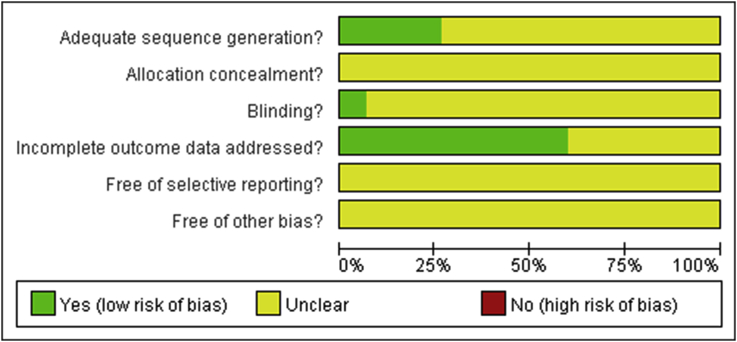
Risk of bias in included studies
Table 2 and Fig. 2 are summaries of the risk of bias in the included trials. Only 4 trials indicated that random number table was used to generate allocation sequence, while all trials were described as randomized. Only 1 trial reported blinding to the patients and surgeons. More than half of the trials had missing data or patients lost to follow-up. We tried to get in touch with authors by e-mail, but did not receive any response.
Table 2.
Risk of bias in included studies.
| Study | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|
| Huang S28 | Yes (random number table) | Unclear | Unclear | Yes | Unclear | Unclear |
| Kong JJ29 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Wang W30 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Zhang CL31 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Zhang JX32 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Zhang LG33 | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
| Zhang X34 | Yes (random number table) | Unclear | Unclear | Yes | Unclear | Unclear |
| Zeng ZJ35 | Yes (random number table) | Unclear | Yes | Yes | Unclear | Unclear |
| Chen CM36 | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
| Chen L37 | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
| Gu XH38 | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
| Li GZ39 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Mao JG40 | Yes (random number table) | Unclear | Unclear | Yes | Unclear | Unclear |
| Zhang QG41 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Zhou MW42 | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
Yes: ‘Low risk’ of bias; No: ‘High risk’ of bias; Unclear: ‘Unclear risk’ of bias.
Fig. 2.
Risk of bias graph.
Effects of interventions
Of the 15 included trials, 7 studies28, 29, 30, 31, 32, 33, 34 reported operating method of PVP, 7 articles36, 37, 38, 39, 40, 41, 42 reported operating method of PKP, and 135 was a comparison of PVP and PKP.
Effects of PVP
-
a)
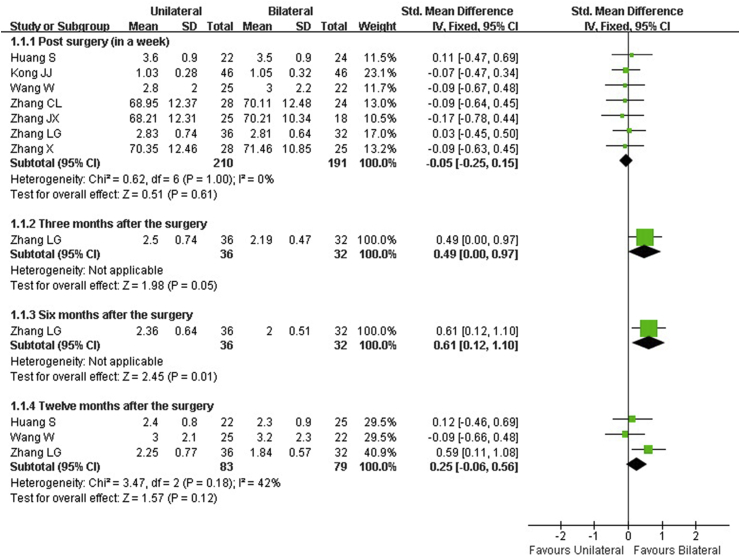
VAS score
Seven articles28, 29, 30, 31, 32, 33, 34 reported VAS score from time point of post surgery (in a week) and 3, 6, 12 months after surgery. There was no statistical heterogeneity between trials in results from post surgery and 12 months after surgery (p = 1.00, I2 = 0%; p = 0.18, I2 = 42%). The result of pooled data revealed no statistical difference between unilateral and bilateral PVP for OVCF (Fig. 3).
-
b)
Vertebral height
Fig. 3.
Unilateral versus bilateral percutaneous vertebroplasty, results for visual analog score.
Four articles28, 30, 34, 35 reported vertebral height at time point of post surgery (in a week) and at 6, 12, 18, 24, 30, and 36 months after the surgery. Pooled data from 3 studies at post surgery (in a week)28, 30, 34 and 2 studies at 12 months after the surgery30, 35 yielded no statistical difference between unilateral and bilateral PVP for OVCF (SMD [standardized mean difference] = −0.10, 95% CI, −0.42 to 0.23; SMD = 0.10, 95% CI, −0.35 to 0.55). The only one reporting data at 6, 18, 24, 30, and 36 months, conducted by Zeng,35 also presented the same results.
-
c)
Kyphotic angle
Only 1 article28 reported the outcome of kyphotic angle post surgery (in a week). There was no statistical difference in unilateral and bilateral PVP for OVCF in this report.
-
d)
Quality of life
Quality of life measure was reported in 5 studies.30, 32, 33, 35, 37 The Oswestry Disability Index (ODI) was used at the time point of post surgery (in a week) and at 1 year after the surgery by Huang.28 The Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) was used at post surgery point (in a week) in 2 studies30, 31 and at 1 year after surgery in Wang's study.30 The Quality of Life Questionnaire of the European Foundation for Osteoporosis was used post surgery (in a week) and 3, 6, and 12 months after the surgery by Zhang.33 The Modified Barthel Index of activities of daily living (MBI of ADL) was used at 6, 12, 18, 24, 30, and 36 months after the surgery by Zeng.35 Significant difference only could be seen at 3, 6, and 12 months after surgery in the study conducted by Zhang,33 while there was no significant difference between 2 groups in the other studies.
Effects of PKP
-
a)
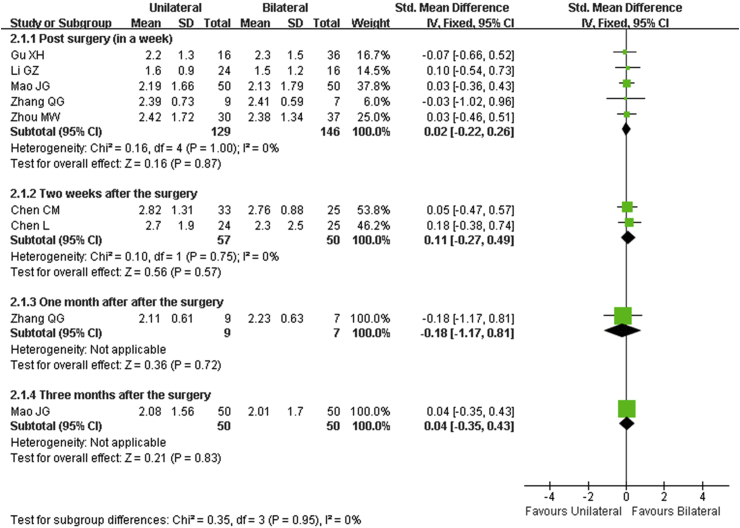
VAS score
Seven articles36, 37, 38, 39, 40, 41, 42 reported VAS score at the time point of post surgery (in a week) and at 2 weeks, and at 1 and 3 months after the surgery. There was no statistical heterogeneity between trials at post surgery (in a week) and 2 weeks after the surgery (p = 1.00, I2 = 0%; p = 0.75, I2 = 0%). Result of pooled data indicated no statistical difference between unilateral and bilateral PKP for OVCF (Fig. 4).
-
b)
Vertebral height
Fig. 4.
Unilateral versus bilateral percutaneous kyphoplasty, results for visual analog score.
Six articles35, 36, 37, 39, 41, 42 reported vertebral height at the time point of post surgery (in a week) and at 2 weeks and 1, 6, 12, 18, 24, 30, and 36 months after surgery. The pooled data from 4 studies at post surgery (in a week)37, 39, 41, 42 revealed no statistical difference between unilateral and bilateral PKP for OVCF (SMD = −0.13, 95% CI, −0.43 to 0.17). There was no statistical difference between the 2 operative methods at 2 weeks after surgery in the report by Chen,36 or at 1 month after the surgery in the report by Zhang.41 Zeng35 reported the same results at 6, 12, 18, 24, 30, and 36 months.
-
c)
Kyphotic angle
Five articles37, 38, 39, 40, 42 reported kyphotic angle at the time point of post surgery (in a week) and 3 months after the surgery. The result of pooled data showed that there was no statistical difference between unilateral and bilateral PKP for OVCF (SMD = −0.05, 95% CI, −0.28 to 0.18). Mao40 reported that there was no statistical difference between unilateral and bilateral PKP for OVCF at 3 months after the surgery.
-
d)
Quality of life
Quality of life was reported by 4 studies.37, 38, 39, 43 ODI was used 2 weeks after the surgery by Chen36 and at 1 month after the surgery by Zhang.41 The SF-36 was used post surgery (in a week) by Chen.37 MBI of ADL was used at 6, 12, 18, 24, 30, and 36 months after the surgery by Zeng.35 There was no significant difference between the 2 groups in any of the reports.
Complications
Twelve of the included studies described the outcome of complications.28, 30, 32, 33, 34, 35, 36, 37, 38, 39, 41, 42 Four studies32, 35, 38, 39 reported that there were no complications in the follow-up period. The most common complication, bone cement leakage, was reported in 8 studies,28, 30, 33, 34, 36, 37, 41, 42 although there were no neurological symptoms or other clinical consequences. Adjacent vertebral fracture was another complication described.28, 34, 37, 41
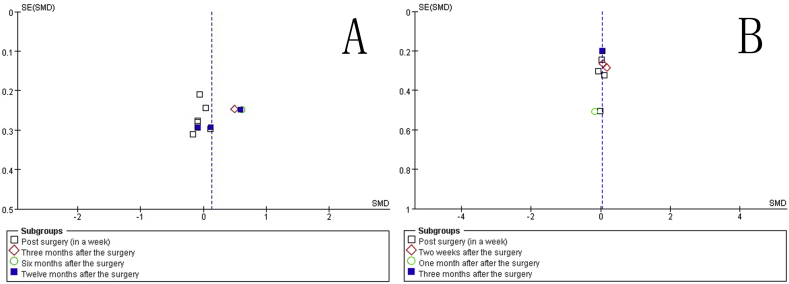
Publication bias
Funnel graph plots SMD against the standard error of SMD for VAS score. The open circles indicate individual studies. The line in the center represents the pooled SMD. Asymmetry in the funnel plot indicates a risk of publication bias (Fig. 5).
Fig. 5.
Funnel plot of included studies. (a) Funnel graph for visual analog score of percutaneous vertebroplasty. (b) Funnel graph for visual analog score of percutaneous kyphoplasty. Asymmetry in the funnel plot indicates a risk of publication bias.
Discussion
Differences in results of 15 RCT examining unilateral and bilateral approaches in treating OVCF were summarized in this systematic review. Based on the outcomes of VAS score, vertebral height, kyphotic angle, quality of life, and complications, this review demonstrated that there was no difference between unilateral and bilateral approaches at different time points. However, because of the low quality of this evidence, further research is very likely to impact our confidence level in the estimate of effect and is likely to change the estimate.
This review identified 15 RCT. Approximately one-quarter of included studies detailed the method of randomization and none of them described allocation concealment. Therefore, there is a possibility of selection bias. Only 1 reported the implementation of blinding. Thus, performance bias was inevitable. We contacted the authors by e-mail for unavailable information; however, we did not receive any response. Publication bias is indicated by the funnel plot. The overall quality of the reports in general was poor.
The patients in the included studies were predominantly elderly women. Previous studies44, 45 also support this finding that osteoporosis is predominantly a condition of the elderly and significantly higher in women.
A study on cadavers about biomechanics46 demonstrated that there was no difference in the restoration of vertebral body strength, stiffness, or height in experimentally induced vertebral compression fractures between unilateral kyphoplasty and bilateral kyphoplasty. Using virtual vertebroplasty on damaged model, Liebschner47 found both unilateral and bilateral approaches to have effect on recovery of vertebral stiffness and strength after fracture; however, unilateral vertebroplasty may not be as effective as vertebroplasty in recovering vertebral body stability, i.e., the unsupported side preferentially deformed when uniaxial compressive stress boundary conditions were applied.
The most common complication reported in most studies was bone cement leakage. Previous reports have indicated high incidence of 19%–65%.48 There is no correlation between perfusion of bone cements and analgesic effect. However, with increasing injection volume, risk of leakage also increases.49 The increased stiffness of vertebral body with bone cement perfusion may be one of the reasons for adjacent vertebral fracture. Osteoporosis and bone cement leakage into the intervertebral disc space have also been considered predictive factors affecting adjacent vertebral fracture.50
Cement dosage is also an important variable in outcome. Retrospective analysis of 158 patients treated with PVP yielded result that there was no significant association between cement dosage and post surgery pain.51 Thus, it is unnecessary to achieve particular cement volume. Therefore, the outcomes we chose to analyze were mainly view of clinical patients and outcome of cement dosage was not included. Systematic review and meta-analysis of unilateral versus bilateral PKP for OVCF indicated that unilateral PKP used smaller quantity of cement than bilateral PKP.52
For this secondary document, the main limitation is that the authenticity of this study depends on original articles. Another limitation is that about half of included studies were in Chinese, which is difficult for English readers to assess.
In view of the low quality of evidence currently available, there is insufficient data to demonstrate if there are any differences between unilateral and bilateral approaches in both PVP and PKP treatment of OVCF. In clinical setting, selection of operative method may depend on patient's condition, including such factors as age, degree of osteoporosis, and fracture type.
Ethical approval
For this secondary document, formal consent is not required.
Conflicts of interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Dervis E. Oral implications of osteoporosis. Oral Surg Oral Med Oral Pathol, Oral Radiol, Endodontol. 2005;100(3):349–356. doi: 10.1016/j.tripleo.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Hallberg I., Rosenqvist A., Kartous L., Löfman O., Wahlström O., Toss G. Health-related quality of life after osteoporotic fractures. Osteoporos Int. 2004;15(10):834–841. doi: 10.1007/s00198-004-1622-5. [DOI] [PubMed] [Google Scholar]
- 3.linville Douglas A., II Vertebroplasty and kyphoplasty. South Med J. 2002;95(6):583–587. [PubMed] [Google Scholar]
- 4.Garfin S.R., Yuan H.A., Reiley M.A. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26(14):1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 5.Ma X., Xing D., Ma J., Xu W., Wang J., Chen Y. Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J. 2012;21(9):1844–1859. doi: 10.1007/s00586-012-2441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kobayashi K., Shimoyama K., Nakamura K., Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol. 2005;15(2):360–367. doi: 10.1007/s00330-004-2549-0. [DOI] [PubMed] [Google Scholar]
- 7.Yang Z., Tan J., Xu Y. Treatment of MM-associated spinal fracture with percutaneous vertebroplasty (PVP) and chemotherapy. Eur Spine J. 2012;21(5):912–919. doi: 10.1007/s00586-011-2105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harbour R., Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323(7308):334–336. doi: 10.1136/bmj.323.7308.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . 2008. Assessment of Osteoporosis at the Primary Health Care Level.http://www.who.int/chp/topics/rheumatic/en/ Available from: [Google Scholar]
- 10.Higgins JP and Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane collaboration. Available from: http://handbook.cochrane.org.
- 11.Sun G., Jin P., Hao R.S. Percutaneous kyphoplasty with double or single balloon in treatment of osteoporotic vertebral body compressive fracture:a clinical controlled study. Natl Med J China. 2008;88(3):149–152. [in Chinese] [PubMed] [Google Scholar]
- 12.Sun G., Jin P., Liu X.W. Kyphoplasty with single balloon inflation followed by cement filling for osteoporotic vertebral compression fractures. J Clin Rehabil Tissue Eng Res. 2008;12(6):1179–1183. [in Chinese] [Google Scholar]
- 13.Song B.K., Eun J.P., Oh Y.M. Clinical and radiological comparison of unipedicular versus bipedicular balloon kyphoplasty for the treatment of vertebral compression fractures. Osteoporos Int. 2009;20(10):1717–1723. doi: 10.1007/s00198-009-0872-7. [DOI] [PubMed] [Google Scholar]
- 14.Chen H.L. Traditional Chinese Medicine Academic Symposium in Guangzhou. 2011. Comparison of therapeutic effects of unilateral and bilateral bone cement plasty for thoracic and lumbar vertebral compression comparison: 2011; pp. 158–160. [in Chinese] [Google Scholar]
- 15.Wang S., Shen J., Gao Y., Hu J.J. The 2nd Academic Symposium of Institute of Orthopedics Branch Combining Chinese and Western Medicine in Guizhou Province. 2011. The effect of unilateral dilatation percutaneous kyphoplasty with double balloon for osteoporotic vertebral compression fracture; pp. 229–230. [in Chinese] [Google Scholar]
- 16.Zhao J.Q., Chen Q., Huang Z.J. A prospective study of unilateral and bilateral percutaneous vertebroplasty for vertebral compression fracture. Chin J Bone Jt Inj. 2011;26(3):229–230. [in Chinese] [Google Scholar]
- 17.Zhang B., Dai M., Tang Y. Unilateral versus bilateral kyphoplasty for osteoporotic vertebral compression fractures. In: Chen R., Sung W.P., editors. Biotechnology, Chemical and Materials Engineering, PTS 1-3. Advanced Materials Research. 2012. pp. 1064–1068. [Google Scholar]
- 18.Feng J., Zheng Q.X., Xiao S.X., Xia P. Clinical comparison of unilateral and bilateral percutaneous kyphoplasty for treating osteoporotic vertebral compression fractures. Chin J Tradit Med Traumatol Orthop. 2012;20(10):26–29. [in Chinese] [Google Scholar]
- 19.Li Q., Lu M.H., Zheng C.K. Unilateral versus bilateral percutaneous kyphoplasty for the treatment of osteoporotic compression fractures: a prospective case control study. Med J Wuhan Univ. 2012;33(4):567–570. [in Chinese] [Google Scholar]
- 20.Li R.J., Yang Q. Dalian Medical University; 2012. Percutaneous on Bipedicular Approachkyphoplasty with Double or Single Balloon in Treatment of Osteoporotic Vertebral Body Compressive Fracture : A Clinical Controlled Contrastive Study. Master thesis. [in Chinese] [Google Scholar]
- 21.Wang B., Yang Q., Wu C.M. Percutaneous kyphoplasty with double or single balloon in treatment of osteoporotic vertebral compression fracture in elderly patients: a clinical controlled study. Chin J Multiple Organ Dis Elder. 2012;11(10):761–764. [in Chinese] [Google Scholar]
- 22.Li C., He C.J. Hebei University of Chinese Medicine; 2013. PKP Holds the Single or Double Side into the Road Treatment of Osteoporptic Vertebral Compression Fracture Curative Effect Comparison. Master thesis. [in Chinese] [Google Scholar]
- 23.Liu B., Chen G.C., Deng L.P. Comparative study of unilateral and bilateral percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. China Med Pharm. 2013;(14) 185–186, 194. [in Chinese] [Google Scholar]
- 24.Li L., Wang M., Ma H.S. Comparison of unilateral and bilateral penetrating kyphoplasty for osteoporotic centrum compression fractures. Orthop J China. 2014;22(8):678–682. [in Chinese] [Google Scholar]
- 25.Song J.G., Miao Y., Cui Y.K., Yin Z.Y., Huang H.F. Research the side-compression fracture of vertebral treatment by percutaneous balloon kyphoplasty. Orthop Biomech Mater Clin Study. 2014;11(1):46–49. [in Chinese] [Google Scholar]
- 26.Su P. Clinical investigation of unilateral percutaneous kyphoplasty in the modified. Jilin Med J. 2011;32(9):1698. [in Chinese] [Google Scholar]
- 27.Qu L.Q., Yang Z.R., Yan K.Z. Comparative study of unilateral and bilateral percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. Med Inf. 2014;7(19):546–547. [in Chinese] [Google Scholar]
- 28.Huang S., Xu J., Xiang Y.C. Comparative study of unipedicular versus bipedicular percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Orthop J China. 2013;21(2):115–118. [in Chinese] [Google Scholar]
- 29.Kong J.J. Comparative study of unilateral and bilateral percutaneous vertebroplasty. Chin Foreign Med Res. 2012;(18):117. [in Chinese] [Google Scholar]
- 30.Wang W., Wang C.W., Zhu S.H. Outcomes of unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures. J Pract Orthop. 2013;19(8):690–692. [in Chinese] [Google Scholar]
- 31.Zhang C.L., Liu J.Y., Liu S.Z. Comparison of therapeutic effects of unilateral and bilateral percutaneous vertebroplasty for thoracic and lumbar vertebral compression comparison. Mod J Integr Tradit Chin West Med. 2013;22(28):3117–3118. [in Chinese] [Google Scholar]
- 32.Zhang J.X., Wang H.P. Comparison of therapeutic effects of unilateral and bilateral PVP for thoracic and lumbar vertebral compression comparison. Shandong Med J. 2009;49(43):94–95. [in Chinese] [Google Scholar]
- 33.Zhang L.G., Gu X., Zhang H.L., Zhang Q.G., Cai X.B., Tao K. Unilateral or bilateral percutaneous vertebroplasty for acute osteoporotic vertebral fracture: a prospective study. J Spinal Disord Tech. 2014 doi: 10.1097/BSD.0000000000000147. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 34.Zhang X., Guan A.H., Hou S.Z., Gu B.L., Sun Z.J. Investigation of the superiority of unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures. Med Innovation China. 2014;(19):17–19. [in Chinese] [Google Scholar]
- 35.Zeng Z.J., Chen G. Prospective study of PKP for senile osteoporotic vertebral compression fractures in acute period. China Mod Med. 2013;20(24) 17–19, 22. [in Chinese] [Google Scholar]
- 36.Chen C., Chen L., Gu Y. Kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approachment: a comparative study in early stage. Injury-Int J Care Inj. 2010;41(4):356–359. doi: 10.1016/j.injury.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 37.Chen L., Yang H., Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures a prospective study. Spine. 2011;36(7):534–540. doi: 10.1097/BRS.0b013e3181f99d70. [DOI] [PubMed] [Google Scholar]
- 38.Gu X.H., Zhang Z., Wu J., Lv J., Wu X.Y. Contrast study between unilateral and bilateral percutaneous balloon kyphoplasty for osteoporotic thoracolumbar compression fractures. Chin J Surg Integr Tradit West Med. 2009;15(3):246–249. [in Chinese] [Google Scholar]
- 39.Li G.Z., Wang Q., Li S., Kang J.P., Wang G.J. Clinical comparison study between unilateral and bilateral PKP for osteoporotic thoracolumbar compression fractures. Orthop Biomech Mater Clin Study. 2012;09(3) 17–18, 21. [in Chinese] [Google Scholar]
- 40.Mao J.G., Xie M., Liu M.Q., Xi Z.R. The effect of unilateral and bilateral percutaneous kyphoplasty for treating osteoporotic vertebral compression fractures. Yiyao Qianyan. 2013;(23):20–21. [in Chinese] [Google Scholar]
- 41.Zhang Q.G., Zhu Y.C., He S.S., Cai Z.D. Percutaneous balloon byphoplasty for treatment of unsymmetrical osteoporotic vertebral compression fractures. J Spinal Surg. 2012;10(2):79–82. [in Chinese] [Google Scholar]
- 42.Zhou M.W., Li S.H., Liu H.P., Wang C.X., Liang X.Y., Sun F.Q. Effect analysis of unilateral and bilateral percutaneous balloon kyphoplasty for aged patients with thoracolumbar vertebral compression fractures. Chin J Osteoporos. 2013;19(5) 488–490, 508. [in Chinese] [Google Scholar]
- 43.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Han Y.J., Tie X.J., Yilihamu T. Meta-analysis on the prevalence rate of osteoporosis in the middle-aged and elderly in China. J Clin Rehabil Tissue Eng Res. 2014;18(7):1129–1134. [In Chinese] [Google Scholar]
- 45.Looker A., Borrud L., Dawson-Hughes B. Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005–2008. NCHS Data Brief. 2012;98:1–8. [PubMed] [Google Scholar]
- 46.Steinmann J., Tingey C.T., Cruz G., Dai Q. Biomechanical comparison of unipedicular versus bipedicular kyphoplasty. Spine. 2005;30(2):201–205. doi: 10.1097/01.brs.0000150831.46856.87. [DOI] [PubMed] [Google Scholar]
- 47.Liebschner M.A., Rosenberg W.S., Keaveny T.M. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine. 2001;26(14):1547–1554. doi: 10.1097/00007632-200107150-00009. [DOI] [PubMed] [Google Scholar]
- 48.Phillips F.M. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine. 2003;28(15S):S45–S53. doi: 10.1097/01.BRS.0000076898.37566.32. [DOI] [PubMed] [Google Scholar]
- 49.Ryu K.S., Park C.K., Kim M.C., Kang J.K. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg Spine. 2002;96(1):56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 50.Rho Y.J., Choe W.J., Chun Y.I. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J. 2012;21(5):905–911. doi: 10.1007/s00586-011-2099-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaufmann T.J., Trout A.T., Kallmes D.F. The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2006;27(9):1933–1937. [PMC free article] [PubMed] [Google Scholar]
- 52.Feng H., Huang P., Zhang X., Zheng G., Wang Y. Unilateral versus bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis of RCTs. J Orthop Res. 2015;33(11):1713–1723. doi: 10.1002/jor.22957. [DOI] [PubMed] [Google Scholar]