Abstract
Objective
The aim of this retrospective study was to find out whether a cut off value existed for elbow flexion and extension after open surgical release of elbow contracture that would correlate with subjective patient satisfaction.
Methods
The study enrolled 77 patients (53 males and 24 females with a mean age of 35.1 (18–77) years at the time of operation) with elbow contracture who attended regular follow-up appointments for more than 12 months. The mean follow up period was 44.2 months (12–186). The preoperative and postoperative modified MAYO elbow scores, objective parameters of increase in both flexion and extension end point measurements and improvement in total ROM were compared in order to determine the cut off degree of ROM in both flexion and extension that significantly correlated with patient satisfaction.
Results
Of the 77 participating patients, 26 patients had an extrinsic (33.8%) and 51 patients had an intrinsic elbow contracture (66.2%). Surgeries performed involved 40 cases of lateral release and 37 cases of both lateral and medial (progressive) release. The median preoperative total flexion-extension arch (ROM) was 45° (20°–65°). The median postoperative total flexion-extension arch (ROM) was 110° (97.5°–125°). The modified MAYO elbow score improved from 60 to 85 points postoperatively. The postoperative flexion cut off value was 115° for an excellent or good postoperative modified MAYO elbow score.
Conclusion
Post-operative flexion cut off value was 115° and had a positive effect on the postoperative patient satisfaction. The cut off value for postoperative extension was 20° but it was not a significant variable on patient satisfaction as was the total increase in ROM.
Level of significance
Level IV Therapeutic Study.
Keywords: Contracture release, Elbow contracture, Elbow flexion
Elbow joint is prone to stiffness after trauma and surgery. It has a small intracapsular volume, predisposing the joint to stiffness with effusion, hemarthrosis, scarring, and thickening of the capsule. Results of conservative treatment of significant elbow contractures are generally unsatisfactory.1, 2, 3, 4, 5, 6 Surgical treatment is technically demanding, as a thorough understanding of the pathoanatomy and formation of an appropriate surgical plan are necessary.6, 7, 8, 9, 10, 11, 12 The goal of open surgical treatment is to completely resect all pathological tissues and protect the collateral ligaments, if possible. Several articles have reported steady improvement in range of motion (ROM) of the elbow joint after operative treatment.5, 8, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 Yet correlation between objective parameters of increase in flexion and extension arch and improvement in total ROM and subjective patient appreciation has not been well established.25, 26, 27, 28, 29, 30, 31, 32, 33
The aim of this retrospective study was to determine whether there was a cut-off point of ROM in both flexion and extension that produced significant correlation with subjective patient satisfaction. Other variables that might have an effect on the clinical results of the procedure were also analyzed.
Patients and methods
Over the 16-year period between 1997 and 2013, 2 surgeons performed open surgical release in adult patients with an established stiff elbow at this hospital. The following criteria were used to define established stiff elbow:
-
1
Loss of extension of greater than 30° or flexion of less than 120°,
-
2
No skeletal injury other than to elbow joint in the same extremity,
-
3
A minimum interval of 3 months between the trauma or most recent surgery and the proposed surgery, and
-
4
Failure of a rehabilitation program or inability to participate in program within 3 months after the trauma or most recent surgery.
Patients with an established stiff elbow were excluded from the study on the basis of the following criteria:
-
1
Active infection,
-
2
Associated nonunion of the humerus, ulna, or radius that necessitated surgical treatment,
-
3
Patients with an associated central nervous system injury that interfered with the rehabilitation of the involved extremity,
-
4
Patients with open physis, or
-
5
Advanced cartilage injury that required some form of interposition arthroplasty in addition to elbow release.
Peripheral nerve dysfunction and presence of an internal fixation device were not considered exclusion criteria. Kocaeli University ethics committee approval was granted for retrospective review of medical documents and follow-up visits of patients, including physical examination and obtaining radiographs. Total of 92 patients who met the enrollment criteria of the study were listed, and 77 of the 92 patients who had regular follow-up period of more than 12 months and who agreed to participate were included in the study. The following data were obtained from medical charts at most recent follow-up:
-
1
Preoperative modified Mayo Elbow Performance Scores,
-
2
Postoperative modified Mayo elbow scores at latest follow-up visit,
-
3
Preoperative and postoperative flexion and extension measurements,
-
4
Postoperative total increase in joint ROM.
ROM was measured with hand-held goniometer. Subjective parameter of patient satisfaction was evaluated on the basis of postoperative modified Mayo elbow score. Objective parameters, such as increase in flexion and extension arch and improvement in total ROM, were compared in order to determine cut-off value of ROM in both flexion and extension that correlated significantly with patient satisfaction.
Other factors that might have had an effect on postoperative patient satisfaction, such as type of contracture (intrinsic or extrinsic), time interval between trauma and proposed surgery, type of surgical plan (lateral exposure, medial exposure, or combined surgery) were also assessed.
Surgical technique
Of the 77 patients, 40 had lateral release and 37 had lateral and medial (progressive) release. This surgical concept is one of the subjective criteria of the study, since progressing to medial release depended on the surgeon's dissatisfaction with peroperative result after lateral release.
All patients were operated on in supine position. Under general anesthesia, the involved upper extremity was prepared and tourniquet was inflated to 250 mmHg after exsanguination. Incision was made over the lateral epicondyle and central portion of the radial head. Anterior and posterior skin flaps were raised to protect the lateral antebrachial cutaneous nerve. Next, incision was made beginning 3–4 cm proximally to the epicondyle and extending distally to just beyond the radial head. The fibers of the extensor carpi radialis longus muscle were identified and were dissected off the anterior capsule with an elevator to identify the plane of the capsule. The tendinous origin of the common extensor tendon was then sharply elevated to complete the exposure of the anterior capsule when the radiocapitellar joint and the anterior aspect of the elbow joint could be seen. The interval between the anterior capsule and the brachialis muscle was then identified and developed with blunt dissection. Deep retractor was then positioned to protect the brachialis muscle while the anterior capsule was excised.
If access to the posterior elbow joint was required, care was taken to protect the origin of the lateral collateral ligament (LCL) from the epicondyle (Fig. 1). Posterior capsulectomy could then be performed and the olecranon and olecranon fossa inspected.
Fig. 1.
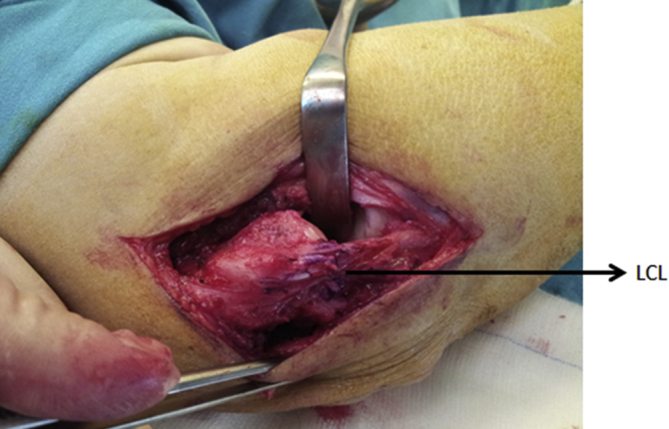
Lateral surgical exposure. LCL: Lateral collateral ligament.
When full ROM was restored with lateral approach, tourniquet was deflated and bleeding was controlled. After inserting suction drain, the anterior and posterior extensor origins were reattached.
Failure to restore nearly full motion with resection from the lateral approach was an indication for additional medial incision. This was also designed over the epicondyle. Care had to be taken to protect the medial ante brachial cutaneous nerve. Ulnar nerve was dissected distally, through the cubital tunnel, and then mobilized with its blood supply. Next, the area anterior to the medial inter muscular septum was exposed. The fascial confluence over the interval between the brachialis and flexor-pronator muscle masses was incised and blunt dissection was performed to expose the median nerve and brachial vessels. These did not need to be dissected, but merely visualized, so that safe resection could be performed. The anterior portion of the flexor–pronator muscle mass was then released, exposing the anterior capsule for resection. Care was taken to protect the anterior bundle of the medial collateral ligament (MCL). Posteriorly, the floor of the cubital tunnel was the posterior MCL and capsule and could now be resected, along with the posteromedial capsule (Fig. 2). Capsulectomy could at this stage be completed and motion assessed. If full motion had been restored, closure was performed. If not, the remaining possible impediments were either the muscles or the anterior MCL. Inspection and palpation of the muscles during motion permitted this distinction to be made. If the restriction was due to the MCL, careful dissection of the remaining portion of the flexor-pronator muscles overlying the MCL was performed. If the ligament was intact and simply adherent to the medial trochlea, lysis could be performed. We tried not to sacrifice the collateral ligaments of any patient in order to obtain more ROM. Peroperative result was accepted as it was in order to avoid use of an external fixation device.6, 34
Fig. 2.
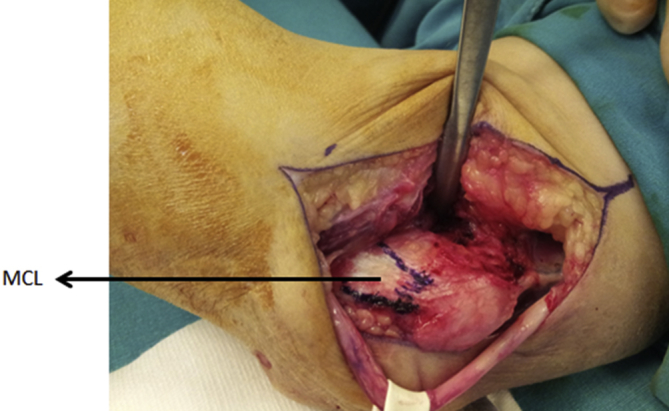
Medial surgical exposure. MCL: Medial collateral ligament.
Postsurgical program
Cold application, elevation, and pain management were started within first 24 h after surgery. Physical therapy for 3 weeks was initiated after 24 h. Passive exercises were performed in first week and assisted active therapy was implemented for next 2 weeks. Physical therapy was extended for additional 3 weeks for patients who could not achieve 120° flexion. Physical therapy, emphasizing long flexion-extension cycle time and gentle stretching to achieve full motion, was utilized for all patients. Static splinting in flexion or extension was employed as needed.6
Statistical analysis
Statistical analyses of the data obtained from 77 patients were performed using SPSS software (IBM SPSS Statistics for Windows, Version 20.0; IBM Corp., Armonk, NY, USA). Nonparametric data of ROM measurements and modified Mayo scores were compared between groups using Mann–Whitney U test. Pearson correlation test was used to analyze whether significant correlation existed between modified Mayo scores and ROM measurements. Receiver operating characteristic (ROC) curve was used to analyze cut-off values of flexion and extension degree using MedCalc program, version 13.0.6.0 (MedCalc Software, Ostend, Belgium). Statistical significance was defined as p < 0.05.
Results
Of total included, 53 patients were male and 24 were female, with average age of 35.1 years (range: 18–77 years) at the time of operation. Among the 77 patients assessed, 26 patients (33.8%) had extrinsic and 51 patients (66.2%) had intrinsic elbow contracture. Mean follow-up period was 44.2 months (range: 12–186 months). In all, 61 of the patients had been operated on at least once before the study; 43 patients had history of 1 operation, 16 patients had 2, and 2 patients had 3 previous operations. Details of patient demographics are provided in Table 1, Table 2.
Table 1.
Demographic data of the patients.
| Number of patients | 77 |
| Male:Female | 53:24 |
| Average age | 35.1 years (range 18–77) |
| Average follow up | 44.2 months (range 12–186) |
| Average time to surgery (median value) | 14 months (8.5–25.5) |
| Extrinsic:Intrinsic | 26:51 |
Table 2.
Etiology of the elbow contracture.
| Posttraumatic | Causes other than trauma | |
|---|---|---|
| Intrinsic | 43 | 8 |
| Extrinsic | 21 | 5 |
Major and minor postoperative complications were observed in 30 patients (39%). These complications can be seen in Table 3. There was no correlation between complication prevalence and type of release (lateral or combined lateral and medial).
Table 3.
Complications of the surgery.
| Minor complications | |
| Superficial infection | 4 (5.2%) |
| Transient cold intolerance | 13 (16.8%) |
| Transient ulnar nerve paresthesia | 10 (13%) |
| Major complications | |
| Re-operations for recurrent contracture | 12 (15.6%) |
| Heterotrophic ossification | 1 (1.3%) |
| Total complications (number of patients) | 30 (39%) |
There was no correlation between etiology of the contracture (intrinsic versus extrinsic) and clinical results of modified Mayo elbow scores and total improvement in postoperative ROM (p > 0.05).
Median preoperative ROM was 45° (range: 20°–65°). Median postoperative ROM was 110° (range: 97.5°–125°). Median values of these measurements are provided in Table 4.
Table 4.
Pre-postoperative ROM measurements (median value).
| Preoperative (°) | Postoperative (°) | |
|---|---|---|
| Flexion degree | 90 (70–105) | 125 (110–130) |
| Extension degree | 40 (30–60) | 10 (0–20) |
| Flexion-extension arch degree | 45 (20–65) | 110 (97.5–125) |
| Pronation degree | 90 (75–90) | 90 (80–90) |
| Supination degree | 80 (60–90) | 90 (80–90) |
| MAYO score | 60 (50–70) | 85 (80–95) |
Modified Mayo elbow score improved from 60 to 85 postoperatively. According to ROC curve analyses, postoperative flexion cut-off value was 115° (p < 0.001) and preoperative flexion cut-off value was 55° (p = 0.0008) for excellent or good postoperative modified Mayo elbow score. Cut-off value for postoperative extension arch was 20° and not statistically significant (p = 0.31).
Preoperative flexion degree of the elbow joint had a statistically significant effect on postoperative ROM (p < 0.001) and postoperative modified Mayo elbow score (p = 0.014), although preoperative extension degree had no such effect (p = 0.919). Also, preoperative flexion and extension measures positively correlated with postoperative flexion and extension measures (p < 0.001 and p = 0.014, respectively), although increase in total ROM by itself had no effect on postoperative modified Mayo elbow score (p = 0.052).
Time interval between establishment of contracture and index operation correlated negatively with postoperative increase in ROM (p = 0.014).
Other variables that had an effect on postoperative modified Mayo elbow score were preoperative modified Mayo elbow score (p < 0.001), postoperative extension (p = 0.006), preoperative total ROM (p = 0.03), and postoperative total ROM (p < 0.001).
Postoperative ROM and postoperative extension were significantly better in lateral release group, compared with lateral and medial combined release group (p = 0.011 and p = 0.011, respectively). This significance did not affect postoperative flexion degree, or consequently, the modified Mayo elbow score (p = 0.065 and p = 0.546, respectively).
Discussion
Contracture of the elbow is a common problem and can be associated with significant morbidity.35 It may develop as result of traumatic or atraumatic etiology. The goals in treating stiff elbow are to establish a pain-free, functional, and stable elbow joint.7 Although non-operative treatment may be considered upon initial presentation, operative treatment is appropriate for those patients who have failed to achieve adequate pain relief or functional range of motion after initial conservative management. The decision to operate is based on elbow function, patient factors, and surgeon preference.7
Stiff elbow has been defined as one with loss of extension of greater than 30° and flexion of less than 120°. Morrey defined functional arc of elbow motion during activities of daily living to be 100° for both flexion-extension (30°–130°) and pronation-supination (50° in either direction).7, 23, 25 Sojbjerg indicated that elbow flexion is more important than extension in order to perform daily activities.23 In our series, cut-off degree of flexion of 115° had significant correlation with subjective patient satisfaction. We think that, elbow flexion combined with normal shoulder and wrist motion might explain the 15° difference in flexion degree from 130° Morrey reported.
Lindenhovius et al found that health status and disability scores improve after open elbow contracture release, but the improvements do not correlate with improvement in elbow motion and that pain was a strong predictor of final general health status and arm-specific disability.26 Gosling et al found a high correlation between Disabilities of the Arm, Shoulder and Hand score and physical function part of the 36-Item Short Form Health Survey, and they thought that ROM, as a single parameter, did not sufficiently assess the outcome of arthrolysis of the elbow.32 In contrast to Lindenhovius and Gosling, we found that the end point of flexion degree must be at least 115° postoperatively for patient satisfaction and that increasing postoperative flexion-extension arc (ROM) or decreasing postoperative extension degree with surgical release had effect on postoperative Mayo score.
Many elbow score rating systems have been described. There is significant lack of agreement between different elbow-scoring systems when they are used to determine categorical rankings for the same group of patients. Each elbow rating system evaluates the joint using specific variables, including both objective and subjective parameters. Although they are used in more than one scoring system, interpretation and comparison of these parameters is difficult, as different weight is given to the same parameter in each of the rating systems. Pain is a subjective parameter that has a strong influence on every elbow score rating system. As a result, both the physician-rated and the patient-rated degree of elbow function are heavily influenced by subjectivity. Therefore, objective improvements in elbow function may be underestimated by nearly all elbow score rating systems. Some authors suggest that subjective factors such as pain should be evaluated separately from objective degree of elbow function. The Mayo elbow score rating system has a clear format.36 The associated costs are low because only a goniometer is necessary. Little training is necessary, and the system is appropriate for use in the clinic.36 Neither strength nor deformity is included in the content of the scale, and motion is assessed only in terms of flexion and extension.36 Function and motion are weighted less heavily than pain. The Mayo elbow scoring was the most appropriate elbow scoring system for our purpose examining patient-perceived assessment of the results.
Many types of operation for contracture of elbow have been performed, including debridement arthroplasty, arthroscopic release, resection arthroplasty, interposition arthroplasty, and total elbow replacement.37 Various approaches can be utilized to release the contracted elbow. The anterior approach was described by Urbaniak et al in 1985, the medial approach was described by Hotchkiss in 1997, and the lateral approach (column procedure) was described by Morrey in 1990. Medial approach was favored in cases with ulnar nerve dysfunction or the presence of extensive medial heterotopic ossification.35 The choice of surgical approach should be dictated by pathoanatomy and informed by wound healing considerations.6 In our study, significantly better results were seen in lateral release cases. The combined exposure was usually performed on more complicated cases, and this might have affected our results.
Column procedure was first suggested for extrinsic contracture of the elbow. Subsequently, this procedure was used for both extrinsic and intrinsic types of contracture.6 In this study, MCL and LCL were protected after resection of anterior and posterior capsule during operation on intrinsic contracture. After this stage, bone resection (olecranon, olecranon fossa, coronoid, and osteophyte of anterior wall of distal humerus) was performed according to pathology of intrinsic causes (Fig. 3a and b). ROM of the elbow was controlled under fluoroscopy. In patients with flexion limitation, MCL was resected with preservation of anterior bundle. LCL did not cause ROM limitation in any of the patients. We used dynamic splint in patients with partial MCL resection. External fixation was not indicated in any patient.
Fig. 3.

(a) Preoperative X-ray of 28-year-old patient with intrinsic contracture. (b) Postoperative X-ray 6 months after surgery. It is imperative to completely remove pathological bone formation at olecranon fossa and spurs at the tip of olecranon.
This study may be limited by its retrospective design and the diversity of the patients. In addition, we did not evaluate the influence of follow-up time on the range of motion. Another limitation is the fact that pain was the main criterion in the scoring system.
In conclusion, open surgical release of stiff elbow is prone to complications, independent of the type of surgical exposure. Delay in surgical treatment has adverse effects on clinical results. Subjective clinical data on patient satisfaction were not influenced by the type of stiffness. Outcome indices improved significantly despite the fact that surgical treatment was not generally able to restore full ROM. Post-operative flexion cut-off value was 115° and had a strong effect on postoperative patient satisfaction. The cut-off degree for postoperative extension was 20°, but it was not a variable with significant effect on patient satisfaction. The majority of postoperative extension measurements of the study were good; this is likely the reason we did not find a significant cut-off value for extension. Increase in total ROM was not a variable with significant effect on patient satisfaction.
Conflicts of interest
The authors report no conflict of interest to disclose.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Duke J.B., Tessler R.H., Dell P.C. Manipulation of the stiff elbow with patient under anesthesia. J Hand Surg Am. 1991;16(1):19–24. doi: 10.1016/s0363-5023(10)80005-x. [DOI] [PubMed] [Google Scholar]
- 2.Jupiter J.B., O'Driscoll S.W., Cohen M.S. The assessment and management of the stiff elbow. Instr Course Lect. 2003;52:93–111. [PubMed] [Google Scholar]
- 3.Mohan K. Myositis ossificans traumatica of the elbow. Int Surg. 1972;57(6):475–478. [PubMed] [Google Scholar]
- 4.Page C., Backus S.I., Lenhoff M.W. Electromyographic activity in stiff and normal elbows during elbow flexion and extension. J Hand Ther. 2003;16(1):5–11. doi: 10.1016/s0894-1130(03)80018-2. [DOI] [PubMed] [Google Scholar]
- 5.Vardakas D.G., Varitimidis S.E., Goebel F., Vogt M.T., Sotereanos D.G. Evaluating and treating the stiff elbow. Hand Clin. 2002;18(1):77–85. doi: 10.1016/s0749-0712(02)00005-7. [DOI] [PubMed] [Google Scholar]
- 6.Hausman M., Gundes H. Treatment of elbow contractures. Curr Opin Orthop. 2000;11:310–318. [Google Scholar]
- 7.Nandi S., Masckhe S., Evans P.J., Lawton J.N. The stiff elbow. Hand (N Y) 2009;4(4):368–379. doi: 10.1007/s11552-009-9181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rhee Y.G., Cho N.S., Lim C.T., Yi J.W. Debridement arthroplasty for post-traumatic stiff elbow: intraoperative factors affecting the clinical results of surgical treatment. Clin Orthop Surg. 2009;1(1):27–33. doi: 10.4055/cios.2009.1.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Husband J.B., Hastings H., 2nd The lateral approach for operative release of posttraumatic contracture of the elbow. J Bone Jt Surg Am. 1990;72(9):1353–1358. [PubMed] [Google Scholar]
- 10.Mansat P., Morrey B.F. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Jt Surg Am. 1998;80(11):1603–1615. [PubMed] [Google Scholar]
- 11.Johannson O. Capsular and ligament injuries of the elbow joint. A clinical and arthrographic study. Acta Scand. 1962;287(suppl):50–65. [PubMed] [Google Scholar]
- 12.Frankle M.A., Koval K.J., Sanders R.W., Zuckerman J.D. Radial head fractures associated with elbow dislocations treated by immediate stabilization and early motion. J Shoulder Elb Surg. 1999;8(4):355–360. doi: 10.1016/s1058-2746(99)90160-x. [DOI] [PubMed] [Google Scholar]
- 13.Gates H.S., 3rd, Sullivan F.L., Urbaniak J.R. Anterior capsulotomy and continuous passive motion in the treatment of post-traumatic flexion contracture of the elbow. A prospective study. J Bone Jt Surg Am. 1992;74(8):1229–1234. [PubMed] [Google Scholar]
- 14.Roberts J.B., Pankratz D.G. The surgical treatment of heterotopic ossification at the elbow following long-term coma. J Bone Jt Surg. 1979;61(5):760–763. [PubMed] [Google Scholar]
- 15.Morrey B.F. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Jt Surg Am. 1990;72(4):601–618. [PubMed] [Google Scholar]
- 16.Morrey B.F. Posttraumatic stiffness: distraction arthroplasty. Orthopedics. 1992;15(7):863–869. doi: 10.3928/0147-7447-19920701-12. [DOI] [PubMed] [Google Scholar]
- 17.Phillips B.B., Strasburger S. Arthroscopic treatment of arthrofibrosis of the elbow joint. Arthroscopy. 1998;14(1):38–44. doi: 10.1016/s0749-8063(98)70118-5. [DOI] [PubMed] [Google Scholar]
- 18.Cheng S.L., Morrey B.F. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J Bone Jt Surg Br. 2000;82(2):233–238. [PubMed] [Google Scholar]
- 19.Evans P.J. Elbow interposition/distraction arthroplasty. In: Yamaguchi K., King G.J.W., McKee M.D., O'Driscoll S.W.M., editors. Advanced Reconstruction Elbow. 1st ed. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2007. p. 435. [Google Scholar]
- 20.Froimson A.I., Morrey B.F. Interposition arthroplasty of the elbow. In: Morrey B.F., editor. Master Techniques in Orthopaedic Surgery: The Elbow. 2nd ed. Lippincott Williams & Wilkins; Philadelphia: 2002. p. 391. [Google Scholar]
- 21.Morrey B.F. Distraction arthroplasty. Clinical applications. Clin Orthop Relat Res. 1993;293:46–54. [PubMed] [Google Scholar]
- 22.Pignatti G., Ferrari D., Tigani D. The treatment of post-traumatic stiffness of the elbow. Chir Organi Mov. 2000;85(4):381–387. [PubMed] [Google Scholar]
- 23.Sojbjerg J.O. The stiff elbow. Acta Orthop Scand. 1996;67(6):626–631. doi: 10.3109/17453679608997771. [DOI] [PubMed] [Google Scholar]
- 24.Tan V., Daluiski A., Capo J., Hotchkiss R. Hinged elbow external fixators: indications and uses. J Am Acad Orthop Surg. 2005;13(8):503–514. doi: 10.5435/00124635-200512000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Marti R.K., Gino M., Kerkhoffs M.J., Maas M., Blankevoort L. Progressive surgical release of a posttraumatic stiff elbow. Technique and outcome after 2–18 years in 46 patients. Acta Orthop Scand. 2002;73(2):144–150. doi: 10.1080/000164702753671713. [DOI] [PubMed] [Google Scholar]
- 26.Lindenhovius A.L., Doomberg J.N., Ring D., Jupiter J.B. Health status after open elbow contracture release. J Bone Jt Surg Am. 2010;92(12):2187–2195. doi: 10.2106/JBJS.H.01594. [DOI] [PubMed] [Google Scholar]
- 27.Ring D., Adey L., Zurakowski D., Jupiter J.B. Elbow capsulectomy for posttraumatic elbow stiffness. J Hand Surg Am. 2006;31(8):1264–1271. doi: 10.1016/j.jhsa.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 28.Meredith P., Strong J., Feeney J.A. Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain. 2006;123(1–2):146–154. doi: 10.1016/j.pain.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 29.Gonzales V.A., Martelli M.F., Baker J.M. Psychological assessment of persons with chronic pain. NeuroRehabilitation. 2000;14(2):69–83. [PubMed] [Google Scholar]
- 30.Ring D., Kadzielski J., Fabian L., Zurakowski D., Malhotra L.R., Jupiter J.B. Selfreported upper extremity health status correlates with depression. J Bone Jt Surg Am. 2006;88(9):1983–1988. doi: 10.2106/JBJS.E.00932. [DOI] [PubMed] [Google Scholar]
- 31.Ring D., Kadzielski J., Malhotra L., Lee S.G., Jupiter J.B. Psychological factors associated with idiopathic arm pain. J Bone Jt Surg Am. 2005;87(2):374–380. doi: 10.2106/JBJS.D.01907. [DOI] [PubMed] [Google Scholar]
- 32.Gosling T., Blauth M., Lange T., Richter M., Bastian L., Krettek C. Outcome assessment after arthrolysis of the elbow. Arch Orthop Trauma Surg. 2004;124(4):232–236. doi: 10.1007/s00402-003-0524-x. [DOI] [PubMed] [Google Scholar]
- 33.Liu S., Fan C.Y., Ruan H.J., Li F.F., Tian J. Combination of arthrolysis by lateral and medial approaches and hinged external fixation in the treatment of stiff elbow. J Trauma. 2011;70(2):373–376. doi: 10.1097/TA.0b013e3181e4f5e3. [DOI] [PubMed] [Google Scholar]
- 34.Hausman M., Gundes H. Atlas of Hand Clinics: Contractures and Splinting. W.B Saunders Company; Philadelphia: 2001. Surgical treatment of elbow contractures; pp. 1–20. 6(1) [Google Scholar]
- 35.Keschner M.T., Paksima N. The stiff elbow. Bull NYU Hosp Jt Dis. 2007;65(1):24–28. [PubMed] [Google Scholar]
- 36.Turchin D.C., Beaton D.E., Richards R.R. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. J Bone Jt Surg Am. 1998;80:154–162. doi: 10.2106/00004623-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Oka Y. Debridement arthroplasty for osteoarthrosis of the elbow, 50 patients followed mean 5 years. Acta Orthop Scand. 2000;71(2):185–190. doi: 10.1080/000164700317413175. [DOI] [PubMed] [Google Scholar]


