Abstract
Objective
The aim of this study was to review the radiological alignment outcomes of patient Specific (PS) cutting blocks and Standard Instrumentation in Primary Total Knee Arthroplasty.
Methods
We hypothesized that the use of PS techniques would significantly improve sagittal, coronal and rotational alignment of the prosthesis on short term. We performed a systematic review and a meta-analysis including all the randomised controlled trials (RCT) using PS and standard (ST) total knee arthroplasty to date.
Results
A total of 538 PS TKA and 549 ST TKA were included in the study. Statistical analysis of the outliers for femoral component sagittal, coronal and rotational positioning, tibial component sagittal and coronal positioning and the overall mechanical axis were assessed. We found that there was no significant benefit from using PS instrumentation in primary knee arthroplasty to aid in the positioning of either the tibial or femoral components. Furthermore sagittal plane tibial component positioning was worse in the PS than the traditional ST group.
Conclusion
Our results suggest that at present PS instrumentation is not superior to ST instrumentation in primary total knee arthroplasty.
Level of evidence
Level 1, Systematic review of therapeutic studies.
Keywords: Alignment, Meta-analysis, Patient-specific, Total knee arthroplasty
Introduction
Component alignment is an important aspect of arthroplasty surgery. The correct placement of the implants improves the longevity of the joint.1 Malalignment of more than 3° in coronal plane after total knee arthroplasty has been found to be associated with increased revision rates and inferior functional scores.2, 3 Patient specific instrumentation is relatively new technique used in total knee arthroplasty. Proponents of this technique suggest that there is lower risk of implant malpositioning and suggest that it a more reliable for accurate component positioning than the standard anatomical referencing techniques. They also suggest this associated with no increase in operative complications.4, 5, 6
In our study, we hypothesized that there are significant benefits regarding the short term radiological alignment of the both femoral and tibial components using the patient specific instrumentation as opposed to the standard instrumentation. The hypothesis was tested using a meta-analysis of randomised controlled trials comparing the above two techniques for primary TKA.
Materials and methods
A systematic review and meta-analysis was conducted according to guidelines described in the Cochrane handbook for systematic reviews of interventions and PRISMA statement.7, 8
Study selection criteria
Types of studies
Only the randomised controlled trials were included in this study.
Types of participants
The participants were adult patients who underwent primary TKA using either a PS or ST instrumentation regardless of the type prosthesis.
Types of interventions
The interventions were PS and ST instrumentations.
Types of outcome measures
The outcome measures were number of mechanical axis, tibial and femoral component outliers in post-operative radiographs or CT scans. Outliers defined as more than 3° deviation from neutral alignment on the sagittal and coronal planes. Furthermore; rotational outliers of the femoral components were also used as an outcome measure.
Exclusion criteria
Studies without randomisation, quazi-randomised studies, animal studies, studies where the above mentioned outcomes were not evaluated and where minimally invasive techniques are utilised are excluded to attempt on reducing the heterogeneity between studies and improve the quality of the meta-analysis.
Search methods for identification of studies
Finding existing systematic reviews and meta-analyses
The following databases were searched in March 2016 to establish whether there has been any previous systematic reviews or meta-analyses comparing PS and ST instrumentation in TKA: Cochrane Database of Systematic Reviews (CDRS), Database of Abstracts of Reviews of Effects (DARE), and Medline (1950 to March 2016).
Finding published and unpublished primary studies
The search terms were used patient specific* and knee replacement, patient specific* and knee arthroplasty, custom fit* and knee arthroplasty, custom fit* and knee replacement, customised* and knee, customized and knee. A MEDLINE search was then refined to find clinical trials and randomised controlled trials (RCTs) in adult humans. The search was extended to other databases, namely EMBASE, the Cochrane Controlled Trials Register, AMED and CINAHL instrumentation and total knee replacement published in any language from 1966 to March 2016. The bibliographies of retrieved trials and other relevant publications were examined for additional articles. The following websites were searched to identify unpublished and ongoing studies: Current Controlled Trials (www.controlled-trials.com); Centre Watch (www.centerwatch.com); Trials Central (www.trialscentral.org); System for Information on Grey Literature in Europe (www.opengrey.eu); The UK National Research Register (www.nihr.ac.uk/Pages/NRRArchive.aspx).
Data collection and analysis
Selection of the studies
Two authors (IA, and AS) applied the search strategy independently and all relevant study abstracts were hand searched by them after which potentially suitable studies were reviewed in full paper format by each of the authors independently. Disagreement was discussed and resolved with the other authors.
Assessment of methodological quality of included studies
The review authors used a modification of the generic evaluation tool used by the Cochrane Bone, Joint and Muscle Trauma Group (Table 1).9 Two authors (MB and RC) assessed the methodological quality of each study. Disagreement was resolved by discussion with the senior authors. Although the total quality assessment scores (QAS) was reported for each study, it was not used to weight the studies in the meta-analysis.
Table 1.
Quality assessment items and possible scores.
| A. Was the assigned treatment adequately concealed prior to allocation? 2 = method did not allow disclosure of assignment 1 = small but possible chance of disclosure of assignment or unclear 0 = quasi-randomised or open list/tables B. Were the outcomes of participants who withdrew described and included in the analysis (intention to treat)? 2 = withdrawals well described and accounted for in analysis 1 = withdrawals described and analysis not possible 0 = no mention, inadequate mention, or obvious differences and no adjustment C. Were the outcome assessors blinded to treatment status? 2 = effective action taken to blind assessors 1 = small or moderate chance of unblinding of assessors 0 = not mentioned or not possible D. Were the treatment and control group comparable at entry? (Likely confounders may be age, partial or total rupture, activity level, acute or chronic injury) 2 = good comparability of groups, or confounding adjusted for in analysis 1 = confounding small; mentioned but not adjusted for 0 = large potential for confounding, or not discussed E. Were the participants blind to assignment status after allocation? 2 = effective action taken to blind participants 1 = small or moderate chance of unblinding of participants 0 = not possible, or not mentioned (unless double-blind), or possible but not done F. Were the treatment providers blind to assignment status? 2 = effective action taken to blind treatment providers 1 = small or moderate chance of unblinding of treatment providers 0 = not possible, or not mentioned (unless double-blind), or possible but not done G. Were care programmes, other than the trial options, identical? 2 = care programmes clearly identical 1 = clear but trivial differences 0 = not mentioned or clear and important differences in care programmes H. Were the inclusion and exclusion criteria clearly defined? 2 = clearly defined 1 = inadequately defined 0 = not defined I. Were the interventions clearly defined? 2 = clearly defined interventions are applied with a standardised protocol 1 = clearly defined interventions are applied but the application protocol is not standardised 0 = intervention and/or application protocol are poorly or not defined J. Were the outcome measures used clearly defined? (by outcome) 2 = clearly defined 1 = inadequately defined 0 = not defined K. Were diagnostic tests used in outcome assessment clinically useful? (by outcome) 2 = optimal 1 = adequate 0 = not defined, not adequate L. Was the surveillance active, and of clinically appropriate duration? 2 = active surveillance and appropriate duration 1 = active surveillance, but inadequate duration 0 = surveillance not active or not defined |
Data extraction and management
A data extraction form was designed and agreed by the authors. Initially, two authors (MB and RC) extracted the data independently which was later on reviewed jointly to produce agreed accurate data.
Statistical analysis
Meta-analysis, performed by Review Manager [Computer program] (Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.), was used to combine the relevant estimates of the effect of interest from the selected studies to provide an overall estimate of the effect. Missing standard deviations were calculated using the range of values given as suggested by Hozo et al10 Dichotomous data for each arm in a particular study were expressed as proportions or risks and the treatment effect as risk ratios. For dichotomous data, the Mantel–Haenszel method was used to combine the estimates, whereas for continuous data the inverse variance method was utilised. Statistical heterogeneity was assessed using the value of I2 and the result of the chi-squared test. A P value of <0.1 and an I2 value greater than 50% were considered suggestive of statistical heterogeneity, prompting random effects modelling estimate. Otherwise, a fixed-effect approach was used. On the other hand, a non-significant chi-squared test result only suggested that there is no evidence of heterogeneity. It did not imply that there was necessarily homogeneity as there may have been insufficient power to be able to detect heterogeneity.
Results
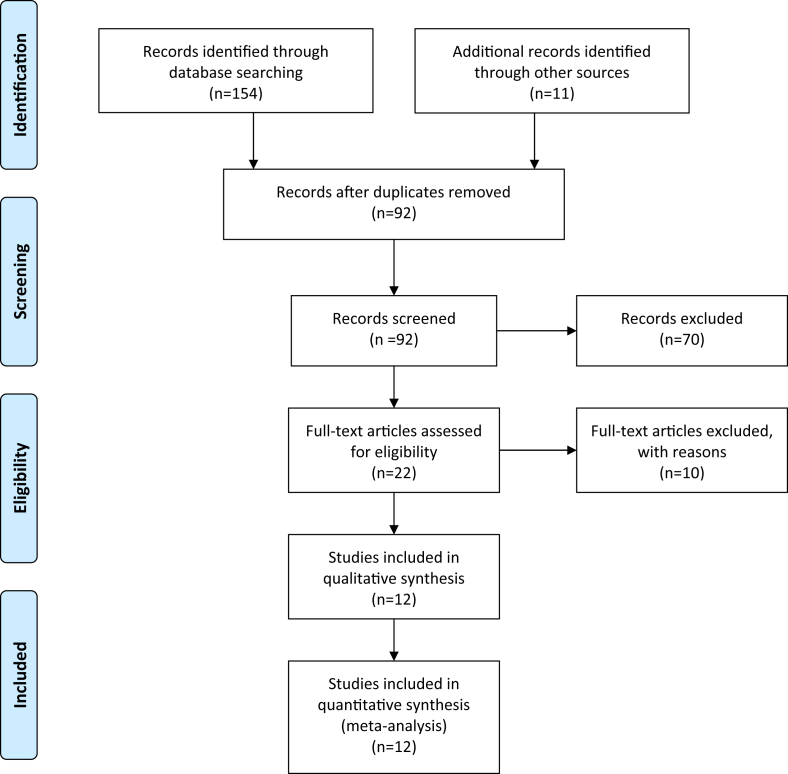
One hundred and fifty four studies were identified. One hundred and thirty two were excluded based on the inclusion/exclusion criteria, leaving 22 potentially relevant papers for detailed evaluation. This was further reduced to 12 studies for inclusion in the meta-analysis, Fig. 1 shows the study selection flow according to PRISMA guidelines. Reasons for exclusion were included irrelevant outcomes measures and incomparable patient groups. After critical appraisal of the full papers Table 2, Table 3 shows the included studies with their characteristics. Pfitzner et al paper compared PSI using CT scans and MRI scans and compared those with standard instrumentation. Therefore, for some of the outcomes this particular study included twice using the CT data once and the MRI data second time.
Fig. 1.
PRISMA chart of the study selection process.
Table 2.
Quality assessment scores of included studies.
| Score | Comments (treatment providers not possible to be blinded in any study) | |
|---|---|---|
| Boonen | 20 | Participants and assessors blinded throughout. Clearly defined outcome measures |
| Abane | 20 | Identical treatment modality apart from surgical technique. Significant number not included in analysis |
| Chareanc. | 19 | Assessors remained blinded to treatment, clear outcomes and assessment methodology |
| Kotela | 20 | Good standardised treatment programmes with blinded assessors. |
| Hamilton | 17 | Assessors blinded to the treatment group, identical treatment strategies (aside from implant) between the two groups. |
| Parratte | 19 | Assessors remained blinded. Standardised technique, participants potentially unblinded. |
| Pfitzner | 20 | Three different implants used in three different groups. |
| Roh | 17 | Comparable groups, clearly defined criteria. Neither participants nor assessors blinded after initial randomisation. |
| Victor | 16 | Good inclusion/exclusion criteria, participants/assessors not blinded after allocation |
| Woolson | 19 | CT scanning of accurate measurements of outcome measures, assessors blinded to treatment. |
| Yan | 16 | Good inclusion/exclusion criteria and defined outcome measures |
| Chotanaphuti | 16 | Standardized treatment protocol, clearly defined outcomes. Assessors not blinded. |
Table 3.
Preoperative characteristics of the included studies.
| PS |
ST |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Implant | M | F | Age | BMI | n | Implant | M | F | Age | BMI | |
| Abane | 70 | Genesis II | 41 | 29 | 67.8 | 28.8 | 70 | Genesis II | 43 | 28 | 70.4 | 28.6 |
| Boonen | 86 | Vanguard | 34 | 56 | 69 | 30.3 | 82 | Vanguard | 40 | 50 | 65 | 29.5 |
| Chareanc. | 40 | NexGen | 6 | 34 | 69.5 | 27.7 | 40 | NexGen | 4 | 36 | 70.3 | 28 |
| Hamilton | 26 | TruMatch | 14 | 21 | 68.1 | 30.9 | 26 | NS | 7 | 19 | 67.6 | 31.1 |
| Kotela | 49 | Vanguard | 16 | 33 | 66.1 | 30.0 | 46 | Vanguard | 13 | 33 | 68.6 | 29.6 |
| Parratte | 20 | NexGen | NS | NS | NS | NS | 20 | NexGen | NS | NS | NS | NS |
| Pfitzner | 60 | TruMatch/Visionaire | 26 | 34 | 64 | 30 | 30 | Journey BCS | 13 | 17 | 64 | 31 |
| Roh | 42 | Vanguard | 3 | 39 | 70 | 27 | 48 | Vanguard | 5 | 43 | 70 | 27 |
| Victor | 64 | Biomet PS | 21 | 43 | 67 | NS | 64 | Biomet PS | 21 | 43 | 66 | NS |
| Woolson | 30 | TruMatch | NS | NS | NS | NS | 33 | NS | NS | NS | NS | NS |
| Yan | 30 | NS | 13 | 17 | 67.5 | NS | 30 | NS | 7 | 23 | 69.8 | NS |
| Chotanaphuti | 40 | TruMatch | NS | NS | 69.7 | 25 | 40 | Sigma | NS | NS | 69.3 | 25 |
n = number of cases, M = male, F = female, BMI = Body mass index, NS = Not specified.
PS instrumentation was used in 538 patients whilst 549 patients underwent ST instrumentation. The mean age of patients was 68.7 (range: 52–87) for the PS and 68.3 (range: 36–92) for the ST group.
Effects of interventions
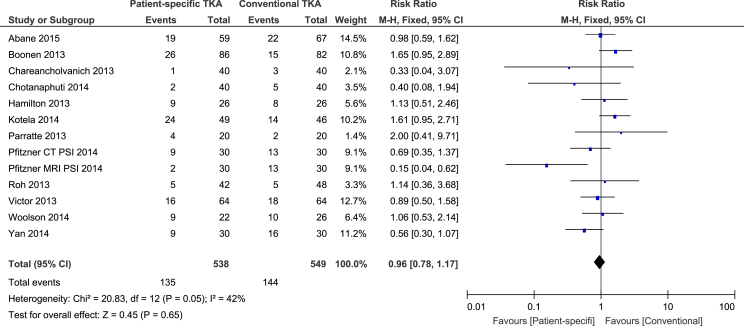
Outliers from mechanical axis
All of the studies11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 were suitable for the meta-analysis of outliers from mechanical axis outcome in 538 PS versus 549 ST knees. The chi-square test for heterogeneity was 20.83 (df = 12, P = 0.05). Number of outliers was similar in both groups 135 vs 144 respectively with risk ratio (RR) 0.96 (95% CI 0.78 to 1.17, p = 0.65) (Table 4).
Table 4.
Outliers from mechanical axis.
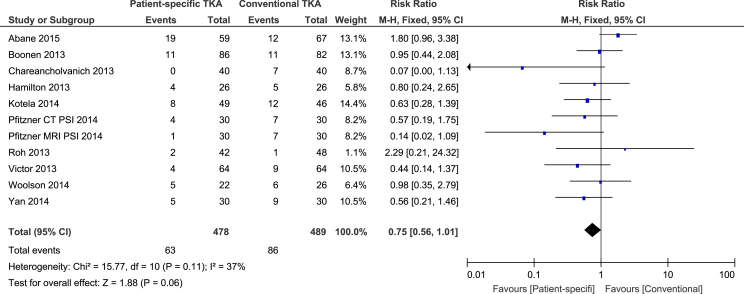
Coronal plane femoral component outliers
Ten studies were suitable for assessment of coronal plane femoral component outliers in 478 PS and 489 ST knees.11, 12, 13, 15, 16, 17, 18, 20, 21, 22 The chi-square test for heterogeneity was 15.77 (df = 10, P = 0.11). There were 63 outliers in PS group and 86 in the ST group, with (RR) 0.75 (95% CI 0.56 to 1.01, p = 0.06) (Table 5).
Table 5.
Coronal plane femoral component outliers.
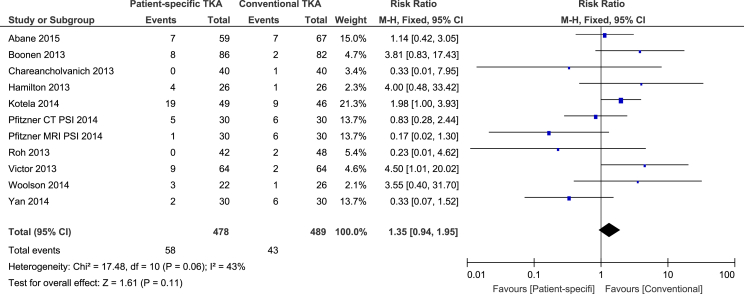
Coronal plane tibial component outliers
The same ten studies as above were eligible for this outcome including 478 PS and 489 ST knees.11, 12, 13, 15, 16, 17, 18, 20, 21, 22 There were 58 outliers in PS group and 43 in ST, with risk ratio (RR) 1.35 (95% CI, 0.94 to 1.95, p = 0.11). The chi-square test for heterogeneity was 17.48 (df = 10, P = 0.06) which necessitate the fixed effect analysis (Table 6).
Table 6.
Coronal plane tibial component outliers.
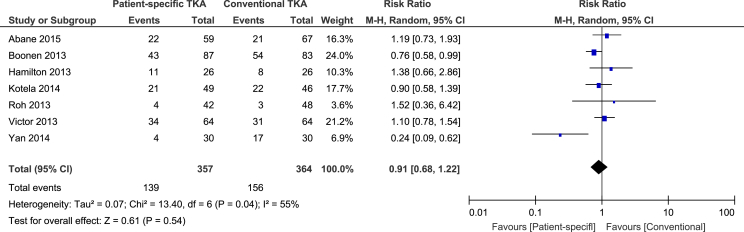
Sagittal plane femoral component outliers
Femoral component sagittal plane outliers were reported in 7 studies11, 13, 15, 16, 18, 20, 21 which included 357 PS and 364 ST cases. The chi-square test for heterogeneity was 13.40 df = 6; P = 0.04. This result leads to a random effects model. There were 139 outliers in the PS group and 156 in the ST group. RR 0.91 (95% CI 0.68 to 1.22, p = 0.54) (Table 7).
Table 7.
Sagittal plane femoral component outliers.
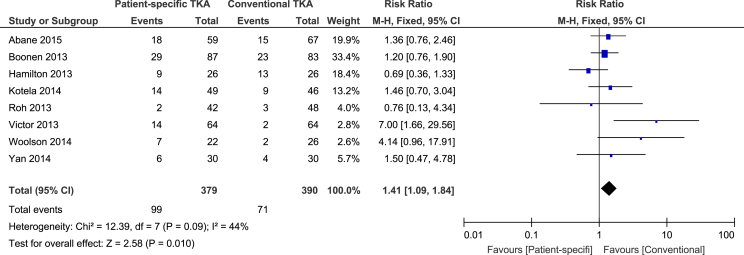
Sagittal plane tibial component outliers
The same seven studies as above were eligible for this outcome, reporting sagittal plane tibial component outliers.11, 13, 15, 16, 18, 20, 21 The chi-square test for heterogeneity was 12.39 (df = 7, P = 0.09). There were 99 outliers in 379 PS knees versus 71 outliers in 390 ST knees. RR 1.41 (95% CI 1.09 to 1.84, p = 0.01) (Table 8). Therefore, the PS group has statistically significantly more outliers than the ST group.
Table 8.
Sagittal plane tibial component outliers.
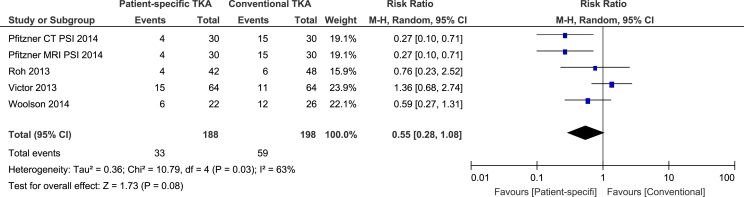
Femoral component rotation outliers
Only four studies15, 16, 17, 22 were suitable for the meta-analysis of femoral component rotation outliers in 188 PS versus 198 ST knees. There were 33 outliers in the first group and 59 in the second one. RR 0.55 (CI 95%, 0.28 to 1.08, p = 0.08). This result is statistically not significant (Table 9). Test for heterogeneity showed chi-squared value of 10.79, df = 4, P = 0.03, prompting a random effects analysis.
Table 9.
Femoral component rotation outliers.
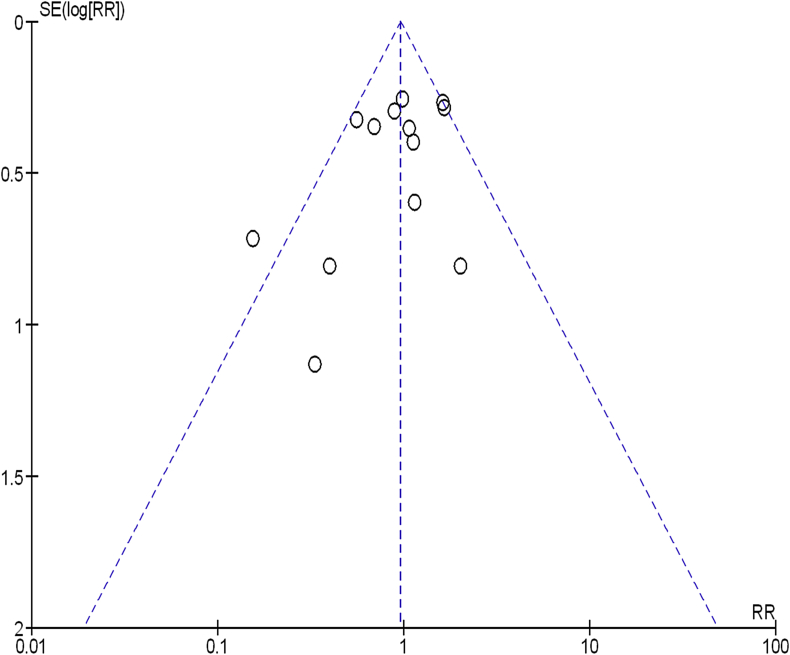
Publication bias
Mechanical alignment outcome was the most commonly used outcome by the studies. Therefore a funnel plot was produced and showed some evidence of a publication bias (Table 10).
Table 10.
Funnel plot analysis for studies reporting on mechanical alignment outcome.
Conclusion
Our findings showed that sagittal plane tibial component outliers were significantly more in the patient specific instrumentation group than the standard group. There was no statistical difference between the femoral component rotation outliers of either group. There were no significant difference between the groups on mechanical axis outliers, tibial component outliers in the coronal planes and no significant difference between the sagittal and coronal femoral component outliers. Therefore; we reject our introductory hypothesis as patient specific instrumentation is not superior to conventional techniques regarding short term alignment of the implants in total knee arthroplasty.
This is also supported by a recent meta-analysis that also included cohort studies as an additional group to the randomised controlled studies.23 They noted that the tibial component positioning in both the sagittal and coronal plane was worse with patient specific instrumentation. However they noted that femoral positioning was improved with the PS instrumentation in the coronal plane only. The use of PS instruments in this study did not reduce the risk of component malalignment.
All of the studies included in this study looked at the use of PS instrumentation for primary osteoarthritis without significant preoperative deformity. Whilst there has been no improvement in component position demonstrated in this group there may be a role in PS instrumentation for the complex total knee replacement where there is a need for intra operative correction of varus/valgus deformity. Further work is needed to fully investigate this.
Limitations of the study included confining the literature search to English language, which may have introduced a language bias. There was significant heterogeneity between findings for some of the outcomes measured. Variations which may have accounted for such heterogeneity include the following; the difference in sample sizes, the variation of patients' demographics such as race, age, gender and BMI, different inclusion and exclusion criteria for each study, The differences in management protocols between centres. Furthermore, there is insufficient data to support the analysis of medium or long term outcomes at present. Therefore, there is a need for well designed future studies to investigate the long term success of this new technique.
The strength of our study is the robust inclusion criteria of only including the randomised controlled trials with the greatest numbers of study participants for the meta-analysis.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Ritter M.A., Herbst S.A., Keating E.M., Faris P.M., Meding J.B. Long-term survival analysis of a posterior cruciate retaining total condylar total knee arthroplasty. Clin Orthop Relat Res. 1994;309:136–145. [PubMed] [Google Scholar]
- 2.Berend M.E., Ritter M.A., Meding J.B. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 3.Huang N.F., Dowsey M.M., Ee E. Coronal alignment correlates with outcome after total knee arthroplasty: five-year follow-up of a randomized controlled trial. J Arthroplast. 2012;27:1737–1741. doi: 10.1016/j.arth.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 4.Lombardi A.V., Jr., Berend K.R., Adams J.B. Patient-specific approach in total knee arthroplasty. Orthopedics. 2008 Sep;31(9):927–930. doi: 10.3928/01477447-20080901-21. [DOI] [PubMed] [Google Scholar]
- 5.Ng V.Y., DeClaire J.H., Berend K.R., Gulick B.C., Lombardi A.V., Jr. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012 Jan;470(1):99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mont M.A., McGrath M.S., Boyd B., Mitrick M.F. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Spencer BA1. Int Orthop. 2009 Dec;33(6):1571–1575. doi: 10.1007/s00264-008-0693-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins J.P.T., Green S. John Wiley & Sons, Ltd; Chichester, UK: 2006. Cochrane Handbook for Systematic Reviews of Interventions 4.2.2. The Cochrane Library, Issue 4. [Google Scholar]
- 8.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Handoll M.M., Elstub H., Elliot J., Cochrane Bone, Joint and Muscle Trauma Group . 2008. About the Cochrane Collaboration (Cochrane Review Groups (CRGS)) (4. Art. No: MUSKINJ.) [Google Scholar]
- 10.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boonen B., Schotanus M.G., Kerens B., van der Weegen W., van Drumpt R.A., Kort N.P. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2013 Oct;21(10):2206–2212. doi: 10.1007/s00167-013-2620-y. [DOI] [PubMed] [Google Scholar]
- 12.Chareancholvanich K., Narkbunnam R., Pornrattanamaneewong C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Jt J. 2013 Mar;95-B(3):354–359. doi: 10.1302/0301-620X.95B3.29903. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton W.G., Parks N.L. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplast. 2014 Jul;29(7):1508–1509. doi: 10.1016/j.arth.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 14.Parratte S., Blanc G., Boussemart T., Ollivier M., Le Corroller T., Argenson J.N. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc. 2013 Oct;21(10):2213–2219. doi: 10.1007/s00167-013-2623-8. [DOI] [PubMed] [Google Scholar]
- 15.Roh Y.W., Kim T.W., Lee S., Seong S.C., Lee M.C. Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of one system. Clin Orthop Relat Res. 2013 Dec;471(12):3988–3995. doi: 10.1007/s11999-013-3206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Victor J., Dujardin J., Vandenneucker H., Arnout N., Bellemans J. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res. 2014 Jan;472(1):263–271. doi: 10.1007/s11999-013-2997-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolson S.T., Harris A.H., Wagner D.W., Giori N.J. Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Jt Surg Am. 2014 Mar 5;96(5):366–372. doi: 10.2106/JBJS.L.01722. [DOI] [PubMed] [Google Scholar]
- 18.Yan C., Chiu K., Ng f., Chan P., Fang C. A randomised controlled trial comparing patient specific instruments with conventional instruments and computer navigation in total knee arthroplasty. Osteoarthr Cartil. April 2014;22(S469–S470):1063–4584. doi: 10.1007/s00167-014-3264-2. [DOI] [PubMed] [Google Scholar]
- 19.Chotanaphuti T., Wangwittayakul V., Khuangsirikul S., Foojareonyos T. The accuracy of component alignment in custom cutting blocks compared with conventional total knee arthroplasty instrumentation: prospective control trial. Knee. 2014 Jan;21(1):185–188. doi: 10.1016/j.knee.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Abane L., Anract P., Boisgard S., Descamps S., Courpied J.P., Hamadouche M. A comparison of patient-specific and conventional instrumentation for total knee arthroplasty: a multicentre randomised controlled trial. Bone Jt J. 2015 Jan;97-B(1):56–63. doi: 10.1302/0301-620X.97B1.34440. [DOI] [PubMed] [Google Scholar]
- 21.Kotela A., Kotela I. Patient-specific computed tomography based instrumentation in total knee arthroplasty: a prospective randomized controlled study. Int Orthop. 2014 Oct;38(10):2099–2107. doi: 10.1007/s00264-014-2399-6. [DOI] [PubMed] [Google Scholar]
- 22.Pfitzner T., Abdel M.P., von Roth P., Perka C., Hommel H. Small improvements in mechanical axis alignment achieved with MRI versus CT-based patient-specific instruments in TKA: a randomized clinical trial. Clin Orthop Relat Res. 2014 Oct;472(10):2913–2922. doi: 10.1007/s11999-014-3784-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thienpont E., Schwab P.E., Fennema P. A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Jt J. 2014 Aug;96-B(8):1052–1061. doi: 10.1302/0301-620X.96B8.33747. [DOI] [PubMed] [Google Scholar]