Abstract
Objective
The aim of this study was to compare the short term effects of home exercise program and virtual reality exergaming in patients with subacromial impingement syndrome (SAIS).
Methods
A total of 30 patients with SAIS were randomized into two groups which are Home Exercise Program (EX Group) (mean age: 40.6 ± 11.7 years) and Virtual Reality Exergaming Program (WII Group) (mean age: 40.33 ± 13.2 years). Subjects were assessed at the first session, at the end of the treatment (6 weeks) and at 1 month follow-up. The groups were assessed and compared with Visual Analogue Scale (based on rest, activity and night pain), Neer and Hawkins Tests, Scapular Retraction Test (SRT), Scapular Assistance Test (SAT), Lateral Scapular Slide Test (LSST) and shoulder disability (Shoulder Pain and Disability Index (SPADI)).
Results
Intensity of pain was significantly decreased in both groups with the treatment (p < 0.05). The WII Group had significantly better results for all Neer test, SRT and SAT than the EX Group (p < 0.05).
Conclusion
Virtual reality exergaming programs with these programs were found more effective than home exercise programs at short term in subjects with SAIS.
Level of Evidence
Level I, Therapeutic study.
Keywords: Shoulder, Rehabilitation, Exercise, Virtual reality, Exergaming
Introduction
Shoulder impingement symptoms in particular appear to be affected by scapular position and motion. Scapular dyskinesis is probably a potential impairment to optimum shoulder function which should be evaluated and treated as part of comprehensive treatment protocol. As a compensatory strategy, scapular dyskinesis is described as the abnormal rhythm of the scapula during shoulder movements.1, 2 Scapular dyskinesis is associated with impingement by altering arm motion upon dynamic elevation and scapular position at rest.3 Scapular dyskinesis can be treated conservatively and shoulder problems related can be avoided. The goal of treatment is to maintain the optimal function of scapular position.1 Exercise approaches such as core stability, open and closed kinetic chain exercises and scapular stabilization exercises are used for the rehabilitation progressions of scapular dyskinesis. The aim of these exercise approaches is to restore the optimal functional position of the scapula and to eliminate muscular imbalance.4, 5, 6
Rehabilitation of these problems should include patient management trends and newest advances in rehabilitation medicine. Virtual reality exergaming is a newly used method and increases motivation of the subject and participation to exercise better than conventional treatments. Virtual reality exergaming program is a three-dimensional and computer-aided program which is built with a system that creates virtual reality movements. This creates high amount of visual and sensory feedback during exercise. Created screen avatar allows subjects to detect movement through remote control.7 To the best of our knowledge, there is a lack of literature about virtual reality exergaming in subjects with orthopedic problems, the aim was to investigate the short term effects of virtual reality exergaming program and home exercise program approaches on scapular dyskinesis in subjects with SAIS.
Patients and methods
The study protocol was approved by the University Ethics Committee (LUT 12/131-28). An informed consent form was taken from all subjects. 30 volunteered subjects diagnosed with SAIS and scapular dyskinesis were randomly divided into 2 groups which are Group 1 – Virtual Reality Exergaming Program (WII) and Group 2 – Home Exercise Program (EX). None of the subjects were affected by any rotator cuff problem. The subjects were randomly assigned to the one of the groups using an online random allocation software program (GraphPad Software QuickCalcs, GraphPad Software Inc., La Jolla, California, USA). All groups were taken into a 6 week treatment program. At the end of the treatment process, 1 month of control period was given to subjects including home exercise program aiming scapular muscles.
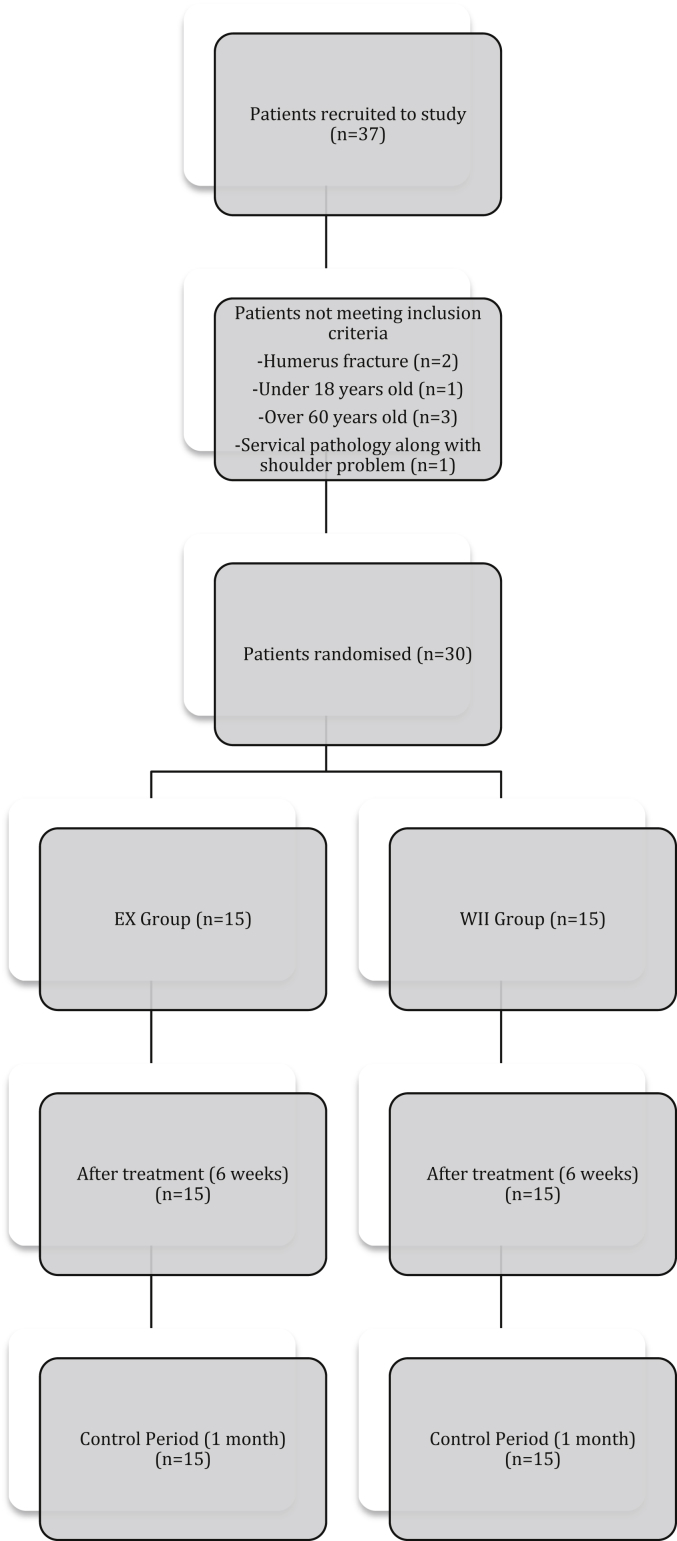
Exclusion criteria were if subject; had any other soft tissue or bone problems affecting shoulder, had any neurologic problems, had scoliosis, had any systematic rheumatic problems, other orthopedic problems or surgery affecting neck, obesity (BMI > 30). The ages of 18–60 years were included in the study (Fig. 1). All patients were diagnosed with type 2 SAIS which was confirmed with MRI.
Fig. 1.
Flow Chart of the study.
Subjects were assessed before, at the end of the treatment (6 weeks) and at control period (1 month after the end of treatment). Assessments included the severity of pain (at rest, during activity and at night) which was evaluated by Visual Analog Scale (VAS). VAS is a 100 mm line with no marks along them, anchored with the words “no pain” on one hand, and “the most severe pain” on the other. Subjects were simply instructed to place a mark along the line at a level representing the intensity of their pain at rest, during activity and at night for the past one month.8, 9, 10
Neer and Hawkins tests were performed for evaluation of SAIS. To perform Neer test, subject sat in upright position. Examiner raised the testing arm to flexion in scapular plane passively. In this way subacromial space was narrowed, and if there is a pathology, pain is provocated. It shows that the test is positive.11 To perform Hawkins test, subject sat in same position. Examiner passively put the subjects' upper extremity in 90° shoulder flexion, maximum internal rotation and 90° elbow flexion. In this way subacromial space was narrowed, and if there is a pathology, pain is provocated. It shows that the test is positive.2, 12
Lateral Scapular Slide Test (LSST), Scapular Retraction Test (SRT) and Scapular Assistance Test (SAT) were used to determine scapular dyskinesis. LSST was performed in three positions. For test position one of the LSST, subjects were instructed to keep their upper extremities relaxed at their sides. The assessor obtained and confirmed the test position and then identified through palpation and marked the inferior aspect of the inferior angle of the scapula and the closest spinous process in the same horizontal plane. The distance between the two reference points was measured bilaterally with a tape measure. For test position two, the subject was instructed to actively place both hands on the ipsilateral hips, and consequently the humerus was positioned in medial rotation at 45° of abduction in the coronal plane. In test position three, subjects were instructed to actively extend both elbows and to elevate and maximally internally rotate (“thumbs down”) both upper extremities to 90° in the coronal plane. All scapular distance measurements were taken two times. A difference of 1.5 cm or more in any of the three positions was considered a positive result of the LSST.1, 3, 10, 13
To perform SRT, the scapula is passively moved toward posterior tilt and external rotation with slight voluntary retraction. This test appears to be altering scapular kinematics by increasing posterior tilt, external rotation, and scapular retraction (defined as the projected angle in the transverse plane formed between the sternum and acromion relative to the frontal plane bisecting the sternal notch) as compared to elevation against resistance without the scapula stabilized.13, 14, 15
SAT was performed with scapular upward rotation manually assisted during arm elevation. It has demonstrated reliability and has been shown to reduce pain in approximately half of symptomatic subjects tested. This test appears to be altering scapular kinematics by increasing posterior tilt and decreasing scapular elevation (defined as the projected angle in the coronal plane formed between the sternum and acromion relative to the transverse plane bisecting the sternal notch).13, 14, 15
Shoulder Pain and Disability Index (SPADI) was used to measure pain and disability associated with shoulder pathology. This index is validated in subjects with shoulder dysfunctions undergoing physical therapy or general medical treatment with diagnoses of impingement syndrome, degenerative joint disease, non-specific shoulder pain, osteoarthritis, total shoulder arthroplasty, rotator cuff surgery, glenohumeral instability/dislocation, rotator cuff syndrome, adhesive capsulitis, status-post fracture and shoulder weakness. Scoring range is 0–50 SPADI points for pain, 0–50 SPADI points for function/disability, total score 0–100 (worse pain and function/disability). Higher scores reflect greater pain and disability.5, 16
Subjects were included in a home exercise program for 6 weeks, 2 days per week and 45 min for day. 6 weeks of treatment was performed for assessment of short term effects. Exercises were done without resistance for the first week. Resistive training was given beginning from the second week with a proper resistance of Theraband®. The proper color of Theraband® was determined for the subject's proper resistance to 10 repetitions of movement. Exercises and Theraband® resistance was checked weekly. Home exercise program included posterior, anterior and inferior capsule stretching, pectoral muscle stretching, serratus anterior muscle strengthening, bilateral shoulder elevation, and scapular mobility exercises.
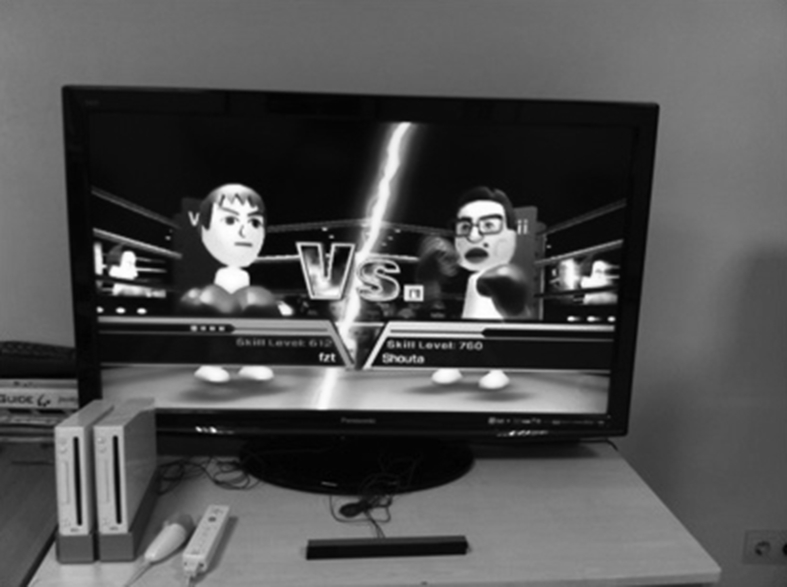
Subjects were included in a supervised virtual reality exergaming program for shoulder movements with Nintendo Wii (Nintendo, Kyoto, Japan) for 6 weeks, 2 days per week and 45 min for day. This program includes warming and cooling periods with posterior, anterior and inferior capsule stretching and pectoral muscle stretching. Exercise training includes bilateral shoulder elevation, boxing, bowling and tennis games accompanied by avatar. These exercises are parallel to the given home exercise program. Exercises were done without resistance for the first week. Progression of the resistive training was provided with Theraband® resistive exercise tools. Exercises and Theraband® resistance was checked weekly (Fig. 2).17, 18
Fig. 2.
Virtual reality exergaming equipment.
All statistical analysis was performed using SPSS v 18 (IBM, Armonk, NY, USA). Kruskal Wallis test and Chi-Square test were used to analyze the homogeneity of groups in sociodemographic parameters. A linear mixed model was used to evaluate the change of the groups across the three assessment time points for each dependent measure separately. The factors of interest were group (WII and EX) and time (before treatment, after treatment and control period). All statistical analysis was set a priori at an alpha level of p ≤ 0.05. If significance was found post-hoc analysis with a Bonferroni correction for multiple comparisons was used to determine differences between specific factors.
Results
The power analysis indicated that 15 subjects for each group were needed with 80% power and a 5% type 1 error. The power analysis of this study showed a power of 80% with shoulder pain at activity as the primary outcome. Thirty subjects with the mean age of 40.6 ± 11.7 years and the mean body mass index of 24.47 ± 4.27 kg/m2 for EX Group and the mean age of 40.33 ± 13.2 years and the mean body mass index of 23.31 ± 4.56 kg/m2 for WII Group participated in this study. Sociodemographic characteristics of participants are shown in Table 1.
Table 1.
Sociodemographic characteristics of subjects.
| EX | WII | p | |
|---|---|---|---|
| Age, years | 40.60 ± 11.77 | 40.33 ± 13.20 | 0.083b |
| BMI, kg/m2 | 24.47 ± 4.27 | 23.31 ± 4.56 | 0.567b |
| Gender, n (%) | |||
| Female | 13 (86.7) | 14 (93.3) | 0.000a,c |
| Male | 2 (13.3) | 1 (6.7) | |
| Dominant side, n (%) | |||
| Right | 15 (100) | 15 (100) | 0.000a,c |
| Left | 0 (0) | 0 (0) | |
| Affected side, n (%) | |||
| Right | 9 (60) | 7 (46.7) | 0.302c |
| Left | 6 (40) | 8 (53.3) | |
X ± SD: mean ± standard deviation, BMI: body mass index, EX: Home Exercise Program, WII: Virtual Reality Exergaming Program.
p < 0.05 statistically different.
Kruskal Wallis Test.
Chi-Square Test.
Intensity of pain was significantly decreased in both groups between time factors (p < 0.05). Statistically significant difference was found in Neer test at WII group (p < 0.05) but Hawkins test did not show any difference in both groups (p > 0.05). Also statistically significant difference was found in SRT and SAT Tests at WII group (p < 0.05), but there was no significant difference at EX group results (p > 0.05). LSST test results did not show any significant difference in both groups at all time factors (p > 0.05). SPADI results showed significant difference at all time factors in WII group (p < 0.05), but only showed significant difference at control period in EX group (p < 0.05) (Table 2).
Table 2.
The mean differences in pain, disability, SAIS symptom tests and scapular dyskinesia test parameters between two groups and three time factors.
| EX |
WII |
pb | |||||
|---|---|---|---|---|---|---|---|
| BT-AT X ± SE (pc) |
AT-C X ± SE (pc) |
BT-C X ± SE (pc) |
BT-AT X ± SE (pc) |
AT-C X ± SE (pc) |
BT-C X ± SE (pc) |
||
| Pain at rest (cm) | 2.20 ± 0.90 (0.065) | 0.20 ± 0.46 (1.00) | 2.41 ± 0.83 (0.028a) | 2.00 ± 1.18 (0.309) | 2.06 ± 0.60 (1.00) | 2.00 ± 1.09 (0.237) | 0.263 |
| Pain during activity (cm) | 3.00 ± 1.03 (0.022a) | 1.16 ± 0.45 (0.050) | 4.16 ± 1.01 (0.001a) | 5.85 ± 1.35 (0.001a) | 0.00 ± 0.59 (1.00) | 5.85 ± 1.33 (0.000a) | 0.446 |
| Pain at night (cm) | 1.79 ± 0.94 (0.209) | 0.79 ± 0.66 (0.730) | 2.58 ± 0.97 (0.039a) | 4.65 ± 1.24 (0.003a) | 5.20 ± 0.86 (1.00) | 4.65 ± 1.27 (0.003a) | 0.050 |
| SPADI Score | 5.50 ± 3.60 (0.414) | 11.41 ± 2.30 (0.000a) | 16.92 ± 4.10 (0.001a) | 13.29 ± 4.71 (0.027a) | 8.13 ± 3.01 (0.036a) | 21.42 ± 5.37 (0.001a) | 0.536 |
| Neer | 0.25 ± 0.16 (0.412) | 0.08 ± 0.08 (1.00) | 0.33 ± 0.13 (0.061) | 0.57 ± 0.21 (0.038a) | 0.00 ± 0.11 (1.00) | 0.57 ± 0.17 (0.010a) | 0.020a |
| Hawkins | 0.33 ± 0.16 (0.169) | 0.00 ± 0.10 (1.00) | 0.33 ± 0.15 (0.127) | 0.57 ± 0.21 (0.050) | 0.00 ± 0.13 (1.00) | 0.57 ± 0.20 (0.051) | 0.349 |
| SRT | 4.44 ± 0.13 (1.00) | 0.08 ± 0.12 (1.00) | 0.08 ± 0.12 (1.00) | 0.57 ± 0.18 (0.011a) | 2.22 ± 0.16 (1.00) | 0.57 ± 0.16 (0.005a) | 0.010a |
| SAT | 0.41 ± 0.16 (0.054) | 0.83 ± 0.12 (1.00) | 0.33 ± 0.13 (0.067) | 0.57 ± 0.21 (0.041a) | 0.00 ± 0.16 (1.00) | 0.57 ± 0.18 (0.011a) | 0.047a |
| LSST-1 | 0.16 ± 0.14 (0.794) | 1.58 ± 1.07 (0.461) | 1.41 ± 1.02 (0.537) | 0.42 ± 0.19 (0.101) | 0.42 ± 1.41 (1.00) | 0.85 ± 1.34 (1.00) | 0.591 |
| LSST-2 | 0.16 ± 0.15 (0.893) | 0.16 ± 0.08 (0.214) | 2.22 ± 0.17 (1.00) | 0.28 ± 0.20 (0.528) | 0.00 ± 0.11 (1.00) | 0.28 ± 0.23 (0.681) | 0.696 |
| LSST-3 | 0.08 ± 0.15 (1.00) | 0.08 ± 0.08 (1.00) | 2.22 ± 0.15 (1.00) | 0.42 ± 0.19 (0.114) | 0.28 ± 0.11 (0.050) | 0.14 ± 0.20 (1.00) | 0.057 |
BT: before treatment, AT: after treatment, C: control period, X ± SE: mean ± standard error, SPADI: Shoulder Pain and Disability Index, SRT: Scapular Retraction Test, SAT: Scapular Assistance Test, LSST-1: Lateral Scapular Slide Test position 1, LSST-2: Lateral Scapular Slide Test position 2, LSST-3: Lateral Scapular Slide Test position 3, EX: Home Exercise Program, WII: Virtual Reality Exergaming Program.
p < 0.05.
Comparison of two groups (Greenhouse-Geisser).
Comparison of three time factors.
Discussion
In this study the short term effects of home exercise program and virtual reality exergaming program on scapular dyskinesis in subjects with SAIS is investigated and found that virtual reality exergaming program has made better improvement in decreasing the symptoms of SAIS and scapular dyskinesis.
Much is known about the decreasing effects of physical exercise on pain related to musculoskeletal system at shoulder region.6, 8, 18, 19, 20 Andersen et al19 stated that special exercise programs given 2 days/week reduce pain in women with severe neck and shoulder pain problems. Parallel to the literature, it is found that exercise is a good solution to reduce pain. Both home exercise program and virtual reality exergaming reduces pain during activity and night at short term (before–after treatment) and long term (1 month follow-up). Virtual reality exergaming has increased the perception of the shoulder joint due to the increase in body awareness of individuals. Through this sensory-perception-motor response resulting in reduction of pain, virtual reality exergaming is thought to be an effective treatment approach. There is limited research in the literature addressing the effects of virtual reality exergaming on musculoskeletal pain problems. For this reason, this study may be important for further studies.
According to many studies in the literature, exercise training decreases disability and increases quality of life.18, 19, 20 In this study, all exercise training protocols have decreased disability and increased quality of life, but virtual reality exergaming has decreased disability in all time factors assessed. It is believed that virtual reality exergaming programs may be more acceptable and exercisable, more comfortably in the field of physiotherapy and rehabilitation because of developing modern life and impacts of technological developments.
Neer and Hawkins tests are the most specifically used symptom aggravating tests in clinic.21 MacDonald et al12 stated that Neer test has a reliability of 75% and Hawkins test 92%. Valadie et al22 reported that both Neer and Hawkins tests are consistent diagnostic methods at determining SAIS in their study on cadavers. According to this study virtual reality exergaming has made significant decrease in SAIS symptom tests. As no similar studies have been found in the literature, this study can show a way to further studies. These effects can lead to important advantages of increasing exercise performance in rehabilitation process.
An important limitation of this study was the lack of three-dimensional kinetic assessment protocol usage in scapular movements. This could be more objective for giving the scapular dyskinesis change results. Another important limitation was that we could not check the patients if they did the exercises at home regularly. We could only check them once a week for the home exercise group.
According to this study results, virtual reality exergaming had positive change in scapular dyskinesis better than home exercise program. Considering this situation, it can be stated that, virtual reality exergaming program is more effective than home exercise program in the treatment of scapular dyskinesis.
Virtual reality exergaming programs provide visual and sensory feedbacks on exercise which makes individual's perception become more and more effective. For physiotherapist, as one of the main treatment modalities of exercise, virtual reality exergaming is a different and newly used method with the phenomenon of sense-perception-motor which is important in delivering the highest level of integrity. As providing sensory-perception-motor input is very important in functional rehabilitation, not only virtual reality exergaming, but also exercises with supervision of a physiotherapist would obtain positive effects on rehabilitation program. In the literature there is lack of studies about virtual reality exergaming on shoulder pathologies and hope that this study would lead a way to further researches. Hence, further studies are needed with more sample sizes, longer treatment periods and different exercise protocols.
Acknowledgements
The authors would like to thank Ahmet Ozgur Atay, MD, Prof. and Mehmet Demirtas MD, Prof. for their contributions in diagnosing patients and guidance.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Tate A.R., McClure P., Kareha S., Irwin D., Barbe M.F. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165–173. doi: 10.4085/1062-6050-44.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hawkins R.H. Clinical assessment of the shoulder. Can J CME. 2001:87–99. [Google Scholar]
- 3.Shadmehr A., Bagheri H., Ansari N.N., Sarafraz H. The reliability measurements of lateral scapular slide test at three different degrees of shoulder joint abduction. Br J Sports Med. 2010;44(4):289–293. doi: 10.1136/bjsm.2008.050872. [DOI] [PubMed] [Google Scholar]
- 4.Phadke V., Camargo P.R., Ludewig P.M. Scapular and rotator cuff muscle activity during arm elevation: a review of normal function and alterations with shoulder impingement. Braz J Phys Ther. 2009;13(1):1–9. doi: 10.1590/S1413-35552009005000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roach K.E., Budiman-Mak E., Songsiridej N., Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4(4):143–149. [PubMed] [Google Scholar]
- 6.Saposnik G., Teasell R., Mamdani M. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: a pilot randomized clinical trial and proof of principle. Stroke. 2010;41(7):1477–1484. doi: 10.1161/STROKEAHA.110.584979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Huiginn B., Smyth B., Coughlan G., editors. Therapeutic Exergaming, Sixth International Workshop on Wearable and Implantable Body Sensor Networks. BSN, Proceedings. 2009. [Google Scholar]
- 8.Ludewig P.M., Borstad J.D. Effects of a home exercise programme on shoulder pain and functional status in construction workers. J Occup Env Med. 2003;60(11):841–849. doi: 10.1136/oem.60.11.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deutsch J.E., Borbely M., Filler J. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther. 2008;88(10):1196–1207. doi: 10.2522/ptj.20080062. [DOI] [PubMed] [Google Scholar]
- 10.Özünlü N., Tekeli H., Baltacı G. Lateral scapular slide test and scapular mobility in volleyball players. J Athl Train. 2011;46(4):462–468. doi: 10.4085/1062-6050-46.4.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neer C.S. Impingement lesions. Clin Orthop Relat Res. 1983;173:70–77. [PubMed] [Google Scholar]
- 12.MacDonald P.B., Clark P., Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000;9(9):299–301. doi: 10.1067/mse.2000.106918. [DOI] [PubMed] [Google Scholar]
- 13.Kibler W.B., Ludewig P.M., McClure P.W., Michener L.A., Bak K., Sciascia A.D. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. 2013;47(14):877–885. doi: 10.1136/bjsports-2013-092425. [DOI] [PubMed] [Google Scholar]
- 14.Kibler W.B., Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44:300–305. doi: 10.1136/bjsm.2009.058834. [DOI] [PubMed] [Google Scholar]
- 15.Kibler W.B., Ludewig P.M., McClure P., Uhl T.L., Sciascia A. Scapular summit 2009: introduction. J Orthop Sports Phys Ther. 2009;39(11):1–13. doi: 10.2519/jospt.2009.0303. [DOI] [PubMed] [Google Scholar]
- 16.McClure P., Michener L. Measures of adult shoulder function: the American Shoulder and Elbow Surgeons standardized shoulder form subject self-report section (ASES), Disabilities of the Arm, Shoulder, and Hand (DASH), Shoulder Disability Questionnaire, Shoulder Pain and Disability Index (SPADI), and simple shoulder test. Arthritis Care Res. 2003;49(5):50–58. [Google Scholar]
- 17.Baltacı G. Sporcularda subakromiyal sıkışma sendromuna yaklaşım: korunma ve egzersiz programları. Acta Orthop Traumatol Turc. 2003;37(1):128–138. [PubMed] [Google Scholar]
- 18.Baltaci G., Harput G., Haksever B., Ulusoy B., Ozer H. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sport Tr A. 2013;21(4):880–887. doi: 10.1007/s00167-012-2034-2. [DOI] [PubMed] [Google Scholar]
- 19.Andersen C.H., Andersen L.L., Pedersen M.T. Dose-response of strengthening exercise for treatment of severe neck pain in women. J Strength Cond Res. 2013;27(12):3322–3328. doi: 10.1519/JSC.0b013e31828f12c6. [DOI] [PubMed] [Google Scholar]
- 20.Ludewig P.M., Cook T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 21.Çalış M., Akgün K., Birtane M., Karacan I., Caliş H., Tüzün F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. 2000;59(1):44–47. doi: 10.1136/ard.59.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valadie A.L., Jobe C.M., Pink M.M., Ekman E.F., Jobe F.W. Anatomy of provocative tests for impingement syndrome of the shoulder. J Shoulder Elbow Surg. 2000;9(1):36–46. doi: 10.1016/s1058-2746(00)90008-9. [DOI] [PubMed] [Google Scholar]