Abstract
Objective
The aim of this study was to evaluate preoperative and postoperative spinopelvic parameters and the influence of lowest instrumented vertebrae on sagittal parameters in Lenke 5 Adolescent Idiopathic Scoliosis (AIS) patients.
Methods
A total of 42 patients (37 females, 5 males; mean age: 16.71 ± 3.46 years) were included in the study. Preoperative and postoperative last follow up lumbar lordosis (LL), thoracic kyphosis (TK), pelvic tilt (PT), pelvic incidence (PI) and sacral slope (SS) angles measured. By stopped fusion in L3, L4 or L5 we divided the group into three parts.
Results
Mean follow-up was 43 months. Preoperatively, the mean TK and LL were 36.8° and 55.3°. At the last follow up, the mean TK and LL were 27.1° and 49.0° degrees, respectively. Preoperatively, the mean PI, PT and SS were 53.3°, 16.1° and 37.4° degrees. At the last follow up, the mean PI, PT and SS were 52.7°, 19.9° and 33.0° respectively. Significant differences were observed for SS (p = 0.003), TK (p = 0.004), LL (p = 0.012) and PT (p = 0.013) postoperatively for all patients. According the L3 and L4 groups there is significant difference in SS, LL (p = 0.013) and PT (p = 0.018) which means a significant decrease occurs in SS and LL when the distal fusion level changes from L3 to L4 but significant increase in PT in L3 group to compensate spinopelvic change after surgery.
Conclusion
The selection of more distal level for fusion adversely affects the compensation mechanisms of sagittal balance in Lenke 5 AIS patients.
Level of Evidence
Level IV, Therapeutic study.
Keywords: Lenke 5, Scoliosis, Sagittal, Spinopelvic, Compensate
Introduction
Although the scoliosis is known to be a three-dimensional deformity for decades, it has recently grasped the attention of the spinal surgeons to pay attention for balance in the sagittal plane.1 As a result of the limited understanding of the interaction between spinal and pelvic motion, methods for achieving better sagittal balance has been difficult and somewhat unclear. Nevertheless, satisfactory treatment for adolescent idiopathic scoliosis (AIS) has been accepted to include adequate restoration of coronal and sagittal deformity.2
Interest to investigate outcomes related to sagittal balance in AIS started to take a rise by the beginning of the third millennium with the introduction of modern spinal instrumentation. In such an effort, Mac-Thiong et al3 evaluated the spinopelvic sagittal alignment in AIS and found lumbar lordosis was strongly related to pelvic configuration. Likewise Upasani et al4 also found that the sagittal contour of the lumbar spine was in strong association with the pelvic positioning. Yang et al5 determined that almost half of AIS patients with Lenke 5 curves had an antevert pelvis which could not be corrected by posterior instrumentation alone especially when patients had small PI or distal lower end vertebra.
Lenke type 5 scoliosis is characterized by a structural thoracolumbar or lumbar (TL/L) curve. For this type, recommended instrumentation for fusion should include the structural region, however this may cause decompensation of spinopelvic alignment due to restriction of mobile segments close to spinopelvic region.6, 7 Thus, we aimed to analyze the pre and postoperative changes and the effect of distal fusion level on spinopelvic parameters in Lenke 5 AIS patients.
Patients and methods
A retrospective study of Lenke 5 AIS patients treated at a single institution between 2010 and 2015 by a single surgeon was conducted. Inclusion criteria included: 1) a diagnosis of Lenke type 5 AIS, 2) patients treated with posterior pedicle screw only instrumentation, 3) no previous spine surgery 4) full sets of preoperative and last follow-up standing full-length AP and lateral radiographs. Patients who had previous spinal surgery, suffered from congenital deformities, hybrid constructs, anterior surgery and osteotomy were excluded. Those whose radiographs did not meet standards were also excluded in order to discard measurement error. A total of 218 AIS patients in the database were assessed and finally 42 patients (37 females, 5 males) with mean ages 16.71 ± 3.46 were included in the study who met all the criteria.
Radiographical assessment
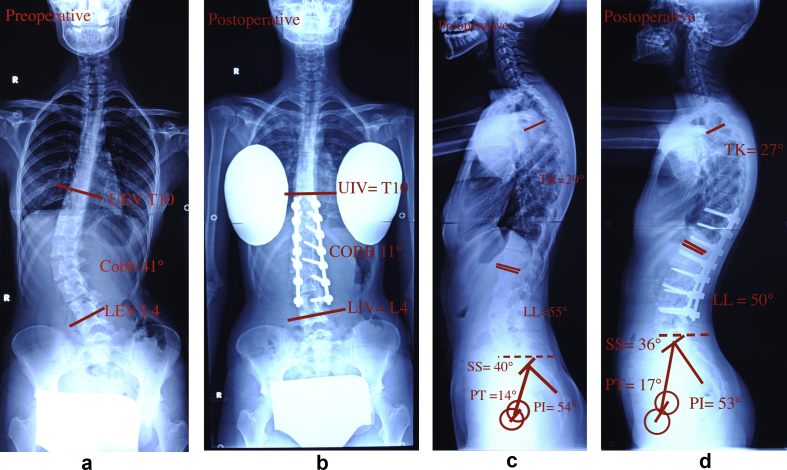
Preoperative, postoperative and last follow-up standing full-length AP radiographs were analyzed by a surgeon who did not attend the surgeries, surveying for study variables with means of a digital software (The Surgimap software New York, NY, USA). Sought out study variables were lumbar lordosis (LL), thoracic kyphosis (TK), pelvic tilt (PT), pelvic incidence (PI) and sacral slope (SS) angles. The definition of the fore mentioned study variables are provided in Fig. 1 to provide better apprehension. Furthermore patients were categorically separated into 3 groups depending on the distal most level fused during the surgery as which being L3 (group L3), L4 (group L4) or L5 (group L5).
Fig. 1.
A. Preoperative lateral view of a 14 year-old girl. Thoracic kyphosis (TK) the angle between superior endplate of T4 and inferior endplate of T12; lumbar lordosis (LL), the angle between superior endplate of L1 and superior endplate of S1; sacral slope (SS), the angle between the superior endplate of S1 and the horizontal line; pelvic incidence (PI), the angle between the line perpendicular to the superior endplate of S1 and the line connecting the midpoint of superior endplate of S1 to hip axis (HA, the midpoint of the line connecting the centers of two femoral heads); pelvic tilt (PT), the angle between the vertical line and the line connecting the midpoint of superior endplate of S1 to HA (considered positive if angulated behind the vertical line and otherwise negative). B. Postoperative lateral view.
Surgical technique
All surgical procedures were performed by the same attending spinal surgeon. The lowest instrumented vertebrae (LIV) was chosen according to the posteroanterior (PA) and lateral side-bending radiographs prior to surgery. Several surgical maneuvers were used in combination, including rod-rotation, apical vertebral derotation, convex compression, and concave distraction. The pedicle screw-rod system was used for fixation.5
Statistical analysis
Statistical analysis was conducted to seek for difference in study variable values between preoperative and last follow-up periods. Further analysis was conducted to look for difference regarding the distal most level fused during the surgery as which being L3 (group L3), L4 (group L4) or L5 (group L5). Application of Kolmogorov–Smirnov test to study variables' values revealed normal distribution, thus mean and standard deviation values were calculated and used instead of median and range. Independent Samples test was utilized to assess intergroup comparison. P value less than 0.05 was considered to be significant.
Results
The mean age of 42 patients with Lenke 5 AIS (37 females, 5 males) included in this study was 16.71 ± 3.46 years. The lowest instrumented vertebra (LIV) was L3 in 21, L4 in 18, and L5 in 3 patients. Mean preoperative TL/L Cobb was 40.11° (range 39), early postoperative Cobb was 7.07° (range 36), and last follow-up Cobb was 7.09° (range 35). Mean correction rate in the early postoperative period was 82.5% (range 92%) and last follow-up was 82.35% (range 90%). The mean follow-up was 43 ± 18.05 months. Preoperatively, the mean TK and LL were 36.8°± 15.8 and 55.3°± 13.7. At the last follow up, the mean TK and LL were 27.1°± 10.2 and 49.0°± 10.4, respectively. Preoperatively, the mean PI, PT and SS were 53.3°± 14.3, 16.1°± 9.5 and 37.4°± 8.9°. At the last follow up, the mean PI, PT and SS were 52.7°± 13.7, 19.9°± 10.8 and 33.0°± 7.4, respectively. Significant decrease was observed for SS (p = 0.003), TK (p = 0.004), LL (p = 0.012) and significant increase for PT (p = 0.013) postoperatively for all patients (Table 1). This may be commented as surgery is effective at correcting major sagittal parameters. Statistical analysis of results when the patients are further grouped for distal most instrumented level revealed significant difference in SS, LL (p = 0.013) and PT (p = 0.018) between group L3 and group L4. However, apart from this difference no other intergroup relation was found. Table 2 represents the measurements of sagittal parameters grouped for lowest instrumented vertebrae.
Table 1.
Preoperative and postoperative values of Cobb angle and spinopelvic parameters.
| Preoperative | Postoperative | p Value | |
|---|---|---|---|
| Cobb angle* | 40.11° | 7.07° | >0.005* |
| PI (Pelvic incidence) | 53.3°± 14.3 | 52.7°± 13.7 | 0.505 |
| PT* (Pelvic tilt) | 16.1°± 9.5 | 19.9°± 10.8 | 0.013* |
| SS* (Sacral slope) | 37.4°± 8.9 | 33.0°± 7.4 | 0.006* |
| LL* (Lumbar lordosis) | 55.3°± 13.7 | 49.0°± 10.4 | 0.015* |
| TK* (Thoracic kyphosis) | 36.8°± 15.8 | 27.1°± 10.2 | 0.003* |
* p < 0.05 is significant.
Table 2.
Measurements of sagittal parameters grouped for lowest instrumented vertebra.
| Postoperative | L3 group | L4 group | p Value |
|---|---|---|---|
| Cobb angle | 7.68° | 7.98° | 0.682 |
| PI (Pelvic incidence) | 57.33° | 48.11° | 0.423 |
| PT* (Pelvic tilt) | 21.48° | 17.85° | 0.018* |
| SS* (Sacral slope) | 35.36° | 29.76° | 0.013* |
| LL* (Lumbar lordosis) | 52.31° | 45.47° | 0.013* |
| TK (Thoracic kyphosis) | 23.73° | 28.76° | 0.068 |
* p < 0.05 is significant.
Discussion
Studies investigating spinopelvic sagittal alignment in AIS are plenty. But, there are few studies which focus on spinopelvic parameters specifically in Lenke 5 AIS patients.5, 8, 9 We believe that for the evaluation of spinopelvic parameters, Lenke 5 patients represent a more valuable subgroup, due to the fact that primary correction takes place in lumbar region.
In our study we found mean presurgical PI and PT values to be 53.3 ± 14.3 and 16.1 ± 9.5 consecutively which indicates that our patients did not have significant pelvic anteversion prior to surgery. This we find a little different then the alike literature since pelvic anteversion is accepted to be a common deformity in Lenke 5 AIS patients. Yang et al5 reported that almost half of their AIS patients had anteverted pelvis. However, Xu et al7 reported that they observed pelvic anteversion in only 25% of their patients, similar to our study. Mac-Thiong et al10 have revealed that the limit of PT was based on the percentage of PI/2 and Roussouly et al11 proposed that there are three variations to the position of pelvis with the regard to PT: anteverted, normal and retroverted. In our study PT value was between 20% of PI/2 and 80% of PI/2, which showed normal version of pelvis.
Several studies have emphasized that increased pelvic anteversion and sacral slope seen in AIS patients is a result of a compensatory change to lumbar hyperlordosis.4, 10, 12 As a result of this one can expect to see improved pelvic sagittal parameters after surgical correction of lumbar hyperlordosis.13
Our study showed that pelvic incidence (PI) did not change significantly after the surgery (53.3°–51.9°) whereas sacral slope (SS) did decrease by surgery (37.4°–33.0°) and pelvic tilt (PT) did increase to compensate (16.1°–19.9°) significantly. The reduction in sacral slope is found to be in tune with improvement in lumbar hyperlordosis (55.3°–49.0°) after the surgery. This indicates that the decrease in the lumbar lordosis is compensated by the decrease in the sacral slope and the increase in the pelvic tilt. As a result, the pelvic incidence has not changed. When we compared these results with alike literature, we found out that Xu et al7 have come along with similar results but reporting no significant change for PI and PT and significant change for SS after surgical correction of lumbar hyperlordosis. Furthermore, two different series by Roussouly and Yang found no significant difference for PI but reported significant difference for SS and PT after the surgery as same as with our findings.5, 11
Yang et al also stated that an abnormal pelvic sagittal state would not generally be corrected when patients have a low PI value (less than 39.8).5, 14 Coherent with this statement we believe that PI values in our patients were not great enough to facilitate any pelvic compensation.
Furthermore, our results contradict to the common opinion that AIS generally represents with thoracic hypokyphosis.15, 16 Mean thoracic kyphosis value for our patients was 36.8° and it changed to 27.1° postoperatively. While these presurgical values do not represent hypokyphosis, surgery seems to be further decreasing amount of kyphosis. This we believe may be a result of compensation to correction of lumbar lordosis or simple over correction by the surgeon.
Choice of lowest instrumented vertebrae is another issue of debate which takes amount of mobility left for patient after the surgery.17 Basic approach to this problem has been that the further the instrumentation goes distal ward the better the correctional results especially for lumbar sagittal parameters.18 On the other hand there are numerous studies which rise uncertainty on this hypothesis.19, 20, 21 Schwab et al found that patients with instrumentation involving L5 represented relatively increased lordosis after the surgery when compared to L4 and L3.13 They believe that fusing L5 decreases the effectiveness of pelvic compensatory mechanisms resulting in relatively higher lumbar lordosis especially in cases which represent profound preoperative anteverted pelvis.
Yang et al5 showed in their patient series that when L3 was the last instrumented vertebrae, correction rate of preoperative anteverted pelvis after the surgery to a normal pelvis was 100%. Whereas, they found this correctional rate to be 68% and 25% when the last instrumented vertebrae was L4 and L5 consecutively. In our study we found significant positive correctional difference in lumbar lordosis (54°–45°) and sacral slope (35.7°–29.7°) when the last instrumented vertebra changed from L3 to L4. When examined in terms of spinopelvic parameters, this surgical-related reduction in sacral slope and lumbar lordosis is compensated by an increase in the pelvic tilt. In L3 group PT was increased to 21.48° from 16.0° significantly, but in L4 group PT was not changed significantly (17.64°–17.85°). These results show that, the compensation mechanism loses magnitude when instrumentation extends to L4 vertebra. However, we found no difference when it was sought between L3 versus L5 and L4 versus L5. This we believe is a result of barely small number of patients in the subgroup in which instrumentation included L5 vertebrae. In other words, our results indicate that the further the instrumentation is advanced distal ward, the better the sagittal parameters come out. Major limitations of this study are the retrospective work, the digital measurement of the x-rays open to failure, fewer patients number in groups.22, 23
Conclusion
The clearest conclusion to be drawn from this study is that, the further the lower level vertebra is included in the spinal instrumentation, the worse the compensation mechanisms of sagittal balance gets affected, therefore we recommend the distal ward instrumentation and fusion should be avoided as much as possible to prevent sagittal compensation. It is crucial for curves including thoracolumbar/lumbar segments like Lenke type 5 patients. It is still need for a comprehensive studies that contains larger series in this issue.
Conflicts of interest
We all certify that there is no conflict of interest with any financial organization regarding the manuscript. The manuscript submitted does not contain information about medical device(s)/drug(s).
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Okan Ozkunt, Email: drdeto@gmail.com.
Gökhan Karademir, Email: dr@gokhankarademir.com.
Kerim Sariyilmaz, Email: ksariyilmaz@gmail.com.
Halil Can Gemalmaz, Email: cgemalmaz@gmail.com.
Fatih Dikici, Email: fatihdikici71@hotmail.com.
References
- 1.Legaye J., Duval-Beaupere G., Hecquet J., Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berthonnaud E., Dimnet J., Roussouly P., Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18(1):40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 3.Mac-Thiong J.M., Labelle H., Charlebois M., Huot M.P., de Guise J.A. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine (Phila Pa 1976) 2003;28(13):1404–1409. doi: 10.1097/01.BRS.0000067118.60199.D1. [DOI] [PubMed] [Google Scholar]
- 4.Upasani V.V., Tis J., Bastrom T. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976) 2007;32(12):1355–1359. doi: 10.1097/BRS.0b013e318059321d. [DOI] [PubMed] [Google Scholar]
- 5.Yang X., Liu L., Song Y. Pre- and postoperative spinopelvic sagittal balance in adolescent patients with lenke type 5 idiopathic scoliosis. Spine (Phila Pa 1976) 2015;40(2):102–108. doi: 10.1097/BRS.0000000000000685. [DOI] [PubMed] [Google Scholar]
- 6.La Maida G.A., Zottarelli L., Mineo G.V., Misaggi B. Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J. 2013;22(suppl 6):S859–S867. doi: 10.1007/s00586-013-3018-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu X.M., Wang F., Zhou X.Y. Sagittal balance in adolescent idiopathic scoliosis: a radiographic study of spinopelvic compensation after selective posterior fusion of thoracolumbar/lumbar (Lenke 5C) curves. Medicine (Baltimore) 2015;94(45):e1995. doi: 10.1097/MD.0000000000001995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clement J.L., Geoffray A., Yagoubi F. Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur Spine J. 2013;22(11):2414–2420. doi: 10.1007/s00586-013-2852-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanguay F., Mac-Thiong J.M., de Guise J.A., Labelle H. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J. 2007;16(4):531–536. doi: 10.1007/s00586-006-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mac-Thiong J.M., Berthonnaud E., Dimar J.R., 2nd, Betz R.R., Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004;29(15):1642–1647. doi: 10.1097/01.brs.0000132312.78469.7b. [DOI] [PubMed] [Google Scholar]
- 11.Roussouly P., Labelle H., Rouissi J., Bodin A. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J. 2013;22(suppl 2):S203–S215. doi: 10.1007/s00586-012-2571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrey C., Roussouly P., Le Huec J.C., D'Acunzi G., Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013;22(suppl 6):S834–S841. doi: 10.1007/s00586-013-3030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwab F., Lafage V., Patel A., Farcy J.P. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34(17):1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 14.Yong Q. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa 1976) 2012;37(12):E714–E720. doi: 10.1097/BRS.0b013e3182444402. [DOI] [PubMed] [Google Scholar]
- 15.Vaz G., Roussouly P., Berthonnaud E., Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11(1):80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lenke L.G., Betz R.R., Harms J. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am. 2001;83-A(8):1169–1181. [PubMed] [Google Scholar]
- 17.Rinella A., Bridwell K., Kim Y. Late complications of adult idiopathic scoliosis primary fusions to L4 and above: the effect of age and distal fusion level. Spine (Phila Pa 1976) 2004;29(3):318–325. doi: 10.1097/01.brs.0000111838.98892.01. [DOI] [PubMed] [Google Scholar]
- 18.Newton P.O., Yazsay P., Upasani V.V. Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35(14):1365–1370. doi: 10.1097/BRS.0b013e3181dccd63. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y., Bünger C.E., Zhang Y. Lowest instrumented vertebra selection for Lenke 5C scoliosis: a minimum 2-year radiographical follow-up. Spine (Phila Pa 1976) 2013;38(14):E894–E900. doi: 10.1097/BRS.0b013e31829537be. [DOI] [PubMed] [Google Scholar]
- 20.Li J., Hwang S.W., Shi Z. Analysis of radiographic parameters relevant to the lowest instrumented vertebrae and postoperative coronal balance in Lenke 5C patients. Spine (Phila Pa 1976) 2011;36(20):1673–1678. doi: 10.1097/BRS.0b013e3182091fba. [DOI] [PubMed] [Google Scholar]
- 21.Tao F., Shi Z., Xie Y. Determination of lowest instrumented vertebra by the location of apical vertebra in Lenke type 1 adolescent idiopathic scoliosis. Int Orthop. 2011;35(4):561–567. doi: 10.1007/s00264-010-1068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu P.P., Yu M., Liu X.G., Chen Z.Q., Liu Z.J. Correlation analysis between the sagittal and coronal parameters of spino-pelvic in Lenke type 1 adolescent idiopathic scoliosis. Beijing Da Xue Xue Bao. 2015;47(2):248–252. [PubMed] [Google Scholar]
- 23.Hu P., Yu M., Liu X. Analysis of the relationship between coronal and sagittal deformities in adolescent idiopathic scoliosis. Eur Spine J. 2016;25(2):409–416. doi: 10.1007/s00586-015-3986-y. [DOI] [PubMed] [Google Scholar]