Abstract
Objective
The aim of this study was to compare the functional and radiological outcomes of vertebroplasty and kyphoplasty in patients with osteoporotic vertebra fractures.
Methods
The files of the patients who underwent vertebroplasty or kyphoplasty for osteoporotic vertebrae fractures were retrieved from the archives. Forty-three patients with complete follow-up data were included in the study group. The patients were evaluated for radiological outcomes in terms of local kyphosis angle, wedging index, compression ratio, visual analog pain scale (VAS) and Oswestry Disability Index (ODI).
Results
In the study group, kyphoplasty was performed on 24 vertebrae of 22 patients (17 females, 5 males; mean age: 73 years) whereas vertebroplasty was applied on 24 vertebrae of 21 (16 females, 5 males; mean age: 74.7 years) patients. The mean follow-up time was 26 months. When the VAS and ODI values of the groups were analyzed, both groups showed statistically significant progress after the operation. Radiological data showed that the kyphoplasty group showed statistically significant improvement in the sagittal index values whereas the vertebroplasty group did not. The overall complication ratio was 4%.
Conclusion
Both vertebroplasty and kyphoplasty are effective treatment methods for functional recovery and pain relief in osteoporotic fractures of the vertebra. Although radiological outcomes of the kyphoplasty seem to be better, this does not have any clinical relevance. We suggest vertebroplasty over kyphoplasty since it is an easier method to manage.
Level of evidence
Level III, Therapeutic study.
Keywords: Clinical results, Functional results, Kyphoplasty, Outcomes, Radiological results, Vertebroplasty
Introduction
Osteoporosis is a disease of the bone characterized with a decrease in the bone mineral density and bone quality. It is vastly a problem of the elderly people and presents as a great public health issue.1 Vertebral body compression fractures are the most encountered type in osteoporosis patients.2 Clinically, these fractures can cause a wide range of symptoms including pain, decrease in quality of life, kyphosis which may lead to respiratory complications, immobilization due to pain, and complications of immobilization, which all may result in depression. Among these comorbidities, immobilization is known to aggravate osteoporosis.
The main goal in the treatment of osteoporotic vertebra fractures is to relieve pain, regain functions of daily living and halt the progression of osteoporosis. It is accepted that surgical interventions with implants cause frequent failures and non-union due to low bone quality in these patients. It has also been shown that morbidity and mortality risks of surgical treatment are higher in elderly patients.3, 4
Several minimally invasive techniques have emerged and gained popularity in the last decade. Vertebroplasty and kyphoplasty have proved popularity among procedures performed percutaneously. These two techniques offer a recognizable increase in quality of life in patients with an osteoporotic vertebra fracture by improving stability and thus relieving pain.
In this study, we aimed to demonstrate the functional and radiological differences of osteoporotic vertebral fracture patients treated with vertebroplasty or kyphoplasty.
Patients and methods
The archives of the Department of Orthopedics and Traumatology at the School of Medicine at Gazi University were scanned for patients who had been diagnosed with an osteoporotic vertebra fracture. Forty-three of these patients over the age of 60, had pain refractory to 4–6 weeks of conservative treatment, and those who had bone marrow edema adjacent to the fracture site on MR scans were included in the study. All patients were treated either by vertebroplasty or kyphoplasty. Patients with secondary osteoporosis (malignancy, metabolic disease, post-radiotherapy) and fractures due to high-energy traumas were excluded.
Surgical treatment was performed on 48 levels of vertebrae in 43 patients (Table 1). Kyphoplasty was performed on 24 vertebrae of 22 patients (17 females, 5 males; mean age: 73 years, range: 63–86 years) while vertebroplasty was performed on 24 vertebrae of 21 patients (16 females, 5 males; mean age: 74.7 years, range: 65–87 years). All patients were invited for final evaluation except one who had died during the follow-up period. Two other patients refused to attend the final follow-up.
Table 1.
Distribution of the patients by the type and level of surgical interventions.
| Level | Vertebroplasty | % | Kyphoplasty | % |
|---|---|---|---|---|
| L1 | 8 | 33.3 | 3 | 12.5 |
| L2 | 5 | 20.8 | 5 | 20.8 |
| L3 | 3 | 12.5 | 2 | 8.3 |
| L4 | 4 | 16.7 | 2 | 8.3 |
| L5 | 1 | 4.2 | 0 | 0 |
| T4 | 0 | 0 | 1 | 4.2 |
| T8 | 1 | 4.2 | 1 | 4.2 |
| T9 | 0 | 0 | 3 | 12.5 |
| T10 | 1 | 4.2 | 0 | 0 |
| T11 | 0 | 0 | 2 | 8.3 |
| T12 | 1 | 4.2 | 5 | 20.8 |
| Total | 24 | 100 | 24 | 100 |
Patients' age, sex, the onset time of symptoms, number of vertebral levels affected by the fracture, mechanism and type of trauma, presence of concomitant or prior fractures, medical history, medications taken currently, risk factors for osteoporosis and medications used for the treatment of osteoporosis were recorded. All patients underwent detailed physical examination including a detailed neurological assessment.
Local kyphosis angle, wedging index and compression ratio were measured from the X-rays taken before the surgical interventions (Fig. 1, Fig. 2, Fig. 3). The local kyphosis angle was measured according to the method defined by Cobb.5 DEXA was ordered for the patients who have not undergone a bone mineral density test within the past year (Table 2). Patients' pain level was assessed preoperatively using the visual analog pain scale (VAS).6
Fig. 1.
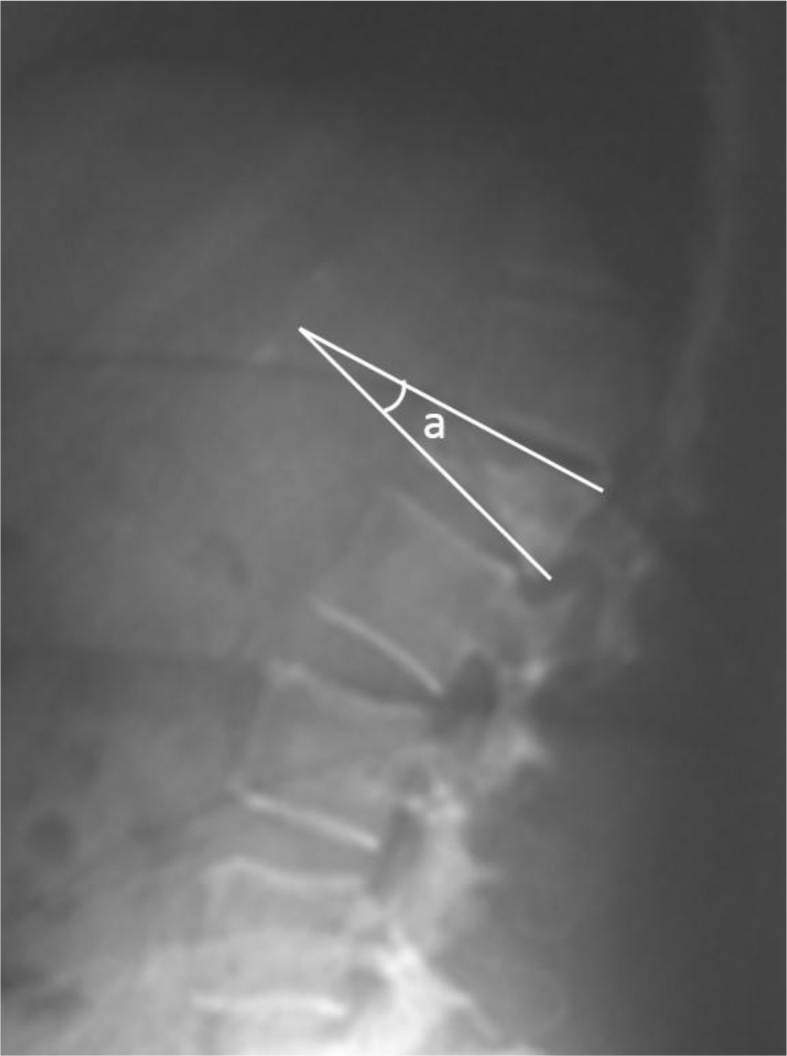
Local kyphosis angle = a.
Fig. 2.
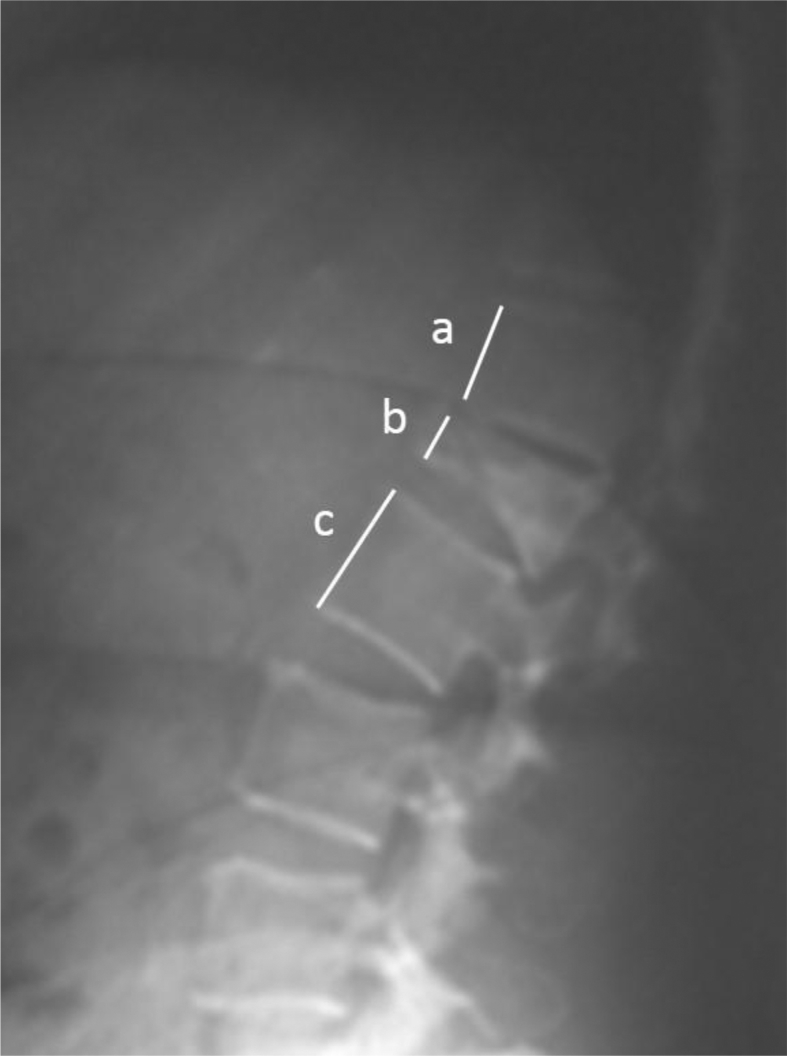
Compression ratio = ((a+c)/2)/b.
Fig. 3.
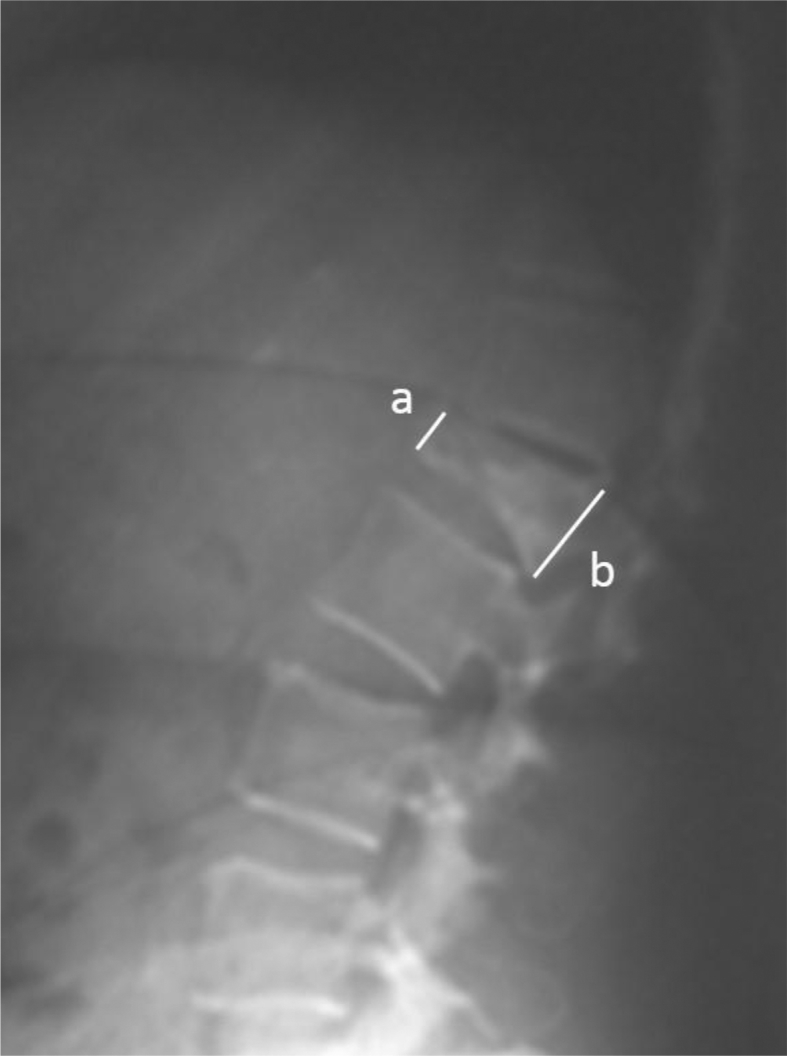
Wedging index = a/b.
Table 2.
Age, DEXA values and the amount of cement injected to the vertebrae during operations.
| Min. | Max. | Mean | SD | ||
|---|---|---|---|---|---|
| Age | Vertebroplasty | 65 | 87 | 74.7 | 6.23 |
| Kyphoplasty | 62 | 86 | 73 | 7.09 | |
| DEXA scores (T scores) | Vertebroplasty | −4.2 | −1.6 | −2.9 | 0.56 |
| Kyphoplasty | −4.54 | −1.45 | −2.8 | 0.68 | |
| Cement amount (cc) | Vertebroplasty | 3 | 7 | 4.5 | 1.1 |
| Kyphoplasty | 3 | 8 | 5 | 1.34 | |
Functional evaluation was done using the Oswestry Disability Index (ODI) version 2.0 which is a patient-reported outcome assessment questionnaire. ODI is a widely used questionnaire form that contains 10 separate sections of six questions regarding level of pain, personal care activities, weight lifting, walking activity, sitting, standing, sleeping, social life activities, transportation, and sexual activities.7, 8 In our study, all participants answered all sections except the ones related to sexual activities. Table 3 summarizes the mean values of outcome variables before and after the operations for both vertebroplasty and kyphoplasty patients.
Table 3.
Comparison of the preoperative and postoperative mean values of outcome variables between groups.
| Before vertebroplasty | After vertebroplasty | Before kyphoplasty | After kyphoplasty | |
|---|---|---|---|---|
| Local kyphosis angle (°) | 27 | 25.6 | 33.4 | 16.9 |
| Wedging index | 60.8 | 63.5 | 62.5 | 75.3 |
| Compression ratio | 61.3 | 61.5 | 64.5 | 75.8 |
| Visual analog scale score | 9 | 1.9 | 8.4 | 1.7 |
| Oswestry score | 70.9 | 26.9 | 74.3 | 29.8 |
Patients who met the above inclusion criteria were treated with the following methodology with a transpedicular approach. All vertebroplasty procedures were done under local anesthesia whereas all kyphoplasties were carried out under deep sedation or general anesthesia, plus local anesthesia as inflation of the balloon and reduction caused formidable pain. A C-arm image intensifier was used in all interventions. Both surgeries were performed using the bilateral pedicles of the corresponding vertebrae. A stab incision was performed 1 cm lateral of the bilateral pedicles and a Jamshidi needle was sent to the vertebral body. A guide was advanced inside this needle, and a working cannula was established. In kyphoplasty, the Kyphon® Balloon Kyphoplasty (Medtronic Inc., Minneapolis, MN, USA) system was utilized. The balloon was filled with radiopaque agent and inflated until desired reduction was observed under fluoroscopy. Injection of the radiopaque agent was commenced in all patients in both groups to check for possible cement leakage before application of the cement. High-viscosity bone cement (Kyphon®, HV-R®; Medtronic Inc., Minneapolis, MN, USA) was used for vertebral augmentation in both interventions. The amount of the cement injected to the vertebral body was noted for all patients (Table 2). Following the operations, all patients were kept immobile in the supine position in bed for 24 h. Then, all patients were mobilized and their VAS evaluation was repeated.9, 10 Postoperative anterior–posterior and lateral X-rays were ordered to check for complications and cement leakage before dispatch. Patients' local kyphosis angle, wedging index and compression ratio were measured once again on the X-rays obtained after surgery (Table 3).
All patients who underwent surgical procedures and did not receive a medication for osteoporosis were prescribed bisphosphonates and an active vitamin D and calcium combination. These patients were also informed about osteoporosis and its possible complications.
Patients were asked to attend the follow-up visits on the 3rd, 6th, and 12th month and every 6 months after the first year. During the follow-up visits, patients were reevaluated with physical examination, VAS and ODI and their roentgenograms were taken to reassess the radiological outcomes on the surgically treated vertebrae and the adjacent levels for any complications (Table 3).
The results were analyzed using the SPSS v.16 software. The paired-sample t-test and Pearson's correlation tests were used to analyze the VAS and ODI results and the differences in radiological readings of the groups. A p value of below 0.05 was accepted as the threshold for statistical significance.
Results
The mean preoperative T score was −2.9 (min: −4.2, max: −1.6) in vertebroplasty and −2.8 (min: −4.5, max: −1.5) in kyphoplasty patients. The mean follow-up length for both groups was 26 (range: 4 to 48) months. Analysis of the demographic and diagnostic variables showed no significant difference between vertebroplasty and kyphoplasty groups. Also, the groups had statistically significant difference in terms of their VAS and ODI scores, thus we can assume these groups to be homogenous.
In the vertebroplasty group, the mean VAS value before vertebroplasty was 9 and 1.7 on the first postoperative day. The mean VAS score at the final follow-up was 1.9. Comparison of the preoperative mean VAS values to postoperative ones showed a statistically significant difference (p < 0.05). In the kyphoplasty group, the mean VAS score was 8.4 preoperatively, 2 on the first postoperative day, and 1.7 at the final follow-up. Comparison of the preoperative mean VAS scores to the postoperative ones also showed a statistically significant difference (p < 0.05).
The mean ODI score in the vertebroplasty group was 70.9 before surgery and 26.9 at the final follow-up. The difference between the two scores showed statistical significance (p < 0.05). Likewise, a statistical difference was detected between the mean preoperative and final follow-up ODI scores (74.3 and 29.8, respectively) of the kyphoplasty group (p < 0.05).
Radiological results showed no significant difference between preoperative and post-vertebroplasty values for the local kyphosis angle, wedging index and compression ratio. On the other hand, when the radiological outcomes of kyphoplasty patients were compared, we found a statistically significant difference (p < 0.05) due to correction of deformity with the balloon application after the kyphoplasty procedure. Table 3 shows the comparison of the radiological outcomes in both groups.
There was no statistically significant difference between the vertebroplasty and kyphoplasty groups in terms of VAS and ODI scores. Both procedures showed identical results in terms of pain control and functional recovery.
As for complications, one patient (4%) from each group experienced cement leakage into the upper intervertebral disc space, which did not cause any neurological compromise. Throughout the follow-up period, one patient in the vertebroplasty group developed a compression fracture in the adjacent vertebral body, which was also treated with vertebroplasty. No adjacent vertebral compression fracture was observed in the kyphoplasty group throughout the follow-up period.
Discussion
Both vertebroplasty and kyphoplasty are known to be effective in pain relief and functional recovery. Yakut, Grados and Kaufmann et al have all shown vertebroplasty to be a very efficient treatment method in osteoporotic vertebral fractures, resulting in good pain relief, functional recovery, increased mobility, and decreased need for painkiller medications.6, 11, 12 Our study supports the findings of the mainstream literature as we also found that VAS and ODI scores have shown improvement after vertebroplasty and throughout the follow-up period. Likewise, our results regarding kyphoplasty is in accordance with the findings of previous studies which also reports good pain relief and functional recovery.13, 14
Current results showed no significant difference between vertebroplasty and kyphoplasty in terms of pain relief and functional recovery.15 The only statistically significant difference between the two groups was in the radiological outcomes. This finding is in line with most of the studies which reports kyphoplasty as a relevant treatment in osteoporotic vertebral compression fractures that improves radiological results in addition to pain-related and functional outcomes.14, 16, 17, 18
Regarding complications of the adjacent fractures, we observed only one patient with an adjacent fracture in the vertebroplasty group. This is relatively a lower rate from that in the literature; however, considering the length of the follow-up period, this may not be a substantial finding. On the other hand, our study and current literature does not answer if vertebroplasty and kyphoplasty surgeries change the odds of adjacent osteoporotic vertebra fractures. Since the literature and our study strongly suggest that these interventions improve patients' outcomes, new studies should be directed on the issue of determining if these procedures change the likelihood of developing adjacent fractures.19, 20, 21 Other important complications of these interventions include cement leakage into the intervertebral disc space and spinal canal, cement embolism to the aorta, vena cava, azygos vein and the lungs, and neurological compromise.22, 23, 24 In our study, cement leakage into the intervertebral space was observed in one patient. Theoretically, cement leakage into the potential space created by kyphoplasty could be less, however, a review of the literature showed no difference between the two procedures in terms of safety.15 Fluoroscopic control with radiopaque agent injection and introduction of cement without any pressure can reduce the cement leakage.
The strength of our study was that both radiological and functional outcomes were assessed and all procedures were performed by the same surgeon. On the other hand, the relatively short follow-up period is a weakness of our study. Other limitations were lack of homogenization for the affected and treated level of the vertebral body and randomization between the two procedures.
As a result, our study supports the current literature by demonstrating kyphoplasty and vertebroplasty as similar interventions with identical results in terms of function and pain relief. In addition, we can conclude that better radiological outcomes associated with kyphoplasty do not prove any useful clinical relevancy.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Steindler A. The classic: osteoporosis. 1956. Clin Orthop Relat Res. 2006;443:3–9. doi: 10.1097/01.blo.0000200246.45178.fe. discussion 2. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O., Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl. 2):S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 3.Jalava T., Sarna S., Pylkkänen L. Association between vertebral fracture and increased mortality in osteoporotic patients. J Bone Miner Res. 2003;18:1254–1260. doi: 10.1359/jbmr.2003.18.7.1254. [DOI] [PubMed] [Google Scholar]
- 4.Lavelle W., Carl A., Lavelle E.D., Khaleel M.A. Vertebroplasty and kyphoplasty. Med Clin North Am. 2007;91:299–314. doi: 10.1016/j.mcna.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Altun N.Ş. Torakolomber vertebra kırıklarının tedavi öncesi ve sonrası değerlendirilmesi. Artroplasti Artroskopik Cerrahi Derg. 1993;4:30–34. [Google Scholar]
- 6.Yakut Y., Yakut E., Bayar K., Uygur F. Reliability and validity of the Turkish version short-form McGill pain questionnaire in patients with rheumatoid arthritis. Clin Rheumatol. 2007;26:1083–1087. doi: 10.1007/s10067-006-0452-6. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank J.C., Pynsent P.B. The oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 8.Yakut E., Düger T., Oksüz C. Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine (Phila Pa 1976) 2004;29:581–585. doi: 10.1097/01.brs.0000113869.13209.03. discussion 585. [DOI] [PubMed] [Google Scholar]
- 9.Belkoff S.M., Mathis J.M., Jasper L.E., Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976) 2001;26:1537–1541. doi: 10.1097/00007632-200107150-00007. [DOI] [PubMed] [Google Scholar]
- 10.Deramond H., Depriester C., Toussaint P., Galibert P. Percutaneous vertebroplasty. Semin Musculoskelet Radiol. 1997;1:285–296. doi: 10.1055/s-2008-1080150. [DOI] [PubMed] [Google Scholar]
- 11.Grados F., Depriester C., Cayrolle G., Hardy N., Deramond H., Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 2000;39:1410–1414. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 12.Kaufmann T.J., Jensen M.E., Schweickert P.A., Marx W.F., Kallmes D.F. Age of fracture and clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2001;22:1860–1863. [PMC free article] [PubMed] [Google Scholar]
- 13.Garfin S.R., Yuan H.A., Reiley M.A. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman I.H., Dudeney S., Reinhardt M.K., Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2001;26:1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 15.Taylor R.S., Taylor R.J., Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine (Phila Pa 1976) 2006;31:2747–2755. doi: 10.1097/01.brs.0000244639.71656.7d. [DOI] [PubMed] [Google Scholar]
- 16.Boszczyk B.M., Bierschneider M., Schmid K., Grillhösl A., Robert B., Jaksche H. Microsurgical interlaminary vertebro- and kyphoplasty for severe osteoporotic fractures. J Neurosurg. 2004;100:32–37. doi: 10.3171/spi.2004.100.1.0032. [DOI] [PubMed] [Google Scholar]
- 17.Majd M.E., Farley S., Holt R.T. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J. 2005;5:244–255. doi: 10.1016/j.spinee.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Shedid D., Togawa D., Lieberman I.H. Kyphoplasty: vertebral augmentation for compression fractures. Clin Geriatr Med. 2006;22:535–544. doi: 10.1016/j.cger.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 19.Harrop J.S., Prpa B., Reinhardt M.K., Lieberman I. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine (Phila Pa 1976) 2004;29:2120–2125. doi: 10.1097/01.brs.0000141176.63158.8e. [DOI] [PubMed] [Google Scholar]
- 20.Lindsay R., Silverman S.L., Cooper C. Risk of new vertebral fracture in the year following a fracture. J Am Med Assoc. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 21.Uppin A.A., Hirsch J.A., Centenera L.V., Pfiefer B.A., Pazianos A.G., Choi I.S. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226:119–124. doi: 10.1148/radiol.2261011911. [DOI] [PubMed] [Google Scholar]
- 22.Lee B.J., Lee S.R., Yoo T.Y. Paraplegia as a complication of percutaneous vertebroplasty with polymethylmethacrylate: a case report. Spine. 2002;27:419–422. doi: 10.1097/00007632-200210010-00022. [DOI] [PubMed] [Google Scholar]
- 23.Lin E.P., Ekholm S., Hiwatashi A., Westesson P.L. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25:175–180. [PMC free article] [PubMed] [Google Scholar]
- 24.Padovani B., Kasriel O., Brunner P., Peretti-Viton P. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 1999;20:375–377. [PMC free article] [PubMed] [Google Scholar]


