Abstract
Objective
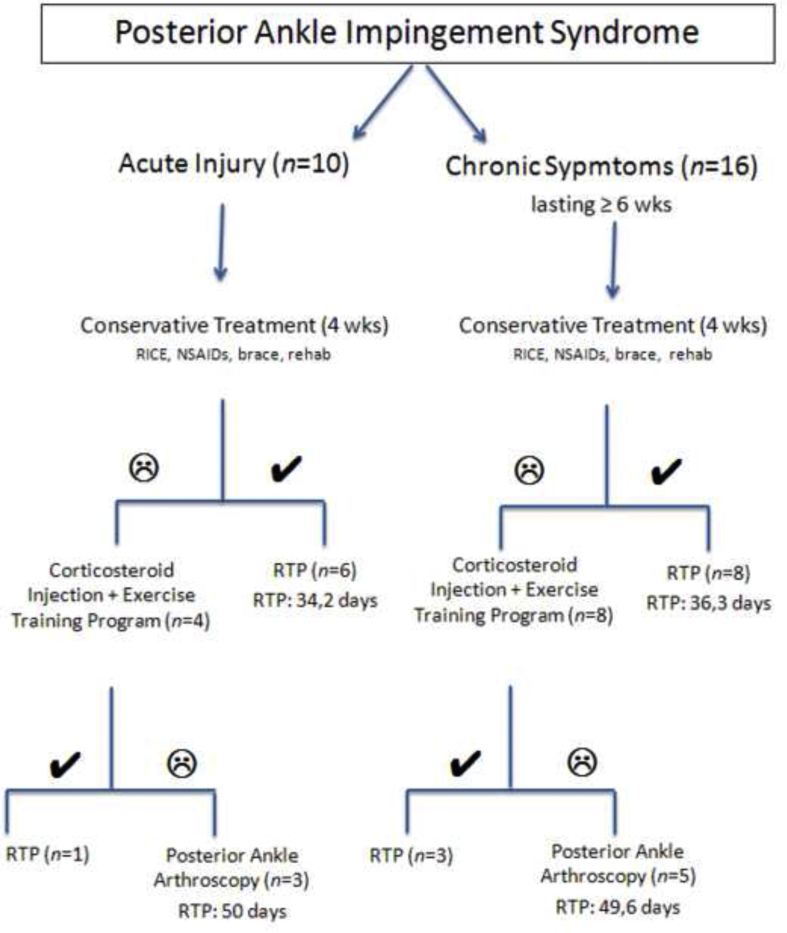
To describe a clinical treatment algorithm for posterior ankle impingement (PAI) syndrome in professional football players.
Material and methods
A case series of 26 elite professional football players diagnosed and treated for posterior ankle impingement syndrome were included for the study. All of the athletes received conservative treatment with physical therapy modalities initially. If the first line medical treatment and rehabilitation was ineffective to alleviate the symptoms, ultrasound-guided corticosteroid injection was proposed and thereafter the patients underwent posterior ankle arthroscopy if the complaints are still unresolved. The pain scores (AOFAS, VAS), and time to return to play were the main outcome measures.
Results
The complaints of 18 (69.2%) players were subsided with non-surgical treatment whereas three of acute cases and five of the chronic cases did not respond to medical treatment and arthroscopic surgery was performed for eight athletes. Eighteen players returned to training for a mean time of 36.3 days (24–42 days) after conservative treatment. The patients who underwent arthroscopic surgery returned to training for a mean time of 49.8 days (42–56 days) after the surgery. All athletes returned to their previous level of competition after treatment without any complications or recurrence in a mean follow-up 36.5 months (19–77 months).
Conclusion
Non-surgical treatment modalities were effective in 2/3 of posterior ankle impingement syndrome in elite football players. On the other hand, posterior ankle arthroscopy is safe and effective treatment option for posterior ankle impingement syndrome if the conservative treatment fails.
Level of evidence
Level IV, Therapeutic study
Keywords: Ankle, Pain, Arthroscopy, Football, Talus, Posterior ankle impingement
Introduction
Posterior ankle impingement (PAI) syndrome is increasingly being diagnosed in ballet dancers, javelin throwers and football players. It is a condition consisting of a group of pathology as a result of exposure of the foot to plantar flexion or repeated trauma.1 Patients usually experience chronic or recurrent posterior ankle pain caused or exacerbated by forced plantar flexion or push-off maneuvers, such as kicking, dribbling or bouncing in which football players usually engage. Compression of the posterior portion of the talus and surrounding soft tissues between the calcaneus and the tibia during plantar flexion results with impingement. The bony lesions such as os trigonum, fragmentation in the lateral talar tubercle and pseudoarthrosis are common cause of PAI syndrome. The accompanying pathologies in soft tissues affect the posterior joint capsule, flexor hallucis longus (FHL) tendon, posterior talofibular ligament, intermalleolar ligament and the tibiofibular ligament.2
Posterior impingement syndrome usually responds to conservative treatment. Operative treatment may be indicated when non-operative measures have failed. Surgical management involves removal of the os trigonum, scar tissue, or hypertrophic posterior talar process. If surgical debridement or excision is deemed necessary, arthroscopic surgery via a posterior approach is recommended to excise impingement lesions with a quicker return to sport expected and minimal complications.3, 4, 5 Herein, a case series of 26 professional football players diagnosed with PAI syndrome and a treatment algorithm for high-level athletes were presented.
Case series
124 professional football players who had posterior ankle pain were applied to Sports Medicine Clinic between the years of 2007 and 2012. After physical examination and imaging techniques, 26 of these athletes were diagnosed as posterior ankle impingement syndrome (Fig. 1, Fig. 2). The patients were all male, elite athletes in professional level at Turkish Super League with a mean age of 21.9 years [range 17–29 years]. Demographic and clinical characteristics of the athletes are given in Table 1.
Fig. 1.

Lateral radiograph of a 19 year-old football player with a 3-year professional background, showing a free bone structure belonging to os trigonum in talus posterior.
Fig. 2.
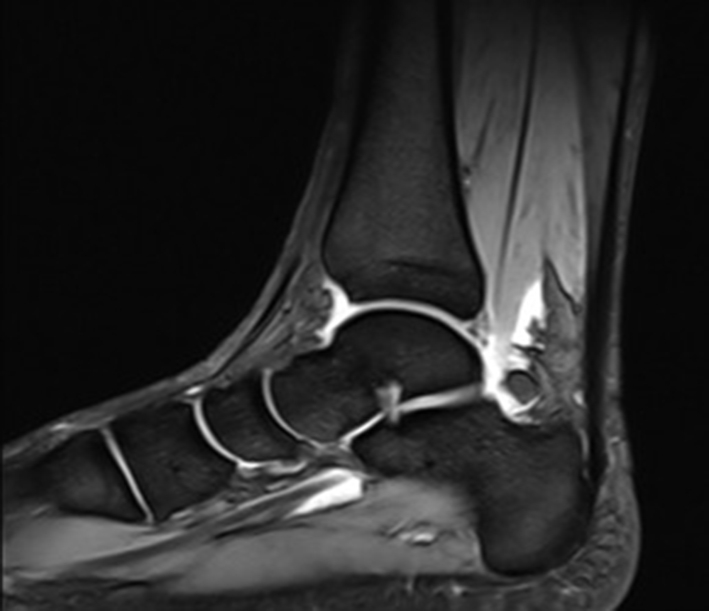
Effusion is seen around os trigonum in T2W sagittal image of the ankle MRI.
Table 1.
Data collected for the present study.
| Age | Dominant foot | Injured foot | Duration of symptoms (weeks) | FHL synovitis | Talar oedema | Tibiotalar synovitis | Subtalar synovitis | Treatment | AOFAS score |
AOFAS score after 4 weeks | AOFAS score final | VAS |
VAS after 4 weeks | VAS final | Return to sports | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Pre-treatment | |||||||||||||||
| 20 | Right | Right | 3 weeks | Yes | Yes | – | – | Cons. | 78 | 100 | 100 | 6 | 0 | 0 | 34 | 19 |
| 24 | Right | Right | 3 weeks | Yes | – | – | Yes | Cons. | 59 | 98 | 98 | 8 | 1 | 1 | 41 | 38 |
| 19 | Left | Left | 2 weeks | Yes | – | – | – | Cons. | 73 | 100 | 100 | 6 | 0 | 0 | 30 | 32 |
| 23 | Right | Right | 2 weeks | Yes | Yes | – | – | Cons. | 62 | 100 | 100 | 7 | 0 | 0 | 40 | 41 |
| 21 | Right | Right | 4 weeks | Yes | Yes | Yes | Yes | Cons. | 82 | 100 | 100 | 6 | 0 | 0 | 36 | 26 |
| 21 | Right | Right | 4 weeks | Yes | – | – | – | Cons. | 87 | 100 | 100 | 5 | 0 | 0 | 24 | 52 |
| 21 | Right | Right | 2 weeks | Yes | Yes | – | – | Cons. + Inj | 67 | 73 | 98 | 8 | 4 | 0 | 42 | 31 |
| 29 | Right | Right | 2 weeks | Yes | – | Yes | Yes | Surgery | 53 | 63 | 97 | 8 | 6 | 1 | 49 | 21 |
| 26 | Right | Right | 1 week | Yes | Yes | Yes | Yes | Surgery | 49 | 67 | 95 | 10 | 6 | 2 | 53 | 42 |
| 21 | Right | Right | 1 week | Yes | Yes | Yes | Yes | Surgery | 71 | 75 | 100 | 8 | 5 | 0 | 48 | 46 |
| 19 | Right | Right | 6 weeks | Yes | Yes | Yes | Yes | Cons. | 66 | 100 | 100 | 7 | 1 | 1 | 35 | 51 |
| 25 | Right | Right | 6 weeks | Yes | – | – | Yes | Cons. | 62 | 100 | 100 | 6 | 0 | 0 | 36 | 77 |
| 26 | Right | Right | 7 weeks | Yes | – | – | Yes | Cons. | 73 | 100 | 100 | 6 | 0 | 0 | 41 | 24 |
| 19 | Right | Right | 7 weeks | – | Yes | – | Yes | Cons. | 67 | 100 | 100 | 6 | 0 | 0 | 40 | 36 |
| 17 | Right | Right | 8 weeks | Yes | – | – | Yes | Cons. | 87 | 100 | 100 | 5 | 0 | 0 | 33 | 62 |
| 24 | Right | Right | 9 weeks | Yes | – | Yes | Yes | Cons. | 71 | 100 | 100 | 6 | 0 | 0 | 29 | 25 |
| 23 | Left | Left | 9 weeks | Yes | – | Yes | Yes | Cons. | 71 | 100 | 100 | 7 | 0 | 0 | 36 | 32 |
| 21 | Right | Left | 10 weeks | – | – | Yes | – | Cons. | 57 | 100 | 100 | 6 | 1 | 1 | 40 | 37 |
| 21 | Right | Left | 6 weeks | – | – | Yes | Yes | Cons. + Inj | 73 | 77 | 100 | 7 | 4 | 0 | 39 | 28 |
| 20 | Left | Left | 12 weeks | – | – | Yes | – | Cons. + Inj | 62 | 75 | 97 | 8 | 5 | 1 | 39 | 31 |
| 20 | Left | Left | 12 weeks | – | Yes | Yes | – | Cons. + Inj | 69 | 79 | 100 | 7 | 4 | 0 | 38 | 34 |
| 19 | Right | Left | 6 weeks | – | Yes | Yes | Yes | Surgery | 45 | 62 | 92 | 10 | 6 | 2 | 53 | 33 |
| 21 | Right | Right | 6 weeks | Yes | – | – | Yes | Surgery | 73 | 75 | 96 | 7 | 5 | 1 | 42 | 46 |
| 18 | Left | Left | 6 weeks | Yes | – | – | Yes | Surgery | 61 | 69 | 90 | 8 | 5 | 2 | 46 | 21 |
| 24 | Left | Left | 7 weeks | – | Yes | Yes | Yes | Surgery | 57 | 67 | 98 | 9 | 6 | 1 | 51 | 29 |
| 27 | Left | Left | 12 weeks | Yes | Yes | Yes | Yes | Surgery | 67 | 72 | 100 | 8 | 4 | 0 | 56 | 35 |
Abbreviations: FHL, flexor hallucis longus; Cons, conservative; Inj, injection; AOFAS, American Orthopaedic Foot and Ankle Society; VAS, visual analogue scale.
Ten of 26 athletes (mean age: 22.5) were admitted with posterior ankle pain after an acute ankle sprain injury and the rest declared complaints of chronic posterior ankle pain at least 6 weeks. The physical examination of patients (n = 10) after ankle sprain demonstrated tenderness on the anterior talofibular ligament (ATFL) adhesion-site, limited ankle range of motion, swelling and posterior ankle pain aggravated with forced plantar flexion. All patients were examined with X-Ray and magnetic resonance imaging (MRI). Complete tear of ATFL was observed in 2 patients and talar bone marrow edema was found in 6 patients. FHL tendon synovitis and os trigonum was depicted in all patients. Initial treatment of ankle sprain injuries was performed with modification of sports activity, RICE protocol, anti-inflammatory drugs, supportive brace (to limit plantar flexion), physical therapy and sports-specific rehabilitation program. Following four weeks of conservative treatment all patients were examined and the complaints of 6 players were subsided. The mean American Orthopaedic Foot and Ankle Society (AOFAS) score was improved to 87.6 (63–100) from 73.5 (59–87) and visual analogue scale (VAS) was decreased to 2.2 (0–6) from 6.3 (5–8). Therefore, five players were participated in team training and returned to sports at a mean time of 34.2 days (24–41 days) of injury. Four patients who have failed with conservative treatment were applied single dose of methyl prednisone acetate injection combined with local anesthesia to the area of maximal tenderness through a lateral approach under ultrasonographic (USG) guidance. A single infiltration was performed on these patients as no improvement was observed for three players after two weeks and therefore surgical repair was the proposed treatment.
All patients were operated by the same surgical team under spinal anesthesia in prone position by applying the tourniquet to the thigh. Superficial anatomical landmarks of heel were marked with a skin pen in all cases prior to the surgery. A stab incision was performed for posterolateral portal between the lateral border of the Achilles tendon and the posterior surfaces of the peroneal tendons in the border of superior surface of the calcaneus with preserving the sural nerve and small saphenous vein. The ankle was approached through standard posteromedial portals between the FHL and the medial border of the Achilles tendon at the same level. A 4.0-mm 30° arthroscope was used. Portals were extended through joint with a blunt obturator. The obturator and the posterior facet of the subtalar joint were detected via application of inversion and eversion to the foot. Posterior aspect of the subtalar joint could be visualized by dissection of soft tissues around the talus with the help of a motorized shaver. Capsulotomy was performed until all the necessary anatomical structures were visualized. Talus and the os trigonum have been viewed in terms of separation or fibrous synchondrosis (Fig. 3). FHL was evaluated for synovitis in terms of proximity to os trigonum. The talar process was removed with a burr until the impingement disappeared after removing the fibers attached to the fibrous tunnel around the posterior tibiotalar ligament, posterior talocalcaneal ligament, and the FHL (Fig. 4). In the presence of non-eligible os trigonum synchondrosis was detached with a small osteotome after removing all the soft tissues and the bone was excised. The operation was completed once the entire residual debris or bone fragments were checked. Portals were sutured primarily with 4.0 prolene and compressive elastic bandage was applied.
Fig. 3.
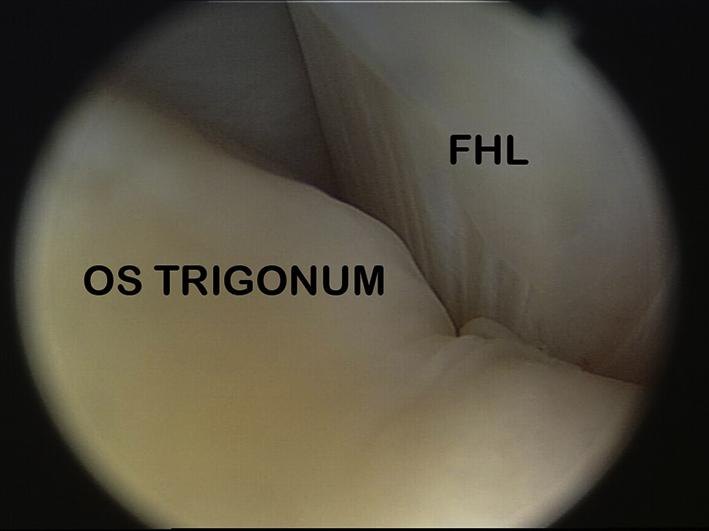
Imaging of FHL and os trigonum during posterior ankle arthroscopy.
Fig. 4.
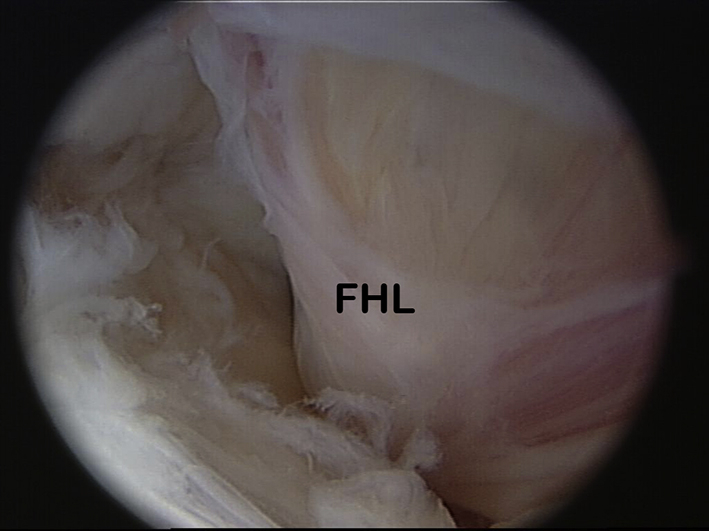
FHL tendon after os trigonum excision.
Partial weight-bearing with crutches was allowed from the first day with crutches and non-steroidal anti-inflammatory drugs were used for 7–10 days to reduce pain and inflammation after surgery. Range of motion exercises were permitted for the first postoperative day and cold application was performed for initial 5 days. Thereafter, in the clinical examination if swelling and tenderness disappeared, the exercise was done with body weight. Patients were allowed for sportive activities after second week, starting with bicycle and swimming; running was initiated in the third week. At the third week proprioceptive exercises were added to sportive rehabilitation. Athletes were allowed for sports specific field exercises at the postoperative fifth week. Preoperative posterior ankle pain of the athletes disappeared completely after surgery, and the three players returned to sports in 50 days (48–53 days) postoperatively. AOFAS showed a mean pre-treatment score of 57.7, whereas postoperative AOFAS increased to 97.3 (95–100). Final pain scores of operated athletes were 1.0 for VAS (8.7 initial score) after a mean follow-up of 36.3 months (21–46 months).
Sixteen patients (mean age: 21.5 years) who had chronic posterior ankle pain (longer than 6 weeks) were also evaluated. MRI depicted talar bone edema in 6 patients and pseudoarthrosis in the lateral talar tubercle in a patient. Tibiotalar synovitis was observed in 10 patients, FHL synovitis in 9 patients and subtalar synovitis in 6 patients. Os trigonum was prominent for all patients. Major complaint of all patients was hindfoot pain produced with forced plantar flexion when kicking the ball. The similar conservative treatment protocol with the acute PAI syndrome patients was performed initially; RICE protocol, non-steroidal anti-inflammatory drugs, supportive brace and sports-specific rehabilitation program. Clinical symptoms were subsided in half of the patients with conservative treatment after four weeks. The mean AOFAS score was improved to 86.0 (62–100) from 66.3 (45–87) and VAS was decreased to 2.6 (0–6) from 7.1 (5–10). The mean time for return to sports was 36.3 days for eight players who felt better after conservative treatment. As is in acute cases USG-guided corticosteroid injection was applied to 8 patients who had failed the initial medical treatment. Control examination after 2 weeks of corticosteroid injection three patients were free of symptoms and the surgical treatment was planned for five patients having ongoing complaints. The athletes returned to previous activity level without any pain in a mean time of 49.6 days. The mean AOFAS score was improved to 95.2 (90–100) from 60.6 (45–73) and VAS was decreased to 1.2 (0–2) from 8.4 (7–10). No severe complications, such as infection, complex regional pain syndrome, or sural or tibial nerve injuries were registered in the present series after surgery with a mean follow-up 32.8 months.
Discussion
Posterior ankle impingement syndrome is a common clinical disorder in football players resulting from repetitive subclinical trauma due to overuse injuries.6 To our best knowledge there is a lack of prospective studies on the natural history of this condition and the outcomes of conservative treatment.7 The present clinical case series revealed our treatment algorithm in professional football players who were diagnosed with posterior ankle impingement syndrome (Table 2). The principal finding of this study was that acute and chronic cases of PAI syndrome showed no difference about return to play time. In addition, corticosteroid injection seems ineffective in almost two thirds of cases after conservative treatment doesn't alleviate the symptoms. Posterior ankle arthroscopy should be considered as the prior option than corticosteroid injection if initial conservative treatment fails in such cases.
Table 2.
Our treatment algorithm for professional athletes in PAI syndrome (RTP: return to play).
Within football players, the ankle is submitted to a great variety of biomechanical chronic forces when jumping, spinning around, or kicking a ball.8, 9 When a football player attempts to force the foot into plantar flexion for instep kicking, the os trigonum or the Stieda's process may be impinged between the calcaneus and the posterior edge of the tibia and causing PAI syndrome. Os trigonum was depicted with imaging in our all patients having PAI syndrome as underlying predisposing factor. In addition, FHL tenosynovitis was seen in 19 patients (73.1%) whereas tibiotalar synovitis was present in 14 patients (53.8%) accompanying with os trigonum.
The main symptom is usually an impingement pain and tenderness localized at the posterolateral aspect of the ankle behind the peroneal tendons. The pain may be acute as a result of trauma or chronic from repetitive stress. Most of our patients admitted with chronic pain lasting more than 6 weeks (61.5%) and commonly dominant ankle was affected (88.5%). Conventional radiography is usually the first imaging technique performed and allows assessment of any potential bone abnormality, particularly in posterior impingement. The evidence of osteophytes, exostosis and presence of the os trigonum on plain films make clinical diagnosis easy in posterior bone impingement.10 MRI always adds important information about chondral or subchondral bone injuries, synovial reaction and adjacent soft tissue involvement. Bone contusions of the lateral talar tubercle, synovial thickening with irregular contours and os trigonum are usually prevalent MR imaging findings.11 Peace et al reported that high T2 signal posterior to the talocalcaneal joint indicating synovitis is the most common imaging feature of PAI syndrome.12 In our case series, all patients with PAI syndrome have been identified as having os trigonum and synovitis (FHL, tibiotalar or subtalar). Since the close proximity of FHL tendon to os trigonum, FHL tenosynovitis is quite common in the posterior impingement syndrome and FHL tenosynovitis was identified almost three fourth of our patients.
Posterior ankle impingement syndrome usually responds to conservative treatment. Pain control and achievement in plantar flexion mechanism with exercise therapy and rehabilitation can be obtained via first line therapy. During the rehabilitation process reducing the activity of the gastrocnemius muscle, deep ankle muscle strengthening exercises and proprioceptive exercises may alleviate the symptoms.13 Dry needling with physical therapy was suggested to accelerate healing via improving blood flow to injured area and collecting local inflammatory mediators to the region.14 In agreement with reported studies the symptoms of almost two thirds of our patients relieved with non-surgical treatment methods.15 The mean return to sports time period was reported 35.4 days (24–41) for all patients. Imaging-guided injection techniques can be used in the management of impingement for pain ablation and to aid clinical diagnosis, especially in hindfoot pain. Corticosteroid and anesthetic injection into a posterolateral capsule abnormality in athletes with clinical posterior impingement with ultrasonography guidance showed good results and rapid return to athletic activity in football players.16, 17 USG-guided corticosteroid injection for 12 patients who did not experience any improvement or even worsen with conservative treatment after 4 weeks was performed. However, symptomatic relief with corticosteroid injection was significantly lower in our group compared with the previous studies.
Operative treatment may be indicated when nonoperative measures have failed. Traditionally, operative treatment involves an open approach; however, more recently posterior ankle arthroscopy has been employed. Bony avulsion fragment from the posterior ankle ligament complex causing impingement should be removed.18 Excision of an os trigonum or a prominent lateral posterior process of the talus, together with release of the FHL tendon sheath was described as surgical treatment methods.19 Endoscopic management is associated with a low morbidity, a short recovery time, and provides good/excellent results at 2–5 years follow-up in 80% of patients.20 Arthroscopic resection of the os trigonum is an advanced procedure that requires an experienced specialist and the surgeon should be aware of posterolateral sural nerve damage.21 Recently, excellent results with arthroscopic surgical resection of the os trigonum via posterior approach in 20 football players having PAI syndrome was reported.8 Time to return to sports activity at a pre-injury level was declared a mean period of 46.9 days from the surgery day until the patient achieved the pre-injury Tegner activity level. Calder et al preferred posterior ankle arthroscopy in professional football players having PAI syndrome and reported the mean length of time to return to training postoperatively as 34 days and return to playing for 41 days (range 29–72 days).22 They found that the duration of symptoms before surgery and excision of bony impingement was significantly correlated with the time to return to training and playing. In our clinical series, the athletes participated the previous level of sports activity with arthroscopic debridement and excision of the os trigonum after an average 49.8 days similar with the previous studies.8, 22 On the other hand, we found no correlation between the duration of symptoms before surgery and time to return to sports. Scholten et al reported median time to return to work and getting involved in sports activities was two and eight weeks, respectively in 55 patients with posterior ankle impingement treated with an endoscopic removal of bone fragments and/or scar tissue.23 Patients treated for posterior ankle impingement caused by overuse have better results (AOFAS hindfoot scores and Likert Scale) than those treated following trauma.23 Noguchi et al operated 12 athletes arthroscopically and stated average period to return to sports as 5.9 weeks with improved AOFAS ankle-hindfoot score from 68.0 to 98.3 points.24 In accordance with these reports, Jourdel et al proposed excellent results in PAI syndrome patients treated surgically.25 The unique study reporting longer average time to return to sports with posterior ankle arthroscopy for hindfoot impingement was done by Willits et al as 5,8 months (range 1–24 months).26
In conclusion, correct diagnosis and treatment are essential in professional athletes with posterior impingement syndrome. It should be stated that conservative treatment often resolves the problem. The complaints of eighteen patients in present case series (69.2%) were subsided without any surgical intervention that was in accordance with the previous literature.14 After failing at appropriate non-operative treatment, surgical excision of the bony involvement can relieve symptoms and allow a return to full pre-injury activities. Arthroscopic treatment for posterior ankle bony impingement syndrome is minimally invasive and suitable for athletes who desire an early return to sports activity.4, 5, 27
Conflict of interest
No conflict of interest was declared by the authors.
References
- 1.Hess G.W. Ankle impingement syndromes: a review of etiology and related implications. Foot Ankle Spec. 2011;4(5):290–297. doi: 10.1177/1938640011412944. [DOI] [PubMed] [Google Scholar]
- 2.Russell J.A., Kruse D.W., Koutedakis Y., McEwan I.M., Wyon M.A. Pathoanatomy of posterior ankle impingement in ballet dancers. Clin Anat. 2010;23(6):613–621. doi: 10.1002/ca.20991. [DOI] [PubMed] [Google Scholar]
- 3.Roche A.J., Calder J.D., Lloyd Williams R. Posterior ankle impingement in dancers and athletes. Foot Ankle Clin. 2013;18(2):301–318. doi: 10.1016/j.fcl.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Zwiers R., Wiegerinck J.I., Murawski C.D., Smyth N.A., Kennedy J.G., van Dijk C.N. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29(7):1263–1270. doi: 10.1016/j.arthro.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 5.Smyth N.A., Murawski C.D., Levine D.S., Kennedy J.G. Hindfoot arthroscopic surgery for posterior ankle impingement: a systematic surgical approach and case series. Am J Sports Med. 2013;41(8):1869–1876. doi: 10.1177/0363546513489489. [DOI] [PubMed] [Google Scholar]
- 6.Giannini S., Buda R., Mosca M., Parma A., Di Caprio F. Posterior ankle impingement. Foot Ankle Int. 2013;34(3):459–465. doi: 10.1177/1071100713477609. [DOI] [PubMed] [Google Scholar]
- 7.Ribbans W.J., Ribbans H.A., Cruickshank J.A., Wood E.V. The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg. 2015;21(1):1–10. doi: 10.1016/j.fas.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 8.López Valerio V., Seijas R., Alvarez P. Endoscopic repair of posterior ankle impingement syndrome due to os trigonum in soccer players. Foot Ankle Int. 2015;36(1):70–74. doi: 10.1177/1071100714552078. [DOI] [PubMed] [Google Scholar]
- 9.Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13(6):365–371. doi: 10.5435/00124635-200510000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Russo A., Zappia M., Reginelli A. Ankle impingement: a review of multimodality imaging approach. Musculoskelet Surg. 2013;97(Suppl. 2):S161–S168. doi: 10.1007/s12306-013-0286-8. [DOI] [PubMed] [Google Scholar]
- 11.Bureau N.J., Cardinal E., Hobden R., Aubin B. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215(2):497–503. doi: 10.1148/radiology.215.2.r00ma01497. [DOI] [PubMed] [Google Scholar]
- 12.Peace K.A., Hillier J.C., Hulme A., Healy J.C. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59(11):1025–1033. doi: 10.1016/j.crad.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Albisetti W., Ometti M., Pascale V., De Bartolomeo O. Clinical evaluation and treatment of posterior impingement in dancers. Am J Phys Med Rehabil. 2009;88:349–354. doi: 10.1097/PHM.0b013e31817fa31d. [DOI] [PubMed] [Google Scholar]
- 14.Speed C.A. Injection therapies for soft-tissue disorders. Rest Pract Res Clin Rheumatol. 2003;17:167–181. doi: 10.1016/s1521-6942(02)00122-5. [DOI] [PubMed] [Google Scholar]
- 15.Marumoto J.M., Ferkel R.D. Arthroscopic excision of the os trigonum: a new technique with preliminary clinical results. Foot Ankle Int. 1997;18(12):777–784. doi: 10.1177/107110079701801205. [DOI] [PubMed] [Google Scholar]
- 16.Mouhsine E., Crevoisier X., Leyvraz P.F., Akiki A., Dutoit M., Garofalo R. Post-traumatic overload or acute syndrome of the os trigonum: a possible cause of posterior ankle impingement. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):250–253. doi: 10.1007/s00167-003-0465-5. [DOI] [PubMed] [Google Scholar]
- 17.Robinson P., Bollen S.R. Posterior ankle impingement in professional soccer players: effectiveness of sonographically guided therapy. Am J Roentgenol. 2006;187(1):W53–W58. doi: 10.2214/AJR.05.0614. [DOI] [PubMed] [Google Scholar]
- 18.Lee K.B., Kim K.H., Lee J.J. Posterior arthroscopic excision of bilateral posterior bony impingement syndrome of the ankle: a case report. Knee Surg Sports Traumatol Arthrosc. 2008;16(4):396–399. doi: 10.1007/s00167-008-0491-4. [DOI] [PubMed] [Google Scholar]
- 19.Wredmark T., Carlstedt C.A., Bauer H., Saartok T. Os trigonum syndrome: a clinical entity in ballet dancers. Foot Ankle. 1991;11(6):404–406. doi: 10.1177/107110079101100613. [DOI] [PubMed] [Google Scholar]
- 20.van Dijk C.N. Anterior and posterior ankle impingement. Foot Ankle Clin. 2006;11(3):663–683. doi: 10.1016/j.fcl.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Ogut T., Ayhan E., Irgit K., Sarikaya A.I. Endoscopic treatment of posterior ankle pain. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1355–1361. doi: 10.1007/s00167-011-1428-x. [DOI] [PubMed] [Google Scholar]
- 22.Calder J.D., Sexton S.A., Pearce C.J. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120–124. doi: 10.1177/0363546509346390. [DOI] [PubMed] [Google Scholar]
- 23.Scholten P.E., Sierevelt I.N., van Dijk C.N. Hindfoot endoscopy for posterior ankle impingement. J Bone Jt Surg Am. 2008;90(12):2665–2672. doi: 10.2106/JBJS.F.00188. [DOI] [PubMed] [Google Scholar]
- 24.Noguchi H., Ishii Y., Takeda M., Hasegawa A., Monden S., Takagishi K. Arthroscopic excision of posterior ankle bony impingement for early return to the field: short-term results. Foot Ankle Int. 2010;31(5):398–403. doi: 10.3113/FAI.2010.0398. [DOI] [PubMed] [Google Scholar]
- 25.Jourdel F., Tourné Y., Saragaglia D. Posterior ankle impingement syndrome: a retrospective study in 21 cases treated surgically. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(3):239–247. doi: 10.1016/s0035-1040(05)84310-7. [Article in French] [DOI] [PubMed] [Google Scholar]
- 26.Willits K., Sonneveld H., Amendola A., Giffin J.R., Griffin S., Fowler P.J. Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy. 2008;24(2):196–202. doi: 10.1016/j.arthro.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 27.Vilá J., Vega J., Mellado M., Ramazzini R., Golanó P. Hindfoot endoscopy for the treatment of posterior ankle impingement syndrome: a safe and reproducible technique. Foot Ankle Surg. 2014;20(3):174–179. doi: 10.1016/j.fas.2014.03.002. [DOI] [PubMed] [Google Scholar]