Abstract
Objective
The aim of this study was to compare clinical outcomes of patients with femoral neck fractures treated with the dynamic hip system blade (DHS-BLADE) or cannulated compression screws.
Methods
Eighty-six patients with femoral neck fractures were treated by closed reduction internal fixation with a DHS-BLADE (n = 42; 18 males and 24 females; mean age: 56.3 years (37–87)) or cannulated compression screws (n = 44; 20 males and 24 females; mean age: 53.8 years (26–83)) between March 2011 and August 2013. The groups were compared with Harris hip score, operation time, surgical blood loss, incision size, hospital stay, and related complications.
Results
The average follow-up time was 27 months (range, 24–36 months). There was no significant difference for the operation time, incision size, hospital stay, and Harris hip score between the groups. Also, no statistically significant differences in the rates of nonunion (4.5% vs. 0) and avascular necrosis of the femoral head (9.1% vs. 7.1%) were observed. However, the screw group experienced significantly less surgical blood loss (32.4 ± 24.7 ml) than the blade group (87.2 ± 46.6 ml; P = 0.041). The incidence of femoral neck shortening above 10 mm in the screw group was significantly higher than that in the blade group (15.9% vs. 2.4%, P = 0.031). The blade group had a significantly lower incidence of screw migration than the screw group (4.8% vs. 22.7%, P = 0.016).
Conclusion
The DHS-BLADE and cannulated compression screws might be equally effective in terms of postoperative fracture union. However, the DHS-BLADE has advantages over cannulated compression screws for preventing femoral neck shortening, screw migration, and cut-out.
Level of evidence
Level III, Therapeutic study.
Keywords: Femoral neck fracture, Cannulated screw, Dynamic hip system blade, Internal fixation
Introduction
The incidence of femoral neck fracture, accounting for 3.6% of all fractures and 53–56% of hip fractures,1, 2 is increasing worldwide together with the trend of population aging.1, 2 Numerous surgical techniques and implants have been developed and used for the treatment of femoral neck fracture, including the dynamic hip system blade (DHS-BLADE) and cannulated compression screw. However, a clear consensus has not been reached regarding which fixation technique can be used as the optimal management.
Cannulated compression screws are one of the most commonly used implants for the treatment of a fractured femoral neck, but are weak in terms of anchorage and holding, especially in patients with osteoporosis.3 Loosening of the cannulated compression screws and compression of the fracture site can lead to femoral neck shortening and compromised hip function. Conversely, the DHS-BLADE is a newly developed implant that has many advantages over the cannulated compression screw in terms of anti-rotation, cut-out, and anchorage.4 Compared with the lag screw, the helical blade design provides enhanced anchorage and rotational stability to the fractures and does not require removal of additional bone, which decreases the incidence of implant cut-out and improves the chances of good clinical outcomes.5, 6 Unlike the DHS, the DHS-BLADE, which is inserted into the cancellous bone by the force of hammer strikes, is also superior to screw fixation in the femoral head, as proven by biomechanical studies.7, 8 Also, free rotation of the femoral head can be locked after implanting the DHS blade. Additionally, the efficacy of the DHS-BLADE in the fixation of intertrochanteric fractures has been well established,9 but its use in femoral neck fractures has rarely been reported.10
Therefore, in the present study, based on the aforementioned considerations, we retrospectively evaluated the clinical results of femoral neck fractures surgically treated by internal fixation with either a DHS-BLADE or cannulated compression screws.
Materials and methods
Patients
During the period between March 2011 and August 2013, a total of 86 patients with femoral neck fracture who underwent internal fixation with a DHS-BLADE (depuy&synthes) or cannulated compression screws (depuy&synthes) were selected and included in our retrospective study. Patient age ranged from 26 to 83 years, with a mean age of 53.8 years. The inclusion criteria were as follows: 1) closed femoral neck fracture; 2) no fractures at other sites; 3) surgical treatment with cannulated compression screws or DHS-BLADE; and 4) follow-up time greater than 2 years. The exclusion criteria included: the presence of a pathological femoral neck fracture, previous femoral neck fracture, and surgical treatment with open reduction.
Based on the internal fixation devices used, the 86 patients were divided into two groups: 42 patients who underwent internal fixation with a DHS-BLADE formed the blade group and 44 patients who underwent internal fixation with cannulated compression screws formed the screw group. The Cannulated Screw group included 44 cases, 20 cases of which were male, 24 cases female. The age ranged from 26 to 83 years old, with an average 53.8 years old. According to Garden Classification, 20 cases belong to Type II, 16 cases Type III and 8 cases Type IV. The DHS-Blade group included 42 cases, 18 cases of which were male, 24 cases female. The age ranged from 37 to 87 years old, with an average 56.3 years old. And 24 cases belong to Type II, 13 cases Type III and 5 cases Type IV. The blade group and screw group included 14 and 16 patients with osteoporosis, respectively. This study was approved by the Ethics Committee of our hospital. All operations were performed by the same senior orthopedic surgeon in our department, and the mean time from trauma to surgical intervention (trauma-surgery interval) was 5 days.
Surgical procedures
For the blade group, the patients were in the supine position on a traction table after administration of general anesthesia. After femoral neck fracture reduction under C-arm control without capsulotomy, a guide pin was inserted into the femoral neck with a 135° angle guide. From the entrance point of the guide pin, a 4–5 cm skin incision was made distally to expose the lateral cortex of the femoral shaft. The length of the DHS-blade was determined to be 10 mm, which was shorter than the guide pin. We reamed the femoral shaft along the direction of the guide pin, and then the tip of the blade was positioned about 5–10 mm beneath the surface of the femoral cartilage. The side plates were placed closely to the bone surface and fixed with two locking screws. Finally, the screw caps and the blade were fastened.
For the screw group, closed reduction was performed under general anesthesia for patients in the supine position followed by percutaneous fixation with three cannulated compression screws. A guide pin was inserted with a lateral entry point at the median line of the lateral cortex, inferior to the greater trochanter. In the anterior view, the guide pin was adjusted to be parallel to the neck-shaft angle and very near to the medial-inferior cortex of the femoral neck. In the lateral view, the guide pin was adjusted to be parallel to the anteversion angle and inserted directly in the center of the femoral head and neck. The head of the guide pin was positioned about 5 mm beneath the surface of the femoral head cartilage. Then a parallel device was located on the guide pin. Using the same method, another two guide pins were inserted superior to the first guide pin, parallel to the long axis of the femoral neck. The three guide pins formed an inverted triangle. Subsequently, the 7.5 mm cannulated compression screws were inserted along the guide pins with removing the guide pins.
Perioperative management
Low molecular heparin was administered subcutaneously to prevent deep vein thrombosis for a mean of 1 week after operation. Rivaroxaban was used as prophylaxis instead of low molecular heparin and continued for 35 days postoperatively. As early as 24 h postoperatively, patients were encouraged to sit on the bed and exercise lower limb muscle. From postoperative day 3, patients were instructed to ambulate along the bed. Weight bearing was started from 20 kg at postoperative 4–6 weeks with an incremental increase of 5 kg per week.
Outcome measurement
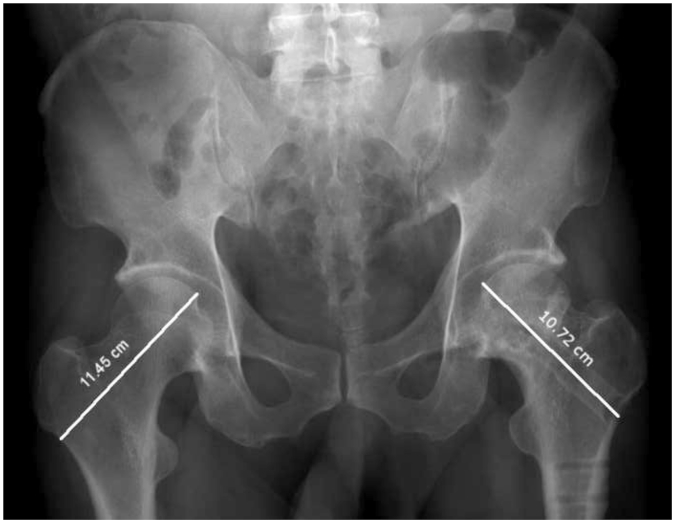
All clinical data for operative time, incision size, surgical blood loss, and hospital stay were recorded. It should be noted that the estimation of surgical blood loss involved estimating the amount of blood on the surgical gowns and drapes, in addition to weighing the sponges and estimating blood loss through suction drainage systems.12, 13 Complications were monitored, including femoral neck shortening, screw-exit, cut-out, nonunion, and avascular necrosis. Femoral neck shortening was evaluated in the vertical plane (femur length decrease) (Fig. 1), which was categorized into four degrees: degree 0 (less than 5 mm shortening); degree 1 (5–10 mm shortening); degree 2 (10–20 shortening); and degree 3 (≥20 mm shortening).14, 15 Hip function was evaluated using the Harris hip score.16, 17 The results were categorized as excellent (90–100), good (80–89), fair (70–79), and poor (≤69). Patients were followed up at 3-month intervals for 2 years.
Fig. 1.
A line was drawn from the rotation center of the femoral head through the center of the femoral neck. The distance from the femoral head cartilage to the greater trochanter cortex was measured. Any difference between the injured and the uninjured side was considered indicative of femoral neck shortening.
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD) and analyzed using Student's t-test. Categorical data were analyzed using χ2 test. Statistical analyses were performed with SPSS 19.0 software (SPSS Inc., USA). A P-value less than 0.05 was considered statistically significant.
Results
Patient information
A total of 86 patients were selected and included in this study: 42 patients in the blade group and 44 patients in the screw group. No significant differences were observed in the baseline characteristics between the two groups (Table 1).
Table 1.
Preoperative general information of the patients.
| Cannulated compression screw group (n = 44) | DHS-BLADE group (n = 42) | |
|---|---|---|
| Male/female (n) | 20/24 | 18/24 |
| Age (year) | 56.8 ± 9.3 | 58.3 ± 8.6 |
| Garden classification (n) | ||
| I | 0 | 0 |
| II | 20 | 24 |
| III | 16 | 13 |
| IV | 8 | 5 |
All the operations were performed successfully, and representative radiographic images of femoral neck fractures fixed with a DHS-BLADE or cannulated compression screws are shown in Fig. 2, Fig. 3. No significant differences were found in terms of the operation time, incision size, and hospital stay between the two groups. However, patients treated with cannulated compression screws experienced significantly less surgical blood loss than those treated with a DHS-BLADE (P = 0.041; Table 2).
Fig. 2.
A 41-year-old man with a Garden III fracture fixed with DHS-BLADE. (A) Preoperative anterioposterior radiograph. (B) Preoperative lateral radiograph. (C) Preoperative CT image. (D) Preoperative three-dimensional CT reconstruction. (E) Postoperative anterioposterior radiograph. (F) Postoperative lateral radiograph. (G) Postoperative anterioposterior radiograph at 1 year. (H) Postoperative lateral radiograph at 1 year.
Fig. 3.
A 56-year-old woman with a Garden III fracture fixed with a cannulated compression screw. (A) Preoperative anterioposterior radiograph. (B) Preoperative lateral radiograph. (C) Preoperative CT image. (D) Preoperative three-dimensional CT reconstruction. (E) Postoperative anterioposterior radiograph. (F) Postoperative lateral radiograph. (G) Postoperative anterioposterior radiograph at 2 years. (H) Postoperative lateral radiograph at 2 years.
Table 2.
Comparison of surgical outcomes between the two groups.
| Cannulated compression screw group (n = 44) | DHS-BLADE group (n = 42) | P-value | |
|---|---|---|---|
| Surgical time (min) | 47.2 ± 18.6 | 43.4 ± 20.3 | 0.862 |
| Incision size (cm) | 3.6 ± 1.5 | 4.2 ± 1.8 | 0.891 |
| Surgical blood loss (ml) | 32.4 ± 24.7 | 87.2 ± 46.6 | 0.041 |
| Hospital stay (day) | 5.6 ± 2.8 | 6.1 ± 2.2 | 0.532 |
| Nonunion | 4.5% | 0% | 0.162 |
| Avascular necrosis | 9.1% | 7.1% | 0.741 |
| Femoral neck shortening ≥10 mm | 15.9% | 2.4% | 0.031 |
| Screw loosening | 22.7% | 4.8% | 0.016 |
| Screw cut-out | 4.5% | 0% | 0.162 |
| Harris hip score | 80.4 ± 9.3 | 86.1 ± 8.4 | 0.178 |
The 86 patients included were followed up for a mean time of 27 months (range, 24–36 months). No cases of postoperative infection, deep vein thrombosis, screw or plate break, or coxa vara occurred in either group. No statistically significant differences in terms of nonunion (4.5% vs. 0), avascular necrosis of the femoral head (9.1% vs. 7.1%), and screw cut-out were observed between the two groups. It should be noted that no patient in the DHS-BLADE group had nonunion or cut-out. However, the screw group showed significantly higher incidences of femoral neck shortening ≥10 mm (15.9% vs 2.4%, P = 0.031) and screw-exit (4.8% vs 22.7%, P = 0.016) compared with the blade group. At the last follow-up postoperatively, no statistically significant difference in Harris Hip scores was found between the two groups (Table 2).
Discussion
Various surgical techniques and instrumentations have been reported for stabilization of femoral neck fractures.18 Protecting the blood supply of the femoral head and reducing the incidence of complications by preventing additional soft tissue injury are the most important factors in choosing surgical fixation. The implants that fit the above criteria are the DHS-BLADE and cannulated compression screws, which were used in the present study. The findings of our study showed that the DHS-BLADE had advantages over cannulated compression screws for preventing femoral neck shortening, screw-exit, and cut-out in the treatment of femoral neck fractures. However, hammering of the DHS-BLADE into the bone can cause compaction of the surrounding cancellous bone, which may lead to microfracture and damage to the trabecular bone. This may increase the risks of failure of internal fixation.19 Fortunately, compaction of cancellous bone can also improve the anchorage of the implant and reduce the incidence of the cut-out.15 In a biomechanical study of an unstable femoral neck fracture, compared with the normal DHS, the DHS-BLADE showed better resistance to cut-out and better anti-rotation ability and greater surface area,20 which is consistent with our observation of no cases of cut-out or coxa vara in the present study. However, the DHS-BLADE can cause femoral neck shortening, which occurs along the direction of the implants with no coxa varus.
To the best of our knowledge of the DHS-BLADE, the locking compression plate (LCP) has replaced the traditional dynamic compression plate. The LCP does not need to be adhered to the bone shaft exactly. Moreover, the LCP is designed to have a degree with the locking screws, allowing a shorter plate and smaller incision, which may decrease the incidence of associated complications. The LCP was inserted with a 4–5 cm incision and 2-hole plate in our study. The DHS-BLADE is an extramedullary device that reduces postoperative hidden blood loss compared with PFNA.21 Meanwhile, the LCP design decreases surgical visible blood loss compared with the common DHS. In our study, the mean surgical blood loss in the DHS-BLADE group (87.2 ± 46.6 ml) was slightly higher than that in the screw group. However, neither group showed signs of severe blood loss and required blood transfusion. Therefore, the DHS-BLADE as a minimally invasive surgery has desirable features in the internal fixation of femoral neck fractures.
Bone union after fracture is determined by many factors, such as the force of trauma, displacement of fracture ends, and internal fixation. The cannulated compression screw is one of the most commonly choice of many surgeons when treating fresh femoral neck fractures. However, it provides weak holding in the fixation of a comminuted fracture, and may lead to secondary displacement of fracture ends and coxa vara.3 On the contrary, the DHS-BLADE has the advantages for the fixation of fractures with osteoporosis or unstable fractures. It has been reported that the DHS-BLADE can be used with one additional cannulated compression screw to improve the anti-rotation and biomechanical performance of unstable femoral neck fractures.22 In our study, although no cannulated compression screw was used in combination with the DHS-BLADE, good union was achieved in the majority of patients. Unfortunately, two patients (4.5%) in the screw group had nonunion and screw-exit. These patients were treated with arthroplasty and recovered well.
Although femoral neck fracture reduction and fixation are performed in an attempt to restore vascular supply to the femoral head, complications such as non-union and avascular necrosis still occur in about 10–20% and 10–30% of patients, respectively.23, 24, 25 Moreover, non-union and avascular necrosis are risk factors for future degenerative arthritis of the hip joint, and the reported percentages of cases requiring revision surgery or conversion to hip replacement range from 20% to 36%,26, 27 whereas the reported incidence of avascular necrosis of the femoral head varies greatly from 10% to 43%.28 In our study, 7.1% of the patients in the DHS-BLADE group developed avascular necrosis of the femoral head. Most cases of the necrosis occurred at 2 years postoperatively, at which time the fracture was healed and no obvious symptoms were observed. In the screw group, necrosis occurred in 9.1% of the patients during the first 2 years of follow-up. Among them, two patients had nonunion of femoral neck fracture, three patients underwent total hip arthroplasty, and one patient was lost to follow-up. Based on our clinical experience and previous studies, early bone union and a stable biomechanical environment in the DHS-BLADE group, which is beneficial to revascularization, were consistent with the less severe symptoms of necrosis.7 However, DHS-BLADE insertion did not reduce the incidence of necrosis compared with the cannulated compression screw.
Additionally, femoral neck shortening, with an incidence of around 31%, was also a common complication after internal fixation of femoral neck fractures,29 which usually occurs in the first 3 months postoperatively and is believed to be associated with bone resorption during the fracture healing. Both the cannulated compression screw and DHS-BLADE can slide to the fractured space, which obtain bone resorption and promote fracture healing by providing a stress stimulus to the fracture ends. However, these also result in a high incidence of femoral neck shortening. It has been suggested that femoral neck shortening by 5 mm can compromise hip function and even cause limp.29 We found that the screw group showed significantly higher incidences of femoral neck shortening ≥10 mm (P = 0.031) than the blade group. Usually, femoral neck shortening, together with screw-exit, can lead to destabilized fixation and irritation to the soft tissues. Screw-exit might be associated with previously existing osteoporosis as well as postoperative bone resorption caused by limited activity. In our study, the patients implanted with the DHS-BLADE showed a significantly lower incidence of screw-exit than those that implanted with cannulated compression screws (4.8% vs. 22.7%, P = 0.016). Since the cannulated compression screw has a small diameter, it is prone to cut-out and break. It has been suggested that implant cut-out was closely associated with the implant design, especially the screw thread design.4 Two patients in the screw group experienced severe implant cut-out and consequent damage to the acetabulum. However, none of the patients in the DHS-BLADE group experienced cut-out, resulting in a rate lower than the reported cut-out rate of 6.2% for helical blades.30 These might be explained by the good center–center position of the implants in our study.31 Interestingly, we noticed that all patients who experienced screw cut-out also had osteoporosis. Therefore, postoperative anti-osteoporosis therapy may help to prevent femoral neck shortening and screw cut-out.
Some limitations of our study should also be noted. First, unlike prospective and randomized studies, this was a single-center retrospective study. Secondly, the small sample size and short follow-up time may affect the accuracy of our findings. Therefore, further multicenter prospective and randomized studies with larger sample sizes and longer follow-up durations are urgently required to address the aforementioned issues.
Conclusion
The DHS-BLADE and cannulated compression screws might be equally effective in terms of postoperative fracture union in the treatment of fresh femoral neck fractures. However, the DHS-BLADE is superior to the cannulated compression screws in preventing femoral neck shortening, screw-exit, and cut-out.
Fund
None.
Conflicts of interest
The authors declare no conflict of interests.
Acknowledgements
None.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Broderick J.M., Bruce-Brand R., Stanley E. Osteoporotic hip fractures: the burden of fixation failure. Sci World J. 2013;2013:515197. doi: 10.1155/2013/515197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilk R., Skrzypek M., Kowalska M. Standardized incidence and trend of osteoporotic hip fracture in Polish women and men: a nine year observation. Maturitas. 2014;77:59–63. doi: 10.1016/j.maturitas.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Parker M.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Jt Surg Am. 2009;91:490–491. [PubMed] [Google Scholar]
- 4.Sommers M.B., Roth C., Hall H. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004;18:361–368. doi: 10.1097/00005131-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Simmermacher R.K., Ljungqvist J., Bail H. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008;39:932–939. doi: 10.1016/j.injury.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Strauss E., Frank J., Lee J. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37:984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Windolf M., Muths R., Braunstein V. Quantification of cancellous bone-compaction due to DHS Blade insertion and influence upon cut-out resistance. Clin Biomech (Bristol, Avon) 2009;24:53–58. doi: 10.1016/j.clinbiomech.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Windolf M., Braunstein V., Dutoit C. Is a helical shaped implant a superior alternative to the Dynamic Hip Screw for unstable femoral neck fractures? A biomechanical investigation. Clin Biomech (Bristol, Avon) 2009;24:59–64. doi: 10.1016/j.clinbiomech.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Leung F., Gudushauri P., Yuen G. Dynamic hip screw blade fixation for intertrochanteric hip fractures. J Orthop Surg. 2013:132–133. doi: 10.1177/230949901202000307. [DOI] [PubMed] [Google Scholar]
- 10.Zhao W.B., Liu L. Effect of dynamic hip system blade on the treatment of femoral neck fractures in elderly patients with osteoporosis. Chin J Traumatol. 2014;17:275–278. [PubMed] [Google Scholar]
- 12.Neilipovitz D.T., Murto K., Hall L., Barrowman N.J., Splinter W.M. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg. 2001;93:82–87. doi: 10.1097/00000539-200107000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Wong J., Hossam E., Suntheralingam Y., Rampersaud R., Chung F. Tranexamic acid reduces blood loss and transfusion in adult patients having spinal fusion surgery. Can J Anesth. 2006;53(suppl 1):26385. [Google Scholar]
- 14.Boraiah S., Paul O., Hammoud S., Gardner M.J., Helfet D.L., Lorich D.G. Predictable healing of femoral neck fractures treated with intraoperative compression and length-stable implants. J Trauma. 2010;69:142–147. doi: 10.1097/TA.0b013e3181bba236. [DOI] [PubMed] [Google Scholar]
- 15.Zlowodzki M., Jönsson A., Paulke R. Shortening after femoral neck fracture fixation: is there a solution? Clin Orthop Relat Res. 2007;461:213–218. doi: 10.1097/BLO.0b013e31805b7ec4. [DOI] [PubMed] [Google Scholar]
- 16.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 17.Marchetti P., Binazzi R., Vaccari V. Long-term results with cementless Fitek (or Fitmore) Cups. J Arthroplasty. 2005;20:730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Estrada L.S., Volgas D.A., Stannard J.P., Alonso J.E. Fixation failure in femoral neck fractures. Clin Orthop Relat Res. 2002;399:110–118. doi: 10.1097/00003086-200206000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Kold S., Bechtold J.E., Mouzin O., Elmengaard B., Chen X., Søballe K. Fixation of revision implants is improved by a surgical technique to crack the sclerotic bone rim. Clin Orthop Relat Res. 2005;432:160–166. doi: 10.1097/01.blo.0000149815.78598.ea. [DOI] [PubMed] [Google Scholar]
- 20.O'Neill F., Condon F., McGloughlin T., Lenehan B., Coffey J.C., Walsh M. Dynamic hip screw versus DHS blade: a biomechanical comparison of the fixation achieved by each implant in bone. J Bone Jt Surg Br. 2011;935:616–621. doi: 10.1302/0301-620X.93B5.25539. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Pei-xun, Dang Yu, Xue Feng. Clinical analysis of obvious and hidden blood loss during treatment of intertrochanter fracture with proximal femoral nail anti-rotation. Chin J Trauma. 2011;27:785–788. [Google Scholar]
- 22.Bhandari M., Rd T.P., Hanson B. Optimal internal fixation for femoral neck fractures: multiple screws or sliding hip screws? J Orthop Trauma. 2009;23:403–407. doi: 10.1097/BOT.0b013e318176191f. [DOI] [PubMed] [Google Scholar]
- 23.Angelini M., Mckee M.D., Waddell J.P. Salvage of failed hip fracture fixation. J Orthop Trauma. 2009;23:471. doi: 10.1097/BOT.0b013e3181acfc8c. [DOI] [PubMed] [Google Scholar]
- 24.Rogmark C., Flensburg L., Fredin H. Undisplaced femoral neck fractures–no problems? A consecutive study of 224 patients treated with internal fixation. Injury. 2009;40:274–276. doi: 10.1016/j.injury.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 25.Haidukewych G.J., Rothwell W.S., Jacofsky D.J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Jt Surg Am. 2004;86-A:1711–1716. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Bosch U., Schreiber T., Krettek C. Reduction and fixation of displaced intracapsular fractures of the proximal femur. Clin Orthop Relat Res. 2002;399:59–71. doi: 10.1097/00003086-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Kold S., Bechtold J.E., Mouzin O. Fixation of revision implants is improved by a surgical technique to crack the sclerotic bone rim. Clin Orthop Relat Res. 2005;432:160–166. doi: 10.1097/01.blo.0000149815.78598.ea. [DOI] [PubMed] [Google Scholar]
- 28.Su Y., Chen W., Zhang Q. An irreducible variant of femoral neck fracture: a minimally traumatic reduction technique. Injury. 2011;42:140–145. doi: 10.1016/j.injury.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Zlowodzki M., Brink O., Switzer J. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Jt Surg Br. 2008;90:1487–1494. doi: 10.1302/0301-620X.90B11.20582. [DOI] [PubMed] [Google Scholar]
- 30.Nüchtern J.V., Ruecker A.H., Sellenschloh K. Malpositioning of the lag-screws by one- or two-screw nailing systems for pertrochanteric femoral fractures: a biomechanical comparison of Gamma3 and Intertan. J Orthop Trauma. 2014;28:276–282. doi: 10.1097/BOT.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 31.Nikoloski A.N., Osbrough A.L., Yates P.J. Should the tip-apex distance (TAD) rule be modified for the proximal femoral nail antirotation (PFNA)? A retrospective study. J Orthop Surg Res. 2013;8:35. doi: 10.1186/1749-799X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]