Abstract
This was a population-based study of adult patients undergoing thyroidectomy using the Premier Healthcare Database, 2005-2014. The aim of this study is to evaluate the clinical and economic outcomes among older adults (age ≥65) undergoing thyroidectomy compared to younger adults (18-64).
Keywords: Thyroidectomy, Older Patients, Premier Database, Epidemiology, Surgery
INTRODUCTION
According to the US census bureau, the population aged greater than 65 years is expected to increase from 4.3 million in 2012 to 8.3 million in 2050, making up 21% of the population. Furthermore, the proportion of adults greater than 80 years old is expected to more than double in size from 11.7 million in 2012 to 30.9 million in 2050 (1). Increasing age is also associated with a higher prevalence of thyroid nodular disease and thyroid cancer (2, 3). Thus the combination of a rise in the proportion of older patients, an increased prevalence of thyroid disease with aging, and continuing technological advances in surgery will lead to more thyroidectomies being performed in older adults. (4). For these reasons, surgical volumes of patients 65 or older are expected to increase from 14% to 47% by 2020 (5).
While numerous single institution studies demonstrate the safety of thyroidectomy in older adults (6–8), population based studies using the Nationwide Inpatient Sample demonstrate worse clinical outcomes (9). However, most thyroidectomies are now being performed as outpatient procedures. Additionally, older patients have been described to have more aggressive thyroid cancers, yet are more likely to be undertreated (10, 11).
The aim of this study is to evaluate the clinical and economic outcomes of thyroidectomy among older adults (age ≥65, ≥70, and ≥80 years old) compared to younger adults.
METHODS
Data Source
The Premier Healthcare Database is a Health Insurance Portability and Accountability Act compliant large US hospital–based database developed for quality and utilization benchmarking (Premier Healthcare Solutions, Inc., Charlotte, NC; available at https://www.premierinc.com). The Premier Healthcare Database contains information from more than 700 geographically diverse, non-profit, nongovernment, urban, rural, teaching and nonteaching hospitals in the United States representing approximately 20% of all U.S. inpatient discharges. Information on more than 89 million inpatient discharges starting from 2000 is included, with a mean of 6.6 million inpatient discharges per year since 2011. The database also includes over 639 million total outpatient encounters. Data are submitted quarterly or monthly and undergo s extensive data validation that occurs during implementation and with each subsequent (monthly) data submission by the hospital. As data is received, rigorous validations are applied to the data and reviewed with each hospital. Normalization is applied to the data for comparisons. Before data can be published into the database, thresholds on cases, charges, and cost must be met, and these are reviewed by Premier on a monthly basis. In addition to the data elements available in most of the standard hospital discharge files, the Premier database also contains a date-stamped log of billed items, including procedures, medications, laboratory test performed, and diagnostic and therapeutic services at the individual patient level. All procedures and diagnoses are captured for each patient, as well as all drugs and devices received. Drug utilization information is available by day of stay and includes quantity, strength used, charge, and hospital reported cost Patient diagnoses and procedures are categorized according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coding system. The ICD-9-CM codes provided by the hospital were assumed to be correct and complete, as with all similarly derived administrative databases. Patient data are de-identified to protect the patients whose data are represented. Consequently, this study did not require institutional review board waiver or approval.
Cohort Identification
Adult patients (age ≥18) who underwent thyroidectomy over a 10-year period between January 2005 and December 2014 were identified using the following current procedural terminology codes: 60210, 60212, 60220, 60240, 60260, 60271, 60225, 60252, 60254, and 60270 (Table 1). Patients with service types of ‘same day surgery’, ‘observation’, or ‘inpatient status’ were included. Patients were excluded if age or gender was unknown, total patient charge was zero, or if admission was classified as “emergency”. Figure 1 illustrates the patient population used for this study.
Table 1.
Current Procedural Terminology (CPT) Codes
| CPT Code | CPT Code Description | Patient Number |
|---|---|---|
| 60210 | Partial thyroid lobectomy: unilateral; with or without isthmusectomy | 6,151 |
| 60212 | Partial thyroid lobectomy with contralateral subtotal lobectomy, including isthmusectomy | 1,011 |
| 60220 | Total thyroid lobectomy, unilateral with or without isthmusectomy | 28,214 |
| 60240 | Total thyroidectomy | 29,946 |
| 60260 | Completion thyroidectomy | 1,089 |
| 60271 | Thyroidectomy – cervical approach | 1,859 |
| 60225 | Thyroid lobectomy with contralateral subtotal lobectomy, including isthmusectomy | 3,736 |
| 60252 | Thyroidectomy with limited neck dissection | 2,801 |
| 60254 | Thyroidectomy with radical neck dissection | 283 |
| 60270 | Thyroidectomy – sternal split or transthoracic approach | 314 |
|
| ||
| Total | 75,404* | |
Total patient number not equal to total sample. More than one CPT code can be assigned to a patient.
Figure 1.
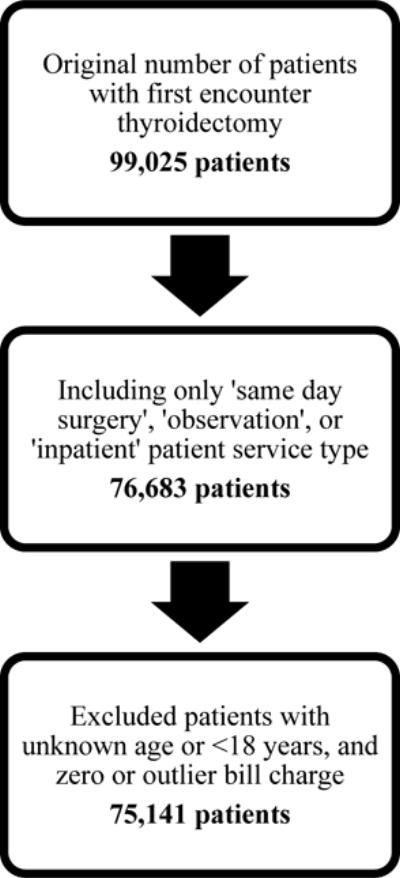
Patient Cohort Exclusion Criteria
Statistical Analysis
The older adult (≥ age 65) cohort was analysed by patient age using three age thresholds: ≥65, ≥70, and ≥80. The following outcomes were evaluated: discharge type, length of stay, complication rates, and total patient charge. Length of stay was analysed as a binary variable with a threshold of 48 hours. Complication rates were analysed based on International Classification of Diseases, ninth revision (ICD-9). Neck swelling was defined as ICD-9 codes 784.2 and 998.13. Multivariate logistic modelling after adjustment for known covariates was employed to estimate the odds ratio for the binary outcomes discharge status, length of stay over 48 hours, and presence of complication. Generalized log-linear regression was utilized to assess total patient charge. The previously mentioned outcomes were compared in this study adjusting for important covariates including: Age, gender, race, census region, hospital type, length of stay, surgeon speciality, payer group, Elixhauser comorbidity (12, 13), presence of complications, rural versus urban environment, final pathology, and labwork performed.
We also compared the association of outcomes with age in categories. All analyses were performed using STATA 14.0/MP for Linux (College Station, Texas).
RESULTS
Patient Demographics
Our study cohort consisted of 75,141 patients (Table 2) of which the majority were female, 62,082 (82.6%). Of this cohort, 15,805 (21.0%) patients were ≥65 years, 8,834 (11.8%) were ≥70 years, and 1,613 (2.2%) were ≥80 years old. The majority of patients were white (53,367; 71.0%), followed by black (8,653; 11.5%), and Hispanic (1924; 2.6%). Over half of patients were married (42,679; 56.8%). Over half of patients were from the South (41,527; 55.3%), followed by the Midwest (13,902; 18.5%), West (12,630; 16.8%), and Northeast (7,082; 9.4%). Managed care was the largest payer group (39,721; 52.9%), followed by Medicare (17,221; 22.9%), commercial (7,746; 10.3%), Medicaid (5,092; 6.8%), self-pay (1,411; 1.9%), direct employer contract (1,263; 1.7%), and charity (274; 0.4%). The Elixhauser comorbidity index ranged from −4 to 23, where most patients (95.7% – 96.3%) in each age group had a score of zero (Table 4). There was no significant difference in score among age groups.
Table 2.
Patient Cohort Demographics
| Patient Number; N = 75,141 (%) | ||
|---|---|---|
| Age | ||
|
| ||
| 18–29 | 5,271 (7.0) | |
| 30–39 | 11,105 (14.8) | |
| 40–49 | 16,176 (21.5) | |
| 50–59 | 18,805 (25) | |
| 60–69 | 14,950 (19.9) | |
| 70–79 | 7,221 (9.6) | |
| 80–89 | 1,613 (2.1) | |
|
| ||
| Gender | ||
|
| ||
| Female | 62,082 (82.6) | |
| Male | 13,059 (17.4) | |
|
| ||
| Race | ||
|
| ||
| White | 53,367 (71.0) | |
| Black | 8,653 (11.5) | |
| Hispanic | 1,924 (2.6) | |
| Other | 11,197 (14.9) | |
|
| ||
| Marital status | ||
|
| ||
| Married | 42,679 (56.8) | |
| Single | 24,615 (32.8) | |
| Other | 7,847 (10.4) | |
|
| ||
| Census region | ||
|
| ||
| South | 41,527 (55.3) | |
| Midwest | 13,902 (18.5) | |
| West | 12,630 (16.8) | |
| Northeast | 7,082 (9.4) | |
|
| ||
| Teaching hospital | ||
|
| ||
| No | 48,516 (64.6) | |
| Yes | 26,625 (35.4) | |
|
| ||
| Vicinity to city | ||
|
| ||
| Rural | 8,162 (10.9) | |
| Urban | 66,979 (89.1) | |
|
| ||
| Hospital beds | ||
|
| ||
| Median (IQR) | 393 (275 – 532) | |
| Range | 22 – 1218 | |
Table 4.
Elixhauser Comorbidity Score by Age Group
| Comorbidities | Age < 65 | Age ≥ 65 | Age < 70 | Age ≥ 70 | Age < 80 | Age ≥ 80 | |
|---|---|---|---|---|---|---|---|
| Total number of encounters | 59,336 | 15,805 | 66,307 | 8,834 | 73,528 | 1,613 | |
| Elixhauser Comorbidity Group | < 0 | 139 (0.2%) | 34 (0.2%) | 151 (0.2%) | 22 (0.2%) | 167 (0.2%) | 6 (0.4%) |
| 0 | 56869 (95.8%) | 15219 (96.3%) | 63578 (95.9%) | 8510 (96.3%) | 70545 (95.9%) | 1543 (95.7%) | |
| 0–10 | 2204 (3.7%) | 514 (3.3%) | 2434 (3.7%) | 284 (3.2%) | 2656 (3.6%) | 62 (3.8%) | |
| >10 | 124 (0.2%) | 38 (0.2%) | 144 (0.2%) | 18 (0.2%) | 160 (0.2%) | 2 (0.1%) |
Patient Care
The majority of patients in our population sought medical care at non-teaching hospitals (48,516; 64.6% vs. 26,625; 35.4%) located in urban areas (66,979; 89.1%). The median number of hospital beds was 393 with a range of 22 to 1,218. The majority of patients were admitted from a ‘nonhealthcare facility’ (75.5%) followed by admissions from ‘clinic’ (14.2%). Procedures were performed by a similar proportion of general surgeons and otolaryngologists (50.4% vs. 49.6%, respectively).
Thyroid Surgery
The majority of patients underwent a total thyroidectomy (29,946; 39.1%), followed by a total thyroid lobectomy, unilateral with or without isthmusectomy (28,214; 37.4%) (Table 1). On pathology, the majority of patients had a benign disease (56,159; 74.7% versus 18,982; 25.3%). The proportion of malignancy was significantly lower among patients ≥65 (p<0.001), ≥70 (p<0.001), and ≥80 years old (p<0.05) when compared to their younger counterparts (22.4% vs 26.7%; 22.6% vs. 25.6%; and 23.0% vs. 25.3%, respectively). There was a significantly lower proportion of neck dissections among those ≥65 years old (3.06%) and ≥70 years old (3.27%) than that of younger patients (4.38% and 4.21%, respectively, p<0.001). No difference was seen when among those ≥80 years old and younger.
Discharge Type
The majority of thyroid surgery admissions were elective (70.9%) and were discharged home (96.6%) as opposed to a home health organization (0.6%). No statistically significant association was found in discharge status among patients ≥70 years old (p=0.3). However, patients ≥65 and ≥80 years were 0.9 times (adjusted OR or aOR 0.86, 95% CI: 0.73-1.00; p=0.048) and 1.6 times (aOR 1.59, 95% CI: 1.25 – 2.02; p<0.001), respectively, more likely to not be discharged to their residence. Furthermore, patients ≥80 years were 2.6 times (aOR 2.577, 95% CI: 1.72 – 3.86; p<0.001) more likely to be discharged to home health organization than to be discharged to their residence.
Length of Stay
Among our patient population, 72,906 (97.0%) were admitted as an outpatient and therefore discharged within 23 hours. Among the 2,235 (3%) of inpatients, the majority were admitted for one day (1.535, 68.7%) followed by 21.8 % for 2 days, 8.3% for 3-5 days, and 1.2% for more than 5 days. The median length of stay for all age groups among inpatients was 1 day (Interquartile range, IQR, 1 – 2) with a range of 1 – 12 days. The proportion of inpatients among those ≥65, ≥70, and ≥80 years was 3.4% (535 patients), 3.4% (300 patients), and 4.4% (71 patients), respectively. There was a significant difference in the proportion of inpatients among all three age thresholds where older adults were more likely to be inpatients compared to those that were younger (Age 65: 2.9% versus 3.4% p<0.01; Age 70: 2.9% versus 3.4% p<0.05; Age 80: 2.9% versus 4.4% p<0.01) No statistically significant association was found in hospital length of stay among patients ≥65, ≥70, and ≥80 years old (p=1.0, p=1.0, p=0.5, respectively). Patients who underwent a total thyroidectomy contributed the most to an inpatient status (1,010, 45.2%), followed by those who underwent a thyroid lobectomy with or without isthmusectomy (516, 23.1%).
Total Patient Charge
Total patient charge was the amount, in dollars, of billable items to the patient. The median total patient charge was $17,841 (IQR: 12,988-24,919) ranging from $4,790-67,254. The median total patient charge among those ≥65, ≥70, and ≥80 years was $17,799, $17,580, and $17,263 respectively. No statistically significant association was found in total patient charge among patients ≥65, ≥70, and ≥80 years when compared to younger adults (p=0.1, p=0.2, p=0.2, respectively). Medicare insurance was associated with a significant decrease in total patient charge (OR = 0.97; 95% CI: 0.96 – 0.98; p<0.001).
Complications
2,750 (3.7%) patients experienced complications after surgery with most reporting only one complication (2,516, 91.5%). The most common complications reported were neck swelling (1,150; 38.5%) and hypocalcemia (1,150; 38.5%) followed by neck hematoma (240; 8.0%), vocal cord paralysis (190, 6.4%) –181 unilateral paralysis and 9 bilateral paralysis, and dysphagia (175; 5.9%). The rate of complications for patients ≥65, ≥70, and ≥80 was 4.2% (667 patients), 4.5% (394 patients), and 6.2% (100 patients), respectively. There was a significant association between patients ≥65 and vocal cord paralysis (p<0.05).
Patients ≥80 years old were 1.6 times more likely to have at least one complication (aOR 1.61, 95% CI: 1.30 – 2.00; p<0.001). Neck swelling and hypocalcemia were the two most common complications among the ≥65, ≥70 and ≥80 years old groups (≥65 years: 299 and 276, 40.0% and 36.0 %; ≥70 years: 170 and 146, 37.7% and 32.4%; ≥80 years: 41 and 33, 36.0% and 29.0%). Excluding neck swelling, those ≥ 80 years were more likely to have complications (OR = 1.63, 95% CI: 1.26-2.11; p<0.001). The rate of hypocalcemia among those ≥65, ≥70, and ≥80 years was 1.75%, 1.65%, and 2.05%, respectively. Hypocalcemia had a statistically significant association with those ≥65 years (p < 0.05).
DISCUSSION
In summary, our study represents one of the largest population-based studies over a 10-year period demonstrating worse outcomes for patients ≥80 years undergoing thyroidectomy. These patients are 2.6 times more likely to be discharged to a home health organization (aOR 2.58, 95% CI: 1.72 – 3.86; p<0.001) and 1.6 times more likely to have at least one complication (aOR 1.61, 95% CI: 1.30 – 2.00; p<0.001) even after controlling for comorbidities. Among patient age ≥80 years, the most common complications were neck swelling (n=41, 36.0%), hypocalcemia (n=33, 29.0%), and vocal cord paralysis (n=20, 17.5%). Individual patient risk stratification and preoperative assessment are important since the effects of aging have significant variability on physiologic function, associated comorbidities, and patient life span (5).
Similarly, using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) during 2003–2004 Sosa et al, reported an adjusted complication rate of 5.6% for patients aged 80 years and older was 5.6%, a significant difference compared to that of patients 65 to 79 years (2.1%), 45 to 64 years (0.3%), and 18 to 44 years (0.2%), respectively (p < 0.001). Using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2005 to 2008, Grogan et al reported that patients ≥80 were five times (OR = 4.9, 95% CI: 2.5–9.6) more likely to develop significant pulmonary, cardiac, and infectious complications after thyroidectomy compared with younger patients (14). Furthermore, Mekel et al reported a 5.5% complication rate among 90 patients aged 80 years and older as compared to 2.5% in 242 patients <80 years old.
We found that older patients (of all three age thresholds) were more likely to undergo thyroidectomy for benign disease in comparison to their younger counterparts. This finding is in agreement with data from HCUP-NIS where older patients were more likely to require thyroidectomy for benign disease (9). Similarly, Mekel et al reported a 20% malignancy rate in patients ≥80 years old, supporting the notion that the majority of elderly patients are undergoing thyroidectomy procedures for benign diseases (15).
However, contrary to previously published studies, we did not find any significant increase in hospital length of stay among older patients. Several studies have reported on the increased length of stay among elderly patients (9, 14, 15). Sosa et al reported that the adjusted average length of stay for patients aged 80 years and older was 2.88 days, a significant difference compared to that of patients 65 to 79 years (2.22 days), 45 to 64 years (1.77 days), and 18 to 44 years (1.62 days), respectively (p < 0.001) (Sosa, Mehta et al. 2008). Similarly, Grogan et al found that patients ≥80 years old (1.8 days) had a significant increase in hospital stay compared with those ≤65years old (1.1 days) (Grogan, Mitmaker et al. 2012). This may be explained by an increasing shift towards performing outpatient thyroidectomy operations or discharge to a facility rather than home.
In contrast to previously published studies, our results did not demonstrate a statistically significant difference in total patient charge among older patients when compared to younger patients. This is also reflected by the lack of significant difference in the hospital length of stay. In our study, we discuss healthcare cost in terms of patient charge, which reflects the amount, in dollars, billed to the patient. For this reason, the median patient charge in our study may be higher than that of others that use patient cost, which reflects the total cost the hospital incurred to treat the patient. Sosa et al (9) reported a 20%, 35%, and 44% cost increase in patients ≥80 years when compared to that of patients 65 to 79 years, 45 to 64 years, and 18 to 44 years, respectively (p < 0.001). A significant difference in adjusted patient cost among all patient age groups was observed.
One of the inherent limitations in our study is its retrospective nature. Moreover, this database does not have long-term follow-up to determine outpatient mortality rates for our sample population. We also were unable to incorporate surgeon volume, however, we feel this is representative of current practice. Furthermore, information to differentiate the incidence of permanent versus transient hypocalcemia was not available. The reason for the age-related disparity in vocal cord paralysis is unclear from this dataset and cannot be attributed to malignancy alone as older patients had lower rates of malignancy. However, the results of our study highlight the need to study this in a prospective fashion in future studies.
Despite these limitations, the results presented in this paper illustrate that even after thyroidectomy, surgical outcomes of older patients are relatively worse than in younger adults. Additional prospective studies are needed to validate these findings and identify risk factors associated with the clinical and surgical outcomes of older patients post thyroidectomy. This will allow clinicians to improve pre-operative counseling, informed consent, and post-operative awareness for the surgical team taking care of this patient among this patient population, as they will be better able to weight the costs and benefits of surgery.
Table 3.
Patient Cohort Clinical Data
| Patient Number; N = 75,141 (%) | ||
|---|---|---|
| Elixhauser Comorbidity Index | ||
|
| ||
| < 0 | 173 (0.2) | |
| 0 | 72,088 (95.9) | |
| 0 – 10 | 2,718 (3.6) | |
| > 10 | 162 (0.2) | |
|
| ||
| Encounter type | ||
|
| ||
| Outpatient | 72,906 (97.0) | |
| Inpatient | 2,235 (3.0) | |
|
| ||
| Admission source | ||
|
| ||
| Non-Healthcare Facility | 56,764 (75.5) | |
| Clinic | 10,641 (14.2) | |
| Other | 7,736 (10.3) | |
|
| ||
| Admission type | ||
|
| ||
| Elective | 53,254 (70.9) | |
| Trauma Center | 34 (0.0) | |
| Urgent | 3,155 (4.2) | |
| Non-coded | 18,698 (24.9) | |
|
| ||
| Discharge status | ||
|
| ||
| Discharge to Home or Self-Care | 72,576 (96.6) | |
| Discharge to Home Health Organization | 420 (0.6) | |
| Other | 2,145 (2.9) | |
|
| ||
| Patient service type | ||
|
| ||
| Same Day Surgery | 39,831 (53.0) | |
| Observation | 32,875 (43.8) | |
| Inpatients | 2,435 (3.2) | |
|
| ||
| Attending physician specialty | ||
|
| ||
| General Surgery | 37,894 (50.4) | |
| Otolaryngology | 37,425 (49.6) | |
|
| ||
| Type of complications | ||
|
| ||
| Neck Swelling | 1,150 (38.5) | |
| Hypocalcemia | 1,150 (38.5) | |
| Neck Hematoma | 240 (8.0) | |
| Unilateral Vocal Cord Paralysis | 181 (6.1) | |
| Dysphagia | 175 (5.9) | |
| Stridor | 28 (1.0) | |
| Laryngeal Edema | 17 (0.6) | |
| Esophageal Disorder, not elsewhere classified | 12 (0.4) | |
| Bilateral Vocal Cord Paralysis | 9 (0.3) | |
| Superficial Nerve Injury | 7 (0.2) | |
| Cellulitis of neck | 5 (0.2) | |
| Pulmonary Insufficiency, not elsewhere classified | 4 (0.1) | |
| Acute Respiratory Failure | 3 (0.1) | |
| Cardiac Arrest | 1 (0.0) | |
| Respiratory Arrest | 1 (0.0) | |
| Postoperative Infection, not elsewhere classified | 1 (0.0) | |
| Aspiration Pneumonitis | 1 (0.0) | |
|
| ||
| Number of complications | ||
|
| ||
| 0 | 72,391 (96.3) | |
| 1 | 2,516 (3.3) | |
| 2 | 233 (0.3) | |
| 3 | 1 (0) | |
|
| ||
| Inpatient length of stay | ||
|
| ||
| 1d | 1,535 (68.7) | |
| 2d | 488 (21.8) | |
| 3–5d | 185 (8.3) | |
| >5d | 27 (1.2) | |
|
| ||
| Patient charges | ||
|
| ||
| Median (IQR) | $17,841 ($12,988 – $24,919) | |
| Range | $ 4,790 – $ 67,254 | |
|
| ||
| Payer group | ||
|
| ||
| Managed care | 39,721 (52.9) | |
| Medicare | 17,221 (22.9) | |
| Commercial | 7,746 (10.3) | |
| Medicaid | 5,092 (6.8) | |
| Other | 2,230 (3.0) | |
| Self-pay | 1,411 (1.9) | |
| Direct employer contract | 1,263 (1.7) | |
| Charity | 274 (0.4) | |
| Indigent | 98 (0.1) | |
| Workers compensation | 85 (0.1) | |
|
| ||
| Labs done | ||
|
| ||
| No | 10,553 (14.0) | |
| Yes | 64,588 (86.0) | |
|
| ||
| Malignancy | ||
|
| ||
| No | 56,159 (74.7) | |
| Yes | 18,982 (25.3) | |
Table 5.
Characteristics According to Age Group in Comparison to Younger Adults
| Odds Ratio (95% Confidence Interval) | ||||||
|---|---|---|---|---|---|---|
| Age ≥ 65 | P-value | Age ≥ 70 | P-value | Age ≥ 80 | P-value | |
| Patient Charges | 1.011 (0.998–1.025) | 0.087 | 0.991 (0.978–1.004) | 0.169 | 0.983 (0.959–1.006) | 0.152 |
| Length of Stay Over 48 Hours | 0.681 (0.420–1.106) | 0.121 | 0.940 (0.602–1.468) | 0.786 | 1.025 (0.955–1.100) | 0.501 |
| Not Discharged Home | 0.855 (0.733–0.998) | 0.048 | 1.026 (0.881–1.195) | 0.740 | 1.587 (1.247–2.020) | <0.001 |
| Discharge to Home Health Organization | 0.940 (0.677–1.306) | 0.713 | 1.174 (0.869–1.587) | 0.295 | 2.577 (1.722–3.856) | <0.001 |
| Complication | 1.094 (0.942–1.271) | 0.238 | 1.145 (0.996–1.318) | 0.058 | 1.610 (1.296–2.000) | <0.001 |
Research Highlights.
Population study over 10 years showing worse outcomes for thyroidectomy patients ≥80 years
Neck swelling, hypocalcemia, and vocal cord paralysis were most common complications
No difference was found in hospital stay or patient charge in patients ≥65, ≥70, and ≥80 years
Preoperative risk stratification is important since the effects of aging are variable
Acknowledgments
None.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. Washington, DC: US Census Bureau; 2014. pp. 25–1140. [Google Scholar]
- 2.Kwong N, Medici M, Angell TE, et al. The influence of patient age on thyroid nodule formation, multinodularity, and thyroid cancer risk. The Journal of Clinical Endocrinology & Metabolism. 2015;100(12):4434–40. doi: 10.1210/jc.2015-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guth S, Theune U, Aberle J, et al. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. European journal of clinical investigation. 2009;39(8):699–706. doi: 10.1111/j.1365-2362.2009.02162.x. [DOI] [PubMed] [Google Scholar]
- 4.Lang BH-H, Lo CY. Technological innovations in surgical approach for thyroid cancer. Journal of oncology. 2010;2010 doi: 10.1155/2010/490719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christmas C, Makary MA, Burton JR. Medical considerations in older surgical patients. Journal of the American College of Surgeons. 2006;203(5):746–51. doi: 10.1016/j.jamcollsurg.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Longheu A, Medas F, Pisano G, et al. Differentiated thyroid cancer in patients≥ 75 years: Histopathological features and results of surgical treatment. International Journal of Surgery. 2016;33:S159–S63. doi: 10.1016/j.ijsu.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Bliss R, Patel N, Guinea A, et al. Age is no contraindication to thyroid surgery. Age and ageing. 1999;28(4):363–6. doi: 10.1093/ageing/28.4.363. [DOI] [PubMed] [Google Scholar]
- 8.Seybt MW, Khichi S, Terris DJ. Geriatric thyroidectomy: safety of thyroid surgery in an aging population. Archives of Otolaryngology–Head & Neck Surgery. 2009;135(10):1041–4. doi: 10.1001/archoto.2009.138. [DOI] [PubMed] [Google Scholar]
- 9.Sosa JA, Mehta PJ, Wang TS, et al. A population-based study of outcomes from thyroidectomy in aging Americans: at what cost? Journal of the American College of Surgeons. 2008;206(6):1097–105. doi: 10.1016/j.jamcollsurg.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Biliotti G, Martini F, Vezzosi V, et al. Specific features of differentiated thyroid carcinoma in patients over 70 years of age. Journal of surgical oncology. 2006;93(3):194–8. doi: 10.1002/jso.20512. [DOI] [PubMed] [Google Scholar]
- 11.Park HS, Roman SA, Sosa JA. Treatment patterns of aging Americans with differentiated thyroid cancer. Cancer. 2010;116(1):20–30. doi: 10.1002/cncr.24717. [DOI] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 13.van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical care. 2009:626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 14.Grogan RH, Mitmaker EJ, Hwang J, et al. A population-based prospective cohort study of complications after thyroidectomy in the elderly. The Journal of Clinical Endocrinology & Metabolism. 2012;97(5):1645–53. doi: 10.1210/jc.2011-1162. [DOI] [PubMed] [Google Scholar]
- 15.Mekel M, Stephen AE, Gaz RD, et al. Thyroid surgery in octogenarians is associated with higher complication rates. Surgery. 2009;146(5):913–21. doi: 10.1016/j.surg.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


