Abstract
Hypertensive crises are elevations of blood pressure higher than 180/120 mmHg. These can be urgent or emergent, depending on the presence of end organ damage. The clinical presentation of hypertensive crises is quite variable in elderly patients, and clinicians must be suspicious of non-specific symptoms. Managing hypertensive crises in elderly patients needs meticulous knowledge of the pathophysiological changes in them, pharmacological options, pharmacokinetics of the medications used, their side effects, and their interactions with other medications. Clevidipine, nicardipine, labetalol, esmolol, and fenoldopam are among the preferred choices in the elderly due to their efficacy and tolerability. Nitroprusside, hydralazine, and nifedipine should be avoided, unless there are no other options available, due to the high risk of complications and unpredictable responses.
Keywords: Beta-blockers, Calcium channel blockers, Clevidipine, Elderly, Esmolol, Fenoldopam, Hypertensive crises, Labetalol, Nicardipine, Nitroprusside
1. Introduction
Hypertension (HTN) remains a common illness around the World.[1] Uncontrolled HTN can lead to hypertensive crises. These are divided into two groups, urgencies and emergencies.[2] Both of them involve severe elevations of blood pressure (BP) more than 180/120 mmHg.[3] The core difference between them is whether severe HTN causes any organ dysfunction (hypertensive emergency) or not (urgency).[1],[3] These crises are common among the elderly.
Management of hypertensive crises in elderly patients should integrate a comprehensive set of pharmacological strategies, depending on the core pathophysiological changes related to aging, preexisting risk factors, coexistent comorbidities, speed of progression of the condition, and the extensiveness of organs involvement. Failure to successfully manage these crises in the elderly is associated with significant morbidity and mortality.[4]
2. Epidemiology and pathophysiology
HTN is one of the most important diseases among in the elderly population. According to the National Health and Nutrition Examination Survey during 2015–2016, 63.1% of American people aged > 60 years have elevated blood pressure.[5] The vast majority of these patients have essential HTN.[6] In addition, HTN remains a major risk factor for cerebrovascular as well as cardiovascular diseases, two of the leading causes of death in the United States causing about 770,000 deaths only in 2016.[7]
The incidence of HTN, and hence, its complications such as hypertensive crises, is different among different groups, and is higher in the elderly and African-Americans.[8]–[11] Hypertension is not just more prevalent in elderly people, but mortality and morbidity are more significant as well.[12] The investigators of the multicenter STAT registry reported a hospital mortality rate of 6.9% among patients with acute hypertensive crises requiring hospitalization and a cumulative 90 day mortality of 11% among these patients.[13]
Severe HTN is predominant among patients with history of HTN in the majority of cases.[10] Many of them have inadequate previous medical management, or poor compliance to treatment.[12] Those preventable causes should be addressed and treated, as the recurrence rate of acute hypertensive crises is high. The STAT investigators reported a 90-day readmission rate of 37%, of which, 25% were due to recurrent acute hypertensive crises.[13]
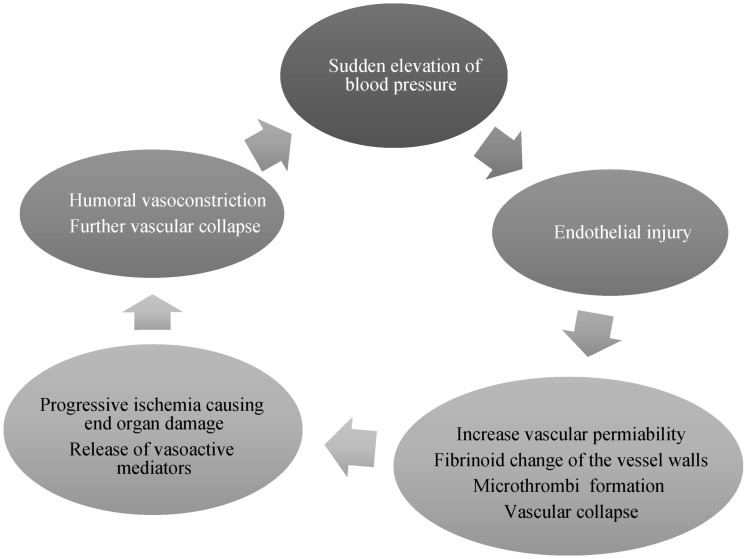
To understand the extent of HTN among the elderly, one must be aware of the pathophysiology of this entity. The regulation of BP is a concert of several organs/systems. The most important mechanisms are the cardiac output and systemic vascular resistance (SVR).[14] Elderly people suffer increased SVR and, hence, elevated BP.[15] Several mechanisms have been suggested to explain the increase in SVR, such as endothelial dysfunction, neuro-hormonal dysregulation, and a reduction in renal homeostatic mechanisms due to decreased glomerular filtration rate (Figure 1).[14],[16],[17]
Figure 1. Pathophysiological mechanisms of acute hypertensive crises.
3. Clinical manifestations
Many elderly patients with severe uncontrolled HTN are totally asymptomatic. Pinna and collaborators, in a study of 1,546 patients (mean age = 69 years) presented with acute hypertensive crises, reported that 55.6% of the patients referred non-specific symptoms such as dizziness, palpitations, and headache.[18] Whereas symptoms related to end-organ damage, such as chest pain and focal neurologic deficits, were evident in 28.3% and 16.1% of patients, respectively.[18] Elderly patients are more likely to have hypertensive emergencies, rather than urgencies, than the general population.[13]
The most frequent end-organ damage associated with hypertensive emergencies are cerebral infarction, acute pulmonary edema, and hypertensive encephalopathy (24%, 23%, and 16%, respectively).[2]
4. Management
The management of hypertensive crises in elderly requires prompt understanding of the pathophysiology of the disease, the physiological changes among them, and mechanism of action and side effects of the medications available (See Table 1). Most experts advise to generally reduce the mean arterial pressure by approximately 10%–15% during the first hour, and another 10%–15% during the next 2 to 4 hours due to the risk of hypoperfusion if the BP is lowered too suddenly or too far (e.g., into the range of < 140/90 mmHg).[19]–[21] However, faster drop in BP is required in certain conditions, such as aortic dissection, in which BP should be kept between 100 and 120 mmHg systolic and less than or equal to 60 to 70 mmHg diastolic as fast as possible.[20],[22],[23] While in the acute phase of ischemic stroke, it has been recommended that lowering of BP should be delayed unless BP is > 220/120 mmHg or > 200/100 mmHg with end organ damage or if the patient will receive thrombolytics.[24] In hemorrhagic stroke, the target BP is variable but generally systolic blood pressure (SBP) can be reduced safely to ≤ 140 mmHg.[25] The INTERACT2 trial showed that a rapid decrease of BP does not have a representative reduction in primary outcome of mortality or severe disability in patients with an acute intracerebral hemorrhage, however, their analysis of modified Rankin scores revealed that patients had a better functional outcome when their BP was intensively decreased.[26]
Table 1. Pharmacokinetics of different medications used in the management of hypertensive crises in the elderly.
| Medication | Mechanism(s) | Dosage | Onset | Half-life |
| Nitroglycerin | Activation of guanylyl cyclase via NO | 5 to 200 µg/min | 2–5 min | 1–4 min |
| Nitroprusside | Activation of guanylyl cyclase via NO | 0.3 to 10 mcg/kg/min | < 2 min | –2 min |
| Nifedipine | 1st generation dihydropyridine calcium-channel blocker | 10 to 20 mg 3 times daily | –20 min | 2.5–5 h |
| Nicardipine | 1st generation dihydropyridine calcium-channel blocker | 5–25 mg/h | 5–15 min | 4–6 h |
| Clevidipine | 3rd generation dihydropyridine calcium-channel blocker | 1–2 mg/h Increase every 10 min up to 16 mg/h | 2–4 min | 5–15 min |
| Labetalol | Selective α1-adrenergic receptor blocker andnonselective β-adrenergic blocker | 200–400 mg per o.s. every 2–3 h | 30–120 min | 2–6 h |
| Esmolol | Beta1 receptor blocker | 0.5–1 mg/kg loading dose.50–300 µg/kg/min infusion | 60 s | 20 min |
| Clonidine | Alpha2 adrenergic agonist and imidazoline I1 receptor agonist | 500 µg/kg in bolus and 25–300 µg/kg/min | 30 min | 12–16 h |
| Fenoldopam | Dopamine type-1 receptor agonist | 0.05–1.6 µg/Kg/ min | 5–10 min | 5 min |
| Hydralazine | Inhibition of calcium influx in vascular smooth muscle cells | 20 mg initial bolus; 20–80 mg repeat boluses | 5–15 min | 3 h |
NO: Nitric oxide.
Regardless of the target BP, the pharmacological management must include agents that are titratable and easily reversible. The choice of the medications also depends on the patient's comorbidities, availability, and end-organ involvement (Table 2).
Table 2. Specific indications and adverse effects of different drugs used in the management of acute hypertension in the elderly.
| Medication | Specific Indications | Adverse Effects |
| Nitroglycerin | Acute coronary syndrome, pulmonary edema, volume overload | Headache, vomiting reflex tachycardia and methemoglobinemia |
| Nitroprusside | Use only in the elderly when other alternatives are not available | Thiocyanate and cyanide intoxication, coronary steal syndrome |
| Nifedipine | Not recommended in the elderly patient | Hypotension, coronary steal syndrome, reflex tachycardia |
| Nicardipine | Most hypertensive crises as a potent vasodilator | Headache, local phlebitis, vomiting |
| Clevidipine | Most hypertensive crises | Headache, tachycardia, heart failure |
| Labetalol | Acute aortic dissection | Heart block and bronchoconstriction |
| Esmolol | Post-operative hypertension, useful in increased cardiac output, easily titration | Heart block and heart failure |
| Clonidine | Severe hypertension associated with pain and anxiety | Rebound hypertension and sedative effects |
| Fenoldopam | Renal arterial disease, glomerulonephritis or vascular diseases with impaired renal function, very useful | Headache, tachycardia, nausea and exacerbation of glaucoma |
| Hydralazine | Not recommended in elderly patients | Reflex tachycardia and severe hypotension |
In patients presenting with hypertensive urgencies, a less drastic approach can be considered. Some authors suggest a decrease of BP over a period of 24–48 hours with an oral short-acting agent, such as angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, followed by close monitoring of the patient for several hours.[1],[21]
The following paragraphs describe some of the common agents used to treat this condition.
5. Common agents
5.1. Nitroglycerin
Nitroglycerin is a potent vasodilator prodrug that acts on Cyclic guanosine monophosphate (cGMP) via release of nitric oxide (NO).[27] The hypotensive effects are secondary to a decrease in the preload and cardiac output.[27]–[29] Based on the data from the Euro-STAT registry, nitroglycerin is the most commonly drug used for acute HTN in the intensive care unit.[30] This agent is available in different routes of administration including intravenous, oral, sublingual, and transdermal.[27] The onset action of nitroglycerin is 2–5 minutes, and it has a plasma half-life of 1–4 minutes with half-life of metabolites of 40 minutes.[27] It metabolizes via erythrocytes, hepatic, and vessels walls.[27] The recommended intravenous dose of nitroglycerin for the treatment of hypertensive crises is from 5 to 200 µg/min.[31] Tachyphylaxis is common. The most common adverse effects include headache, vomiting, reflex tachycardia and methemoglobinemia.[32] Nitroglycerin is particularly useful in clinical practice in acute coronary syndromes and pulmonary edema as an adjunctive agent.[1],[4],[16],[33],[34]
5.2. Sodium nitroprusside
Nitroprusside is a potent vasodilator that elicits its effects on both arteries and veins.[35] It is comprised of a ferrous ion center complexed with five cyanide moieties and a nitrosyl group. Once infused, it can interact with oxyhemoglobin, dissociating immediately and forming methemoglobin while releasing cyanide and NO.[35] Nitric oxide causes then vasodilation, and mediates the antihypertensive properties of the medication while cyanide can accumulate potentially to toxic levels.[36] For years, it used to be the gold standard; however, because the cyanide toxicity is so significant, the Food and Drug Administration placed a black box warning in 1991.[37] Nevertheless, this medication is still being used, although less than before.[35] In the STAT registry, nitroprusside was the 4th most commonly used drug (13%) in management of hypertensive crises with neurological manifestations.[38]
Wood and coworkers showed that elderly patients are at a particular risk for developing complications when receiving nitroprusside; and that hypotension is very common among them.[39] The ECLIPSE trial compared nitroprusside versus other antihypertensives; it showed that this agent caused higher mortality when compared with other agents.[40] From our standpoint, nitroprusside should only be used when other safer alternatives are not available, especially among elderly patients.
5.3. Nifedipine
Nifedipine is a first generation calcium channel blocker.[41] For a period of time, it had been used widely through oral and sublingual capsules for the management of hypertensive crises.[16] However, it is poorly soluble, and poorly absorbed through the buccal mucosa, and swallowing the drug is the only effective method of administration.[42] The American Geriatrics Society, in the updated Beers criteria, strongly recommended avoiding nifedipine in patients older than 65 years, due to the potential risk of hypotension, which may precipitate for myocardial ischemia.[43] In addition, in elderly patients, it can cause a rapid fall in BP, coronary steal syndrome, and reflex tachycardia.[44],[45] Given those serious side effects and complete lack of outcome data, Grossman and coworkers pointed out that in true hypertensive emergencies, this agent is contraindicated.[44]
5.4. Nicardipine
Nicardipine is a second generation dihydropyridine L-type calcium channel blocker.[41] It is highly selective to vessels without affecting cardiac contractility.[46] It is a potent coronary dilator as it is more selective to coronary beds than systematic beds.[33] In a retrospective analysis to compare nicardipine to labetalol in managing HTN in critically-ill patients, Malesker and Hilleman found that nicardipine was as efficacious as labetalol with significantly fewer side effects, which were mainly hypotension and bradycardia.[47] Although it has been reported to cause bradycardia in elderly patients,[48] tachycardia is a more common side effect.[49] Animal studies have shown a direct sympathetic activator effect, in addition to its effects through baroreflex.[50] Additional side effects include headache, flushing, and local phlebitis after prolonged infusion in a single site.[49] Nicardipine is rapidly and extensively metabolized by the liver and should be avoided in patients with hepatic impairment.[33] The manufacturer dose range is between 5–15 mg/hr, but in our experience, up to 25 mg/hr can be tolerated safely.[1],[51]
5.5. Clevidipine
Clevidipine is the newest, ultrashort, dihydropyridine calcium channel blocker.[52] It is a pure arteriodilator, and does not affect the venous tone or cardiac muscle contractility.[53] It is given as a lipid emulsion as it is water insoluble.[54] This agent should be avoided in patients with egg and soybean allergy.[55] It has rapid onset and offset of action. It has been shown to achieve the first 15% reduction in SBP within 5–6 minutes of intravenous administration.[56],[57] Its antihypertensive effects are abolished 5–15 minutes after weaning off the medication in most patients.[55]
Clevidipine had also achieved significant reduction in BP in patients with acute HTN when compared to placebo in the ESCAPE I & II trials.[56],[57] When compared to nitroglycerin, nitroprusside, and nicardipine in ECLIPSE trial, it showed comparable safety profile to them, and a significant reduction in mortality.[40] Indeed, it was more effective than nitroglycerin (P = 0.0006) and nitroprusside (P = 0.003) in maintaining BP within the predetermined range.[40] This agent was as effective as nicardipine, in maintaining BP within a predetermined range.[40] The VELOCITY trial showed a rapid and effective reduction in BP, with a decrease of 6% of BP within three minutes, 15% within 9.5 minutes and a 27% reduction in BP 18 hours after infusion initiation.[58] Clevidipine does not induce a reflex increase in heart rate. It has coronary vasodilatory properties.[53] These anti ischemic properties make clevidipine one of the best options for elderly patients presenting with hypertensive crises.
5.6. Labetalol
Labetalol is a combined α1-adrenergic and β-adrenergic receptors blocker, with greater effect on β-receptors as compared to α-receptors.[1] Labetalol can be administered either as a bolus or continuous infusion.[59] It has negative chronotropic and inotropic effects, which made it one of the preferred agents in the management of hypertensive crises in acute aortic dissection.[16],[23] Labetalol was compared with nicardipine in the CLUE trial; and results showed that nicardipine is more likely than labetalol to achieve target blood pressure within 30 minutes.[60] Reported side effects include hypotension, bradycardia nausea, vomiting, scalp tingling, and burning sensation in the groin.[61] In elderly, labetalol's side effects are even more significant, mainly due to delayed clearance of the agent in elderly.[62]
5.7. Esmolol
Esmolol is an ultrashort cardioselective beta-blocker.[16] It is mainly used for post-operative HTN; and in combination with nicardipine or nitroglycerin to maintain hemodynamic stability in the perioperative period.[63]
Esmolol is well tolerated in patients with myocardial infarction and patients with contraindications for other beta-blockers.[64] This agent is contraindicated in congestive heart failure, bradycardia, and chronic obstructive pulmonary disease.[32],[64] In the authors' experience, these contraindications are relative.[34] Esmolol is particularly useful in situations in which the cardiac output, BP, and heart rate are increased.[28] The onset of action is within 60 seconds, and the duration of action is upon 20 minutes.[16] The loading dose is 0.5–1 mg/kg over 1 minute, and the maintenance is infusion of 50 µg/kg/min.[28] The metabolism of esmolol is through hydrolysis of ester linkages by esterases of erythrocytes.[34] Esmolol is safe in elderly patients because it can be easily titrated.[65]
5.8. Clonidine
Clonidine was first used as a nasal decongestant, but because of its other effects, such as hypotension, bradycardia, and sedation, is now used in other conditions.[66] This drug is an alpha2-adrenergic agonist (affinity 200:1 vs. alpha1 receptors) and an agonist at the imidazoline receptors.[67] Its hypotensive effect is secondary to stimulation of the alpha-adrenergic receptors in the vasomotor center of medulla oblongata, and a decrease in renin and aldosterone.[67] These effects are elicited within 30 minutes of oral administration, with peak plasma levels achieved within 2–4 hours, and half-life is 12 to 16 hours.[28],[34],[65] However, the antihypertensive effects may persist 24 hours or more.[68] Clonidine is almost completely absorbed after oral administration.[66] The metabolism of this agent is primarily by hepatic (-50%) and the excretion is 40%–60% in the urine, and 20% in feces.[69] Clonidine is used in severe HTN associated with pain and anxiety, due to its sedative-analgesic effects. Rapid withdrawal from this medication may cause rebound HTN.[28],[34],[65] This agent must be used with caution in the elderly, as confusion may be a significant side effect.[70]
5.9. Fenoldopam
Fenoldopam is a selective dopamine type-1 receptor agonist that works by increasing renal blood flow, improving renal function, and stimulating natriuresis.[71],[72] This drug has an onset of action of 5–10 minutes with a half-life of five min.[73] It is rapidly metabolized by hepatic methylation without participation of cytochrome P450 enzymes, and the excretion is mostly by urine (90%).[65] Fenoldopam is preferred in hypertensive emergencies mediated by renal arterial disease, glomerulonephritis, or vascular diseases with impaired renal function.[23] Fenoldopam can be used also in hypertensive emergencies in perioperative situations.[32] Recommended dosage of this agent is 0.01–1.5 µg/kg/min and the titration is recommended by increase of 0.05–0.1 µg/kg/min every 15 min.[34]
Intravenous fenoldopam has no effect on the central nervous system, and does not cross the blood-brain barrier.[32] Due to its properties, it is considered a choice of treatment in elderly to reduce BP in severe HTN with acute kidney injury, heart failure, and in perioperative situations, specifically in vascular surgery.[32]
5.10. Hydralazine
Hydralazine is a vasodilator that elicits effects purely on the arterial system.[14] It is thought that it inhibits calcium influx in vascular smooth muscle cells, causing hyperpolarization of the cell membrane, or induces cGMP.[65] Hydralazine has an onset of action of 5–15 min and a half-life of only three hours.[74] However, its antihypertensive effects are completely unpredictable, and can last up to 24 hours.[75] Hydralazine remains a common agent in the treatment of preeclampsia and eclampsia.[76] However, new evidence shows that hydralazine can cause maternal hypotension and is harmful to fetus.[32] Other adverse effects of hydralazine include reflex tachycardia, severe hypotension, and oxygen consumption.[28] Hydralazine should be avoided in patients with cardiomyopathies.[77] Recommended dosage of intravenous hydralazine is 10–20 mg.[32] Because of its large number of adverse effects, poor safety of dosage, and unpredictable antihypertensive effects, we do not recommend its use in the elderly patients.[1],[34],[51]
5.11. Phentolamine
Phentolamine is a reversible α1- and α2 antagonist receptor.[78] It is mostly used to treat hypertensive emergencies due to a sympathetic crises, such as pheochromocytoma, interactions between monoamine oxidase inhibitors and other drugs or food, cocaine toxicity, amphetamine overdose, or clonidine withdrawal.[19],[78]–[80] This agent may cause tachydysrhythmias or angina in the elderly. This agent may cause tachydysrhythmias or angina in the elderly. Once the patient's BP is controlled, it is recommended to switch to oral phenoxybenzamine.[4]
6. Other agents
Several other agents have been used to treat hypertensive crises in the elderly, including enalaprilat, diazoxide, and trimethaphan camsylate.[81]–[83] However, these drugs are associated with significant side effects, and should not be considered as primary choices in elderly patients.[84]
Enalaprilat is an intravenous angiotensin converting enzyme (ACE) inhibitor, with an onset of action of 15 min.[85] It may be beneficial in managing hypertensive crises with congestive heart failure in some patients.[81] As an ACE inhibitor, it can potentially compromise the already declined renal function in elderly patients making it less favorable option.[16] In addition, reflex tachycardia due to hypotension may be present.[4],[34]
Trimethaphan camsylate is a non-depolarizing sympathetic and parasympathetic ganglia blocker.[4] It competes with acetylcholine for cholinergic receptors.[4] This medication is effective in decreasing BP, but is associated with significant side effects, including tachycardia and exacerbation of ischemic heart disease; therefore, its use should be avoided in the elderly.[86]
Diazoxide is another potent peripheral vasodilating agent.[87] When administered intravenously, diazoxide can precipitate severe hypotension and ischemic heart disease.[88]
All of these therapeutic agents, in our opinion, are dangerous options in managing hypertensive crises in the elderly and should be avoided.
7. Conclusions
The management of hypertensive crises in the elderly is a clinical challenge to the treating clinician. The pathophysiological changes in these patients make them more vulnerable to complications. Therefore, extensive knowledge of the available agents, their side effects, and interactions with other agents, is essential for a successful outcome. We recommend using easily titratable agents, such as clevidipine, nicardipine, esmolol, and fenoldopam as first choices and avoid agents such as nitroprusside, hydralazine, and nifedipine due to their established side effects.
References
- 1.Padilla Ramos A, Varon J. Current and newer agents for hypertensive emergencies. Curr Hypertens Rep. 2014;16:450. doi: 10.1007/s11906-014-0450-z. [DOI] [PubMed] [Google Scholar]
- 2.Zampaglione B, Pascale C, Marchisio M, et al. Hypertensive urgencies and emergencies. Prevalence and clinical presentation(查到的文献题目中多了标黄的部分) Hypertension. 1996;27:144–147. doi: 10.1161/01.hyp.27.1.144. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension J Am Coll Cardiol. 2018;71:2199–2269. 2017. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Varon J, Strickman N. Diagnosis and treatment of hypertensive crises in the elderly patients. J Geriatr Cardiol. 2007;4:50–51. [Google Scholar]
- 5.Fryar CD, Ostchega Y, Hales CM, et al. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 6.Nwankwo T, Yoon SS, Burt V, et al. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013:1–8. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention, National Center for Health Statistics. About Uunderlying cCause of dDeath 1999–2016, 2017. on CDC WONDER Online Database, released December, 2017. Data are from the Multiple Cause of Death Files, 1999–2016, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. [(accessed Apr 26, 2018)]. Accessed at http://wonder.cdc.gov/ucd-icd10.html on.
- 8.Bennett NM, Shea S. Hypertensive emergency: case criteria, sociodemographic profile, and previous care of 100 cases. Am J Public Health. 1988;78:636–640. doi: 10.2105/ajph.78.6.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaplan NM. Treatment of hypertensive emergencies and urgencies. Heart Dis Stroke. 1992;1:373–378. [PubMed] [Google Scholar]
- 10.Smith CB, Flower LW, Reinhardt CE, et al. Control of hypertensive emergencies. Postgrad Med. 1991;89:111–6. 119. doi: 10.1080/00325481.1991.11700894. [DOI] [PubMed] [Google Scholar]
- 11.Marik PE, Varon J. Perioperative hypertension: a review of current and emerging therapeutic agents. J Clin Anesth. 2009;21:220–229. doi: 10.1016/j.jclinane.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Chobanian A, Bakris G, Black H, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 13.Katz JN, Gore JM, Amin A, et al. Practice patterns, outcomes, and end-organ dysfunction for patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) registry. Am Heart J. 2009;158:599–606. doi: 10.1016/j.ahj.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Lionakis N, Mendrinos D, Sanidas E, et al. Hypertension in the elderly. World J Cardiol. 2012;4:135–147. doi: 10.4330/wjc.v4.i5.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dharmashankar K, Widlansky ME. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. 2010;12:448–455. doi: 10.1007/s11906-010-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68:283–297. doi: 10.2165/00003495-200868030-00003. [DOI] [PubMed] [Google Scholar]
- 17.Singh M. Hypertensive crisis-pathophysiology, initial evaluation, and management. JICC. 2011;1:36–39. [Google Scholar]
- 18.Pinna G, Pascale C, Fornengo P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter italian study. PLoS ONE. 2014;9:e93542. doi: 10.1371/journal.pone.0093542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliott WJ. Clinical features in the management of selected hypertensive emergencies. Prog Cardiovasc Dis. 2006;48:316–325. doi: 10.1016/j.pcad.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Tulman DB, Stawicki SP, Papadimos TJ, et al. Advances in management of acute hypertension: a concise review. Discov Med. 2012;13:375–383. [PMC free article] [PubMed] [Google Scholar]
- 21.Muiesana ML, Salvettia M, Amadorob V, et al. An update on hypertensive emergencies and urgencies. J Cardiovasc Med. 2015;16:372–382. doi: 10.2459/JCM.0000000000000223. [DOI] [PubMed] [Google Scholar]
- 22.Li JZ, Eagle KA, Vaishnava P, et al. Hypertensive and acute aortic syndromes. Cardiol Clin. 2013;31:493–501. doi: 10.1016/j.ccl.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 23.Gupta PK, Gupta H, Khoynezhad A, et al. Hypertensive emergency in aortic dissection and thoracic aortic aneurysm—a review of management. Pharmaceuticals. 2009;2:66–76. doi: 10.3390/ph2030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bath PM, Krishnan K. Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database Syst Rev. 2014;10:CD000039. doi: 10.1002/14651858.CD000039.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Butcher KS, Jeerakathil T, Hill M, et al. ICH ADAPT Investigators: The IntraCerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial (ICH ADAPT) Stroke. 2013;44:620–626. doi: 10.1161/STROKEAHA.111.000188. [DOI] [PubMed] [Google Scholar]
- 26.Anderson CS, Heeley E, Huang Y, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–2365. doi: 10.1056/NEJMoa1214609. [DOI] [PubMed] [Google Scholar]
- 27.Divakaran S, Loscalzo J. The role of nitroglycerin and other nitrogen oxides in cardiovascular therapeutics. J Am Coll Cardiol. 2017;70:2393–2410. doi: 10.1016/j.jacc.2017.09.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marik PE, Rivera R. Hypertensive emergencies:an update. Curr Opin Crit Care. 2011;17:569–580. doi: 10.1097/MCC.0b013e32834cd31d. [DOI] [PubMed] [Google Scholar]
- 29.Ranadive SM, Eugene AR, Dillon G, et al. Comparison of the vasodilatory effects of sodium nitroprusside vs. nitroglycerin. J Appl Physiol. 2017;123:402–406. doi: 10.1152/japplphysiol.00167.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vuylsteke A, Vincent JL, Payen de La Garanderie DP, et al. Characteristics, practice patterns, and outcomes in patients with acute hypertension: European registry for studying the treatment of acute hypertension (Euro-STAT) Crit Care. 2011;15:R271. doi: 10.1186/cc10551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 2. Am J Health Syst Pharm. 2009;66:1448–1457. doi: 10.2146/ajhp080348.p2. [DOI] [PubMed] [Google Scholar]
- 32.Sarafidis PA, Georgianos PI, Malindretos P, et al. Pharmacological management of hypertensive emergencies and urgencies: focus on newer agents. Expert Opin Investig Drugs. 2012;21:1089–1106. doi: 10.1517/13543784.2012.693477. [DOI] [PubMed] [Google Scholar]
- 33.Varon J. The diagnosis and treatment of hypertensive crises. Postgrad Med. 2009;121:5–13. doi: 10.3810/pgm.2009.01.1950. [DOI] [PubMed] [Google Scholar]
- 34.Varon J, Marik PE. The diagnosis and management of hypertensive crisis. Chest. 2000;118:214–227. doi: 10.1378/chest.118.1.214. [DOI] [PubMed] [Google Scholar]
- 35.Friederich JA, Butterworth JD., 4th Sodium nitroprusside: twenty years and counting. Anesth Analg. 1995;81:152–162. doi: 10.1097/00000539-199507000-00031. [DOI] [PubMed] [Google Scholar]
- 36.Rindone JP, Sloane EP. Cyanide toxicity from sodium nitroprusside: risks and management. Ann Pharmacother. 1992;26:515–519. doi: 10.1177/106002809202600413. [DOI] [PubMed] [Google Scholar]
- 37.Nightingale S. From the food and drug administration. JAMA. 1991;265:847. [PubMed] [Google Scholar]
- 38.Mayer SA, Kurtz P, Wyman A, et al. Clinical practices, complications, and mortality in neurological patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) registry. Crit Care Med. 2011;39:2330–2336. doi: 10.1097/CCM.0b013e3182227238. [DOI] [PubMed] [Google Scholar]
- 39.Wood M, Hyman S, Wood AJ, et al. A clinical study of sensitivity to sodium nitroprusside during controlled hypotensive anesthesia in young and elderly patients. Anesth Analg. 1987;66:132–136. [PubMed] [Google Scholar]
- 40.Aronson S, Dyke CM, Stierer KA, et al. The ECLIPSE trials: comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth Analg. 2008;107:1110–1121. doi: 10.1213/ane.0b013e31818240db. [DOI] [PubMed] [Google Scholar]
- 41.Ozawa Y, Hayashi K, Kobori H, et al. New generation calcium channel blockers in hypertensive treatment. Curr Hypertens Rev. 2006;2:103–111. doi: 10.2174/157340206776877370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Harten J, Burggraaf K, Danhof M, et al. Negligible sublingual absorption of nifedipine. Lancet. 1987;12:1363–1365. doi: 10.1016/s0140-6736(87)91258-x. [DOI] [PubMed] [Google Scholar]
- 43.By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel..(查到的是标黄部分) American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–2246. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 44.Grossman E, Messerli FH, Grodzicki T, et al. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996;276:1328–1331. [PubMed] [Google Scholar]
- 45.Varon J, Marik PE. Clinical review: the management of hypertensive crises. Crit Care. 2003;7:374–384. doi: 10.1186/cc2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaplan JA. Clinical considerations for the use of intravenous nicardipine in the treatment of postoperative hypertension. Am Heart J. 1990;119:443–446. doi: 10.1016/s0002-8703(05)80066-3. [DOI] [PubMed] [Google Scholar]
- 47.Malesker MA, Hilleman DE. Intravenous labetalol compared with intravenous nicardipine in the management of hypertension in critically ill patients. J Crit Care. 2012;27:528.e7–528.e14. doi: 10.1016/j.jcrc.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 48.Abboud ME, Frasure SE. Bradycardia caused by intravenous nicardipine in an elderly patient with acute ischemic infarct. Am J Emerg Med. 2016;34:761.e1–761.e2. doi: 10.1016/j.ajem.2015.08.030. [DOI] [PubMed] [Google Scholar]
- 49.Wallin JD, Cook ME, Blanski L, et al. Intravenous nicardipine for the treatment of severe hypertension. Am J Med. 1988;85:331–338. doi: 10.1016/0002-9343(88)90582-7. [DOI] [PubMed] [Google Scholar]
- 50.Damase-Michel C, Valet P, Montastruc JL, et al. Nicardipine causes sympathetic activation that does not involve baroreceptor reflex tachycardia in conscious sinoaortic-denervated dogs. Eur J Pharmacol. 1987;142:145–149. doi: 10.1016/0014-2999(87)90665-0. [DOI] [PubMed] [Google Scholar]
- 51.Varon J, Marik PE. Perioperative hypertension management. Vasc Health Risk. 2008;4:615–627. doi: 10.2147/vhrm.s2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vuylsteke A, Milner Q, Ericsson H, et al. Pharmacokinetics and pulmonary extraction of clevidipine, a new vasodilating ultrashort-acting dihydropydine, during bypass. Br J Anaesth. 2000;85:683–689. doi: 10.1093/bja/85.5.683. [DOI] [PubMed] [Google Scholar]
- 53.Kieler-Jensen N, Jolin-Mellgard A, Nordlander M, et al. Coronary and systemic hemodynamic effects of clevidipine, an ultra-short-acting calcium antagonist, for treatment of hypertension after coronary artery surgery. Acta Anaesthesiol Scand. 2000;44:186–193. doi: 10.1034/j.1399-6576.2000.440210.x. [DOI] [PubMed] [Google Scholar]
- 54.Ericsson H, Fakt C, Jolin-Mellgard A, et al. Clinical and pharmacokinetic results with a new ultrashort-acting calcium antagonist, clevidipine, following gradually increasing intravenous doses to healthy volunteers. Br J Clin Pharmacol. 1999;47:531–538. doi: 10.1046/j.1365-2125.1999.00933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.The Medicines Company: Cleviprex (Clevidipine Butyrate) injectable emulsion for intravenous use: US prescribing information, 2008. [online] [([Last accessed Feb, 22 February 2018)]]. Available from: CHIESI USA, Inc. website http://resources.chiesiusa.com/Cleviprex/CLEVIPREX_US_PI.pdf.
- 56.Levy JH, Mancao MY, Gitter R, et al. Clevidipine effectively and rapidly controls blood pressure preoperatively in cardiac surgery patients: the results of the randomized, placebo-controlled Efficacy Study of clevidipine assessing its preoperative antihypertensive effect in cardiac surgery-1. Anesth Analg. 2007;105:918–925. doi: 10.1213/01.ane.0000281443.13712.b9. [DOI] [PubMed] [Google Scholar]
- 57.Singla N, Warltier DC, Gandhi SD, et al. Treatment of acute postoperative hypertension in cardiac surgery patients: an efficacy study of clevidipine assessing its postoperative antihypertensive effect in cardiac surgery-2 (ESCAPE-2), a randomized, double-blind, placebo-controlled trial. Anesth Analg. 2008;107:59–67. doi: 10.1213/ane.0b013e3181732e53. [DOI] [PubMed] [Google Scholar]
- 58.Pollack CV, Varon J, Garrison NA, et al. Clevidipine, an intravenous dihydropyridine calcium channel blocker, is safe and effective for the treatment of patients with acute severe hypertension. Ann Emerg Med. 2009;53:329–338. doi: 10.1016/j.annemergmed.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 59.Huey J, Thomas JP, Hendricks DR, et al. Clinical evaluation of intravenous labetalol for the treatment of hypertensive urgency. Am J Hypertens. 1988;1:284s–289s. doi: 10.1093/ajh/1.3.284s. [DOI] [PubMed] [Google Scholar]
- 60.Peacock WF, Varon J, Baumann BM, et al. CLUE: a randomized comparative effectiveness trial of IV nicardipine versus labetalol use in the emergency department. Crit Care. 2011;15:R157. doi: 10.1186/cc10289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.MacCarthy EP, Bloomfield SS. Labetalol: a review of its pharmacology, pharmacokinetics, clinical uses and adverse effects. Pharmacotherapy. 1983;3:193–217. doi: 10.1002/j.1875-9114.1983.tb03252.x. [DOI] [PubMed] [Google Scholar]
- 62.Abernethy DR, Schwartz JB, Plachetka JR, et al. Comparison in young and elderly patient of pharmacodynamics and dispositio of labetalol in systemic hypertension. Am J Cardiol. 1987;60:697–702. doi: 10.1016/0002-9149(87)90385-7. [DOI] [PubMed] [Google Scholar]
- 63.Sun SH, Yang L, Sun DF, et al. Effects of vasodilator and esmolol-induced hemodynamic stability on early post-operative cognitive dysfunction in elderly patients: a randomized trial. Afr Health Sci. 2017;16:1056–1066. doi: 10.4314/ahs.v16i4.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mooss AN, Hileman DE, Mohiuddin SM, et al. Safety of esmolol in patients with acute myocardial infarction trated with thrombolytic therapy who had relative contraindications to beta-blocker therapy. Ann Pharmacother. 1994;28:701–703. doi: 10.1177/106002809402800601. [DOI] [PubMed] [Google Scholar]
- 65.Salgado DR, Silva E, Vincent JL, et al. Control of hypertension in the critically ill: a pathophysiological approach. Ann Intensive Care. 2013;3:17. doi: 10.1186/2110-5820-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Giovannitti JA, Thoms SM, Crawford JJ, et al. Alpha-2 adrenergic receptor agonists: a review of current clinical applications. Anesth Prog. 2015;62:31–39. doi: 10.2344/0003-3006-62.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Neil M. Clonidine: clinical pharmacology and therapeutic use in pain management. Curr Clin Pharmacol. 2011;6:280–287. doi: 10.2174/157488411798375886. [DOI] [PubMed] [Google Scholar]
- 68.Lowenthal DT, Matzek KM, MacGregor TR, et al. Clinical pharmacokinetics of clonidine. Clin Pharmacokinet. 1988;14:287–310. doi: 10.2165/00003088-198814050-00002. [DOI] [PubMed] [Google Scholar]
- 69.Anderson RJ, Reed WG. Current concepts in treatment of hypertensive urgencies. Am Heart J. 1986;111:211–219. doi: 10.1016/0002-8703(86)90583-1. [DOI] [PubMed] [Google Scholar]
- 70.Fleg JL, Aronow WS, Frishman WH, et al. Cardiovascular drug therapy in the elderly: benefits and challenges. Nat Rev Cardiol. 2011;8:13–28. doi: 10.1038/nrcardio.2010.162. [DOI] [PubMed] [Google Scholar]
- 71.Shusterman NH, Elliott WJ, White WB, et al. Fenoldopam, but not nitroprusside, improves renal function in secerly hypertensive patients with impaired renal function. Am J Med. 1993;95:161–168. doi: 10.1016/0002-9343(93)90256-o. [DOI] [PubMed] [Google Scholar]
- 72.Elliott WJ, Weber RR, Nelson KS, et al. Renal and hemodynamic effects of intravenous fenoldopam versus nitroprusside in severe hypertension. Circulation. 1990;81:970–977. doi: 10.1161/01.cir.81.3.970. [DOI] [PubMed] [Google Scholar]
- 73.White WB, Radford MJ, Gonzalez FM, et al. Selective dopamine-1 agonist therapy in severe hypertension: effects of intravenous fenoldopam. J Am Coll Cardiol. 1988;11:1118–1123. doi: 10.1016/s0735-1097(98)90073-0. [DOI] [PubMed] [Google Scholar]
- 74.O'Malley K, Segal JL, Israili ZH, et al. Duration of hydralazine action in hypertension. Clin Pharmacol Ther. 1975;18:581–586. doi: 10.1002/cpt1975185part1581. [DOI] [PubMed] [Google Scholar]
- 75.Ludden TM, Shepherd AM, McNay JL, et al. Hydralazine kinetics in hypertensive patients after intravenous administration. Clin Pharmacol Ther. 1980;28:736–742. doi: 10.1038/clpt.1980.229. [DOI] [PubMed] [Google Scholar]
- 76.Magee LA, Abalos E, von Dadelszen P, et al. How to manage hypertension in pregnancy effectively. Br J Clin Pharmacol. 2011;72:394–401. doi: 10.1111/j.1365-2125.2011.04002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Powers DR, Papadakos PJ, Wallin JD, et al. Parenteral hydralazine revisited. J Emerg Med. 1998;16:191–196. doi: 10.1016/S0736-4679(97)00287-4. [DOI] [PubMed] [Google Scholar]
- 78.Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 1. Am J Health-Syst Pharm. 2009;66:1343–1352. doi: 10.2146/ajhp080348.p1. [DOI] [PubMed] [Google Scholar]
- 79.Tuncel M, Ram VC. Hypertensive emergencies. Am J Cardiovasc Drugs. 2003;3:21–31. doi: 10.2165/00129784-200303010-00003. [DOI] [PubMed] [Google Scholar]
- 80.Fenves AZ, Ram CV. Drug treatment of hypertensive urgencies and emergencies. Semin Nephrol. 2005;25:272–280. doi: 10.1016/j.semnephrol.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 81.MacFadyen RJ, Lees KR, Reid JL, et al. Double blind controlled study of low dose intravenous perindoprilat or enalaprilat infusion in elderly patients with heart failure. Br Heart J. 1993;69:293–297. doi: 10.1136/hrt.69.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huysmans F, Thien T, Koene R, et al. Acute treatment of hypertension with slow infusion of diazoxide. Arch Intern Med. 1983;143:882–884. [PubMed] [Google Scholar]
- 83.Stumpf JL. Drug therapy of hypertensive crises. Clin Pharm. 1988;7:582–591. [PubMed] [Google Scholar]
- 84.Hirschl MM, Binder M, Bur A, et al. Clinical evaluation of different doses of intravenous enalaprilat in patients with hypertensive crises. Arch Intern Med. 1995;155:2217–2223. [PubMed] [Google Scholar]
- 85.I. Merck: Vasotec® I.V.(enalaprilat) prescribing information [online]. Merck website. [(a[Accessed April, 26 2018)]]. Available from URL: https://www.merck.ca/static/pdf/VASOTEC-PM_E.pdf.
- 86.Gifford RW., Jr Management of hypertensive crises. JAMA. 1991;266:829–835. [PubMed] [Google Scholar]
- 87.Koch-Weser J. Diazoxide. N Engl J Med. 1976;294:1271–1274. doi: 10.1056/NEJM197606032942306. [DOI] [PubMed] [Google Scholar]
- 88.Reuler JB, Magarian GJ. Hypertensive emergencies and urgencies: definition, recognition, and management. J Gen Intern Med. 1988;31:64–74. doi: 10.1007/BF02595759. [DOI] [PubMed] [Google Scholar]